Abstract
Background: Health workers (HWs) faced considerable psychosocial hazards during the COVID-19 pandemic, which profoundly affected their occupational health and job performance. The potential indirect relationship between workplace violence (WPV) and burnout among HWs needs to be further explored. The purpose of this study is to examine the chain mediating effects of sleep disturbance and work ability in the relationship between WPV and burnout among HWs. Methods: A cross-sectional study was conducted in a secondary hospital two years after the COVID-19 outbreak in Wuhan, China. A sample of 571 HWs was recruited using a cluster sampling method, achieving a response rate of 80.06%. Participants completed self-report questionnaires that included demographic information and measures of WPV, burnout, sleep disturbance, and work ability. Results: The prevalence rates of burnout and WPV among HWs two years after the COVID-19 outbreak were 37.30% and 31.52%, respectively. WPV was significantly associated with burnout (β = 0.446, p < 0.001). Sleep disturbance was identified as a mediator in the relationship between WPV and burnout (β = 0.063, 95% CI: 0.027–0.105), accounting for 14.13% of the total effect. Similarly, work ability also played a mediating role in this relationship (β = 0.142, 95% CI: 0.065–0.225), accounting for 31.84%. Additionally, both sleep disturbance and work ability exhibited a chain mediation effect on the association between WPV and burnout (β = 0.020, 95% CI: 0.008–0.036), and the total indirect effect accounted for 50.67%. Conclusions: Among Chinese HWs, WPV exerts significant direct and indirect effects on burnout symptoms, mediated by sleep disturbance and work ability. This finding provides valuable empirical insights for designing interventions to mitigate the adverse effects of psychosocial factors such as WPV and burnout among HWs. After exposure to WPV, measures focused on reducing sleep disturbance and enhancing work ability may prove effective in alleviating burnout in subsequent interventions.
1. Introduction
Ensuring occupational safety and health (OSH) in the workplace is foundational for advancing the “Decent work for all” policy advocated by the Sustainable Development Goals (SDGs) of the United Nations [1]. Health workers (HWs) are particularly susceptible to significant psychosocial hazards in healthcare settings, including burnout, work-related stress, sleep disturbances, and various forms of workplace violence (WPV). Particularly during the COVID-19 pandemic, HWs were at an increased risk of experiencing psychological consequences compared to the general population, which profoundly impacted their well-being and work performance [2]. To mitigate the potential consequences of psychosocial factors, proactive measures are increasingly implemented across numerous workplaces. Endorsed by the SOLVE (Integrating Health Promotion into Workplace OSH Policies) training program [3], a tool of the International Labour Organization (ILO) designed to address workplace psychosocial hazards and risks, health promotion programs at the workplace can be developed to enable workers to cope with psychosocial factors more effectively, such as stress, violence, or unhealthy sleep. Additionally, integrating health promotion into OSH policies not only enhances occupational health practice but also fosters a culture of prevention. Thus, it plays a pivotal role in elucidating the interplay between these psychosocial hazards.
Burnout is a psychological syndrome characterized by job-related stress in various healthcare practice environments [4]. It comprises the following three dimensions: emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment [5]. The COVID-19 pandemic introduced a multitude of psychological stressors, leading to numerous reports of unprecedented levels of burnout [6]. Additionally, the prevalence of burnout was rampant, reaching global levels in occupational settings, especially among professional HWs [7,8,9]. Studies have demonstrated that the prevalence of burnout among physicians was 82.1% in mainland China [10], 38.2% in the United States [11], and 2.5% to 87.9% in low- and middle-income countries as reported from a meta-analysis across 43 studies [12]. Recently, burnout has been classified as an occupational phenomenon rather than a medical condition in the 11th Revision of the International Classification of Diseases (ICD-11) by the World Health Organization (WHO) [13]. It exerts adverse effects on HWs and the healthcare system, manifesting in poor physical and mental health, impaired work–life balance, and reduced quality of patient care [7,14,15]. Additionally, burnout can escalate both direct and indirect medical costs [15,16].
WPV is conceptualized by the ILO as “a range of unacceptable behaviors and practices, or threats thereof, whether a single occurrence or repeated, that aims at, result in, or are likely to result in physical, psychological, sexual or economic harm, and includes gender-based violence and harassment” [17]. Characterized by its nature of intolerable and resulting harm, WPV is prevalent across diverse work environments and occupational groups. On a global scale, the COVID-19 pandemic has been associated with exacerbated incidences of WPV against HWs, even considering the variability of the data [18,19]. Hadavi demonstrated that the overall prevalence of WPV among HWs during the COVID-19 pandemic was 45.80% [20], with psychiatric nurses being the most affected professionals [21]. Zhang et al. reported HWs employed during the COVID-19 pandemic faced a higher risk of both physical and psychological WPV [22]. According to another study focusing on the gender disparity among HWs, it showed that the prevalence of WPV tended to be higher toward men in Asia, while it was higher toward women in Latin America during the COVID-19 pandemic [23]. WPV poses a serious threat to the safety and well-being of HWs in multiple dimensions, leading to diminished job satisfaction, increased occupational burnout, and severe psychological issues, including post-traumatic stress disorder and suicidal ideation [24,25]. Data also show the possible consequences in physicians’ burnout and the deterioration of quality of life, which are linked to physical and mental health problems, which, in a domino effect, fall on patients’ quality of care [26,27]. Additionally, it presents a significant obstacle to achieving the objective of the “Decent work for all” policy of the SDGs [1].
Recent research has consistently shown a correlation between exposure to WPV and heightened levels of burnout. Notably, a substantial proportion of the participants across these studies were HWs [28,29,30]. Some other studies have reported the indirect relationship with WPV predicting burnout, showing that there may be different mediators between them, such as work ability, a sense of coherence, and depression [31,32,33], while research during the COVID-19 pandemic remains limited. Therefore, to contribute insights to the development of integrated health promotion policies for OSH, further investigation into potential mediating factors between WPV and burnout during and after the COVID-19 pandemic is needed.
Sleep disturbance, as an occupational hazard, is prevalent in almost four out of ten HWs [34]. Strong evidence indicates that insufficient sleep is associated with substantial health and cognitive performance consequences [35,36]. At the same time, work ability also served as a comprehensive concept for occupational health and prevention. For example, Shechter et al. conducted a cross-sectional study and highlighted that poor sleep and insomnia symptoms were significantly associated with the emotional exhaustion aspect of burnout [37]. Converso et al. have explored whether work ability affects the burnout of HWs [38,39]. Additionally, previous research has demonstrated that exposure to WPV can increase the risk of sleep disturbance and diminished work ability [40,41,42]. However, there have been limited investigations on the interplay and relationship between WPV, sleep disturbance, work ability, and burnout [43,44].
Given the constraints of the previous studies, including the potential indirect relationship between WPV and burnout during and after the COVID-19 pandemic, as well as the limited investigations into the interplay between WPV, sleep disturbance, work ability, and burnout, this study aims to investigate the relationship between WPV, sleep disturbance, work ability, and burnout among HWs two years after the COVID-19 outbreak. The findings will address pressing implications for health promotion and psychosocial risk factors for occupational safety and health (OSH). The study will also address the urgent implications for health promotion related to psychosocial risk factors for OSH. To address this objective, we formulated the following hypotheses: Firstly, there exists an association between WPV and burnout among HWs in China. Secondly, sleep disturbance and work ability mediate the relationship between WPV and burnout, respectively. Lastly, sleep disturbance and work ability exhibit a chain mediation effect between WPV and burnout.
2. Materials and Methods
2.1. Study Design and Participants
This cross-sectional study was conducted at a secondary general hospital (hereafter referred to as “the sample hospital”) between June and July 2022 in Wuhan, Hubei Province, China. This hospital is located merely a mile away from the Wuhan Huanan Seafood Wholesale Market, and it was among the first hospitals designated for COVID-19 infections in Wuhan between 21 January and 6 March 2020. It has 477 open beds and 27 clinical specialties, including intensive care units, the most famous of which are the Sleep Medicine Center, Thyroid and Breast Surgery, Endocrinology, Pain Medicine, Neurology, and Obstetrics. In 2021 and 2022, the ILO-Peking Union Medical College (ILO-PUMC) team conducted both online and in-person Work Improvement in Health Services (HealthWISE) training workshops at this hospital. The workshop consisted of the following four sessions: thematic reports on national and international OSH, good practices from HealthWISE pilot hospitals, instruction on HealthWISE modules, and walk-through interventions in this hospital. A total of 23 department heads and hospital leaders from this hospital participated in the training workshop and demonstrated significant improvements in knowledge awareness, beliefs and attitudes, and capacity building after the training. The effectiveness of this workshop highlighted its crucial role in assisting this hospital in establishing a fundamental framework for OSH management systems specifically tailored to HWs.
Among hospitals nationwide, we considered the sample hospital as a cluster and included all of its HWs who met our criteria as participants. A sample of 574 HWs was recruited through the cluster sampling method between June and July 2022, achieving a response rate of 80.06%. The sample covered all departments within the hospital. Inclusion criteria included the following: (a) certification as a healthcare professional; (b) voluntary participation with informed consent; (c) employment at the hospital as a regular employee for over one year. Exclusion criteria included the following: (a) absence from duty for over one month during the investigation period; (b) failure to complete the questionnaire in the opening hours.
An online version of the questionnaire was distributed to entire staff of the hospital through Wenjuanxing, a widely used web-based survey platform in China. A total of 574 questionnaires were collected, with 3 excluded due to logical errors (such as an age less than 5 years old or inconsistencies between work years, title, and salary) or missing key values (such as WPV, burnout, WAI, or sleep), resulting in a final sample of 571 questionnaires.
2.2. Ethics Statement
This study was conducted after approval from the Chinese Academy of Medical Sciences & Peking Union Medical College Ethics Committee (Registration number CAMS&PUMC-IEC-2022-044) in 2022. Participation was voluntary and informed consent was presented on the first page of the questionnaire. All participants were provided with detailed explanations regarding the attributes, benefits, uses, and potential adverse effects of the study. All data were anonymized to ensure the privacy and confidentiality of the participants. Additionally, participants were assured that their data would be used solely for research purposes.
2.3. Measurement of Burnout
Burnout was assessed using the Chinese version of 2 single-item measures adapted from the full Maslach Burnout Inventory (MBI) [5]: (1) “I felt burned out from my work”; (2) “I have become more callous toward people since I took this job”. As assessed by the full MBI, these 2 items are strongly associated with the emotional exhaustion and depersonalization domains of burnout, with the area under the receiver operating characteristic curve of 0.94 for the single item of emotional exhaustion and 0.93 for the single item of depersonalization [45,46]. The 2-item scale has been widely adopted by numerous scholars in previous research to assess burnout among HWs [11,47]. We used a 7-point Likert scale ranging from 0 (never) to 6 (every day). The total score ranged from 0 to 12, with higher scores indicating more severe levels of burnout. Individuals with a high score (frequency≥ once per week/score ≥ 4) on either of these two items were identified as having burnout symptoms [45,46].
2.4. Measurement of WPV
The Chinese version of Workplace Violence in the Health Sector Country Case Studies Research Instruments Survey Questionnaire [48] was used to assess WPV among HWs. Developed by the ILO and the WHO, this questionnaire was translated into Chinese by Liu et al. [49,50]. This scale is widely utilized in China and has previously been employed to evaluate WPV among Chinese HWs [51,52,53,54]. The Cronbach’s α coefficient for this scale was 0.83 [49]. It categorizes WPV into several types, including physical violence and psychological violence, which encompass verbal abuse, bullying/mobbing, racial harassment, and sexual harassment. The complete questionnaire was detailed in our prior research [49,55]. In this study, WPV was evaluated based on the frequency of incidents reported by HWs in the year before the investigation day. Response options included the following: 0 (never), 1 (1 time), 2 (2–4 times), 3 (5–10 times), 4 (several times per month), and 5 (almost every day). The total score ranged from 0 to 25, with higher scores indicating more severe levels of WPV experienced by HWs. Individuals scoring equal to or higher than 1 (frequency ≥1 time) on any type of WPV were classified as having experienced WPV.
2.5. Measurement of Work Ability
The work ability of HWs was measured using the Chinese version of the Work Ability Index (WAI), which was translated by Zhang et al. in 2003 [56,57]. The WAI serves as a universal instrument for evaluating self-assessed work ability concerning job demands, health status, and personal resources [58]. It has been widely validated [59,60] and extensively utilized [38,61]. In the present study, Cronbach’s α coefficient was 0.78. It comprised the following 7 sections: (1) current work ability compared with lifetime best (score range: 1–10), (2) work ability in relation to mental and physical demands (score range: 2–10), (3) number of diagnosed diseases (score range: 1–7), (4) work impairment due to diseases (score range: 1–6), (5) sick leave over the past 12 months (score range: 1–5), (6) self-prognosis of work ability in the next 2 years (score range: 1–4 or 7), and (7) mental resources (score range: 1–4). The total score ranged from 7 to 49 and was categorized into the following four levels: excellent (44–49), good (37–43), moderate (28–36), and poor (7–27).
2.6. Measurement of Sleep Disturbance
Sleep disturbance was assessed through self-reported responses on the following three questions, with options for “yes” or “no” answers: (1) “Did you experience difficulties falling asleep at night?” (2) “Did you frequently awaken in the early hours, unable to return to sleep?” (3) “Did you consume sleeping pills more than three times per week?” These questions have been widely used in epidemiological studies to evaluate sleep disturbance in adults [62,63,64]. In this study, the cumulative number of affirmative responses (ranging from 0 to 3) was considered as the mediating variable.
2.7. Statistical Analyses
All data analysis and processing were conducted using the BruceR packages (https://psychbruce.github.io/bruceR/, accessed on 10 March 2024) in R software version 4.3.2 (R Development Core Team, Vienna, Austria). Firstly, descriptive analysis, the independent-samples t-test, and one-way analysis of variance were used to describe and compare the demographic characteristics of the study population. Secondly, Spearman’s correlation analysis was used to investigate the relationships between burnout, WPV, sleep disturbance, and work ability. Finally, to assess the potential chain mediation effects, we utilized a bootstrap method using bias-corrected 95% confidence intervals (BC 95% CIs). It was estimated through the Serial-Multiple Mediation Model 6 of PROCESS macro version 3.5 in R, developed by Hayes [65]. Hayes argued that bootstrapping is the most powerful method to assess indirect effects because it does not rely on assumptions regarding the sampling distribution of the indirect effect and offers better control over type I errors [66]. The indirect effect and BC 95% CIs were based on 10,000 bootstrapping samples. If the BC 95% CIs did not contain zero, the mediating effect was considered significant. Gender, age, department, occupation, years of working, number of employees coworking, shift work, night work, and direct contact with patients were treated as covariates. Harman’s univariate test, conducted using SPSS 25, assessed the severity of the common method bias [67].
3. Results
3.1. Participant Characteristics and Prevalence of WPV and Burnout
The results of Harman’s univariate test revealed five factors with a characteristic root >1. Among these, the first factor accounted for 24.71% of the variance, which is below the critical standard of 40.00%. Consequently, the findings suggest that there is no significant common method bias in this study.
Table 1 presents a summary of the demographic characteristics of the participants and the difference in burnout scores between groups. A total of 571 valid questionnaires were collected in our study. Participant ages ranged from 19 to 69 years old, with a mean of 37.11 ± 8.53 years old (mean ± SD). Female HWs comprised 78.46% of the sample. Table 1 illustrates the significant differences in the burnout scores among HWs in age, occupation, number of employees coworking, shift work, night work, and direct contact with patients. Considering the results of our previous studies and the differences in burnout shown in Table 1, we considered the above variables as confounders and adjusted them in the chain mediation analysis.

Table 1.
The characteristics of participants and distribution of the burnout score (N = 571).
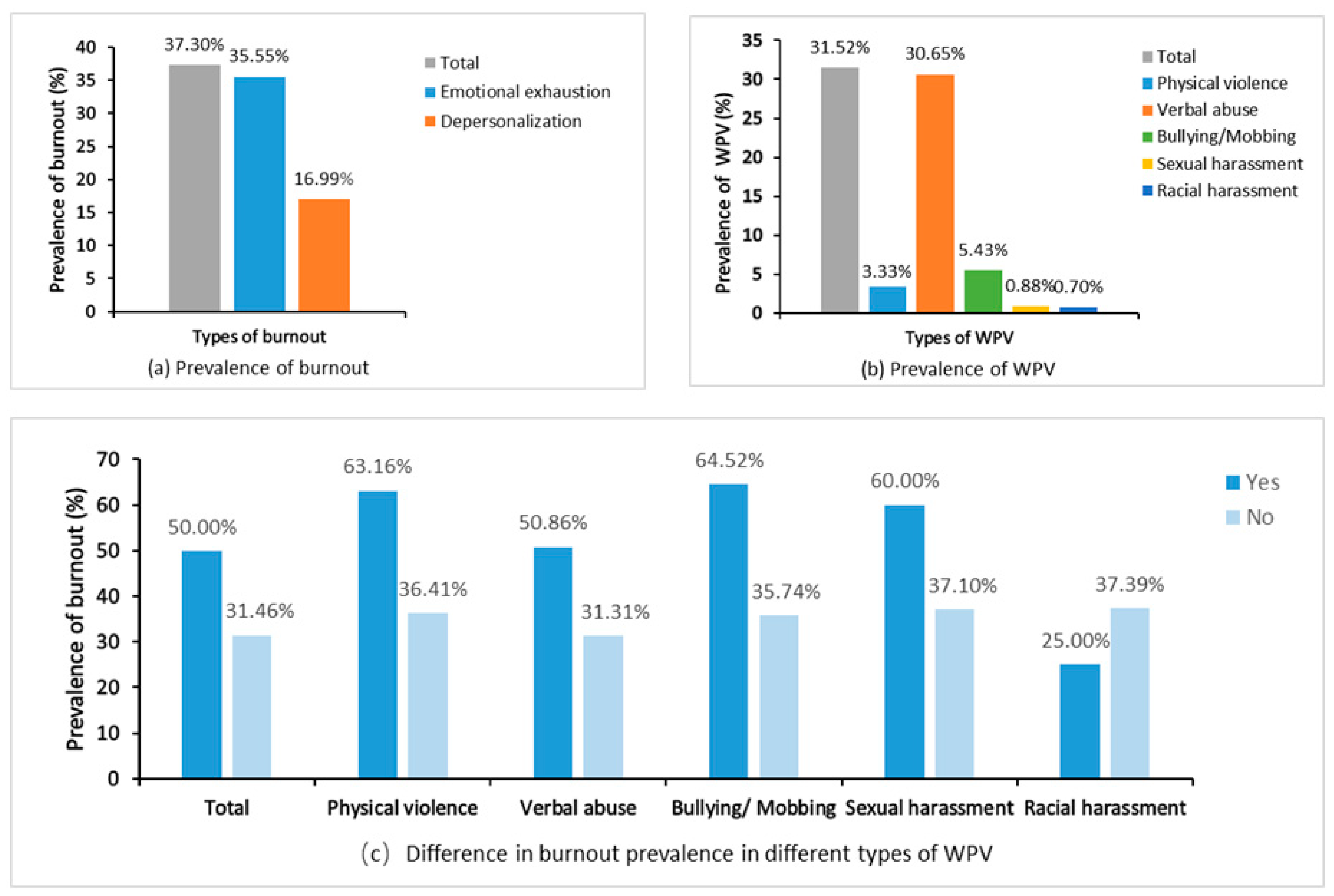
Among all 571 participants, the mean scores of burnout and WPV were 5.07 ± 3.13 and 0.87 ± 1.66, respectively. Two years after the COVID-19 outbreak, a total of 180 (31.52%) and 213 (37.30%) HWs fulfilled the criteria for WPV and burnout, respectively (Figure 1a,b). When comparing participants with and without an experience of WPV two years after the COVID-19 pandemic, those meeting the criteria for any type of WPV, except racial harassment, reported a higher prevalence of burnout (Figure 1c).
Figure 1.
Prevalence of burnout and WPV among HWs two years after the COVID-19 outbreak. Note: WPV, workplace violence.
3.2. Correlation Analysis
Table 2 reveals that burnout exhibited a positive correlation with WPV (r = 0.256, p < 0.001) and sleep disturbance (r = 0.322, p < 0.001), while demonstrating a negative correlation with work ability (r = −0.454, p < 0.001). The p values associated with these correlations were statistically significant. The correlation coefficient indicated effect sizes exceeding 0.2 between the variables.

Table 2.
Means, standard deviations, and Spearman correlations between WPV, sleep disturbance, work ability, and burnout (N = 571).
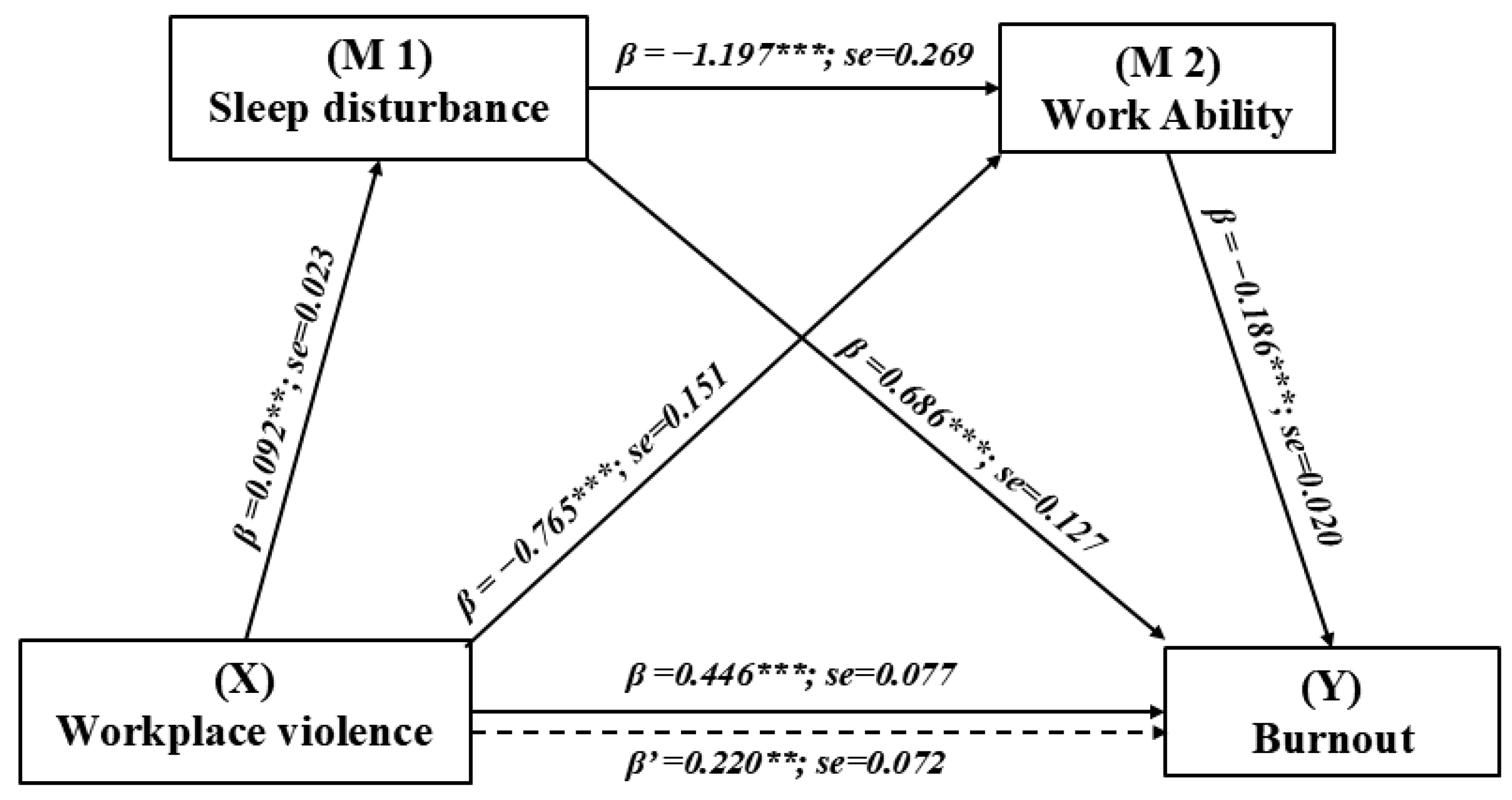
3.3. The Chain Mediating Effect of WPV on Burnout
The indirect and specific effects of WPV on burnout, mediated through sleep disturbance and work ability, is shown in Table 3. Figure 2 shows the chain mediation model. After adjusting for covariates, the total effect of WPV on burnout was found to be significant (c = 0.446, SE = 0.077, p < 0.001). When accounting for all variables (including covariates) in the model, the pathways through the single mediation of sleep disturbance (β = 0.063; bias-corrected (BC) 95% CIs: 0.027, 0.105), single mediation of work ability (β = 0.142; BC 95% CIs: 0.065, 0.225), and both mediators (β = 0.020; BC 95% CIs: 0.008, 0.036) were all statistically significant. These pathways accounted for 14.13%, 31.84%, and 4.48% of the total effect, respectively. The overall indirect effect, as measured through the mediation of sleep disturbance and work ability, was found to be statistically significant (β = 0.226; BC 95% CIs: 0.133, 0.321). This indirect effect accounted for 50.67% of the total effect size, indicating that the pathway through both mediators plays a significant role in the relationship between WPV and burnout. Additionally, the indirect effect through both sleep disturbance alone and work ability alone was also significant.

Table 3.
Comparison of indirect effects of WPV on burnout mediated by sleep disturbance and work ability.
Figure 2.
Chain mediation effect of sleep disturbance and work ability in the relationship between WPV and burnout with non-standardized beta values and standard error. X is the predictor, M1 and M2 are mediators, and Y is the outcome variable. ** p < 0.01; *** p < 0.001.
This study analyzed divergent outcomes to determine if specific indirect effects mediated by certain factors were stronger than others. As indicated in Table 3, all three contrasts demonstrated statistically significant results, with the BC 95% CIs excluding the zero-point estimate. According to the comparison of these specific direct effects, we observed that both pathways mediated solely by sleep disturbance and solely by work ability exhibited stronger mediating effects compared to the pathway mediated through a chain of sleep disturbance and work ability.
4. Discussion
To the best of our knowledge, this investigation represents the first to examine the chain mediation relationships involving sleep disturbance and work ability in the association between WPV and burnout among HWs in China. Overall, we revealed the prevalence of burnout and WPV among HWs two years after the COVID-19 outbreak, which were 37.30% and 31.52%, respectively. Consistent with our hypotheses, the result demonstrates a positive association between WPV and burnout in HWs. Moreover, regarding the hypothesis of the mediating relationship, the positive predictive effect of WPV on burnout is mitigated by the buffering influence of sleep disturbance and work ability. Therefore, our research findings validate all of the hypotheses posited.
4.1. Prevalence of Burnout and WPV Two Years after the COVID-19 Outbreak
This study revealed a notable prevalence rate of WPV (31.52%) and overall burnout (37.30%) among HWs two years after the COVID-19 outbreak, as shown in emotional exhaustion (35.55%) and depersonalization (16.99%). A meta-analysis encompassing 239 studies showed that the burnout prevalence rate among HWs exposed to COVID-19 was 37% [68], slightly lower than the 37.30% of our study. However, a similar cross-sectional study conducted in six Wuhan hospitals two years after the pandemic revealed a comparatively higher burnout rate (67.09%) than that identified in our study [69], which may reflect the differences in the impact of outbreaks in different regions. Compared to the beginning of the epidemic, this study shows that the prevalence of burnout is still higher, suggesting that the impact of the epidemic on HWs’ mental health is long-term. This is also supported by the study by Hu et al. [70] and the systematic review by Macaron et al. [71], where the prevalence of burnout remained significant even in the later stages of the epidemic. A systematic review by Macaron et al. showed the prevalence of burnout among physicians during the early pandemic period was 60.7% compared to 49.3% during the late pandemic period [71]. The COVID-19 pandemic has led to persistently high levels of burnout and WPV among healthcare professionals [70].
Our survey revealed similar results in terms of the prevalence of WPV. A comprehensive meta-analysis has reported that the global prevalence of any form of WPV during the COVID-19 epidemic was 43% among HWs. This figure is notably higher than the 31.52% prevalence rate observed in our study. This variance could potentially be attributed to the conduction of the HealthWISE training at the sample hospital by the ILO-PUMC team in both 2020 and 2021, which highlights the importance of targeted training and interventions in reducing WPV. Before conducting this survey, the sample hospital had received certain occupational health interventions and guidance on burnout and WPV, potentially contributing to the maintenance of a moderate level of burnout. Although the prevalence of WPV in the sample hospitals was lower than the global average, more than one-third of HWs reported experiencing WPV, indicating that there is still significant potential to further reducing WPV and burnout levels. Consequently, hospital management needs to continue to pay attention and take measures to improve the working environment.
4.2. The Direct Effect of WPV on Burnout
The results of our study indicate a significantly positive correlation between WPV and burnout among Chinese HWs (r = 0.256, p < 0.001), which is in agreement with previous research [28,43]. Additionally, a survey conducted after a year of the COVID-19 pandemic revealed that exposure to WPV at “intermediate and high” levels is associated with a markedly higher risk of burnout among Bangladeshi nurses (RR = 3.65, 95% CI: 2.40–5.56) [72]. Some studies suggest that WPV may serve as a predictor of burnout, albeit indirectly. While experiencing verbal or physical violence in the workplace may not directly cause burnout, it can contribute through other factors, such as work ability, emotional reaction, and sense of coherence [31,32,38], ultimately resulting in significant burnout levels. This indirect pathway implies that interventions should target not only reducing WPV but also enhancing protective factors that mitigate the impact of WPV on mental health. The comparison of these studies calls for further research to explore the specific mechanisms through which WPV contributes to burnout and to evaluate the effectiveness of various intervention strategies.
As advocated by the SOLVE training program of the ILO, health promotion and prevention measures targeting psychosocial factors should be integrated into the risk management framework of a comprehensive OSH management system [3]. To mitigate the adverse effects of psychosocial factors such as WPV and burnout, the assessment and control of these factors should be regarded as essential practices. Therefore, identifying the intertwined correlation between WPV and burnout, including their direct and indirect pathways to other psychosocial factors, is crucial for effectively preventing adverse outcomes. Furthermore, it emphasizes the importance of translating research findings into practical actions that can be implemented in healthcare settings to protect the mental health of HWs.
4.3. The Mediation Effect of Sleep Disturbance and Work Ability
A novel finding in this study is the mediating effect of sleep disturbance between WPV and burnout. This result indicates that HWs who experience WPV are at an increased risk for sleep disturbance, subsequently leading to an increased level of burnout within their professional environment. Previous studies have consistently shown that sleep-related impairment was associated with various psychosocial outcomes [73], including increased burnout [37]. Sleep is an important process for physical and psychological recovery, and sleep deprivation can interfere with the restoration of physical and mental energy and resources [74]. In fact, insomnia or sleep disturbance often persists throughout a health worker’s entire career, especially during an international public health emergency such as the COVID-19 pandemic. A study conducted among the general population, HWs, and quarantined individuals during the COVID-19 pandemic reveals that the prevalence of sleep disturbances was the highest among HWs, at 29.8% [75]. Therefore, when HWs are exposed to violence, whether at the physical or psychological level, the consequences may initially manifest in their daily lives, such as shortened sleep duration and poor sleep quality, and subsequently lead to emotional exhaustion or depersonalization at work. From a preventive perspective, sleep interventions for HWs exposed to WPV should be implemented as follows: (1) disseminate information and guidance on issues related to healthy sleep; (2) ensure that shift and night work scheduling is fair, reasonable, and gender-sensitive; (3) provide targeted training on sleep and rest management for HWs engaged in night or shift work; (4) offer adequate support, counseling, and psychotherapy, as appropriate [3].
In addition, the results indicated that HWs who experienced WPV were more likely to experience declined work ability, subsequently causing an elevated level of burnout. Limited studies have explored the relationship between exposure to violence, work ability, and burnout. Our finding aligns with Converso’s research [38], which reported a similar mediating effect of work ability between WPV and burnout among nursing staff [76]. However, other studies have shown that work ability declines as burnout levels rise [77,78], which contrasts with the findings of this study. One possible explanation could be that work ability and burnout interact with each other and are mutually causal. People with strong work ability may be more capable of recovering from burnout, thereby mitigates its effects, while people with weaker work ability may find it more challenging to recover from burnout, which reflects the difference in resilience. Therefore, both of the above pathways between burnout and work ability could be reasonable [79]. In addition, workforce aging affects work ability differently. Hatch et al. [78] indicated that increased age correlates with declines in physical work ability. In contrast, they found that psychological work ability decreases with age only at higher burnout levels, while, at lower levels, it improves. Sottimano’s research underscores work ability as a mediator in the relationship between aging and emotional exhaustion [76]. Working ability is closely linked to overall health, and for HWs exposed to WPV, the recovery of work ability depends on a combination of professional knowledge as well as organizational, ergonomic, and psychosocial conditions in the workplace [80]. For hospitals and managers, it is crucial to promote HWs’ work ability through the following measures: (1) streamlining work tasks to be more autonomous; (2) improving work postures, work tools, and the workplace temperature according to work demands and environment; (3) optimizing work community, role clarity, and work experience in work organization; (4) expanding more possibilities for development and training for professional competence; (5) encouraging weight control, physical activities, and engagement in hobbies to support health and functional capacity [81,82].
4.4. The Chain Mediation Effect
To the best of our knowledge, the current study contributes to evaluating the chain mediating effect of sleep disturbance and work ability between WPV and burnout among HWs, a relationship that has not been explored previously. The findings of this study demonstrate that exposure to WPV is sequentially associated with an increased level of sleep disturbance initially, followed by decreased work ability, which subsequently exacerbates burnout. According to the SOLVE program of the ILO [3], this association suggests that integrated health promotion intervention targeting any steps may help mitigate the occurrence of adverse outcomes.
The results of the chain mediating analysis revealed that the total indirect effect of sleep disturbance and work ability accounted for 50.67% of the total effect size (B = 0.446, p < 0.001) between WPV and burnout. This percentage is comparable to that observed in other studies [31,38]. Yeping Fei et al. reported an indirect effect of 62.45% between WPV and burnout mediated by the sense of coherence [31] during the COVID-19 pandemic, surpassing 50.67% in our study. However, their investigation exclusively focused on nurses, which may not fully capture the experiences of all HWs.
Sleep disturbance and work ability are key factors in mitigating burnout. Our study provides further clarity by demonstrating that decreased sleep disturbance levels and improved work ability could be beneficial for HWs in alleviating burnout symptoms after exposure to WPV. The mediating mechanisms involving sleep disturbance and work ability provide valuable insights into addressing the occupational health challenges encountered by HWs after the COVID-19 outbreak. In clinical practice, the application of our findings calls for the implementation of comprehensive and early intervention strategies to address adverse outcomes of WPV. Firstly, in the initial phases of psychosocial events, healthcare institutions must respond promptly by implementing occupational health surveillance and workplace health promotion programs to facilitate early-stage recognition of WPV and mitigate severe burnout. Secondly, during and immediately following such events, families and healthcare institutions should provide timely support, focusing on relaxation techniques and conducive work environments to enhance the well-being of HWs, including the sleep hygiene and work ability enhancement. Lastly, long-term occupational care strategies should be instituted to foster and enhance individuals’ resilience.
In terms of health policy, our findings highlight the need for broader initiatives that address the systemic issues contributing to WPV and its downstream effects. Policymakers should consider regulations that protect HWs from WPV and provide resources for organizations to implement evidence-based interventions. Furthermore, the development of guidelines that emphasize the importance of sleep and work ability in the context of occupational health could help to standardize care and improve outcomes for HWs.
While single mediation pathways through sleep disturbance (accounting for 14.13%) and work ability (accounting for 31.84%) showed stronger effects than the chain mediation (accounting for 4.48%), this does not diminish the value of a comprehensive strategy. For hospitals with limited resources, prioritizing interventions that target sleep disturbance or work ability may be a pragmatic initial step. However, the ultimate goal should be to develop and implement a holistic program that addresses all aspects of this complex relationship.
4.5. Limitations
Some limitations still exist in our study. Firstly, the recruitment of HWs was conducted only from one secondary grade A comprehensive hospital in Wuhan, which may affect the representativeness of the data and lead to some sampling bias in this survey. Future research should aim to investigate HWs from diverse levels of hospitals by multicenter random sampling across different regions for a more comprehensive understanding. Secondly, given the cross-sectional design of this study, it is not conducive to confirming a causal relationship between WPV, sleep disturbance, work ability, and burnout. Therefore, further work should prioritize longitudinal or experimental studies to elucidate the causal relationships among these variables and explore other variables that may influence burnout. Thirdly, all variables were assessed using self-reported measures in this study. This may introduce response bias and social desirability bias.
5. Conclusions
In conclusion, this study established a chain mediating model to examine the impact of WPV on burnout among Chinese HWs two years after the COVID-19 outbreak, mediated by sleep disturbance and work ability. Specifically, this research provides valuable empirical insights for designing interventions to mitigate the adverse effects of psychosocial factors such as WPV and burnout. After exposure to WPV, intervention focused on reducing sleep disturbance and enhancing work ability among HWs may prove effective in alleviating burnout in subsequent interventions.
Author Contributions
Conceptualization, F.W., M.Z. and N.X.; data curation, F.W., M.Z., Y.H., Y.T., C.H., X.F. (Xinxin Fang), X.F. (Xi Fang), L.C. and Q.Z.; formal analysis, F.W. and M.Z.; funding acquisition, M.Z.; investigation, F.W., M.Z. and N.X.; methodology, F.W., M.Z., Y.H., Y.T., C.H., X.F. (Xinxin Fang), X.F. (Xi Fang), L.C. and Q.Z.; project administration, M.Z. and N.X.; resources, M.Z.; software, F.W., Y.H., Y.T., C.H. and X.F. (Xinxin Fang); supervision, M.Z.; validation, F.W. and M.Z.; visualization, F.W. and M.Z.; writing—original draft, F.W., M.Z. and N.X.; writing—review and editing, F.W., M.Z., N.X., Y.H., Y.T., C.H., X.F. (Xinxin Fang), X.F. (Xi Fang), L.C. and Q.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Peking Union Medical College Grant Agreement (No. 2020P053GW006).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Chinese Academy of Medical Sciences & Peking Union Medical College (protocol code CAMS&PUMC-IEC-2022-044 on 12 April 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The dataset is available on request from the corresponding author.
Acknowledgments
We would like to express our sincere gratitude to Nian Xiong and the health worker teams at Wuhan Red Cross Hospital for their invaluable support and assistance in the implementation of this survey. Moreover, we would like to express our sincere appreciation to the Department of Occupational Health of the National Health Commission and the Health Commission of Hubei Province for their support of this study. Furthermore, we extend our appreciation to all the dedicated health workers who participated in the investigation and contributed to this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- The United Nations. 17 Goals to Transform Our World. Available online: https://www.un.org/sustainabledevelopment/ (accessed on 10 March 2024).
- Rodríguez, B.O.; Sánchez, T.L. The Psychosocial Impact of COVID-19 on health care workers. Int. Braz. J. Urol. 2020, 46 (Suppl. S1), 195–200. [Google Scholar] [CrossRef] [PubMed]
- International Labour Organization. SOLVE: Integrating Health Promotion into Workplace OSH Policies—Trainer’s Guide. Available online: https://www.ilo.org/resource/training-material/solve-integrating-health-promotion-workplace-osh-policies-trainers-guide (accessed on 10 March 2024).
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Burnout among Physicians: A Systematic Review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory Manual, 3rd ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1996. [Google Scholar]
- Kabir, T.; Tan, A.Y.H.; Koh, F.H.X.; Chew, M.H. Burnout and professional fulfilment among surgeons during the COVID-19 pandemic. Br. J. Surg. 2021, 108, e3–e5. [Google Scholar] [CrossRef] [PubMed]
- Hodkinson, A.; Zhou, A.; Johnson, J.; Geraghty, K.; Riley, R.; Zhou, A.; Panagopoulou, E.; Chew-Graham, C.A.; Peters, D.; Esmail, A.; et al. Associations of physician burnout with career engagement and quality of patient care: Systematic review and meta-analysis. BMJ Clin. Res. Ed. 2022, 378, e070442. [Google Scholar] [CrossRef] [PubMed]
- Papazian, L.; Hraiech, S.; Loundou, A.; Herridge, M.S.; Boyer, L. High-level burnout in physicians and nurses working in adult ICUs: A systematic review and meta-analysis. Intensive Care Med. 2023, 49, 387–400. [Google Scholar] [CrossRef] [PubMed]
- Zhou, A.Y.; Panagioti, M.; Esmail, A.; Agius, R.; Van Tongeren, M.; Bower, P. Factors Associated with Burnout and Stress in Trainee Physicians: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e2013761. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Hu, B.; Peng, Z.; Song, H.; Cai, S.; Rao, X.; Li, L.; Li, J. Prevalence of burnout among intensivists in mainland China: A nationwide cross-sectional survey. Crit. Care 2021, 25, 8. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; West, C.P.; Sinsky, C.; Trockel, M.; Tutty, M.; Wang, H.; Carlasare, L.E.; Dyrbye, L.N. Changes in Burnout and Satisfaction with Work-Life Integration in Physicians and the General US Working Population between 2011 and 2020. Mayo Clin. Proc. 2022, 97, 491–506. [Google Scholar] [CrossRef]
- Wright, T.; Mughal, F.; Babatunde, O.O.; Dikomitis, L.; Mallen, C.D.; Helliwell, T. Burnout among primary health-care professionals in low- and middle-income countries: Systematic review and meta-analysis. Bull. World Health Organ. 2022, 100, 385–401A. [Google Scholar] [CrossRef]
- World Health Organization. Burn-out an “Occupational Phenomenon”: International Classification of Diseases. Available online: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases (accessed on 10 January 2024).
- Moss, M.; Good, V.S.; Gozal, D.; Kleinpell, R.; Sessler, C.N. A Critical Care Societies Collaborative Statement: Burnout Syndrome in Critical Care Health-care Professionals. A Call for Action. Am. J. Respir. Crit. Care Med. 2016, 194, 106–113. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician burnout: Contributors, consequences and solutions. J. Intern. Med. 2018, 283, 516–529. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Awad, K.M.; Fiscus, L.C.; Sinsky, C.A.; Shanafelt, T.D. Estimating the Attributable Cost of Physician Burnout in the United States. Ann. Intern. Med. 2019, 171, 600–601. [Google Scholar] [CrossRef]
- International Labour Organization. Violence and Harassment in the World of Work: A Guide on Convention No. 190 and Recommendation No. 206. Available online: https://www.ilo.org/global/topics/violence-harassment/resources/WCMS_814507/lang--en/index.htm (accessed on 5 March 2024).
- Devi, S. COVID-19 exacerbates violence against health workers. Lancet 2020, 396, 658. [Google Scholar] [CrossRef] [PubMed]
- Thornton, J. Violence against health workers rises during COVID-19. Lancet 2022, 400, 348. [Google Scholar] [CrossRef] [PubMed]
- Hadavi, M.; Ghomian, Z.; Mohammadi, F.; Sahebi, A. Workplace violence against health care workers during the COVID-19 Pandemic: A systematic review and meta-analysis. J. Saf. Res. 2023, 85, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Rossi, M.F.; Beccia, F.; Cittadini, F.; Amantea, C.; Aulino, G.; Santoro, P.E.; Borrelli, I.; Oliva, A.; Ricciardi, W.; Moscato, U.; et al. Workplace violence against healthcare workers: An umbrella review of systematic reviews and meta-analyses. Public. Health 2023, 221, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhao, Z.; Zhang, H.; Zhu, Y.; Xi, Z.; Xiang, K. Workplace violence against healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. Int. 2023, 30, 74838–74852. [Google Scholar] [CrossRef]
- Matta, M.G.; Gupta, S.; Alfonso, J.M.; Carrero, M.C.; Agahari, I.; Sabouret, P.; Gulati, M.; Baranchuk, A.; Garcia-Zamora, S. Prevalence and patterns of gender disparity in workplace violence among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Public. Health 2024, 235, 76–83. [Google Scholar] [CrossRef]
- Nielsen, M.B.; Nielsen, G.H.; Notelaers, G.; Einarsen, S. Workplace Bullying and Suicidal Ideation: A 3-Wave Longitudinal Norwegian Study. Am. J. Public. Health 2015, 105, e23–e28. [Google Scholar] [CrossRef]
- Ferri, P.; Silvestri, M.; Artoni, C.; Di Lorenzo, R. Workplace violence in different settings and among various health professionals in an Italian general hospital: A cross-sectional study. Psychol. Res. Behav. Manag. 2016, 9, 263–275. [Google Scholar] [CrossRef]
- Caruso, R.; Toffanin, T.; Folesani, F.; Biancosino, B.; Romagnolo, F.; Riba, M.B.; McFarland, D.; Palagini, L.; Belvederi Murri, M.; Zerbinati, L.; et al. Violence Against Physicians in the Workplace: Trends, Causes, Consequences, and Strategies for Intervention. Curr. Psychiatry Rep. 2022, 24, 911–924. [Google Scholar] [CrossRef] [PubMed]
- Tiesman, H.M.; Hendricks, S.A.; Wiegand, D.M.; Lopes-Cardozo, B.; Rao, C.Y.; Horter, L.; Rose, C.E.; Byrkit, R. Workplace Violence and the Mental Health of Public Health Workers during COVID-19. Am. J. Prev. Med. 2023, 64, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zeng, Q.; Wang, Y.; Liao, X.; Xie, C.; Wang, G.; Zeng, Y. Workplace violence and the risk of post-traumatic stress disorder and burnout among nurses: A systematic review and meta-analysis. J. Nurs. Manag. 2022, 30, 2854–2868. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Oe, M.; Ishida, T.; Matsuoka, M.; Chiba, H.; Uchimura, N. Workplace Violence and Its Effects on Burnout and Secondary Traumatic Stress among Mental Healthcare Nurses in Japan. Int. J. Environ. Res. Public. Health 2020, 17, 2747. [Google Scholar] [CrossRef]
- Gibbs, A.; Jewkes, R.; Willan, S.; Al Mamun, M.; Parvin, K.; Yu, M.; Naved, R. Workplace violence in Bangladesh’s garment industry. Soc. Sci. Med. 2019, 235, 112383. [Google Scholar] [CrossRef] [PubMed]
- Fei, Y.; Yang, S.; Zhu, Z.; Lv, M.; Yin, Y.; Zuo, M.; Chen, Y.; Sheng, H.; Zhang, S.; Zhang, M. Workplace violence and burnout among Chinese nurses during the COVID-19 pandemic: Does the sense of coherence mediate the relationship? BMC Psychiatry 2023, 23, 573. [Google Scholar] [CrossRef]
- Chang, A.K.; Kim, A.Y. Verbal violence and turnover intention among new nurses in Korea: A time-lagged survey. J. Nurs. Manag. 2022, 30, 1823–1830. [Google Scholar] [CrossRef]
- Zhao, X.; Zhang, Z.; Chen, Z.; Tian, Y.; Chen, H.; Zhou, J. Mediating role of depression between workplace violence and job burnout among healthcare workers. J. Cent. South. Univ. Med. Sci. 2023, 48, 903–908. [Google Scholar]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Cheung, V.; Yuen, V.M.; Wong, G.T.C.; Choi, S.W. The effect of sleep deprivation and disruption on DNA damage and health of doctors. Anaesthesia 2019, 74, 434–440. [Google Scholar] [CrossRef]
- Nguyen, E.; Meadley, B.; Harris, R.; Rajaratnam, S.M.W.; Williams, B.; Smith, K.; Bowles, K.-A.; Dobbie, M.L.; Drummond, S.P.A.; Wolkow, A.P. Sleep and mental health in recruit paramedics: A 6-month longitudinal study. Sleep. 2023, 46, zsad050. [Google Scholar] [CrossRef] [PubMed]
- Shechter, A.; Firew, T.; Miranda, M.; Fray, N.; Norful, A.A.; Gonzalez, A.; Chang, B.P. Sleep Disturbance and Burnout in Emergency Department Health Care Workers. JAMA Netw. Open 2023, 6, e2341910. [Google Scholar] [CrossRef] [PubMed]
- Converso, D.; Sottimano, I.; Balducci, C. Violence exposure and burnout in healthcare sector: Mediating role of work ability. Med. Lav. 2021, 112, 58–67. [Google Scholar] [PubMed]
- Pranjic, N.; Males-Bilic, L. Work ability index, absenteeism and depression among patients with burnout syndrome. Mater. Sociomed. 2014, 26, 249–252. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Jing, W.; Wei, Z.; Wang, Y.; Sun, L. Associations Between Workplace Violence and Mental Health Among Chinese Health Technicians: A Moderated Mediation Analysis of Sleep Quality and Physical Activity. Psychol. Res. Behav. Manag. 2023, 16, 2045–2057. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Di Stasio, E.; Capitanelli, I.; Lops, E.A.; Chirico, F.; Garbarino, S. Sleep Problems and Workplace Violence: A Systematic Review and Meta-Analysis. Front. Neurosci. 2019, 13, 997. [Google Scholar] [CrossRef]
- Wang, P.X.; Wang, M.Z.; Hu, G.X.; Wang, Z.M. Study on the relationship between workplace violence and work ability among health care professionals in Shangqiu City. J. Hyg. Res. 2006, 35, 472–475. [Google Scholar]
- Havaei, F.; Astivia, O.L.O.; MacPhee, M. The impact of workplace violence on medical-surgical nurses’ health outcome: A moderated mediation model of work environment conditions and burnout using secondary data. Int. J. Nurs. Stud. 2020, 109, 103666. [Google Scholar] [CrossRef]
- Chang, Y.-P.; Lee, D.-C.; Lee, Y.-H.; Chiu, M.-H. Nurses’ perceived health and occupational burnout: A focus on sleep quality, workplace violence, and organizational culture. Int. Nurs. Rev. 2024. ahead of print. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Sloan, J.A.; Shanafelt, T.D. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J. Gen. Intern. Med. 2009, 24, 1318–1321. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Satele, D.V.; Sloan, J.A.; Shanafelt, T.D. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J. Gen. Intern. Med. 2012, 27, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Shanafelt, T.D.; Kolars, J.C. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA 2011, 306, 952–960. [Google Scholar] [CrossRef] [PubMed]
- ILO; WHO; ICN; PSI. Workplace Violence in the Health Sector Country Case Studies Research Instruments: Survey Questionnaire. Available online: https://www.who.int/publications/m/item/workplace-violence-in-the-health-sector---country-case-study-research-instruments---survey-questionnaire (accessed on 15 February 2024).
- Liu, Y.; Zhang, M.; Li, R.; Chen, N.; Huang, Y.; Lv, Y.; Wang, Y. Risk assessment of workplace violence towards health workers in a Chinese hospital: A cross-sectional study. BMJ Open 2020, 10, e042800. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Zhang, M.; Li, R.; Wang, f.; Wang, Y. Investigation on workplace violence in a Grade 2A hospital—A survey using the investing tool for workplace violence in hospitals developed by the World Health Organization. Chin. Occup. Med. 2019, 46, 157–162. [Google Scholar]
- Huang, Y.; Min, Z.; Liu, Y.; Chen, N.; He, C. Workplace violence and its influencing factors among female medical workers in a hospital. Chin. J. Med. Manag. Sci. 2023, 13, 52–59. [Google Scholar]
- Chen, N.; Zhang, M.; Li, R.; Wang, Y. Investigation on workplace violence countermeasures in a Grade 2A hospital. Chin. Occup. Med. 2021, 48, 301–305. [Google Scholar]
- Huang, Y.; Zhang, M.; Li, R.; Liu, Y.; Chen, N.; Wang, Y. Status and influencing factors of psychological violence against healthcare workers in a secondary Grade A hospital. Chin. Occup. Med. 2021, 48, 306–312. [Google Scholar]
- Liu, Y.; Zhang, M.; Li, R.; Huang, Y.; Chen, N.; Liu, R.; Wang, Y. Investigation and analysis on the status quo of nurses subjected to workplace violence in a class B hospital and response modes. Chin. J. Med. Manag. Sci. 2021, 11, 59–66. [Google Scholar]
- Hu, Y.; Luo, Q.; Li, R.; Zhang, M.; Wang, Y.; Su, P.; Sun, J.; Li, Y.; Liu, Y.; Chen, N.; et al. Anti-violence measures developed by ILO and WHO: Analysis of the prevalence of workplace violence and the effects of implementation in a general hospital in China. Front. Public. Health 2022, 10, 1049832. [Google Scholar] [CrossRef]
- Tuomi, K.I.J.; Jahkola, A.; Katjarinne, L.; Tulkki, A. Work Ability Index, 2nd ed.; Finnish Institute of Occupational Health: Helsinki, Finland, 1998. [Google Scholar]
- Zhang, L.; Wang, Z.; Wang, J.; Lan, Y.; Zeng, F. Evaluation for work ability index scale. Chin. J. Ind. Med. 2003, 1, 1–5. [Google Scholar]
- Ilmarinen, J.; Tuomi, K.; Seitsamo, J. New dimensions of work ability. Int. Congr. Ser. 2005, 1280 (Suppl. S1), 3–7. [Google Scholar] [CrossRef]
- Ilmarinen, J.; Tuomi, K. Work ability of aging workers. Scand. J. Work. Environ. Health 1992, 18, 8–10. [Google Scholar] [PubMed]
- Ilmarinen, J.; Tuomi, K.; Klockars, M. Changes in the work ability of active employees over an 11-year period. Scand. J. Work. Environ. Health 1997, 23 (Suppl. S1), 49–57. [Google Scholar]
- Pacheco, E.; Bártolo, A.; Pereira, A.; Duarte, J.C.; Silva, C.F. The role of fear in the relationship between vicarious violence at work and work ability in nurses: A cross-sectional study. Nurs. Health Sci. 2022, 24, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Ingelsson, E.; Lind, L.; Arnlöv, J.; Sundström, J. Sleep disturbances independently predict heart failure in overweight middle-aged men. Eur. J. Heart Fail. 2007, 9, 184–190. [Google Scholar] [CrossRef]
- Tan, X.; Cedernaes, J.; Forsberg, L.A.; Schiöth, H.B.; Benedict, C. Self-reported sleep disturbances and prostate cancer morbidity and mortality in Swedish men: A longitudinal study over 40 years. J. Sleep. Res. 2018, 27, e12708. [Google Scholar] [CrossRef]
- Tan, X.; Cedernaes, J.; Risérus, U.; Benedict, C. Lack of association between self-reported insomnia symptoms and clamp-derived insulin sensitivity in elderly men. Psychoneuroendocrinology 2019, 102, 256–260. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Zhou, J.; Yang, Y.; Qiu, X.; Yang, X.; Pan, H.; Ban, B.; Qiao, Z.; Wang, L.; Wang, W. Serial multiple mediation of organizational commitment and job burnout in the relationship between psychological capital and anxiety in Chinese female nurses: A cross-sectional questionnaire survey. Int. J. Nurs. Stud. 2018, 83, 75–82. [Google Scholar] [CrossRef]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.-Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef]
- Aymerich, C.; Pedruzo, B.; Pérez, J.L.; Laborda, M.; Herrero, J.; Blanco, J.; Mancebo, G.; Andrés, L.; Estévez, O.; Fernandez, M.; et al. COVID-19 pandemic effects on health worker’s mental health: Systematic review and meta-analysis. Eur. Psychiatry 2022, 65, e10. [Google Scholar] [CrossRef]
- Liu, Y.; Zou, L.; Yan, S.; Zhang, P.; Zhang, J.; Wen, J.; Mao, J.; Li, L.; Wang, Y.; Fu, W. Burnout and post-traumatic stress disorder symptoms among medical staff two years after the COVID-19 pandemic in Wuhan, China: Social support and resilience as mediators. J. Affect. Disord. 2023, 321, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.; Kong, Y.; Li, W.; Han, Q.; Zhang, X.; Zhu, L.X.; Wan, S.W.; Liu, Z.; Shen, Q.; Yang, J.; et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinicalMedicine 2020, 24, 100424. [Google Scholar] [CrossRef] [PubMed]
- Macaron, M.M.; Segun-Omosehin, O.A.; Matar, R.H.; Beran, A.; Nakanishi, H.; Than, C.A.; Abulseoud, O.A. A systematic review and meta analysis on burnout in physicians during the COVID-19 pandemic: A hidden healthcare crisis. Front. Psychiatry 2022, 13, 1071397. [Google Scholar] [CrossRef]
- Chowdhury, S.R.; Kabir, H.; Chowdhury, M.R.; Hossain, A. Workplace Bullying and Violence on Burnout Among Bangladeshi Registered Nurses: A Survey Following a Year of the COVID-19 Pandemic. Int. J. Public. Health 2022, 67, 1604769. [Google Scholar] [CrossRef]
- Scott, A.J.; Webb, T.L.; Martyn-St James, M.; Rowse, G.; Weich, S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep. Med. Rev. 2021, 60, 101556. [Google Scholar] [CrossRef]
- Palagini, L.; Hertenstein, E.; Riemann, D.; Nissen, C. Sleep, insomnia and mental health. J. Sleep. Res. 2022, 31, e13628. [Google Scholar] [CrossRef]
- He, Q.; Fan, B.; Xie, B.; Liao, Y.; Han, X.; Chen, Y.; Li, L.; Iacobucci, M.; Lee, Y.; Lui, L.M.W.; et al. Mental health conditions among the general populatsssion, healthcare workers and quarantined population during the coronavirus disease 2019 (COVID-19) pandemic. Psychol Health Med. 2022, 27, 186–198. [Google Scholar] [CrossRef] [PubMed]
- Sottimano, I.; Guidetti, G.; Converso, D.; Viotti, S.; Koniaris, L.G. We cannot be “forever young,” but our children are: A multilevel intervention to sustain nursery school teachers’ resources and well-being during their long work life cycle. PLoS ONE 2018, 13, e0206627. [Google Scholar] [CrossRef]
- Lu, Y.; Liu, Q.; Yan, H.; Gao, S.; Liu, T. Job burnout and its impact on work ability in biosafety laboratory staff during the COVID-19 epidemic in Xinjiang. BMC Psychiatry 2021, 21, 543. [Google Scholar] [CrossRef]
- Hatch, D.J.; Freude, G.; Martus, P.; Rose, U.; Muller, G.; Potter, G.G. Age, burnout and physical and psychological work ability among nurses. Occup. Med. 2018, 68, 246–254. [Google Scholar] [CrossRef]
- Viotti, S.; Guidetti, G.; Sottimano, I.; Martini, M.; Converso, D. Work ability and burnout: What comes first? A two-wave, cross-lagged study among early childhood educators. Saf. Sci. 2019, 118, 898–906. [Google Scholar] [CrossRef]
- Nikolić, D.; Višnjić, A. Mobbing and Violence at Work as Hidden Stressors and Work Ability Among Emergency Medical Doctors in Serbia. Medicina 2020, 56, 31. [Google Scholar] [CrossRef] [PubMed]
- Stimpfel, A.W.; Arabadjian, M.; Liang, E.; Sheikhzadeh, A.; Weiner, S.S.; Dickson, V.V. Organization of Work Factors Associated with Work Ability among Aging Nurses. West. J. Nurs. Res. 2020, 42, 397–404. [Google Scholar] [CrossRef]
- Tuomi, K.; Huuhtanen, P.; Nykyri, E.; Ilmarinen, J. Promotion of work ability, the quality of work and retirement. Occup. Med. 2001, 51, 318–324. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).