The Nursing Theory of Complex Adaptive Systems: A New Paradigm for Nursing
Abstract
1. Introduction
2. Basic Concepts of the Complex Adaptive Systems
- Adaptability is the system’s ability to respond flexibly to change without losing integrity [12]. Adaptability requires agents within the system (such as nurses) to develop problem-solving and quick decision-making skills.
- Self-organization is the ability of the system to organize spontaneously without the need for centralized planning [10]. In healthcare environments, this principle translates into the ability of operators to coordinate and collaborate flexibly.
- Emergence is the ability of a system to generate new properties and unpredictable behaviors from the interactions between its components [36]. Applied to nursing, this principle suggests that nurses can generate innovative solutions through their actions and interactions.
- Nonlinearity, meaning that the relationships between the system components are not linear but are characterized by complex feedback and interdependencies [16]. This makes it difficult to predict how the system will evolve accurately.
- Sensitivity to initial conditions small changes in the system’s initial conditions can lead to significant differences in its evolution over time [12]. This principle emphasizes the importance of understanding the context and specific circumstances in which the system operates.
2.1. Nursing Theories
2.2. Theoretical Development of Complex Adaptive Systems
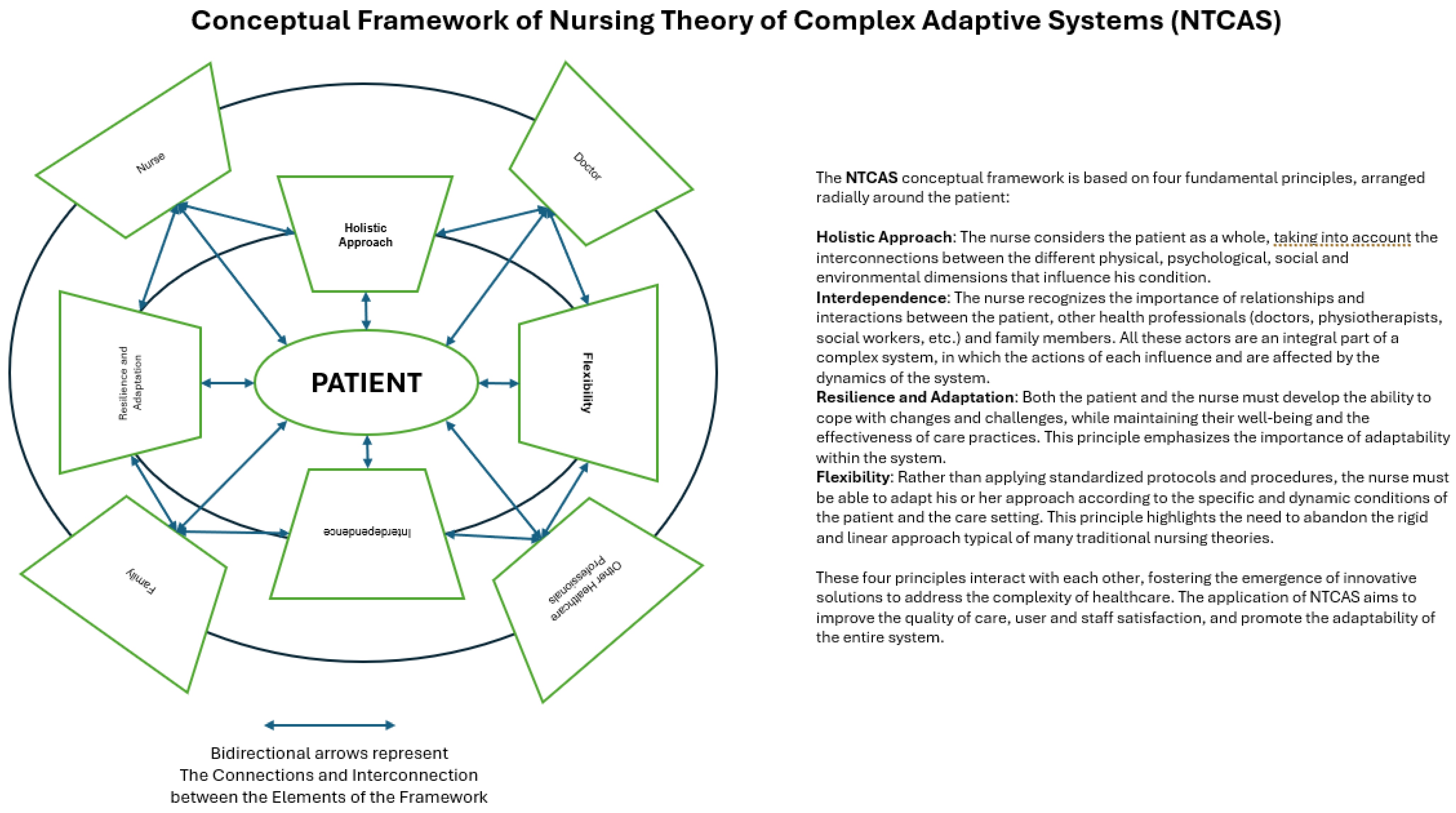
- Holistic approach: consider the patient a complex, interconnected system rather than a collection of isolated symptoms.
- Interdependence: recognize the importance of relationships and interactions between patients, nurses, and other healthcare professionals.
- Resilience and Adaptation: promote the ability of patients and nursing staff to adapt to changes and challenges.
- Flexibility: adapt nursing practices according to patients’ specific and dynamic conditions and the context.
3. Implications for Nursing
Limitations and Future Research
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ratnapalan, S.; Lang, D. Health Care Organizations as Complex Adaptive Systems. Health Care Manag. 2020, 39, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Glover, W.J.; Nissinboim, N.; Naveh, E. Examining innovation in hospital units: A complex adaptive systems approach. BMC Health Serv. Res. 2020, 20, 554. [Google Scholar] [CrossRef] [PubMed]
- White, M.; Hill, G. Special Collection Editorial: Nursing through times of challenge and adversity. J. Res. Nurs. 2023, 28, 394–400. [Google Scholar] [CrossRef]
- Ee, C.; Lake, J.; Firth, J.; Hargraves, F.; de Manincor, M.; Meade, T.; Marx, W.; Sarris, J. An integrative collaborative care model for people with mental illness and physical comorbidities. Int. J. Ment. Health Syst. 2020, 14, 83. [Google Scholar] [CrossRef]
- Sun, S.; Xie, Z.; Yu, K.; Jiang, B.; Zheng, S.; Pan, X. COVID-19 and healthcare system in China: Challenges and progression for a sustainable future. Glob. Health 2021, 17, 14. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sloane, D.M.; Bruyneel, L.; Van den Heede, K.; Griffiths, P.; Busse, R.; Diomidous, M.; Kinnunen, J.; Kózka, M.; Lesaffre, E.; et al. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet 2014, 383, 1824–1830. [Google Scholar] [CrossRef]
- Duffy, J.R. Quality Caring in Nursing and Health Systems: Implications for Clinicians, Educators, and Leaders; Springer Publishing Company: New York, NY, USA, 2022. [Google Scholar]
- Plsek, P.E. Redesigning health care with insights from the science of complex adaptive systems. In Crossing the Quality Chasm: A New Health System for the 21st Century; National Academies Press: Washington, DC, USA, 2001; pp. 309–322. [Google Scholar]
- Kunjir, A. Exploring the Applications of Complex Adaptive Systems in the Real World: A Review. Artif. Intell. Mach. Learn. User Interface Des. 2024, 1, 136–160. [Google Scholar] [CrossRef]
- Begun, J.W.; Zimmerman, B.; Dooley, K. Health care organizations as complex adaptive systems. Adv. Health Care Organ. Theory 2003, 253, 288. [Google Scholar]
- Olsson, A.; Thunborg, C.; Björkman, A.; Blom, A.; Sjöberg, F.; Salzmann-Erikson, M. A scoping review of complexity science in nursing. J. Adv. Nurs. 2020, 76, 1961–1976. [Google Scholar] [CrossRef]
- Rouse, W.B. Health care as a complex adaptive system: Implications for design and management. Bridge-Wash.-Natl. Acad. Eng. 2008, 38, 17. [Google Scholar]
- Ulrich, F.; Nielsen, P.A. Chaos and creativity in dynamic idea evaluation: Theorizing the organization of problem-based portfolios. Creat. Innov. Manag. 2020, 29, 566–580. [Google Scholar] [CrossRef]
- Benhamou, S.; Artificial Intelligence and the Future of Work. Revue d’Économie Industrielle [En Ligne], 169 | 1er Trimestre 2020, mis en Ligne le 05 Janvier 2023, Consulté le 17 Juin 2024. Available online: http://journals.openedition.org/rei/8727 (accessed on 17 June 2024).
- Rapp, A.; Boldi, A. Exploring the Lived Experience of Behavior Change Technologies: Towards an Existential Model of Behavior Change for HCI. ACM Trans. Comput.-Hum. Interact. 2023, 30, 81. [Google Scholar] [CrossRef]
- Plsek, P.E.; Greenhalgh, T. Complexity science: The challenge of complexity in health care. BMJ 2001, 323, 625–628. [Google Scholar] [CrossRef] [PubMed]
- Reilly, C.M.; Kaplan, B.; Porter-O’Grady, T. Nursing Leadership during Crisis: Insights Guiding Leaders from the COVID-19 Pandemic; Sigma Theta Tau: Indianapolis, IN, USA, 2022. [Google Scholar]
- García, M.; Aguilar, J. Emergent control in the context of industry 4.0. Int. J. Comput. Integr. Manuf. 2022, 35, 247–262. [Google Scholar] [CrossRef]
- van Schothorst-van Roekel, J.; Weggelaar-Jansen, A.M.J.W.M.; Hilders, C.C.G.J.M.; De Bont, A.A.; Wallenburg, I. Nurses in the lead: A qualitative study on the development of distinct nursing roles in daily nursing practice. BMC Nurs. 2021, 20, 97. [Google Scholar] [CrossRef] [PubMed]
- González-Sánchez, R.; Pelechano-Barahona, E.; Alonso-Muñoz, S.; García-Muiña, F.E. Absorptive Routines and the Economic Impact of Incremental Innovations: Developing Continuous Improvement Strategies. J. Open Innov. Technol. Mark. Complex. 2020, 6, 167. [Google Scholar] [CrossRef]
- Estrada-Jimenez, L.A.; Pulikottil, T.; Peres, R.S.; Nikghadam-Hojjati, S.; Barata, J. Complexity theory and self-organization in Cyber-Physical Production Systems. Procedia CIRP 2021, 104, 1831–1836. [Google Scholar] [CrossRef]
- Albsoul, R.A.; FitzGerald, G.; Hughes, J.A.; Ahmed Alshyyab, M. Missed nursing care and complexity theory: A conceptual paper. J. Res. Nurs. 2021, 26, 809–823. [Google Scholar] [CrossRef]
- Rigtering, C.; Spaans, L.J.; de Jong, J.P. How to bridge the nurse innovation-diffusion gap? An in-depth case study of Create4Care. Front. Public Health 2023, 11, 1209965. [Google Scholar] [CrossRef]
- Zumstein-Shaha, M.; Grace, P.J. Competency frameworks, nursing perspectives, and interdisciplinary collaborations for good patient care: Delineating boundaries. Nurs. Philos. Int. J. Healthc. Prof. 2023, 24, e12402. [Google Scholar] [CrossRef]
- Keshavarz Mohammadi, N.; Rezaei, Z.; Burggraf, L.; Pype, P. Exploring settings as social complex adaptive systems in setting-based health research: A scoping review. Health Promot. Int. 2024, 39, daae001. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.L. A New Paradigm for Nurse Leader Decision-Making Within Complex Adaptive Systems. Nurs. Adm. Q. 2024, 48, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Borghmans, F.; Laletas, S. Complex adaptive phenomenology: A conceptual framework for healthcare research. J. Eval. Clin. Pract. 2023, 29, 756–764. [Google Scholar] [CrossRef] [PubMed]
- Burrows, K.E.; Abelson, J.; Miller, P.A.; Levine, M.; Vanstone, M. Understanding health professional role integration in complex adaptive systems: A multiple-case study of physician assistants in Ontario, Canada. BMC Health Serv. Res. 2020, 20, 365. [Google Scholar] [CrossRef] [PubMed]
- Yaroson, E.V.; Breen, L.; Hou, J.; Sowter, J. Advancing the understanding of pharmaceutical supply chain resilience using complex adaptive system (CAS) theory. Supply Chain Manag. Int. J. 2021, 26, 323–340. [Google Scholar] [CrossRef]
- Burke, C.M.; Morley, M.J. Toward a non-organizational theory of human resource management? A complex adaptive systems perspective on the human resource management ecosystem in (con) temporary organizing. Hum. Resour. Manag. 2023, 62, 31–53. [Google Scholar] [CrossRef]
- Ogden, K.; Kilpatrick, S.; Elmer, S. Examining the nexus between medical education and complexity: A systematic review to inform practice and research. BMC Med. Educ. 2023, 23, 494. [Google Scholar] [CrossRef]
- Whelan, J.; Fraser, P.; Bolton, K.A.; Love, P.; Strugnell, C.; Boelsen-Robinson, T.; Blake, M.R.; Martin, E.; Allender, S.; Bell, C. Combining systems thinking approaches and implementation science constructs within community-based prevention: A systematic review. Health Res. Policy Syst. 2023, 21, 85. [Google Scholar] [CrossRef]
- Dammery, G.; Ellis, L.A.; Churruca, K.; Mahadeva, J.; Lopez, F.; Carrigan, A.; Halim, N.; Willcock, S.; Braithwaite, J. The journey to a learning health system in primary care: A qualitative case study utilizing an embedded research approach. BMC Prim. Care 2023, 24, 22. [Google Scholar] [CrossRef]
- Conroy, T.; Pinero de Plaza, M.A.; Mudd, A.; Mitchell, M.; Kitson, A. Measuring fundamental care using complexity science: A descriptive case study of a methodological innovation. J. Clin. Nurs. 2023, 32, 2903–2912. [Google Scholar] [CrossRef]
- Bolous, N.S.; Graetz, D.E.; Ashrafian, H.; Barlow, J.; Bhakta, N.; Sounderajah, V.; Dowdeswell, B. Harnessing a clinician-led governance model to overcome healthcare tribalism and drive innovation: A case study of Northumbria NHS Foundation Trust. J. Health Organ. Manag. 2022, 37, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Sturmberg, J.P.; O’Halloran, D.M.; Martin, C.M. Understanding health system reform–a complex adaptive systems perspective. J. Eval. Clin. Pract. 2014, 20, 1087–1094. [Google Scholar] [CrossRef] [PubMed]
- Orem, D.E. Nursing: Concepts of Practice; Mosby: London, UK, 1991. [Google Scholar]
- Roy, C. Adaptation: A conceptual framework for nursing. Nurs. Outlook 1970, 18, 42–45. [Google Scholar]
- Chandler, J.; Rycroft-Malone, J.; Hawkes, C.; Noyes, J. Application of simplified Complexity Theory concepts for healthcare social systems to explain the implementation of evidence into practice. J. Adv. Nurs. 2016, 72, 461–480. [Google Scholar] [CrossRef] [PubMed]
- Meleis, A.I.; Sawyer, L.M.; Im, E.O.; Hilfinger Messias, D.K.; Schumacher, K. Experiencing transitions: An emerging middle-range theory. ANS Adv. Nurs. Sci. 2000, 23, 12–28. [Google Scholar] [CrossRef] [PubMed]
- Pype, P.; Mertens, F.; Helewaut, F.; Krystallidou, D. Healthcare teams as complex adaptive systems: Understanding team behaviour through team members’ perception of interpersonal interaction. BMC Health Serv. Res. 2018, 18, 570. [Google Scholar] [CrossRef]
- Walton, A.L.; McGee, K.; Padilla, B.I.; Wrigley, J.; Noonan, D.; Derouin, A.; Ledbetter, L.; Gonzalez-Guarda, R.M. An exploration of language: How nurses describe social factors that contribute to health. Nurs. Outlook 2023, 71, 101908. [Google Scholar] [CrossRef]
- Thompson, W.; Mcnamara, M. The advanced nurse practitioner in context: Systemic processes. J. Nurs. Scholarsh. 2023, 55, 886–897. [Google Scholar] [CrossRef]
- Chidi, R.; Adeniyi, A.O.; Okolo, C.A.; Babawarun, O.; Arowoogun, J.O. Psychological resilience in healthcare workers: A review of strategies and intervention. World J. Biol. Pharm. Health Sci. 2024, 17, 387–395. [Google Scholar] [CrossRef]
- Mrayyan, M.T.; Abunab, H.Y.; Abu Khait, A.; Rababa, M.J.; Al-Rawashdeh, S.; Algunmeeyn, A.; Abu Saraya, A. Competency in nursing practice: A concept analysis. BMJ Open 2023, 13, e067352. [Google Scholar] [CrossRef]
- Suciu, N.; Meliț, L.E.; Mărginean, C.O. A Holistic Approach of Personality Traits in Medical Students: An Integrative Review. Int. J. Environ. Res. Public Health 2021, 18, 12822. [Google Scholar] [CrossRef] [PubMed]
- Lyng, H.B.; Macrae, C.; Guise, V.; Haraldseid-Driftland, C.; Fagerdal, B.; Schibevaag, L.; Alsvik, J.G.; Wiig, S. Balancing adaptation and innovation for resilience in healthcare—A metasynthesis of narratives. BMC Health Serv. Res. 2021, 21, 759. [Google Scholar] [CrossRef] [PubMed]
- Stein Backes, D.; Gomes, R.C.C.; Rupolo, I.; Büscher, A.; da Silva, M.J.P.; Ferreira, C.L.L. Leadership in Nursing and Health Care in the Light of Complexity Thinking. Rev. Esc. Enferm. USP 2022, 56, e20210553. [Google Scholar] [CrossRef] [PubMed]
- Riaz, S.; Morgan, D.; Kimberley, N. Managing organizational transformation (OT) using complex adaptive system (CAS) framework: Future lines of inquiry. J. Organ. Change Manag. 2023, 36, 493–513. [Google Scholar] [CrossRef]
- Anderson, J.E.; Ross, A.J.; Macrae, C.; Wiig, S. Defining adaptive capacity in healthcare: A new framework for researching resilient performance. Appl. Ergon. 2020, 87, 103111. [Google Scholar] [CrossRef]
- Halabi, I.O.; Scholtes, B.; Voz, B.; Gillain, N.; Durieux, N.; Odero, A.; Baumann, M.; Ziegler, O.; Gagnayre, R.; Guillaume, M.; et al. “Patient participation” and related concepts: A scoping review on their dimensional composition. Patient Educ. Couns. 2020, 103, 5–14. [Google Scholar] [CrossRef]
- Song, Y.; Wang, Z.; Song, L.J. Going the extra mile for patients: Service-oriented high-performance work systems drive nurses’ job crafting and extra-role service behaviour. J. Adv. Nurs. 2024, 80, 3637–3652. [Google Scholar] [CrossRef]
- Montgomery, A.J.; Van der Doef, M.; Panagopoulou, E.; Leiter, M.P. Connecting Health Care Worker Well-Being, Patient Safety and Organizational Change: The Triple Challenge. Springer International Publishing: Cham, Switzerland, 2020; pp. 1–7. [Google Scholar]
- Salvatore, F.P.; Fanelli, S. Patient-Related Complexity of Care in Healthcare Organizations: A Management and Evaluation Model. Int. J. Environ. Res. Public Health 2020, 17, 3463. [Google Scholar] [CrossRef]
- Bloemhof, J.; Knol, J.; Van Rijn, M.; Buurman, B.M. The implementation of a professional practice model to improve the nurse work environment in a Dutch hospital: A quasi-experimental study. J. Adv. Nurs. 2021, 77, 4919–4934. [Google Scholar] [CrossRef]
- Papamichael, I.; Voukkali, I.; Loizia, P.; Pappas, G.; Zorpas, A.A. Existing tools used in the framework of environmental performance. Sustain. Chem. Pharm. 2023, 32, 101026. [Google Scholar] [CrossRef]
- Gonçalves, I.; Mendes, D.A.; Caldeira, S.; Jesus, É.; Nunes, E. The Primary Nursing Care Model and Inpatients’ Nursing-Sensitive Outcomes: A Systematic Review and Narrative Synthesis of Quantitative Studies. Int. J. Environ. Res. Public Health 2023, 20, 2391. [Google Scholar] [CrossRef] [PubMed]
- Ignatowicz, A.; Tarrant, C.; Mannion, R.; El-Sawy, D.; Conroy, S.; Lasserson, D. Organizational resilience in healthcare: A review and descriptive narrative synthesis of approaches to resilience measurement and assessment in empirical studies. BMC Health Serv. Res. 2023, 23, 376. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Notarnicola, I.; Lommi, M.; Ivziku, D.; Carrodano, S.; Rocco, G.; Stievano, A. The Nursing Theory of Complex Adaptive Systems: A New Paradigm for Nursing. Healthcare 2024, 12, 1997. https://doi.org/10.3390/healthcare12191997
Notarnicola I, Lommi M, Ivziku D, Carrodano S, Rocco G, Stievano A. The Nursing Theory of Complex Adaptive Systems: A New Paradigm for Nursing. Healthcare. 2024; 12(19):1997. https://doi.org/10.3390/healthcare12191997
Chicago/Turabian StyleNotarnicola, Ippolito, Marzia Lommi, Dhurata Ivziku, Sara Carrodano, Gennaro Rocco, and Alessandro Stievano. 2024. "The Nursing Theory of Complex Adaptive Systems: A New Paradigm for Nursing" Healthcare 12, no. 19: 1997. https://doi.org/10.3390/healthcare12191997
APA StyleNotarnicola, I., Lommi, M., Ivziku, D., Carrodano, S., Rocco, G., & Stievano, A. (2024). The Nursing Theory of Complex Adaptive Systems: A New Paradigm for Nursing. Healthcare, 12(19), 1997. https://doi.org/10.3390/healthcare12191997







