The Role of Health Belief Model Constructs and Content Creator Characteristics in Social Media Engagement: Insights from COVID-19 Vaccine Tweets
Abstract
:1. Introduction
1.1. HBM Construct and Social Media Messages
1.2. Social Media User Engagement
1.3. The Present Study
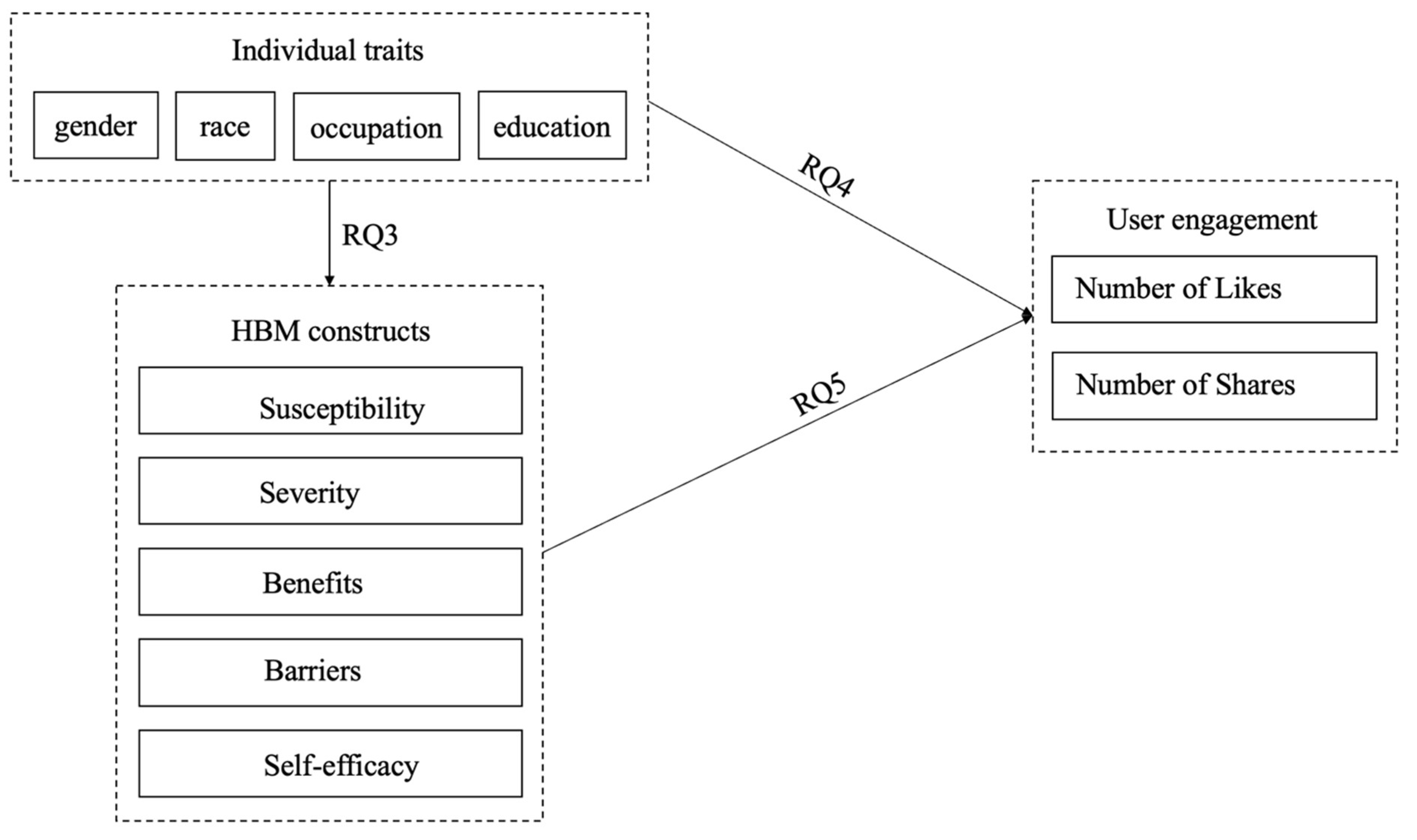
- RQ1: Which constructs of the HBM are evident in COVID-19 vaccine tweets?
- RQ2: What are the demographic characteristics of the Twitter content creators responsible for generating tweets about the COVID-19 vaccine?
- RQ3: Do the demographic characteristics of Twitter content creators use specific HBM constructs in their tweets?
- RQ4: Are there specific demographic characteristics associated with Twitter content creators that result in higher user engagement?
- RQ5: What HBM constructs are typically used in tweets that lead to higher user engagement?
2. Methods
2.1. Sample
- Selection Based on Significant Events: To ensure the sample was relevant to significant COVID-19 vaccine events, at least one significant event related to the COVID-19 vaccine (e.g., CDC recommends pausing the J&J vaccine) had to have occurred on that date.
- Exclusion of Retweets: Our study focused on the characteristics of tweets and creators leading to user engagement. Therefore, we included only original tweets and excluded retweets.
- High Engagement Tweets: Our sample prioritized tweets with high user engagement that consisted of the top 1000 tweets with the most retweets and the top 1000 tweets with the most favorites.
- Bot Exclusion: To filter out bot-generated tweets, Botometer was used, a tool that assigns a Complete Automation Probability (CAP) score to each Twitter account. Accounts with a CAP score above 95% were labeled as bots.
2.2. Coding Scheme
2.3. Coding Procedures
2.4. Data Analysis
3. Results
3.1. Descriptive Statistics
3.2. Characteristics of COVID-19 Vaccine-Related Posts
3.3. Characteristics of Content Creators and User Engagement
3.4. Characteristics of Content Creators and Use of HBM in Social Media Posts
3.5. Relationship between HBM Use in Social Media Posts and User Engagement
4. Discussion
4.1. Implications
4.2. Limitations and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Su, Z.; Wen, J.; McDonnell, D.; Goh, E.; Li, X.; Šegalo, S.; Ahmad, J.; Cheshmehzangi, A.; Xiang, Y.-T. Vaccines are not yet a silver bullet: The imperative of continued communication about the importance of COVID-19 safety measures. Brain Behav. Immun. Health 2021, 12, 100204. [Google Scholar] [CrossRef]
- Jia, X.; Ahn, S.; Carcioppolo, N. Measuring information overload and message fatigue toward COVID-19 prevention messages in USA and China. Health Promot. Int. 2023, 38, daac003. [Google Scholar] [CrossRef]
- Chaurasia, R.; Ghose, U. Social media and the COVID-19 pandemic: Boons and banes. Digit. Innov. Pandemics 2022, 183–223. [Google Scholar]
- Huang, Q.; Mao, B.; Jia, X.; Peng, W. COVID-19 information overload mediated the effects of cross-channel information differences on health information elaboration. J. Health Commun. 2023, 28, 401–411. [Google Scholar] [CrossRef]
- Abuhashesh, M.Y.; Al-Dmour, H.; Masa’deh, R.; Salman, A.; Al-Dmour, R.; Boguszewicz-Kreft, M.; AlAmaireh, Q.N. The Role of Social Media in Raising Public Health Awareness during the Pandemic COVID-19: An International Comparative Study. Informatics 2021, 8, 80. [Google Scholar] [CrossRef]
- Mao, B.; Jia, X.; Huang, Q. How do information overload and message fatigue reduce information processing in the era of COVID-19? An ability–motivation approach. J. Inf. Sci. 2022, 01655515221118047. [Google Scholar] [CrossRef]
- Bonnevie, E.; Gallegos-Jeffrey, A.; Goldbarg, J.; Byrd, B.; Smyser, J. Quantifying the rise of vaccine opposition on Twitter during the COVID-19 pandemic. J. Commun. Health 2020, 14, 12–19. [Google Scholar] [CrossRef]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccines Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef]
- Gillani, N.; Yuan, A.; Saveski, M.; Vosoughi, S.; Roy, D. Me, My Echo Chamber, and I. In Proceedings of the 2018 World Wide Web Conference, Lyon, France, 23–27 April 2018; pp. 823–831. [Google Scholar] [CrossRef]
- Rosenstock, I.M. Historical Origins of the Health Belief Model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Glanz, K.; Rimer, B.K.; Viswanath, K. Health Behavior and Health Education: Theory, Research, and Practice; Jossey-Bass: Hoboken, NJ, USA, 2008. [Google Scholar]
- Alhaimer, R.; Villace, T. The health belief model: Evaluating governmental public health messages on social media aimed at preventing a COVID-19 epidemic in Kuwait. Cogent Bus. Manag. 2022, 9, 2031682. [Google Scholar] [CrossRef]
- Zhang, X.; Baker, K.; Pember, S.; Bissell, K. Persuading Me to Eat Healthy: A Content Analysis of YouTube Public Service Announcements Grounded in the Health Belief Model. South. Commun. J. 2017, 82, 38–51. [Google Scholar] [CrossRef]
- Guidry, J.P.; Carlyle, K.E.; LaRose, J.G.; Perrin, P.; Messner, M.; Ryan, M. Using the Health Belief Model to Analyze Instagram Posts about Zika for Public Health Communications. Emerg. Infect. Dis. 2019, 25, 179–180. [Google Scholar] [CrossRef]
- Raamkumar, A.S.; Tan, S.G.; Wee, H.L. Use of Health Belief Model–Based Deep Learning Classifiers for COVID-19 Social Media Content to Examine Public Perceptions of Physical Distancing: Model Development and Case Study. JMIR Public Health Surveill. 2020, 6, e20493. [Google Scholar] [CrossRef] [PubMed]
- Du, J.; Cunningham, R.M.; Xiang, Y.; Li, F.; Jia, Y.; Boom, J.A.; Myneni, S.; Bian, J.; Luo, C.; Chen, Y.; et al. Leveraging deep learning to understand health beliefs about the Human Papillomavirus Vaccine from social media. NPJ Digit. Med. 2019, 2, 27. [Google Scholar] [CrossRef]
- Guidry, J.P.; Laestadius, L.I.; Vraga, E.K.; Miller, C.A.; Perrin, P.B.; Burton, C.W.; Ryan, M.; Fuemmeler, B.F.; Carlyle, K.E. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am. J. Infect. Control 2021, 49, 137–142. [Google Scholar] [CrossRef]
- Anuar, H.; Shah, S.A.; Gafor, H.; Mahmood, M.I.; Ghazi, H.F. Usage of Health Belief Model (HBM) in health behavior: A systematic review. Malays. J. Med. Health Sci. 2020, 16, 2636–9346. [Google Scholar]
- Becker, M.H. The health belief model and personal health behavior. Health Educ. Monogr. 1974, 2, 324–473. [Google Scholar] [CrossRef]
- Carpenter, C.J. A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior. Health Commun. 2010, 25, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Harrison, J.A.; Mullen, P.D.; Green, L.W. A meta-analysis of studies of the Health Belief Model with adults. Health Educ. Res. 1992, 7, 107–116. [Google Scholar] [CrossRef]
- Janz, N.K.; Becker, M.H. The Health Belief Model: A Decade Later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef]
- Jones, C.L.; Jensen, J.D.; Scherr, C.L.; Brown, N.R.; Christy, K.; Weaver, J. The Health Belief Model as an Explanatory Framework in Communication Research: Exploring Parallel, Serial, and Moderated Mediation. Health Commun. 2015, 30, 566–576. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, R.S.; Vernberg, D. Models of preventative health behavior: Comparison, critique and meta-analysis. In Advances in Medical Sociology, Health Behavior Models: A Reformulation; Albrecht, G., Ed.; JAI Press: Greenwich, CT, USA, 1994; pp. 45–67. [Google Scholar]
- Chen, M.-F.; Wang, R.-H.; Schneider, J.K.; Tsai, C.-T.; Jiang, D.D.-S.; Hung, M.-N.; Lin, L.-J. Using the Health Belief Model to Understand Caregiver Factors Influencing Childhood Influenza Vaccinations. J. Community Health Nurs. 2011, 28, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Mesch, G.S.; Schwirian, K.P. Social and political determinants of vaccine hesitancy: Lessons learned from the H1N1 pandemic of 2009–2010. Am. J. Infect. Control 2015, 43, 1161–1165. [Google Scholar] [CrossRef]
- Smith, P.J.; Humiston, S.G.; Marcuse, E.K.; Zhao, Z.; Dorell, C.G.; Howes, C.; Hibbs, B. Parental Delay or Refusal of Vaccine Doses, Childhood Vaccination Coverage at 24 Months of Age, and the Health Belief Model. Public Health Rep. 2011, 126, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Donadiki, E.M.; Jiménez-García, R.; Hernández-Barrera, V.; Sourtzi, P.; Carrasco-Garrido, P.; de Andrés, A.L.; Velonakis, E.G. Health Belief Model applied to non-compliance with HPV vaccine among female university students. Public Health 2014, 128, 268–273. [Google Scholar] [CrossRef]
- Terrasse, M.; Gorin, M.; Sisti, D. Social media, e-health, and medical ethics. Hastings Cent. Rep. 2019, 49, 24–33. [Google Scholar] [CrossRef]
- O’Brien, H.L.; Toms, E.G. What is user engagement? A conceptual framework for defining user engagement with technology. J. Am. Soc. Inf. Sci. Technol. 2008, 59, 938–955. [Google Scholar] [CrossRef]
- Schivinski, B.; Christodoulides, G.; Dabrowski, D. Measuring Consumers’ Engagement with Brand-Related Social-Media Content. J. Advert. Res. 2016, 56, 64–80. [Google Scholar] [CrossRef]
- Bryła, P.; Chatterjee, S.; Ciabiada-Bryła, B. The Impact of Social Media Marketing on Consumer Engagement in Sustainable Consumption: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 16637. [Google Scholar] [CrossRef]
- Ibrahim, N.F.; Wang, X.; Bourne, H. Exploring the effect of user engagement in online brand communities: Evidence from Twitter. Comput. Hum. Behav. 2017, 72, 321–338. [Google Scholar] [CrossRef]
- Voorveld, H.A.M.; van Noort, G.; Muntinga, D.G.; Bronner, F. Engagement with Social Media and Social Media Advertising: The Differentiating Role of Platform Type. J. Advert. 2018, 47, 38–54. [Google Scholar] [CrossRef]
- Manthanam, A.; Sanghvi, H.; Saini, G.; Patel, K.; Agarwal, V. Impact of content, context and creator on user engagement on Instagram. Int. J. Multidiscip.Res. 2022, 4, 1–7. [Google Scholar]
- Gilbert, E.; Bakhshi, S.; Chang, S.; Terveen, L. "I need to try this"? A statistical overview of Pinterest. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Paris, France, 27 April–2 May 2013; pp. 2427–2436. [Google Scholar]
- Jaakonmäki, R.; Müller, O.; Vom Brocke, J. The impact of content, context, and creator on user engagement in social media marketing. In Proceedings of the 50th Hawaii International Conference on System Sciences, Hawaii, USA, 4–7 January 2017. [Google Scholar]
- Chandler, R.; Guillaume, D.; Parker, A.G.; Mack, A.; Hamilton, J.; Dorsey, J.; Hernandez, N.D. The impact of COVID-19 among Black women: Evaluating perspectives and sources of information. Ethn. Health 2021, 26, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Seelig, M.I.; Millette, D.; Zhou, C.; Huang, J. A new culture of advocacy: An exploratory analysis of social activism on the web and social media. Atl. J. Commun. 2019, 27, 15–29. [Google Scholar] [CrossRef]
- Chapman, S. Does celebrity involvement in public health campaigns deliver long term benefit? Yes. BMJ 2012, 345, e6364. [Google Scholar] [CrossRef]
- Veale, H.J.; Sacks-Davis, R.; Weaver, E.R.; Pedrana, A.E.; Stoové, M.A.; Hellard, M.E. The use of social networking platforms for sexual health promotion: Identifying key strategies for successful user engagement. BMC Public Health 2015, 15, 85. [Google Scholar] [CrossRef]
- Zhang, Y.; Xia, T.; Huang, L.; Yin, M.; Sun, M.; Huang, J.; Ni, Y.; Ni, J. Factors Influencing User Engagement of Health Information Disseminated by Chinese Provincial Centers for Disease Control and Prevention on WeChat: Observational Study. JMIR mHealth uHealth 2019, 7, e12245. [Google Scholar] [CrossRef]
- Marsh, D.; Hart, P.T.; Tindall, K. Celebrity politics: The politics of the late modernity? Political Stud. Rev. 2010, 8, 322–340. [Google Scholar] [CrossRef]
- Wheeler, M. Celebrity Politics; Polity: Cambridge, UK, 2013. [Google Scholar]
- Wu, Z.; Liao, J.; Zhang, L. Predicting on retweeting of hot topic tweets in microblog. In Proceedings of the IEEE International Conference on Broadband Network & Multimedia Technology, Guilin, China, 17–19 November 2013; pp. 119–123. [Google Scholar]
- Xu, Z.; Yang, Q. Analyzing user retweet behavior on twitter. In Proceedings of the IEEE/ACM International Conference on Advances in Social Networks Analysis and Mining, Istanbul, Türkiye, 26–29 August 2012; pp. 46–50. [Google Scholar]
- Krippendorff, K. Content Analysis: An Introduction to Its Methodology, 4th ed.; SAGE: Los Angeles, CA, USA, 2019. [Google Scholar]
- Neuendorf, K.A. The Content Analysis Guidebook; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2017. [Google Scholar] [CrossRef]
- Riffe, D.; Lacy, S.; Watson, B.R.; Lovejoy, J. Analyzing Media Messages: Using Quantitative Content Analysis in Research; Routledge: New York, NY, USA, 2023. [Google Scholar]
- DeVerna, M.R.; Pierri, F.; Truong, B.T.; Bollenbacher, J.; Axelrod, D.; Loynes, N.; Torres-Lugo, C.; Yang, K.-C.; Menczer, F.; Bryden, J. CoVaxxy: A collection of English-language Twitter posts about COVID-19 vaccines. In Proceedings of the AAAI International Conference on Web and Social Media (ICWSM), Buffalo, NY, USA, 3–6 June 2021. [Google Scholar]
- Al-Metwali, B.Z.; Al-Jumaili, A.A.; Al-Alag, Z.A.; Sorofman, B. Exploring the acceptance of COVID-19 vaccine among healthcare workers and general population using health belief model. J. Eval. Clin. Pr. 2021, 27, 1112–1122. [Google Scholar] [CrossRef]
- Chen Li, X.; Gao, J.; Liu, X.; Mao, Y.; Wang, R.; Zheng, P.; Xiao, Q.; Jia, Y.; Fu, H.; Dai, J. Health belief model perspective on the control of COVID-19 vaccine hesitancy and the promotion of vaccination in China: Web-based cross-sectional study. J. Med. Internet Res. 2021, 23, 293–329. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Lau, J.T.; She, R.; Chen, X.; Li, L.; Li, L.; Chen, X. Prevalence and associated factors of intention of COVID-19 vaccination among healthcare workers in China: Application of the Health Belief Model. Hum. Vaccines Immunother. 2021, 17, 2894–2902. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Windows, version 27.0; Computer Software; IBM Corp.: Armonk, NY, USA, 2020. [Google Scholar]
- Perrin, A.; Anderson, M. Share of U.S. Adults Using Social Media, Including Facebook, Is Mostly Unchanged since 2018; Pew Research Center: Washington, DC, USA, 2019. [Google Scholar]
- Cogburn, C.D. Culture, Race, and Health: Implications for Racial Inequities and Population Health. Milbank Q. 2019, 97, 736–761. [Google Scholar] [CrossRef] [PubMed]
- Quinn, S.C.; Jamison, A.M.; An, J.; Hancock, G.R.; Freimuth, V.S. Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: Results of a national survey of White and African American adults. Vaccine 2019, 37, 1168–1173. [Google Scholar] [CrossRef]
- Horton, D.; Richard Wohl, R. Mass communication and para-social interaction: Observations on intimacy at a distance. Psychiatry 1956, 19, 215–229. [Google Scholar] [CrossRef]
- Quinn, S.; Jamison, A.; Musa, D.; Hilyard, K.; Freimuth, V. Exploring the Continuum of Vaccine Hesitancy Between African American and White Adults: Results of a Qualitative Study. PLoS Curr. 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- Viswanath, K. Public Communications and Its Role in Reducing and Eliminating Health Disparities. Examining the Health Disparities Research Plan of the National Institutes of Health: Unfinished Business; Institute of Medicine: Washington, DC, USA, 2006; pp. 215–253. [Google Scholar]
- Massey, P.M.; Kearney, M.D.; Hauer, M.K.; Selvan, P.; Koku, E.; Leader, A.E. Dimensions of Misinformation About the HPV Vaccine on Instagram: Content and Network Analysis of Social Media Characteristics. J. Med. Internet Res. 2020, 22, e21451. [Google Scholar] [CrossRef]
- Ciszek, E.; Haven, P.; Logan, N. Amplification and the limits of visibility: Complicating strategies of trans voice and representations on social media. New Media Soc. 2021, 25, 1605–1625. [Google Scholar] [CrossRef]

| Variables | Sub-Items | Number of Presences/Range | Percent (%) of Presences/M& SD | Cohen’s Kappa |
|---|---|---|---|---|
| Relevance | 0.83 | |||
| Metadata | Coding_ID | |||
| Tweet_ID | ||||
| Created_at | ||||
| Language | ||||
| Full_text | ||||
| Word_counts | 5–55 | M = 33.27 SD = 12.59 | ||
| User_ID | ||||
| User_name | ||||
| Location | ||||
| User_description | ||||
| Number of followers | 122–80,144,312 | M = 2,473,188.10 | ||
| SD = 9,312,872.58 | ||||
| User engagement | Number of likes | 1836–695,439 | M = 19,426.58 | |
| SD = 45,323.17 | ||||
| Number of retweets | 34–112,841 | M = 3778.28 | ||
| SD = 7886.67 | ||||
| Source characteristics | Source | 0.91 | ||
| 1: Organization | 41 | 11.3 | ||
| 2: Individual | 321 | 88.7 | ||
| Gender | 0.91 | |||
| 0: N/A | 58 | 16 | ||
| 1: Female | 111 | 30.7 | ||
| 2: Male | 193 | 53.3 | ||
| Race/ethnicity | 0.88 | |||
| 0: N/A | 95 | 26.2 | ||
| 1: White | 208 | 57.5 | ||
| 2: Black | 35 | 9.7 | ||
| 3: Asian or Pacific Islander | 24 | 6.6 | ||
| 4: American Indian or Alaskan Native | 0 | 0 | ||
| 5: Hispanic | 0 | 0 | ||
| 6: Other | 1 | 0.3 | ||
| Occupation | 0.80 | |||
| 0: N/A | 158 | 43.6 | ||
| 1: Health professionals and public health experts | 45 | 12.4 | ||
| 2: Celebrities (actors, singers, SMIs) | 15 | 4.1 | ||
| 3: Politicians | 43 | 11.9 | ||
| 4: Media practitioners (writers, journalists, anchors) | 66 | 18.2 | ||
| 5: Others (artists, scholars, businessmen, lawyers) | 35 | 9.7 | ||
| Education | 0.91 | |||
| 0: N/A | 316 | 87.3 | ||
| 1: MD | 35 | 9.7 | ||
| 2: PhD | 11 | 3 | ||
| 3: Master’s | 0 | 0 | ||
| 4: Others | 0 | 0 | ||
| Targeting perceived severity | Item1: Death rate is high | 23 | 6.4 | 0.89 |
| Item2: COVID-19 can be fatal | 32 | 8.8 | 0.85 | |
| Item3: COVID-19 has serious after effects | 11 | 3 | 1 | |
| Item4: Lost job | 0 | 0 | N/A | |
| Item5: Family/friends dying | 5 | 1.4 | 1 | |
| Item6: Widespread transmission | 22 | 6.1 | 0.89 | |
| Item7: Social isolation/mental health issues | 1 | 0.3 | N/A | |
| Item8: Expensive treatment | 1 | 0.3 | N/A | |
| Targeting perceived susceptibility | Item1: Elderly people | 1 | 0.3 | N/A |
| Item2: Disadvantaged groups | 1 | 0.3 | N/A | |
| Item3: Healthcare workers | 0 | 0 | N/A | |
| Item4: Pregnant women | 1 | 0.3 | N/A | |
| Item5: Children | 4 | 1.1 | 1 | |
| Item6: Unvaccinated people | 0 | 0 | N/A | |
| Item7: People who do not wear masks | 1 | 0.3 | N/A | |
| Item8: Homeless | 0 | 0 | N/A | |
| Item9: People with specific health conditions | 4 | 1.1 | 1 | |
| Targeting perceived benefits of COVID-19 vaccination | Item1: Reduce the chance of infection | 67 | 18.5 | 0.76 |
| Item2: Decrease the severity and the chance of having complications | 26 | 7.2 | 0.83 | |
| Item3: Feel protected from COVID-19 infection | 2 | 0.6 | N/A | |
| Item4: Restore a normal social life | 15 | 4.1 | 0.80 | |
| Item5: Relief from worrying | 0 | 0 | N/A | |
| Item6: Protect family, friends, and others | 36 | 9.9 | 0.79 | |
| Item7: Transmission reduction/end the pandemic | 58 | 16 | 0.91 | |
| Item8: Save medical resources | 14 | 3.9 | N/A | |
| Item9: Works for variants | 10 | 2.8 | N/A | |
| Targeting perceived barriers of COVID-19 vaccination | Item1: Efficacy | 78 | 21.5 | 0.88 |
| Item2: Safety | 112 | 30.9 | 0.74 | |
| Item3: Side effects | 19 | 5.2 | 0.74 | |
| Item4: Getting sick from COVID-19 vaccine | 1 | 0.3 | N/A | |
| Item5: Inconvenience of getting vaccinated | 2 | 0.6 | N/A | |
| Item6: Transportation to vaccination site | 1 | 0.3 | N/A | |
| Item7: Don’t have time to get vaccinated | 1 | 0.3 | N/A | |
| Item8: Conspiracy theory | 46 | 12.7 | 0.76 | |
| Item9: Cannot accept injection | 1 | 0.3 | N/A | |
| Item10: Lack of knowledge/data | 17 | 4.7 | 0.85 | |
| Item11: Rushed | 9 | 2.5 | N/A | |
| Item12: Vaccination passport/mandatory vaccine requirement | 22 | 6.1 | 0.79 | |
| Item13: Family/friends do not support/social norm | 3 | 0.8 | N/A | |
| Item14: Misinformation/ disinformation | 5 | 1.4 | N/A | |
| Item15: History of medical exploitation (Black people) | 1 | 0.3 | N/A | |
| Targeting self-efficacy | Item1: Getting vaccinated is easy | 12 | 3.3 | N/A |
| Item2: Getting vaccinated is free | 10 | 2.8 | 1 | |
| Item3: Have ability to deal with side effects | 6 | 1.7 | N/A |
| Constructs | Min | Max | M | SD |
|---|---|---|---|---|
| Severity | 0 | 3 | 0.26 | 0.69 |
| Susceptivity | 0 | 3 | 0.03 | 0.22 |
| Benefits | 0 | 4 | 0.63 | 0.93 |
| Barriers | 0 | 3 | 0.88 | 0.7 |
| Self-esteem | 0 | 2 | 0.08 | 0.3 |
| b | SE | β | Back-Transformed β | t | p | |
|---|---|---|---|---|---|---|
| Intercept | 7.73 | 0.11 | 70.16 | <0.01 ** | ||
| Severity | 0.11 | 0.08 | 0.08 | 1.08 | 1.42 | 0.16 |
| Benefits | −0.04 | 0.06 | −0.04 | 0.96 | −0.64 | 0.52 |
| Barriers | 0.005 | 0.08 | 0.004 | 1.00 | 0.06 | 0.95 |
| Susceptibility | −0.81 | 0.31 | −0.14 | 0.87 | −2.59 | 0.01 * |
| Self-efficacy | −0.50 | 0.20 | −0.13 | 0.88 | −2.48 | 0.014 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jia, X.; Ahn, S.; Seelig, M.I.; Morgan, S.E. The Role of Health Belief Model Constructs and Content Creator Characteristics in Social Media Engagement: Insights from COVID-19 Vaccine Tweets. Healthcare 2024, 12, 1845. https://doi.org/10.3390/healthcare12181845
Jia X, Ahn S, Seelig MI, Morgan SE. The Role of Health Belief Model Constructs and Content Creator Characteristics in Social Media Engagement: Insights from COVID-19 Vaccine Tweets. Healthcare. 2024; 12(18):1845. https://doi.org/10.3390/healthcare12181845
Chicago/Turabian StyleJia, Xiaofeng, Soyeon Ahn, Michelle I. Seelig, and Susan E. Morgan. 2024. "The Role of Health Belief Model Constructs and Content Creator Characteristics in Social Media Engagement: Insights from COVID-19 Vaccine Tweets" Healthcare 12, no. 18: 1845. https://doi.org/10.3390/healthcare12181845






