Development and Evaluation of Nursing Clinical Practice Education Using M-Learning
Abstract
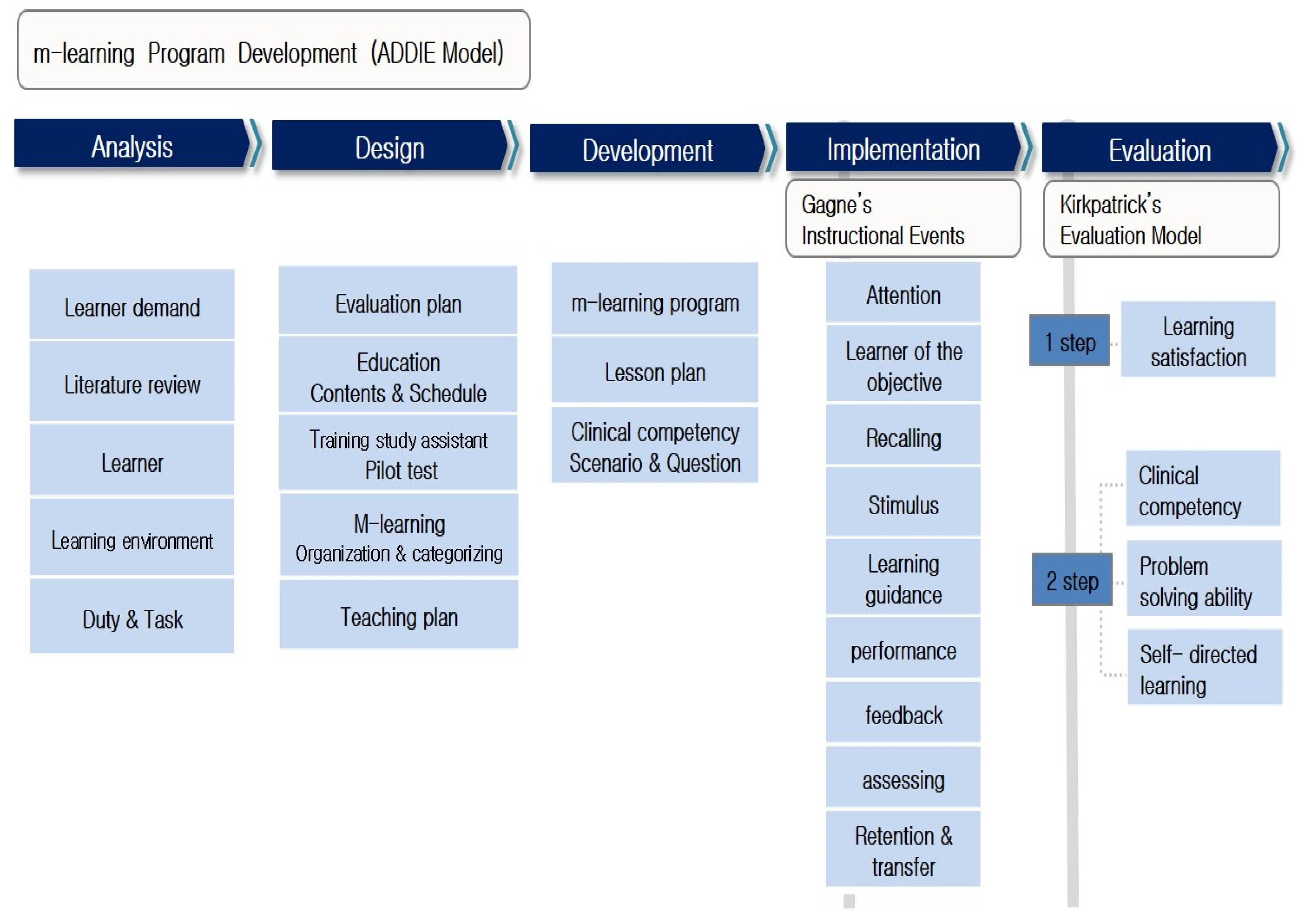
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Ethical Considerations
2.4. Measurements
2.4.1. Learning Satisfaction
2.4.2. Clinical Competency
2.4.3. Problem-Solving Ability
2.4.4. Self-Directed Learning
2.5. Development of Nursing Clinical Practice Education with M-Learning
2.5.1. Analysis
2.5.2. Design
2.5.3. Development
2.5.4. Implementation
2.5.5. Evaluation
2.6. Data Analysis
3. Results
3.1. Homogeneity Test for General Characteristics
3.2. Effects of Nursing Practice Education Using M-Learning
4. Discussion
4.1. Development of Nursing Education Using M-Learning
4.2. Effectiveness of the Nursing Practice Education Using M-Learning
4.3. Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Günay, U.; Kılınç, G. The transfer of theoretical knowledge to clinical practice by nursing students and the difficulties they experience: A qualitative study. Nurse Educ. Today 2018, 65, 81–86. [Google Scholar] [CrossRef]
- Carless-Kane, S.; Nowell, L. Nursing students learning transfer from classroom to clinical practice: An integrative review. Nurse Educ. Pract. 2023, 71, 103731. [Google Scholar] [CrossRef]
- Olaussen, C.; Aase, I.; Jelsness-Jørgensen, L.P.; Tvedt, C.R.; Steindal, S.A. Supplementing clinical practice in nursing homes with simulation training: A qualitative study of nursing students’ experiences. SAGE Open Nurs. 2020, 6, 2377960820981786. [Google Scholar] [CrossRef]
- Park, K.; Kim, J.K. Experience of incivility to nursing students during clinical practice. J. Korean Acad. Nurs. Adm. 2017, 23, 524–534. [Google Scholar] [CrossRef]
- Song, H.S.; Lim, S.H. A phenomenological study on the first clinical practice experience of nursing students. AJMAHS 2019, 9, 533–543. [Google Scholar] [CrossRef]
- Shin, S.; Tak, Y.R.; Song, R.; Kwon, S.; Song, J.; Kim, J.S. Improvement strategies for clinical nursing education to strengthen clinical competencies of nursing students: A focus group interview study. J. Qual. Res. 2022, 23, 104–116. [Google Scholar] [CrossRef]
- Willman, A.; Bjuresäter, K.; Nilsson, J. Insufficiently supported in handling responsibility and demands: Findings from a qualitative study of newly graduated nurses. J. Clin. Nurs. 2021, 30, 83–92. [Google Scholar] [CrossRef]
- Koukourikos, K.; Tsaloglidou, A.; Kourkouta, L.; Papathanasiou, I.V.; Iliadis, C.; Fratzana, A.; Panagiotou, A. Simulation in clinical nursing education. Acta Inform. Med. 2021, 29, 15–20. [Google Scholar] [CrossRef]
- Hashemiparast, M.; Negarandeh, R.; Theofanidis, D. Exploring the barriers of utilizing theoretical knowledge in clinical settings: A qualitative study. Int. J. Nurs. Sci. 2019, 6, 399–405. [Google Scholar] [CrossRef]
- Saifan, A.; Devadas, B.; Daradkeh, F.; Abdel-Fattah, H.; Aljabery, M.; Michael, L.M. Solutions to bridge the theory-practice gap in nursing education in the UAE: A qualitative study. BMC Med. Educ. 2021, 21, 490. [Google Scholar] [CrossRef]
- Gause, G.; Mokgaola, I.O.; Rakhudu, M.A. Technology usage for teaching and learning in nursing education: An integrative review. Curationis 2022, 45, e1–e9. [Google Scholar] [CrossRef]
- Suartama, I.K.; Setyosari, P.; Sulthoni, S.; Ulfa, S. Development of ubiquitous learning environment based on Moodle learning management system. Int. J. Interact. Mob. Technol. 2020, 14, 182–204. [Google Scholar] [CrossRef]
- Iivari, N.; Sharma, S.; Ventä-Olkkonen, L. Digital transformation of everyday life—How COVID-19 pandemic transformed the basic education of the young generation and why information management research should care? Int. J. Inf. Manag. 2020, 55, 102183. [Google Scholar] [CrossRef]
- Fawaz, M.A.; Hamdan-Mansour, A.M.; Tassi, A. Challenges facing nursing education in the advanced healthcare environment. Int. J. Afr. Nurs. Sci. 2018, 9, 105–110. [Google Scholar] [CrossRef]
- Shuja, A.; Qureshi, I.A.; Schaeffer, D.M.; Zareen, M. Effect of m-learning on students’ academic performance mediated by facilitation discourse and flexibility. Knowl. Manag. E-Learn. 2019, 11, 158–200. [Google Scholar] [CrossRef]
- Dennick, R. Constructivism: Reflections on twenty five years teaching the constructivist approach in medical education. Int. J. Med. Educ. 2016, 7, 200–205. [Google Scholar] [CrossRef]
- Dong, H.; Lio, J.; Sherer, R.; Jiang, I. Some learning theories for medical educators. Med. Sci. Educ. 2021, 31, 1157–1172. [Google Scholar] [CrossRef]
- Kang, M.; Yoon, H.; Kim, J.; Kim, H. Investigating the relationship among learning authenticity, learning motivation, and performance in web-based project learning. J. Educ. Technol. 2008, 24, 23–51. [Google Scholar] [CrossRef]
- Seo, Y.H. Development and Effect of Simulation Nursing Education Program Using the Outcome-Present State-Test (OPT) Model. Ph.D. Thesis, Mokpo National University, Mokpo, Republic of Korea, 28 February 2016. [Google Scholar]
- Lee, E.K. Evaluation of Internet-Based Distance Education System Operation. Master’s Thesis, Yonsei University, Seoul, Republic of Korea, 28 February 1999. [Google Scholar]
- Seong, K.Y. Effects of Practice Nursing Education: Using Standardized Patients on Subcutaneous Insulin Injection. Master’s Thesis, Eulji University, Daejeon, Republic of Korea, 28 February 2008. [Google Scholar]
- Lee, W.H.; Kim, J.J.; Yoo, J.S.; Hur, H.K.; Kim, K.S.; Lim, S.M. Development of clinical performance measurement tools for nursing students. J. Yonsei Coll. Nurs. 1990, 13, 17–29. [Google Scholar]
- Kwon, K.N. Clinical Competence, Critical Thinking Disposition and Self-Leadership of Nursing Students in a City. Master’s Thesis, Keimyung University, Daegu, Republic of Korea, 28 February 2014. [Google Scholar]
- Lee, J.S. The Effects of Process Behaviors on Problem Solving Performance on Various Tests. Ph.D. Thesis, University of Chicago, Chicago, IL, USA, 28 February 1978. [Google Scholar]
- Woo, O.H. The Effect of PBL(Problem-Based Learning) on the Problem Solving Process of Student by Their Meta-Cognitive Levels. Master’s Thesis, Korea National University of Education, ChungBuk, Republic of Korea, 2000. [Google Scholar]
- Lee, S.J.; Jang, Y.K.; Leem, H.N.; Park, K.Y. A Study on the Development of Life-Skills: Communication, Problem Solving, and Self-Directed Learning; Korean Educational Development Institute: Seoul, Republic of Korea, 2003; pp. 1–145. [Google Scholar]
- Branch, M.R. Instructional Design: The ADDIE Approach; Springer: New York, NY, USA, 2009; pp. 22–163. [Google Scholar]
- Gagné, R.M.; Briggs, L.J.; Wager, W.W. Principles of Instructional Design, 4th ed.; Harcourt Brace Jovanovich, College of Publishers: Forth Worth, TX, USA, 1992; pp. 1–356. [Google Scholar]
- Kim, S. Learning needs related to ubiquitous based learning in undergraduate nursing students for improvement of clinical practice ability: Focus group interview analysis. J. Daedong Coll. 2015, 22, 95–106. [Google Scholar]
- Kirkpatrick, D.L.; Kirkpatrick, J.D. Evaluating Training Programs: The Four Levels, 3rd ed.; Berrett-Koehler Publishers: Oakland, CA, USA, 2014; pp. 1–392. [Google Scholar]
- Ozkale, A.; Koc, M. Investigating academicians’ use of table PC from the perspectives of human computer interaction and technology acceptance model. Int. J. Technol. Educ. Sci. 2020, 4, 37–52. [Google Scholar] [CrossRef]
- Kim, J.H.; Park, H. Effects of smartphone-based mobile learning in nursing education: A systematic review and meta-analysis. Asian Nurs. Res. 2019, 13, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Haleem, A.; Javaid, M.; Qadri, M.A.; Suman, R. Understanding the role of digital technologies in education: A review. Sustain. Oper. Comput. 2022, 3, 275–285. [Google Scholar] [CrossRef]
- Miner, A.; Mallow, J.; Theeke, L.; Barnes, E. Using Gagne’s 9 events of instruction to enhance student performance and course evaluations in undergraduate nursing course. Nurse Educ. 2015, 40, 152–154. [Google Scholar] [CrossRef]
- Rajaguru, V.; Oh, J.; Im, M. Development and evaluation of the course on global health nursing for Indian nursing students. Int. J. Environ. Res. Public Health 2022, 19, 1978. [Google Scholar] [CrossRef]
- McNeill, L.; Fitch, D. Microlearning through the lens of Gagne’s nine events of instruction: A qualitative study. TechTrends 2023, 67, 521–533. [Google Scholar] [CrossRef]
- Lee, S.G.; Shin, Y.H. Effects of self-directed feedback practice using smartphone videos on basic nursing skills, confidence in performance and learning satisfaction. J. Korean Acad. Nurs. 2016, 46, 283–292. [Google Scholar] [CrossRef]
- Jang, S.; Suh, E.E. Development and application of a mobile-based multimedia nursing competency evaluation system for nursing students: A mixed-method randomized controlled study. Nurse Educ. Pract. 2022, 64, 103458. [Google Scholar] [CrossRef]
- Kim, S.J.; Shin, H.W.; Lee, J.E.; Kang, S.R.; Bartlett, R. A smartphone application to educate undergraduate nursing students about providing care for infant airway obstruction. Nurs. Educ. Tod. 2017, 48, 142–152. [Google Scholar] [CrossRef]
- Papastavrou, E.; Dimitriadou, M.; Tsangari, H.; Andreou, C. Nursing students’ satisfaction of the clinical learning environment: A research study. BMC Nurs. 2016, 19, 55. [Google Scholar] [CrossRef]
- Fernández-García, D.; Moreno-Latorre, E.; Giménez-Espert, M.D.C.; Prado-Gascó, V. Satisfaction with the clinical practice among nursing students using regression models and qualitative comparative analysis. Nurse Educ. Today 2021, 100, 104861. [Google Scholar] [CrossRef] [PubMed]
- Yeo, E.; Kim, J.B.; Han, S. Applying MOOC-based flipped learning to business education: Analysis of academic achievement and student satisfaction. Korea Bus. Rev. 2015, 19, 181–202. [Google Scholar] [CrossRef]
- Afrasiabifar, A.; Asadolah, M. Effectiveness of shifting traditional lecture to interactive lecture to teach nursing students. Investig. Educ. Enferm. 2019, 37, e07. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, L.M.; Kirkegaard, H.; Østergaard, L.G.; Bovbjerg, K.; Breinholt, K.; Maribo, T. Comparison of self-reported and performance-based measures of functional ability in elderly patients in an emergency department: Implications for selection of clinical outcome measures. BMC Geriatr. 2016, 16, 199. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, M.A.; Schlager, M.S. Discovery learning and transfer of problem-solving skills. Congr. Instr. 1990, 7, 129–159. [Google Scholar] [CrossRef]
- Gholami, M.; Changaee, F.; Karami, K.; Shahsavaripour, Z.; Veiskaramian, A.; Birjandi, M. Effects of multiepisode case-based learning (CBL) on problem-solving ability and learning motivation of nursing students in an emergency care course. J. Prof. Nurs. 2021, 37, 612–619. [Google Scholar] [CrossRef]
- Kang, J.; Seomun, G. Evaluating web-based nursing education’s effects: A systematic review and meta-analysis. West J. Nurs. Res. 2018, 40, 1677–1697. [Google Scholar] [CrossRef]
- O’Shea, E. Self-directed learning in nurse education: A review of the literature. J. Adv. Nurs. 2003, 43, 62–70. [Google Scholar] [CrossRef]
- Chen, B.; Yang, T.; Wang, Y.; Xiao, L.; Xu, C.; Shen, Y.; Qin, Q.; Wang, Y.; Li, C.; Chen, F.; et al. Nursing students’ attitudes toward mobile learning: An integrative review. Int. J. Nurs. Sci. 2021, 8, 477–485. [Google Scholar] [CrossRef]
- Park, E.H.; Hwang, S.Y. Development and effects of an e-learning program in operating room nursing for nursing students. J. Korean Acad. Nurs. 2011, 41, 36–46. [Google Scholar] [CrossRef]
- Shao, M.; Hong, J.C.; Zhao, L. Impact of the self-directed learning approach and attitude on online learning ineffectiveness: The mediating roles of internet cognitive fatigue and flow state. Front. Public Health 2022, 41, 927454. [Google Scholar] [CrossRef] [PubMed]
- Dhawan, S. Online learning: A panacea in the time of COVID-19 crisis. J. Educ. Technol. Syst. 2020, 49, 5–22. [Google Scholar] [CrossRef]
- Park, N. Exploring a new educational paradigm for the post COVID-19 era. Korean J. Elem. Educ. 2021, 32, 17–32. [Google Scholar] [CrossRef]
| Group | Intervention | Posttest | Intervention | Post-Test |
|---|---|---|---|---|
| Cont. | X1 | c1 | ||
| Exp. | X2 | e1 |
| Time | Usage of Tablet PC |
|---|---|
| Before clinical practice |
|
| In clinical practice |
|
| After clinical practice |
|
| Week | Program Title | Learning Content |
|---|---|---|
| 1st week |
|
|
| 2nd week |
|
|
| 3rd week |
|
|
| Stage | Instructional Events | Contents/Activities | |
|---|---|---|---|
| 1 | Gaining attention |
| |
| 2 | Informing the objectives |
| |
| 3 | Stimulation recall of prior learning |
| |
| 4 | Presenting stimuli with distinctive features |
| |
| 5 | Providing learning guidance | 1st week |
|
| 2nd week |
| ||
| 3rd week |
| ||
| 6 | Eliciting performance |
| |
| 7 | Providing informative feedback |
| |
| 8 | Assessing performance |
| |
| 9 | Enhancing retention and learning transfer |
| |
| Characteristics | Categories | Exp. (n = 21) | Con. (n = 21) | χ2 or t | p |
|---|---|---|---|---|---|
| n (%) or Mean (SD) | n (%) or Mean (SD) | ||||
| Gender | Female | 19 (90.5) | 21 (100.0) | 2.10 * | 0.488 |
| Male | 2 (9.5) | 0 (0.0) | |||
| Age (years) | ≦21 | 16 (76.2) | 11 (52.4) | 7.09 | 0.281 |
| ≧22 | 5 (23.8) | 10 (47.6) | |||
| Grades | ≧4.0 | 2 (9.5) | 3 (14.3) | 0.23 * | 1.00 |
| 3.0~3.9 | 18 (85.7) | 17 (81.0) | |||
| <3.0 | 1 (4.8) | 1 (4.8) | |||
| Adult nursing score | ≧90 | 6 (28.6) | 4 (19.0) | 1.07 * | 0.801 |
| 80~89 | 12 (57.1) | 12 (57.1) | |||
| 70~79 | 2 (9.5) | 4 (19.0) | |||
| 60~69 | 1 (4.8) | 1 (4.8) | |||
| Satisfaction with major of nursing | 6.10 ± 1.55 | 7.33 ± 2.22 | 2.10 | 0.052 | |
| Interest with major of nursing | 6.29 ± 1.49 | 6.91 ± 2.07 | 1.11 | 0.273 |
| Characteristics | Categories | Exp. (n = 21) | Con. (n = 21) | t | p |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | ||||
| Learning satisfaction | 3.98 (0.52) | 3.91 (0.59) | 0.37 | 0.711 | |
| Clinical competency | 2.87 (0.33) | 2.12 (0.32) | 7.44 | <0.001 | |
| Nursing process | 2.79 (0.45) | 2.06 (0.40) | 5.62 | <0.001 | |
| Nursing skill | 3.26 (0.41) | 2.11 (0.38) | 9.49 | <0.001 | |
| Cooperation | 2.46 (0.28) | 1.76 (0.49) | 5.73 | <0.001 | |
| Communication | 3.13 (0.49) | 2.62 (0.86) | 2.36 | 0.023 | |
| Professionalism | 2.68 (0.54) | 2.37 (0.27) | 2.39 | 0.022 | |
| Problem-solving ability | 3.74 (0.41) | 3.44 (0.43) | 2.28 | 0.028 | |
| Self-directed learning | 3.39 (0.44) | 3.18 (0.32) | 1.68 | 0.101 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.; Im, M. Development and Evaluation of Nursing Clinical Practice Education Using M-Learning. Healthcare 2024, 12, 206. https://doi.org/10.3390/healthcare12020206
Kim S, Im M. Development and Evaluation of Nursing Clinical Practice Education Using M-Learning. Healthcare. 2024; 12(2):206. https://doi.org/10.3390/healthcare12020206
Chicago/Turabian StyleKim, Sungeun, and Mihae Im. 2024. "Development and Evaluation of Nursing Clinical Practice Education Using M-Learning" Healthcare 12, no. 2: 206. https://doi.org/10.3390/healthcare12020206
APA StyleKim, S., & Im, M. (2024). Development and Evaluation of Nursing Clinical Practice Education Using M-Learning. Healthcare, 12(2), 206. https://doi.org/10.3390/healthcare12020206







