Predictive Factors for Onset of Moderate-to-Severe Disability Following Hospital Discharge Due to Rib Fractures
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
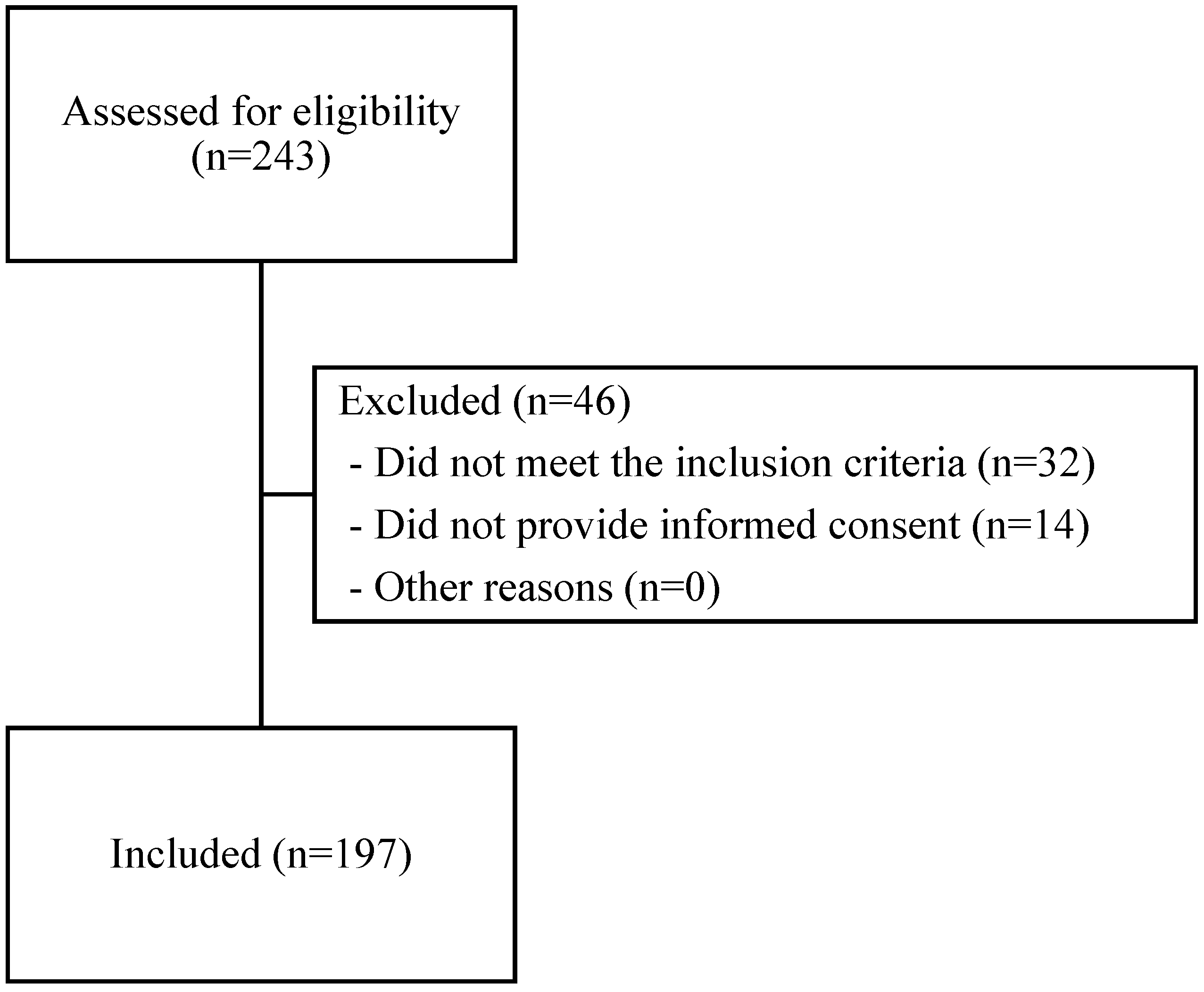
2.2. Participants
2.3. Data Collection
2.4. Statistical Analysis
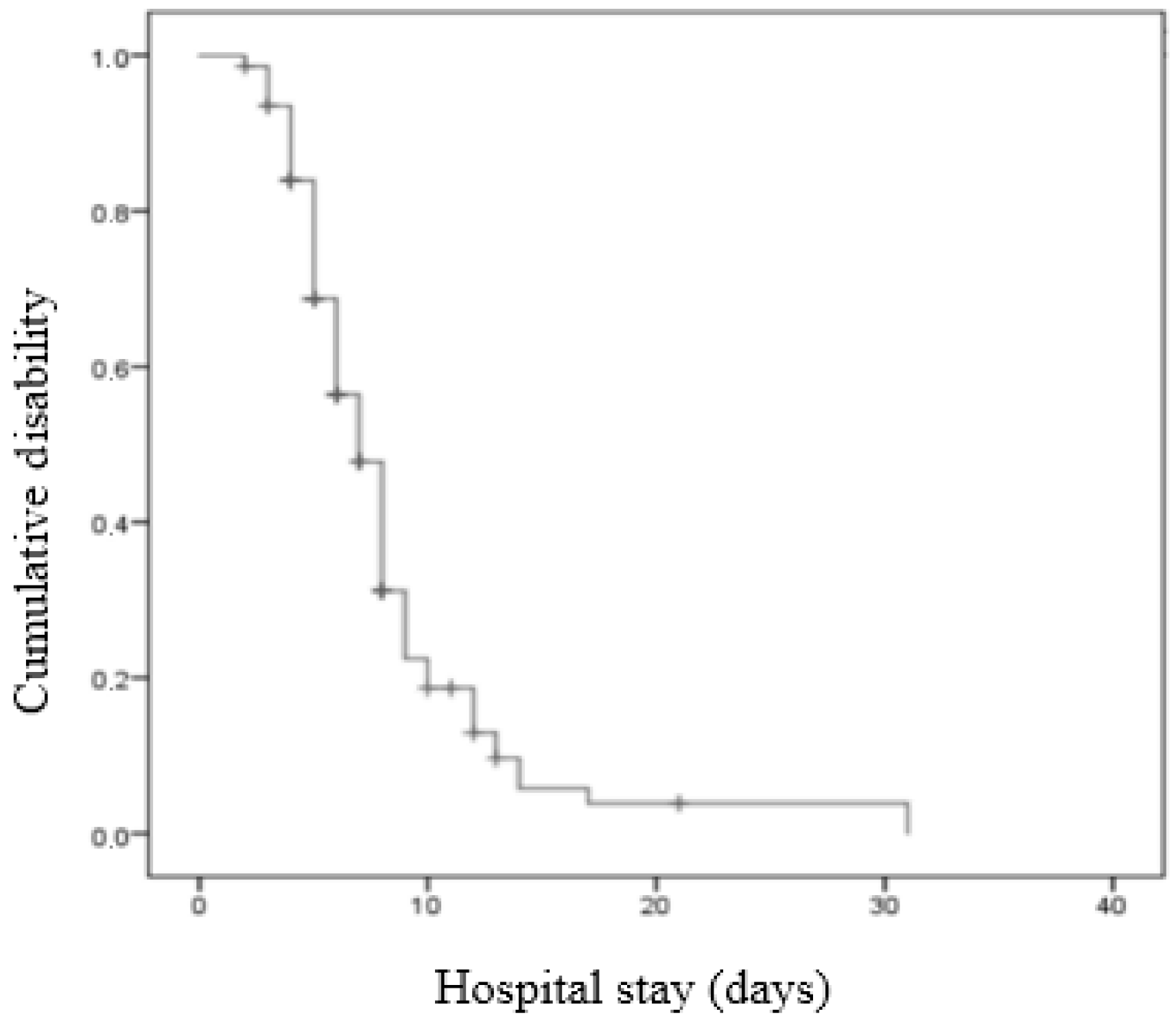
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Prins, J.T.H.; Van Lieshout, E.M.M.; Reijnders, M.R.L.; Verhofstad, M.H.J.; Wijffels, M.M.E. Rib fractures after blunt thoracic trauma in patients with normal versus diminished bone mineral density: A retrospective cohort study. Osteoporos. Int. 2020, 31, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Ezzati, M.; Lopez, A.D.; Rodgers, A.; Vander Hoorn, S.; Murray, C.J. Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet 2002, 360, 1347–1360. [Google Scholar] [CrossRef]
- Gowing, R.; Jain, M.K. Injury patterns and outcomes associated with elderly trauma victims in Kingston, Ontario. Can. J. Surg. 2007, 50, 437–444. [Google Scholar] [PubMed]
- He, Z.; Zhang, D.; Xiao, H.; Zhu, Q.; Xuan, Y.; Su, K.; Liao, M.; Tang, Y.; Xu, E. The ideal methods for the management of rib fractures. J. Thorac. Dis. 2019, 11 (Suppl. S8), S1078–S1089. [Google Scholar] [CrossRef] [PubMed]
- Easter, A. Management of patients with multiple rib fractures. Am. J. Crit. Care 2001, 10, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Gasparri, M.G.; Tisol, W.B.; Haasler, G.B. Rib stabilization: Lessons learned. Eur. J. Trauma Emerg. Surg. 2010, 36, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Sarani, B. Surgical Stabilization of Rib Fractures: Indications and Technique. In Atlas of Trauma; Springer: Cham, Switzerlsnd, 2020; pp. 23–27. [Google Scholar]
- Sirmali, M.; Türüt, H.; Topçu, S.; Gülhan, E.; Yazici, Ü.; Kaya, S.; Taştepe, I. A comprehensive analysis of traumatic rib fractures: Morbidity, mortality and management. Eur. J. Cardio-Thorac. Surg. 2003, 24, 133–138. [Google Scholar] [CrossRef]
- Metaxas, E.K.; Moustardas, M.P.; Gerazounis, M.I. Rib Fractures: Retrospective Analysis of 1428 Cases. Surg. Chron. 2014, 19, 37–39. [Google Scholar]
- Iqbal, H.J.; Alsousou, J.; Shah, S.; Jayatilaka, L.; Scott, S.; Scott, S.; Melling, D. Early surgical stabilization of complex chest wall injuries improves short-term patient outcomes. J. Bone Jt. Surg. 2018, 100, 1298–1308. [Google Scholar] [CrossRef]
- Dalton, M.K.; Minarich, M.J.; Twaddell, K.J.; Hazelton, J.P.; Fox, N.M. The expedited discharge of patients with multiple traumatic rib fractures is cost-effective. Injury 2019, 50, 109–112. [Google Scholar] [CrossRef]
- Bulger, E.M.; Arneson, M.A.; Mock, C.N.; Jurkovich, G.J. Rib fractures in the elderly. J. Trauma Acute Care Surg. 2000, 48, 1040–1047. [Google Scholar] [CrossRef] [PubMed]
- Barnea, Y.; Kashtan, H.; Skornick, Y.; Werbin, N. Isolated rib fractures in elderly patients: Mortality and morbidity. Can. J. Surg. 2002, 45, 43–46. [Google Scholar] [PubMed]
- Bergeron, E.; Lavoie, A.; Clas, D.; Moore, L.; Ratte, S.; Tetreault, S.; Lemaire, J.; Martin, M. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J. Trauma Acute Care Surg. 2003, 54, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Kerr-Valentic, M.A.; Arthur, M.; Mullins, R.J.; Pearson, T.E.; Mayberry, J.C. Rib fracture pain and disability: Can we do better? J. Trauma Acute Care Surg. 2003, 54, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Fabricant, L.; Ham, B.; Mullins, R.; Mayberry, J. Prolonged pain and disability are common after rib fractures. Am. J. Surg. 2013, 205, 511–516. [Google Scholar] [CrossRef]
- Martin, T.J.; Eltorai, A.S.; Dunn, R.; Varone, A.; Joyce, M.F.; Kheirbek, T.; Adams, C., Jr.; Daniels, A.H.; Eltorai, A.E.M. Clinical management of rib fractures and methods for prevention of pulmonary complications: A review. Injury 2019, 50, 1159–1165. [Google Scholar] [CrossRef]
- Covinsky, K.E.; Pierluissi, E.; Johnston, C.B. Hospitalization-Associated Disability: “She Was Probably Able to Ambulate, but I’m Not Sure”. JAMA 2011, 306, 1782–1793. [Google Scholar] [CrossRef]
- Gordy, S.; Fabricant, L.; Ham, B.; Mullins, R.; Mayberry, J. The contribution of rib fractures to chronic pain and disability. Am. J. Surg. 2014, 207, 659–663. [Google Scholar] [CrossRef]
- Benchimol, E.I.; Smeeth, L.; Guttmann, A.; Harron, K.; Moher, D.; Petersen, I.; Sørensen, H.T.; von Elm, E.; Langan, S.M. The Reporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med. 2015, 12, e1001885. [Google Scholar] [CrossRef]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Chen, J.; Jeremitsky, E.; Philp, F.; Fry, W.; Smith, R.S. A chest trauma scoring system to predict outcomes. Surgery 2014, 156, 988–994. [Google Scholar] [CrossRef] [PubMed]
- Samman, Y.; Masood, I.; Killampalli, V.V.; Howell, N.; Alpar, E.K.; Banerjee, S.K. The value of lung injury score in assessing the outcome of patients with rib fracture. Eur. J. Trauma 2005, 31, 133–137. [Google Scholar] [CrossRef]
- Alvarez Solar, M.; Alaiz Rojo, A.T.; Brun Gurpegui, E.; Cabañeros Vicente, J.J.; Calzón Frechoso, M.; Cosío Rodríguez, I.; García López, P.; García-Cañedo Fernández, R.; Pardo González, I.; Suárez González, A. Capacidad funcional de pacientes mayores de 65 años, según el índice de Katz. Fiabilidad del método. Aten. Prim. 1992, 10, 812–815. [Google Scholar]
- Sum, S.-K.; Peng, Y.-C.; Yin, S.-Y.; Huang, P.-F.; Wang, Y.-C.; Chen, T.-P.; Tung, H.-H.; Yeh, C.-H. Using an incentive spirometer reduces pulmonary complications in patients with traumatic rib fractures: A randomized controlled trial. Trials 2019, 20, 797. [Google Scholar] [CrossRef] [PubMed]
- Abdelwahed, H.S.; Martinez, F.E. Multiple Rib Fractures Management in a Tertiary Trauma Center: A Retrospective Observational Study. Egypt. J. Crit. Care Med. 2022, 9, 10–15. [Google Scholar] [CrossRef]
- Giardina, C.; Cutroneo, P.M.; Mocciaro, E.; Russo, G.T.; Mandraffino, G.; Basile, G.; Rapisarda, F.; Ferrara, R.; Spina, E.; Arcoraci, V. Adverse drug reactions in hospitalized patients: Results of the forward (facilitation of reporting in hospital ward) study. Front. Pharmacol. 2018, 9, 350. [Google Scholar] [CrossRef]
- Stürmer, E.K.; Seidlová-Wuttke, D.; Sehmisch, S.; Rack, T.; Wille, J.; Frosch, K.H.; Wuttke, W.; Stürmer, K.M. Standardized bending and breaking test for the normal and osteoporotic metaphyseal tibias of the rat: Effect of estradiol, testosterone, and raloxifene. J. Bone Miner. Res. 2006, 21, 89–96. [Google Scholar] [CrossRef]
- Sigurdsson, G.; Aspelund, T.; Chang, M.; Jonsdottir, B.; Sigurdsson, S.; Eiriksdottir, G.; Gudmundsson, A.; Harris, T.B.; Gudnason, V.; Lang, T.F. Increasing sex difference in bone strength in old age: The Age, Gene/Environment Susceptibility-Reykjavik study (AGES-REYKJAVIK). Bone 2006, 39, 644–651. [Google Scholar] [CrossRef]
- Schafman, M.A.; Kang, Y.-S.; Moorhouse, K.; White, S.E.; Bolte, J.H.; Agnew, A.M. Age and sex alone are insufficient to predict human rib structural response to dynamic A-P loading. J. Biomech. 2016, 49, 3516–3522. [Google Scholar] [CrossRef]
- Etxebarria-Foronda, I.; Caeiro-Rey, J.R.; Larrainzar-Garijo, R.; Vaquero-Cervino, E.; Roca-Ruiz, L.; Mesa Ramos, M.; Pérez, J.M.; Carpintero-Benitez, P.; Cebrián, A.F.; Gil-Garay, E. SECOT-GEIOS guidelines in osteoporosis and fragility fracture. An update. Rev. Esp. Cir. Ortop. Traumatol. 2015, 59, 373–393. [Google Scholar] [CrossRef]
- Chona, D.; Lakomkin, N.; Bulka, C.; Mousavi, I.; Kothari, P.; Dodd, A.C.; Shen, M.S.; Obremskey, W.T.; Sethi, M.K. Predicting the post-operative length of stay for the orthopaedic trauma patient. Int. Orthop. 2017, 41, 859–868. [Google Scholar] [CrossRef]
- Shafi, S.; Barnes, S.; Nicewander, D.; Ballard, D.; Nathens, A.B.; Ingraham, A.M.; Hemmila, M.; Goble, S.; Neal, M.; Pasquale, M.; et al. Health care reform at trauma centers—Mortality, complications, and length of stay. J. Trauma Acute Care Surg. 2010, 69, 1367–1371. [Google Scholar] [CrossRef] [PubMed]
- Lang, P.; Heitz, D.; Hédelin, G.; Dramé, M.; Jovenin, N.; Ankri, J.; Somme, D.; Novella, J.; Gauvain, J.B.; Couturier, P.; et al. Early markers of prolonged hospital stays in older people: A prospective, multicenter study of 908 inpatients in french acute hospitals. J. Am. Geriatr. Soc. 2006, 54, 1031–1039. [Google Scholar] [CrossRef] [PubMed]
- Brotemarkle, R.A.; Resnick, B.; Michaels, K.; Morton, P.; Wells, C. Length of hospital stay and discharge disposition in older trauma patients. Geriatr. Nurs. 2015, 36, S3–S9. [Google Scholar] [CrossRef] [PubMed]
- Beal, S.L.; Oreskovich, M.R. Long-term disability associated with flail chest injury. Am. J. Surg. 1985, 150, 324–326. [Google Scholar] [CrossRef] [PubMed]
- Baker, E.; Xyrichis, A.; Norton, C.; Hopkins, P.; Lee, G. The long-term outcomes and health-related quality of life of patients following blunt thoracic injury: A narrative literature review. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 67. [Google Scholar] [CrossRef]
- Luceri, R.E.; Glass, N.E.; Bailey, J.A.; Sifri, Z.C.; Kunac, A.; Bonne, S.L.; Yonclas, P.P.; Mosenthal, A.C.; Livingston, D.H. First rib fracture: A harbinger of severe trauma? Am. J. Surg. 2018, 216, 740–744. [Google Scholar] [CrossRef]
- Fokin, A.; Wycech, J.; Picard, E.B.; Weisz, R.; Puente, I.M. Is first rib fracture a culprit or a sign of injury severity? It is both. J. Orthop. Trauma 2018, 32, 391–396. [Google Scholar] [CrossRef]
- Miller, D.L.; Mansour, K.A. Blunt traumatic lung injuries. Thorac. Surg. Clin. 2007, 17, 57–61. [Google Scholar] [CrossRef]
- Flagel, B.T.; Luchette, F.A.; Reed, R.L.; Esposito, T.J.; Davis, K.A.; Santaniello, J.M.; Gamelli, R.L. Half-a-dozen ribs: The breakpoint for mortality. Surgery 2005, 138, 717–725. [Google Scholar] [CrossRef]
- Carrie, C.; Guemmar, Y.; Cottenceau, V.; de Molliens, L.; Petit, L.; Sztark, F.; Biais, M. Long-term disability after blunt chest trauma: Don’t miss chronic neuropathic pain! Injury 2019, 50, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Todd, S.R.; McNally, M.M.; Holcomb, J.B.; Kozar, R.A.; Kao, L.S.; Gonzalez, E.A.; Cocanour, C.S.; Vercruysse, G.A.; Lygas, M.H.; Brasseaux, B.K.; et al. A multidisciplinary clinical pathway decreases rib fracture–associated infectious morbidity and mortality in high-risk trauma patients. Am. J. Surg. 2006, 192, 806–811. [Google Scholar] [CrossRef] [PubMed]
- Siew, E.D.; Abdel-Kader, K.; Perkins, A.M.; Greevy, R.A.; Parr, S.K.; Horner, J.; Vincz, A.J.; Denton, J.; Wilson, O.D.; Hung, A.M.; et al. Timing of recovery from moderate to severe aki and the risk for future loss of kidney function. Am. J. Kidney Dis. 2020, 75, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Tung, B.; Chu, P.; Tai, S.; Wang, Y.; Tsai, T.; Lee, T.; Hsu, Y. Predictors and timing of recovery in patients with immediate facial nerve dysfunction after parotidectomy. Head Neck 2014, 36, 247–251. [Google Scholar] [CrossRef]
| Outcomes Measures | Short Hospital Stay (n = 15) | Long Hospital Stay (n = 182) | p-Value | |
|---|---|---|---|---|
| General characteristics | Age (years) | 62.27 ± 16.25 | 59.77 ± 17.80 | 0.600 |
| Sex, n (male%) | 4 (26.7) | 50 (27.5) | 0.946 | |
| Comorbidities | 1.71 ± 1.82 | 1.65 ± 1.89 | 0.908 | |
| Rib fracture causes | Fall, n (%) | 8 (53.3) | 100 (55.2) | 0.886 |
| Traffic, n (%) | 7 (46.7) | 79 (43.4) | 0.807 | |
| Pharmacotherapy | No. drugs | 2.5 ± 3.06 | 4.40 ± 5.69 | 0.035 * |
| Rib fracture pattern | No. rib fractures | 4.53 ± 2.06 | 5.20 ± 2.55 | 0.324 |
| First Rib Fractured, n (%) | 2 (13.3) | 20 (11.3) | 0.814 | |
| Bilateral rib fractures, n (%) | 3 (18.2) | 29 (16) | 0.848 | |
| Flail chest, n (%) | 13 (86.7) | 149 (82) | 0.652 | |
| Clavicle fracture, n (%) | 0 | 22 (12.2) | 0.152 | |
| Sternum fracture, n (%) | 2 (13.3) | 12 (6.6) | 0.333 | |
| Scapular fracture, n (%) | 1 (6.7) | 9 (5) | 0.774 | |
| Transverse process fracture, n (%) | 0 | 7 (3.9) | 0.438 | |
| Rib fracture severity | Chest trauma score | 4.60 ± 1.21 | 4.94 ± 1.58 | 0.421 |
| Lung injury score | 0.22 ± 0.41 | 0.64 ± 0.57 | 0.007 * | |
| Pre-injury disability | Katz | 1.93 ± 1.58 | 2.09 ± 1.59 | 0.711 |
| Short Hospital Stay | Long Hospital Stay | ||||
|---|---|---|---|---|---|
| Outcomes Measures | Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | |
| General characteristics | Age (years) | 0.98 (0.94–1.02) | 0.361 | 0.99 (0.98–1.01) | 0.526 |
| Sex (male) | 0.62 (013–2.99) | 0.552 | 0.73 (0.61–0.87) | <0.001 ** | |
| Comorbidities | 0.77 (0.49–1.18) | 0.229 | 1.04 (0.95–1.14) | 0.251 | |
| Rib fracture causes | Fall | 1.49 (0.39–5.54) | 0.554 | 0.96 (0.83–1.11) | 0.569 |
| Traffic | 0.67 (0.18–2.51) | 0.554 | 1.03 (0.89–1.19) | 0.673 | |
| Pharmacotherapy | No. drugs | 0.96 (0.85–1.08) | 0.553 | 1.01 (0.93–1.08) | 0.812 |
| Rib fracture pattern | No. rib fractures | 0.94 (0.68–1.29) | 0.699 | 0.98 (0.89–1.08) | 0.164 |
| First Rib Fractured | 0.91 (0.01–1.45) | 0.09 | 1.78 (0.71–4.44) | 0.047 * | |
| Bilateral rib fractures | 0.19 (0.06–0.55) | 0.464 | 0.87 (0.69–1.09) | 0.227 | |
| Flail chest | 0.04 (0.01–1.62) | 0.781 | 1.29 (1.01–1.65) | 0.046 * | |
| Clavicle fracture | - | - | 1.17 (0.94–1.46) | 0.14 | |
| Sternum fracture | 0.49 (0.1–2.37) | 0.376 | 1.01 (0.72–1.39) | 0.96 | |
| Scapular fracture | - | - | 0.88 (0.58–1.33) | 0.564 | |
| Transverse process fracture | - | - | 1.54 (0.93–2.55) | 0.47 * | |
| Rib fracture severity | Chest trauma score | 0.87 (0.51–1.49) | 0.629 | 0.96 (0.84–1.09) | 0.444 |
| Lung injury score | 0.9 (0.1–11.12) | 0.336 | 1.65 (0.44–0.93) | <0.001 ** | |
| Pre-injury disability | Katz | 1.47 (0.79–2.74) | 0.216 | 1.37 (1.16–1.62) | <0.001 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Granados Santiago, M.; López López, L.; Quero Valenzuela, F.; Calvache Mateo, A.; Martín Núñez, J.; Ortiz Rubio, A.; Valenza, M.C. Predictive Factors for Onset of Moderate-to-Severe Disability Following Hospital Discharge Due to Rib Fractures. Healthcare 2024, 12, 1984. https://doi.org/10.3390/healthcare12191984
Granados Santiago M, López López L, Quero Valenzuela F, Calvache Mateo A, Martín Núñez J, Ortiz Rubio A, Valenza MC. Predictive Factors for Onset of Moderate-to-Severe Disability Following Hospital Discharge Due to Rib Fractures. Healthcare. 2024; 12(19):1984. https://doi.org/10.3390/healthcare12191984
Chicago/Turabian StyleGranados Santiago, María, Laura López López, Florencio Quero Valenzuela, Andrés Calvache Mateo, Javier Martín Núñez, Araceli Ortiz Rubio, and Marie Carmen Valenza. 2024. "Predictive Factors for Onset of Moderate-to-Severe Disability Following Hospital Discharge Due to Rib Fractures" Healthcare 12, no. 19: 1984. https://doi.org/10.3390/healthcare12191984









