A Comparative Study of Hospitalization Mortality Rates between General and Emergency Hospitalized Patients Using Survival Analysis
Abstract
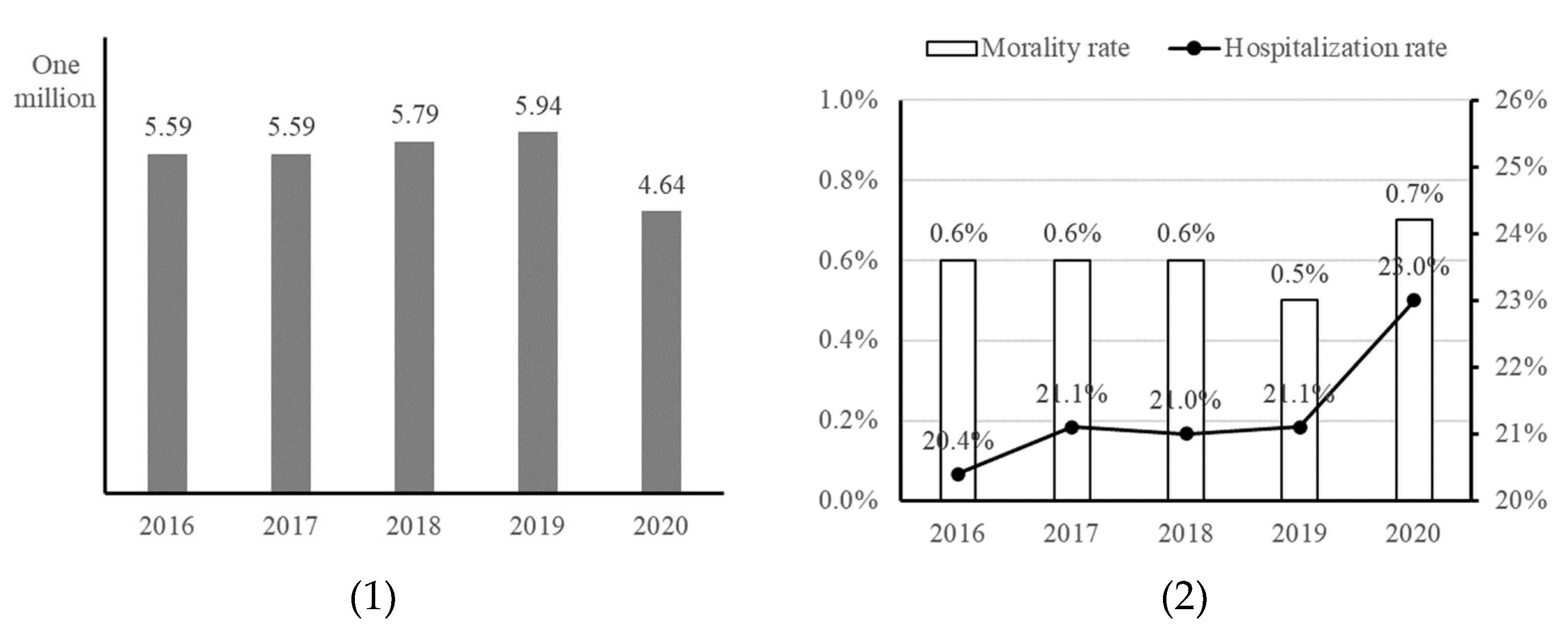
:1. Introduction
2. Theoretical Background
2.1. Emergency Medical Services (EMS)
2.2. Survival Analysis
3. Research Methodology
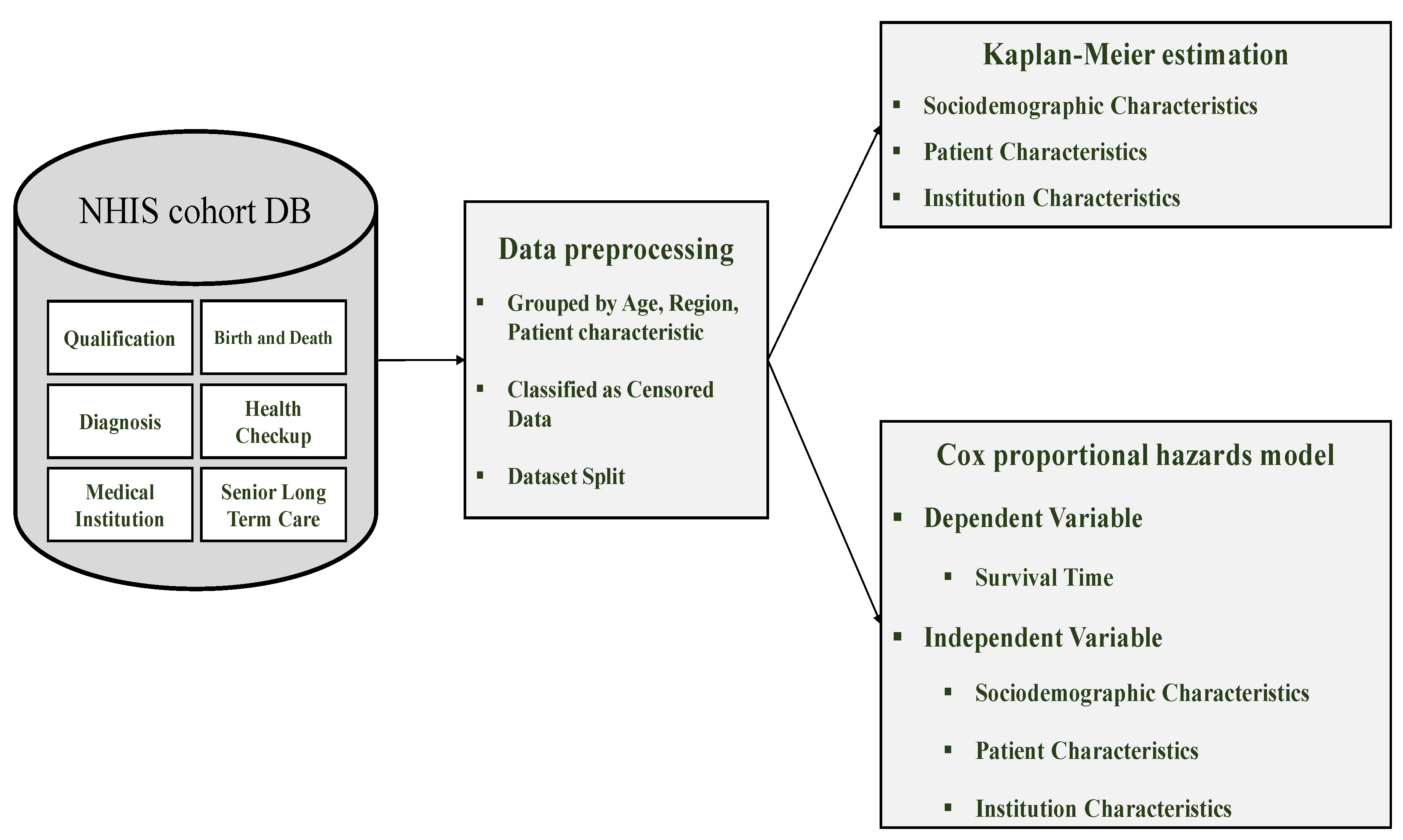
3.1. Research Framework
3.2. Data Collection
3.3. Data Preprocessing
4. Results
4.1. Determinants of Survival Time among General Inpatients
4.1.1. Characteristics of General Inpatients
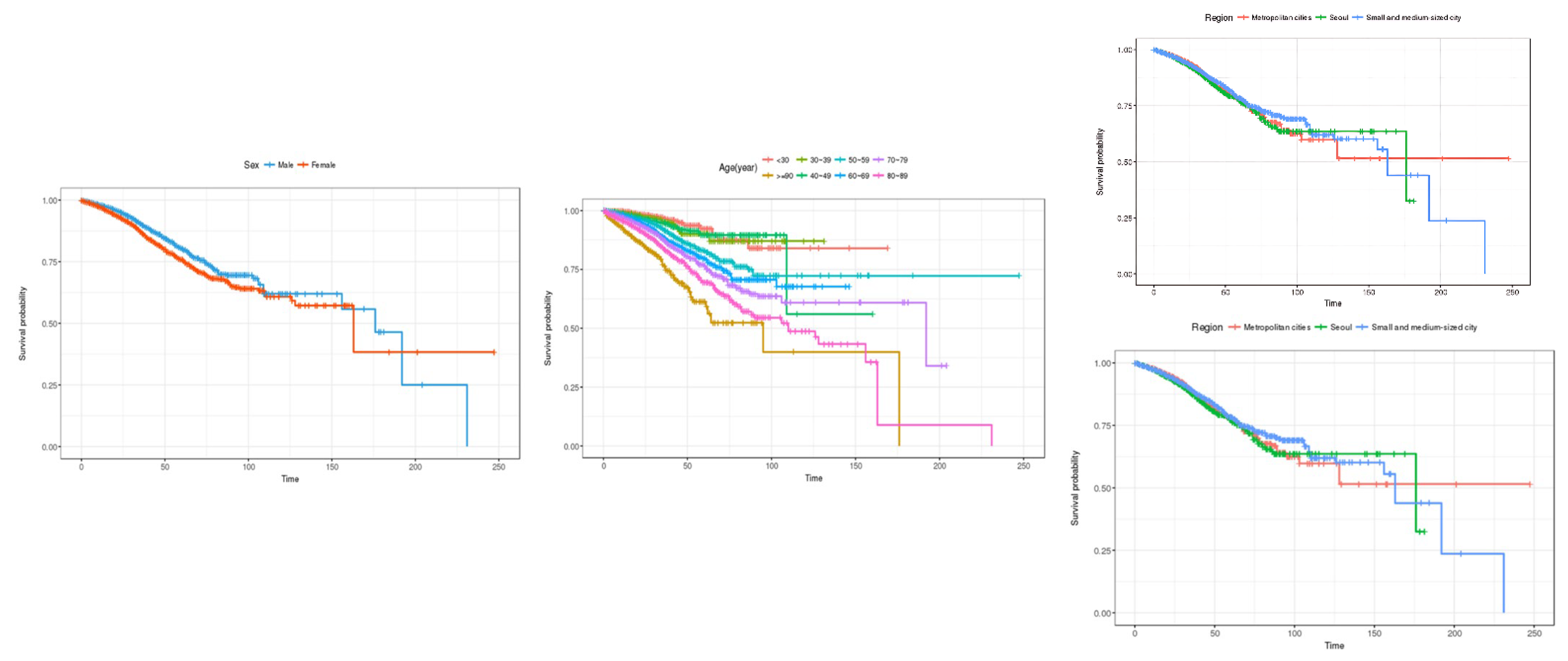
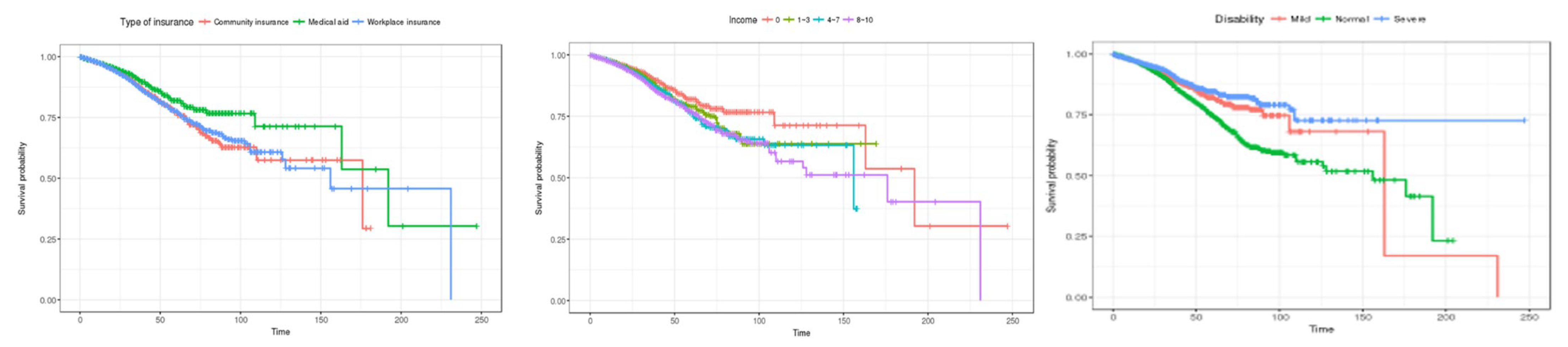
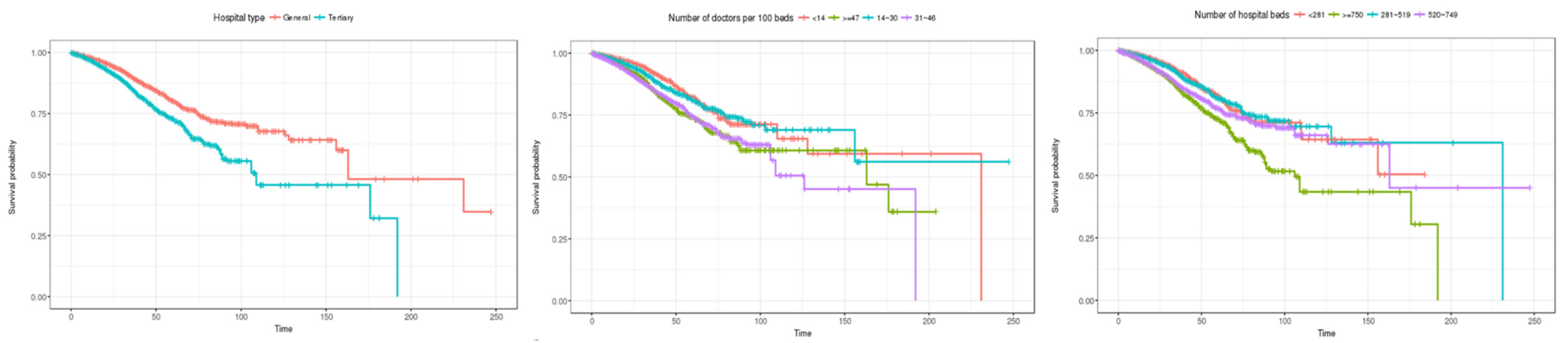
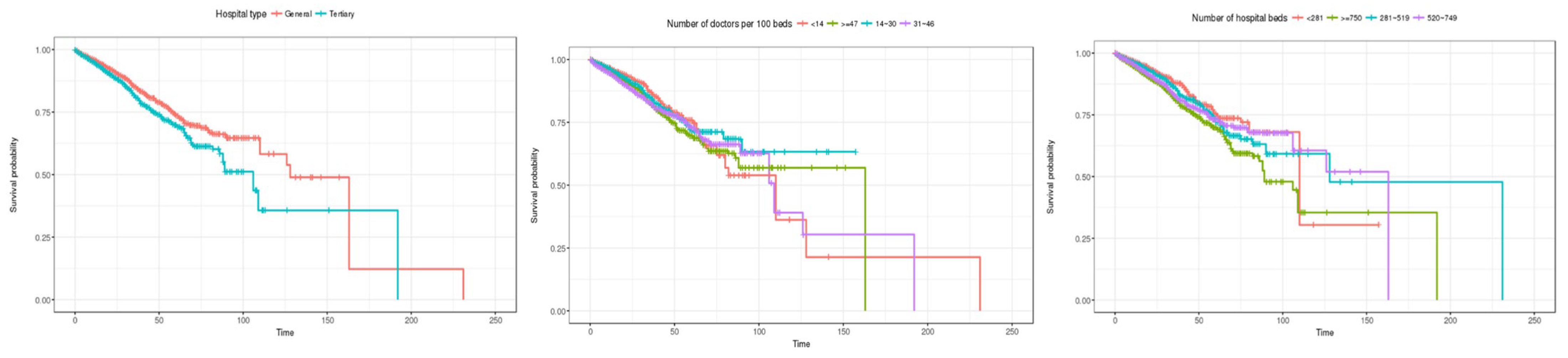
4.1.2. Kaplan–Meier Estimation (General Inpatients)
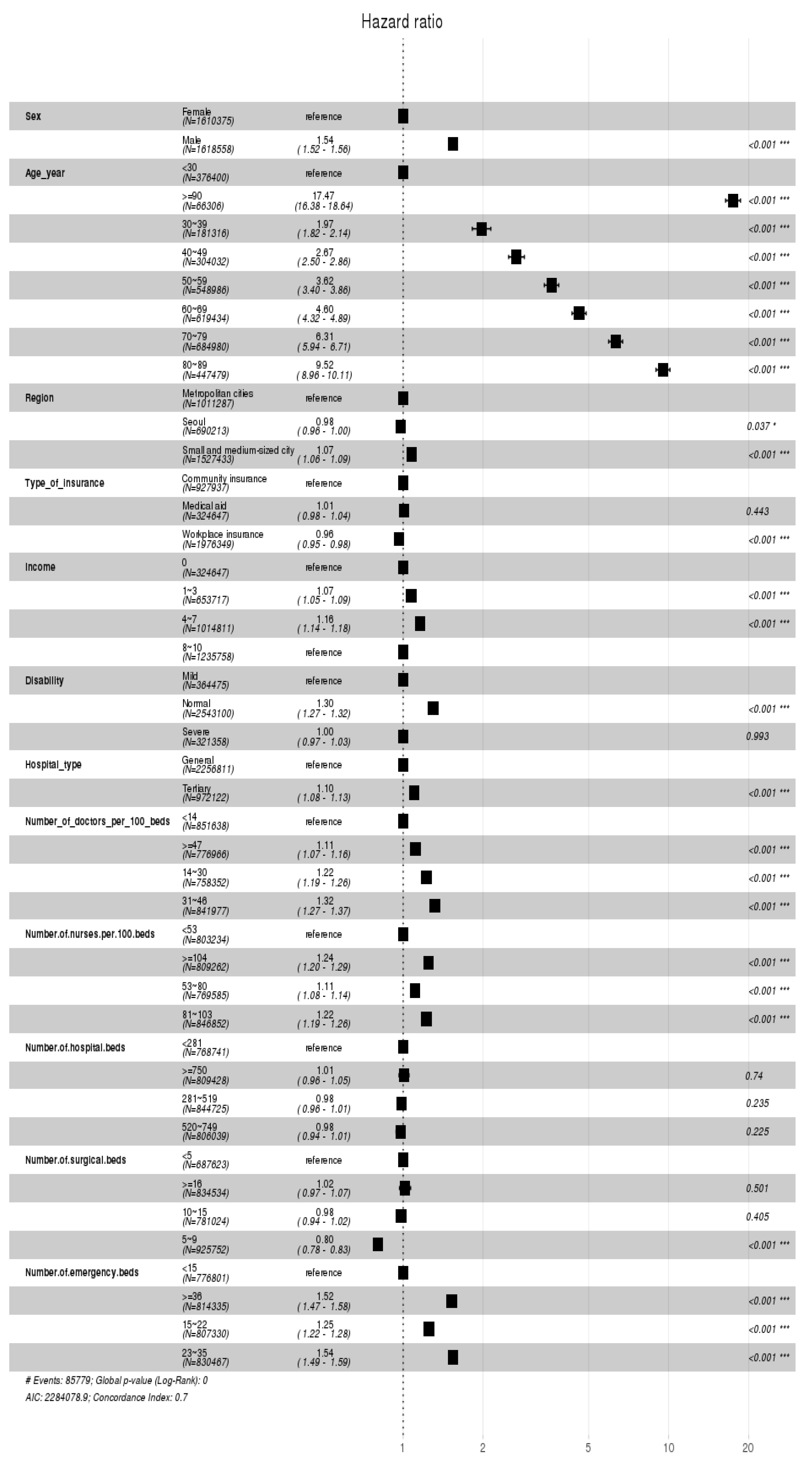
4.1.3. Cox Proportional Hazards Model (General Inpatients)
4.2. Determinants of Survival Time among Inpatients Admitted through Emergency Room
4.2.1. Characteristics of Inpatients Admitted through the Emergency Room
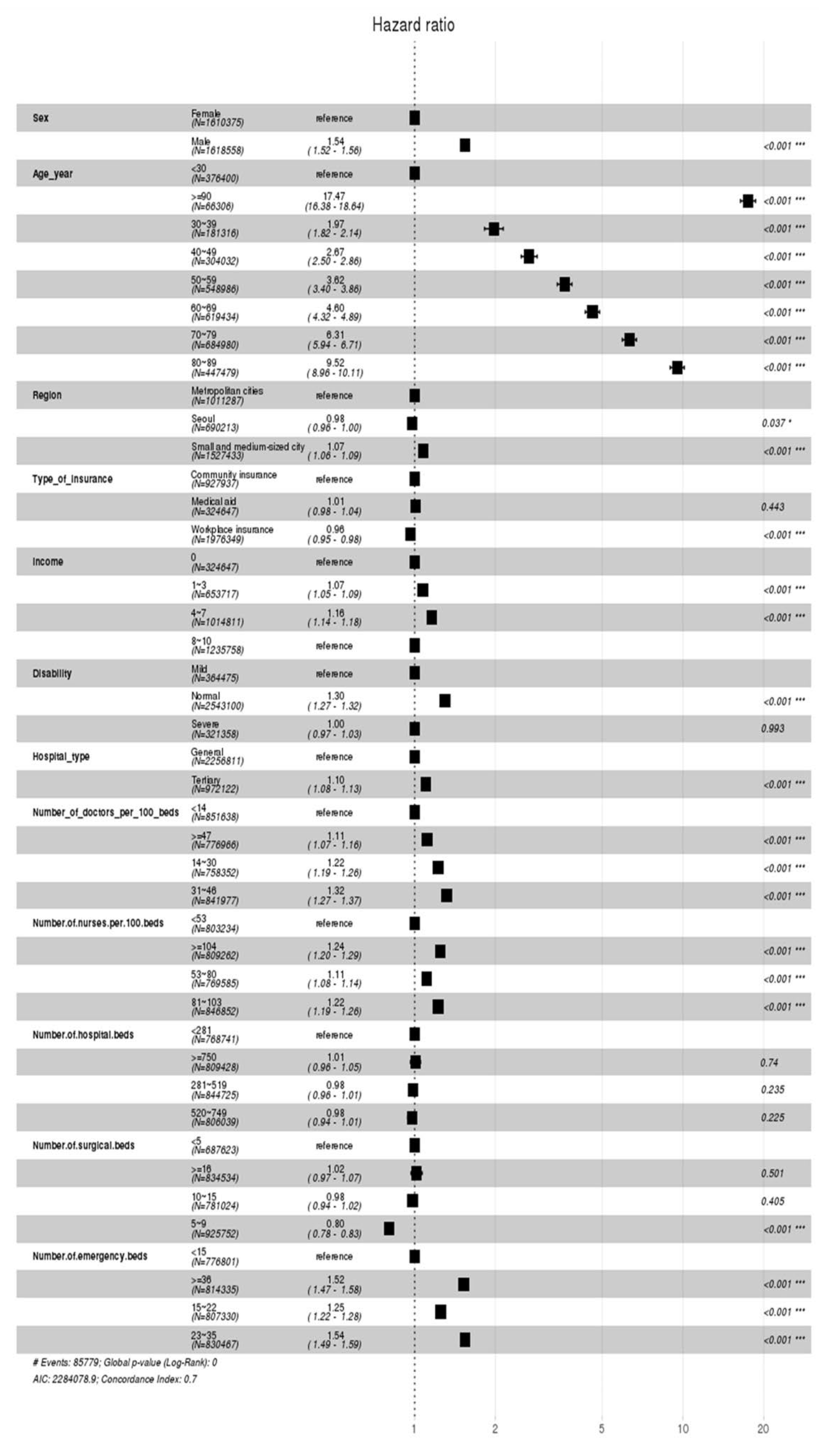
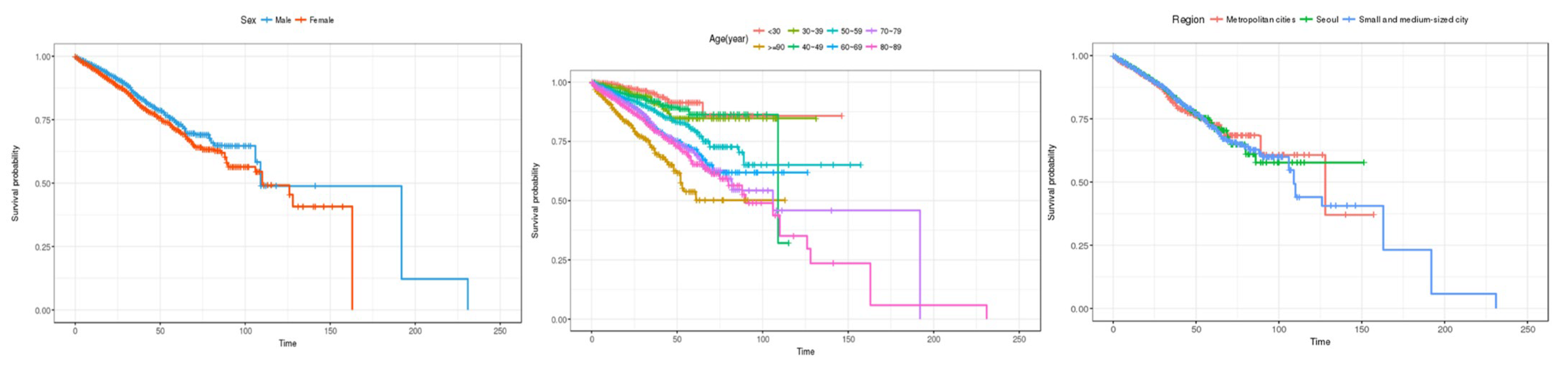
4.2.2. Kaplan–Meier Estimation (Inpatients Admitted through the Emergency Room)
4.2.3. Cox Proportional Hazards Model (Inpatients Admitted through the Emergency Room)
4.3. Summarized Results and Implication
5. Conclusions
5.1. Research Implications
5.2. Limitations and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yoon, K.J. Infectious diseases and public healthcare through the response to COVID-19. Health Welf. Issue Focus 2020, 377, 1–11. [Google Scholar]
- Oh, Y.H. Problems and policy directions of the emergency medical system in Korea. Health Welf. Issue Focus 2011, 105, 1–8. [Google Scholar]
- Jeon, B.; Kim, K.; Jin, Y. Ontology Design to Improve User Fitness of Emergency Medical Statistics Quality(EMSQ). J. Korea Acad.-Ind. Coop. Soc. 2024, 25, 208–215. [Google Scholar]
- Hwang, H.E.; Kahng, H.; Lee, E.S.; Kim, J.Y.; Yoon, Y.H.; Kim, S.B. Early Prediction of Patient Disposition for Emergency Department Visits Using Machine Learning. J. Korean Inst. Ind. Eng. 2021, 47, 263–271. [Google Scholar]
- Jung, G.H.; Kweon, J. A study on space use analysis at emergency room in local emergency medical center. J. Digit. Des. 2017, 17, 81–92. [Google Scholar]
- Kim, T.Y.; Kang, G.H.; Jang, Y.S.; Kim, W.; Choi, H.Y.; Kim, J.G.; Lee, Y.; Song, H.W. Effect of admission decision by emergency physicians on length of stay of emergency room and prognosis for patients diagnosed with medical diseases. J. Korean Soc. Emerg. Med. 2021, 32, 189–197. [Google Scholar]
- Lee, E.B.; Paek, S.H.; Kwon, J.H.; Park, S.-H.; Kim, M.-J.; Byun, Y.-H. Characteristics of children hospitalized through the pediatric emergency department and effects of pediatric emergency ward hospitalization. Pediatr. Emerg. Med. J. 2023, 10, 124–131. [Google Scholar] [CrossRef]
- Lee, S.D. Preventable Trauma Death Rate Improves over 3 Years: 19.9% → 15.7%. Medical News. 2022. Available online: http://www.bosa.co.kr/news/articleView.html?idxno=2169044 (accessed on 21 March 2023).
- Kim, Y.; Jung, K.Y.; Cho, K.H.; Kim, H.; Ahn, H.C.; Oh, S.H.; Lee, J.B.; Yu, S.J.; Lee, D.I.; Im, T.H.; et al. Preventable trauma deaths rates and management errors in emergency medical system in Korea. J. Korean Soc. Emerg. Med. 2006, 17, 385–394. [Google Scholar]
- Lee, E.J.; Song, Y.S.; Oh, S.H. Survival analysis approach for student departure of freshmen: Focusing on the case of S university. J. Korean Assoc. Learn.-Centered Curric. Instr. 2020, 20, 235–258. [Google Scholar] [CrossRef]
- Shin, W.M.; Kim, J.M.; Park, C.Y.; Shin, E.; Tchoe, B. Analysis of factors influencing the survival of patients with Out-of-Hospital of Cardiac Arrest (OHCA). Korean Public Health Res. 2020, 46, 93–105. [Google Scholar]
- Yoo, I.S. What to do to improve emergency care. Health Welf. Forum 2010, 169, 45–57. [Google Scholar]
- Kim, J.H.; Han, M.S.; Kim, C.-K.; Sun, S.; Kim, G.J.; Bae, S.H.; Kim, Y.K. A Study on the legal definition and the demands of the times of a medical technician according to changes in the medical market. J. Digit. Converg. 2021, 19, 397–406. [Google Scholar]
- Lee, J.R.; Do, N.Y. Effect of brand on survival and closing of stores. J. Korea Real Estate Anal. Assoc. 2019, 25, 49–62. [Google Scholar]
- Jing, B.; Zhang, T.; Wang, Z.; Jin, Y.; Liu, K.; Qiu, W.; Ke, L.; Sun, Y.; He, C.; Hou, D.; et al. A deep survival analysis method based on ranking. Artif. Intell. Med. 2019, 98, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Schober, P.; Vetter, T.R. Survival analysis and interpretation of time-to-event data: The tortoise and the hare. Anesth. Analg. 2018, 127, 792. [Google Scholar] [CrossRef] [PubMed]
- In, J.; Lee, D.K. Survival analysis: Part I-analysis of time-to-event. Korean J. Anesthesiol. 2018, 71, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.H.; Yang, J.W.; Min, J.H. Credit prediction based on Kohonen network and survival analysis. J. Korean Oper. Res. Manag. Sci. Soc. 2009, 34, 35–54. [Google Scholar]
- Gémar, G.; Moniche, L.; Morales, A.J. Survival analysis of the Spanish hotel industry. Tour. Manag. 2016, 54, 428–438. [Google Scholar] [CrossRef]
- Gemar, G.; Soler, I.P.; Guzman-Parra, V.F. Predicting bankruptcy in resort hotels: A survival analysis. Int. J. Contemp. Hosp. Manag. 2019, 31, 1546–1566. [Google Scholar] [CrossRef]
- Kristanti, F.T.; Effendi, N. A survival analysis of indonesian distressed company using cox hazard model. Int. J. Econ. Manag. 2017, 11, 155–167. [Google Scholar]
- Kristanti, F.T.; Herwany, A. Corporate governance, financial ratios, political risk and financial distress: A survival analysis. Account. Financ. Rev. 2017, 2, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Nagy, Á.; Munkácsy, G.; Győrffy, B. Pancancer survival analysis of cancer hallmark genes. Sci. Rep. 2021, 11, 6047. [Google Scholar] [CrossRef] [PubMed]
- Viljanen, M.; Airola, A.; Heikkonen, J.; Pahikkala, T. Playtime measurement with survival analysis. IEEE Trans. Games 2017, 10, 128–138. [Google Scholar] [CrossRef]
- Lee, J.B.; Woo, H. Determinants of length of stay in ischemic heart disease patients. J. Health Inform. Stat. 2020, 45, 52–59. [Google Scholar] [CrossRef]


| Category | Characteristics | Limitation |
|---|---|---|
| Linear Regression | Dependent variable: time | Cannot consider the presence of censored data |
| Logistic Regression | Dependent variable: event | Cannot consider time |
| Survival Analysis | Can consider both time and the presence of censored data |
| Researchers | Research Methodology | Research Subjects | Research Purpose |
|---|---|---|---|
| [19] | Log-rank test Cox proportional hazards model | Resort facilities in Spain | To identify financial and non-financial factors affecting the survival of resort facilities in Spain |
| [20] | Log-rank test Cox proportional hazards model | Resort facilities in Spain | To investigate factors affecting the survival of resort facilities in Spain |
| [21] | Cox proportional hazards model | Companies undergoing financial distress | To investigate how restraints to corruptions and financial ratios affect the survival of companies undergoing financial distress |
| [22] | Cox proportional hazards model | Companies undergoing financial distress | To investigate how factors including corporate governance, financial ratios, and political risk affect the company’s survival |
| [23] | Kaplan–Meier estimation Cox proportional hazards model | Pancreatic cancer patients | To estimate the prognostic effect of the established cancer hallmark genes in various cancer types |
| [24] | Kaplan–Meier estimation | Playtimes in game | To propose new methods to measure game playtimes |
| Table | Description |
|---|---|
| Qualification | Includes socio-demographic information (gender, age, residential area, income range, insurance type) of a health checkup examinee (excluding foreigners) or information about the matter of death. |
| Birth and Death | Includes information on subjects whose death has been verified, linked with birth and the cause of death information provided by Statistics Korea. |
| Diagnosis | Includes medical records (main diagnosis information, prescription history, cost-related information, admission records, the department of treatment, etc.); consists of ten DB partitions. |
| Health Checkup | Includes checkup records (Lab value, past medical history, hereditary conditions, lifestyle, etc., retrieved from survey questionnaires) of a health checkup examinee. |
| Medical Institution | Includes information of a medical institution (address, the number of hospital beds) attended by a health checkup examinee. |
| Senior Long-Term Care | Includes information on subjects’ application for long-term care services, usage records, and the status of facilities |
| Table | Feature Code * | Feature Description | Purpose of Use |
|---|---|---|---|
| Common | STD_YYYY | Year between 2016 and 2019 | Merging between tables |
| RN_INDI | A six-digit code for interlinking the tables | ||
| RN_INST | A six-digit code for interlinking the tables | ||
| Qualification | SEX | 1: Male, 2: Female | Sociodemographic feature |
| AGE | Patient’s age in a corresponding year | ||
| SIDO | City code | ||
| GAIBJA_TYPE | A code indicating the type of insurance | Patient feature | |
| CTRB | Income quantile (1–10) | ||
| DSB_SVRT_CD | No inclusion, severe, mild level of disability | ||
| Birth and Death | DTH_YYYYMM | The date of one’s death | Dependent variable |
| Diagnosis | HSPTZ_PATH_TYPE | Admission route | Grouping |
| MCARE_RSLT_TYPE | Patient’s condition on the day of one’s final treatment | Censoring | |
| Medical Institution | INST_CLSFC_CD | Type of medical institutions | Institution feature |
| CNT_DR_TOT | The number of doctors | ||
| CNT_NRS_TOT | The number of nurses | ||
| CNT_BED_INP | The number of hospital beds | ||
| Medical Institution | CNT_BED_OP | The number of surgical beds | Institution feature |
| CNT_BED_ER | The number of emergency beds |
| Category | Feature | Preprocessed Results |
|---|---|---|
| Sociodemographic Information | Gender | [Grouping] Male/Female |
| Age | [Grouping] 10-year unit | |
| City | [Grouping] Seoul/Metropolitan city/Small and medium-sized city | |
| Patient Information | Insurance status | [Grouping] Workplace/Regional/Medical insurees [Grouping] 0/1–3/4–7/8–10 [Grouping] No inclusion, severe, mild |
| Income quantile | ||
| Severity of disability | ||
| Institution Information | Institution type The number of doctors per 100 hospital beds | [Grouping] top general hospitals/general hospitals [Feature preprocessing] (the number of doctors/the number of hospital beds) × 100 [Grouping] in four quantiles [Feature preprocessing] (the number of nurses/the number of hospital beds) × 100 [Grouping] in four quantiles [Grouping] in four quantiles |
| The number of nurses per 100 hospital beds | ||
| The number of hospital beds The number of surgical beds The number of emergency beds |
| Category | Feature | Number of Patients | Number of Dead | Censored Data | ||
|---|---|---|---|---|---|---|
| N | % | |||||
| Sociodemographic Characteristics | Gender | Male | 1,618,558 | 493,753 | 1,124,805 | 69.49 |
| Female | 1,610,375 | 362,935 | 1,247,440 | 77.46 | ||
| Age | ~29 | 376,400 | 8,557 | 367,843 | 97.73 | |
| 30~39 | 181,316 | 11,059 | 170,257 | 93.9 | ||
| 40~49 | 304,032 | 38,933 | 265,099 | 87.19 | ||
| 50~59 | 548,986 | 97,958 | 451,028 | 82.16 | ||
| 60~69 | 619,434 | 155,199 | 464,235 | 74.95 | ||
| 70~79 | 684,980 | 261,576 | 423,404 | 61.81 | ||
| 80~89 | 447,479 | 236,122 | 211,357 | 47.23 | ||
| 90~ | 66,306 | 47,284 | 19,022 | 28.69 | ||
| City | Seoul | 690,213 | 216,436 | 473,777 | 68.64 | |
| Metropolitan city | 1,011,287 | 240,263 | 771,024 | 76.24 | ||
| Small, medium-sized city | 1,527,433 | 399,989 | 1,127,444 | 73.81 | ||
| Patient Characteristics | Insurance status | Medical insuree | 324,647 | 110,780 | 213,867 | 65.88 |
| Regional insurance | 927,937 | 247,733 | 680,204 | 73.30 | ||
| Workplace insurance | 1,976,349 | 498,175 | 1,478,174 | 74.79 | ||
| Income quantile | 0 (= Medical aid) | 324,647 | 110,780 | 213,867 | 65.88 | |
| 1~3 | 653,717 | 161,816 | 491,901 | 75.25 | ||
| 4~7 | 1,014,811 | 238,137 | 776,674 | 76.53 | ||
| 8~10 | 1,235,758 | 345,955 | 889,803 | 72.00 | ||
| Severity of Disability | Normal | 2,543,100 | 596,918 | 1,946,182 | 76.53 | |
| Mild | 364,475 | 129,482 | 234,993 | 64.47 | ||
| Severe | 321,358 | 130,288 | 191,070 | 59.46 | ||
| Institution Characteristics | Type of medical institution | General hospital | 2,256,811 | 521,261 | 1,735,550 | 76.9 |
| Top general hospital | 972,122 | 335,427 | 636,695 | 65.5 | ||
| Number of doctors per 100 hospital beds | ~13 | 851,638 | 164,396 | 687,242 | 80.7 | |
| 14~30 | 758,352 | 173,799 | 584,553 | 77.08 | ||
| 31~46 | 841,977 | 271,496 | 570,481 | 67.75 | ||
| 47~ | 776,966 | 246,997 | 529,969 | 68.21 | ||
| Number of nurses per 100 hospital beds | ~52 | 803,234 | 167,841 | 635,393 | 79.1 | |
| 53~80 | 769,585 | 179,191 | 590,394 | 76.72 | ||
| 81~103 | 846,852 | 245,625 | 601,227 | 71.00 | ||
| 104~ | 809,262 | 264,031 | 545,231 | 67.37 | ||
| Number of hospital beds | ~280 | 768,741 | 144,734 | 624,007 | 81.17 | |
| ~281~519 | 844,725 | 193,682 | 651,043 | 77.07 | ||
| 520~749 | 806,039 | 238,870 | 567,169 | 70.36 | ||
| 750~ | 809,428 | 279,402 | 530,026 | 65.48 | ||
| Number of surgical beds | ~4 | 687,623 | 141,742 | 545,881 | 79.39 | |
| 5~9 | 925,752 | 190,039 | 735,713 | 79.47 | ||
| 10~15 | 781,024 | 250,246 | 530,778 | 67.96 | ||
| 16~ | 834,534 | 274,661 | 559,873 | 67.09 | ||
| Number of emergency beds | ~15 | 776,801 | 146,626 | 630,175 | 81.12 | |
| 15~22 | 807,330 | 190,381 | 616,949 | 76.42 | ||
| 23~35 | 830,467 | 250,014 | 580,453 | 69.89 | ||
| 36~ | 814,335 | 269,667 | 544,668 | 66.89 | ||
| Total | 3,228,933 | 856,688 | 2,372,245 | |||
| Category | Feature | Number of Patients | Number of Dead | Censored Data | ||
|---|---|---|---|---|---|---|
| N | % | |||||
| Sociodemographic Characteristics | Gender | Male | 571,640 | 371,216 | 200,424 | 35.06 |
| Female | 543,474 | 388,387 | 155,087 | 28.54 | ||
| Age | ~29 | 143,679 | 139,950 | 3729 | 2.60 | |
| 30~39 | 63,773 | 59,087 | 4686 | 7.35 | ||
| 40~49 | 93,932 | 81,225 | 12,707 | 13.53 | ||
| 50~59 | 161,395 | 127,515 | 33,880 | 20.99 | ||
| 60~69 | 186,934 | 129,766 | 57,168 | 30.58 | ||
| 70~79 | 237,902 | 132,291 | 105,611 | 44.39 | ||
| 80~89 | 194,696 | 81,129 | 113,567 | 58.33 | ||
| 90~ | 32,803 | 8640 | 24,163 | 73.66 | ||
| City | Seoul | 258,178 | 169,368 | 88,810 | 34.4 | |
| Metropolitan city | 284,779 | 195,224 | 89,555 | 31.45 | ||
| Small, medium-sized city | 572,157 | 395,011 | 177,146 | 30.96 | ||
| Patient Characteristics | Insurance status | Medical insuree | 110,136 | 64,425 | 45,711 | 41.50 |
| Regional insurance | 320,967 | 219,090 | 101,877 | 31.74 | ||
| Workplace insurance | 684,011 | 476,088 | 207,923 | 30.4 | ||
| Income quantile | 0 (=Medical aid) | 110,136 | 64,425 | 45,711 | 41.50 | |
| 1~3 | 224,901 | 158,102 | 158,102 | 70.3 | ||
| 4~7 | 341,334 | 247,235 | 247,235 | 72.43 | ||
| 8~10 | 438,743 | 289,841 | 148,902 | 33.94 | ||
| Severity of Disability | Normal | 865,904 | 622,833 | 242,261 | 27.98 | |
| Mild | 127,769 | 72,803 | 54,966 | 43.02 | ||
| Severe | 122,251 | 63,967 | 58,284 | 47.68 | ||
| Institution Characteristics | Type of medical institution | General hospital | 684,519 | 487,287 | 197,232 | 28.81 |
| Top general hospital | 430,595 | 272,316 | 158,279 | 36.76 | ||
| Number of doctors per 100 hospital beds | ~13 | 135,227 | 96,104 | 39,123 | 28.93 | |
| 14~30 | 245,888 | 177,896 | 67,992 | 27.65 | ||
| 31~46 | 398,310 | 263,256 | 135,054 | 33.91 | ||
| 47~ | 335,689 | 222,347 | 113,342 | 33.76 | ||
| Number of nurses per 100 hospital beds | ~52 | 139,881 | 97,734 | 42,147 | 30.13 | |
| 53~80 | 227,528 | 163,339 | 64,189 | 28.21 | ||
| 81~103 | 390,697 | 267,089 | 123,608 | 31.64 | ||
| 104~ | 357,008 | 231,441 | 125,567 | 35.17 | ||
| Number of hospital beds | ~280 | 138,642 | 102,709 | 35,933 | 25.92 | |
| ~281~519 | 230,297 | 163,236 | 67,061 | 29.12 | ||
| 520~749 | 393,323 | 269,569 | 123,754 | 31.46 | ||
| 750~ | 352,852 | 224,089 | 128,763 | 36.49 | ||
| Number of surgical beds | ~4 | 130,599 | 94,109 | 36,940 | 28.29 | |
| 5~9 | 243,815 | 179,372 | 64,443 | 26.43 | ||
| 10~15 | 372,513 | 248,428 | 124,085 | 33.31 | ||
| 16~ | 368,187 | 237,694 | 130,493 | 35.44 | ||
| Number of emergency beds | ~15 | 115,294 | 81,769 | 33,525 | 29.08 | |
| 15~22 | 243,659 | 177,732 | 65,927 | 27.06 | ||
| 23~35 | 370,612 | 249,681 | 120,931 | 32.63 | ||
| 36~ | 385,549 | 250,421 | 135,128 | 35.05 | ||
| Total | 1,115,114 | 759,603 | 355,511 | |||
| Category | Feature | General inpatient | Inpatients Admitted through ER |
|---|---|---|---|
| Sociodemographic Characteristics | Gender | Male > Female | Male > Female |
| Age | Above 90s > 80s > 70s > 60s > 50s > 40s > 30s > below 30s | Above 90s > 80s > 70s > 60s > 50s > 40s > 30s > below 30s | |
| City | Small and medium-sized city > Seoul > Metropolitan city | Metropolitan city > Small and medium-sized city > Seoul | |
| Patient Characteristics | Insurance status | (Medical insurees = Regional insurance) > Workplace insurance | Medical insurees > Regional insurance > Workplace insurance |
| Income quantile | 4–7 quantiles > 1–3 quantiles >(0 quantile = 8–10 quantiles) | 4–7 quantiles > 1–3 quantiles > (0 quantiles = 8–10 quantiles) | |
| Severity of disability | Normal > (Severe = Mild) | Normal > Mild > Severe | |
| Institution Characteristics | Type of institution | Top general hospital > General hospital | Top general hospital > General hospital |
| Number of doctors per 100 hospital beds | 31–48 > 14–30 > above 47 > below 14 | 14–30 > 31–48 > (above 47 = below 14) | |
| Number of nurses per 100 hospital beds | Above 104 > 81–103 > 53–80 > below 53 | (Below 53 = Above 104) > 53–80 > 81–103 | |
| Number of hospital beds | Below 281 = 281–519 = 520–749 = above 750 | 281–519 > above 750 > (below 281 = 520–749) | |
| Number of surgical beds | (Below 5 = 10–15 = above 16) > 5–9 | Above 16 > 10–15 > below 5 > 5–9 | |
| Number of emergency beds | 23–35 > above 36 > 15–22 > below 15 | Above 36 > 23–35 > 15–22 > below 15 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, H.; Ryu, S.; Choi, I.; Kwon, A.E.; Kim, J. A Comparative Study of Hospitalization Mortality Rates between General and Emergency Hospitalized Patients Using Survival Analysis. Healthcare 2024, 12, 1982. https://doi.org/10.3390/healthcare12191982
Chang H, Ryu S, Choi I, Kwon AE, Kim J. A Comparative Study of Hospitalization Mortality Rates between General and Emergency Hospitalized Patients Using Survival Analysis. Healthcare. 2024; 12(19):1982. https://doi.org/10.3390/healthcare12191982
Chicago/Turabian StyleChang, Haegak, Seiyoung Ryu, Ilyoung Choi, Anglea Eunyoung Kwon, and Jaekyeong Kim. 2024. "A Comparative Study of Hospitalization Mortality Rates between General and Emergency Hospitalized Patients Using Survival Analysis" Healthcare 12, no. 19: 1982. https://doi.org/10.3390/healthcare12191982






