Identifying Witnessed Suicides in National Violent Death Reporting System Narratives
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Methods for Case Classification of Witnessed Suicide
2.2.1. Definition of Witnessed Suicide
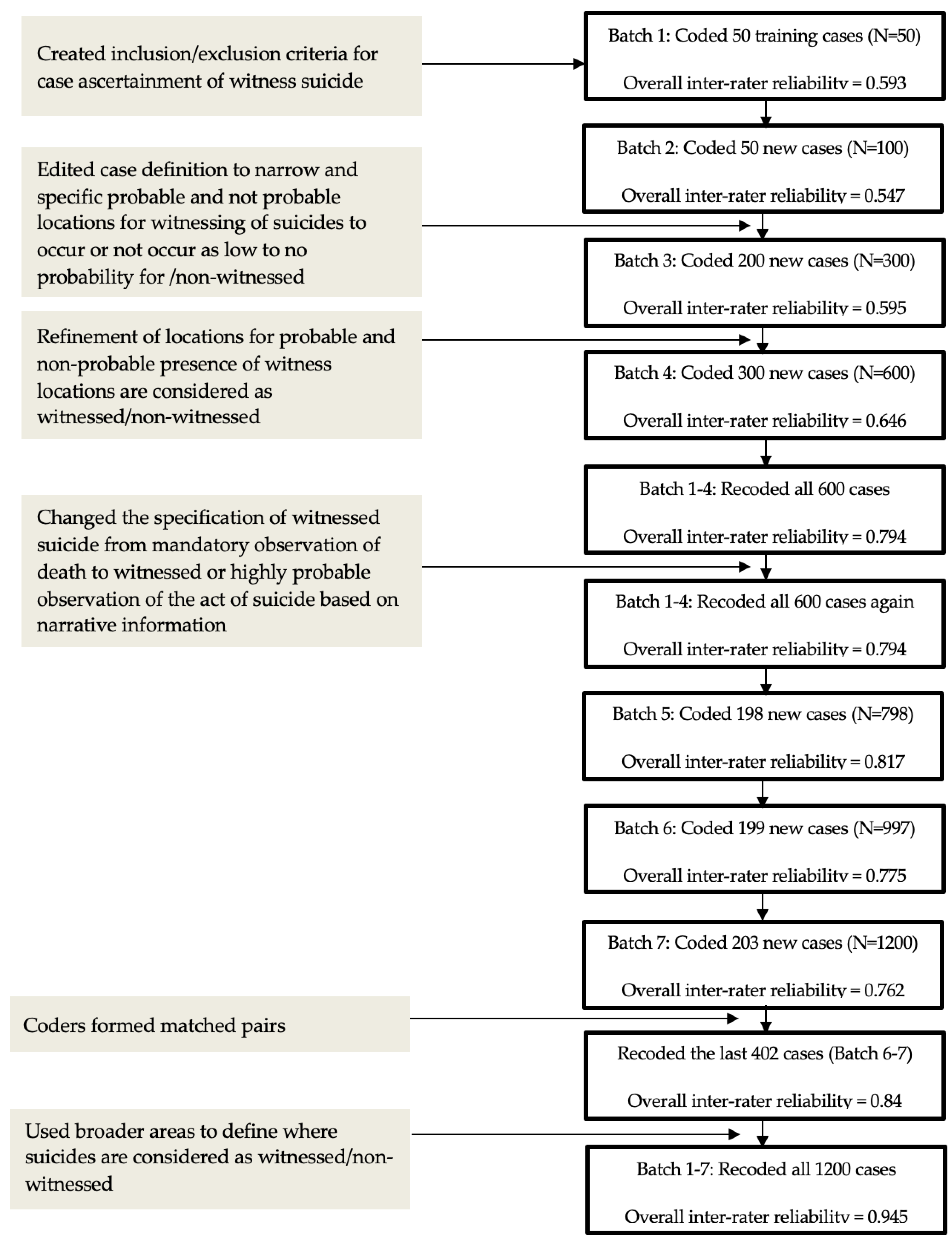
2.2.2. Coding Procedures and Inter-rater Agreement
2.2.3. Data Analytic Plan
3. Results
3.1. Decedent Characteristics of Witnessed Suicide
Additional Characteristics from Narratives
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Curtin, S.C.; Garnett, M.F.; Ahmad, F.B. Provisional numbers and rates of suicide by month and demographic characteristics: United States, 2021. Natl. Vital Stat. Rep. 2021, 24, 60–84. [Google Scholar]
- Cerel, J.; Brown, M.M.; Maple, M.; Singleton, M.; Van de Venne, J.; Moore, M.; Flaherty, C. How many people are exposed to suicide? Not six. Suicide Life Threat. Behav. 2019, 49, 529–534. [Google Scholar] [CrossRef]
- Meyer, C.; Irani, T.; Hermes, K.; Yung, B. Explaining Suicide: Patterns, Motivations, and What Notes Reveal; Academic Press: London, UK, 2017. [Google Scholar]
- Ooi, T.H.; Irani, T.H.; Hermes, K.A.; Meyer, C.L. Deconstructing witnessed suicide: A portrait of those who die by suicide in front of others. Curr. Psychol. 2020, 28, 6481–6489. [Google Scholar] [CrossRef]
- Andress, V.R.; Corey, D.M. Survivor-victims: Who discovers or witnesses suicide? Psychol. Rep. 1978, 42, 759–764. [Google Scholar] [CrossRef]
- Agjei, R.O.; Kolog, E.A.; Dei, D.; Tengey, Y.T. Emotional impact of suicide on active witnesses: Predicting with machine learning. Adv. Sci. Technol. Eng. Syst. J. 2018, 3, 501–509. [Google Scholar] [CrossRef]
- Dorpat, T.; Ripley, H.A.A. A study of suicide in the Seattle area. Compr. Psychiatry 1963, 4, 117–123. [Google Scholar] [CrossRef]
- McDowell, C.P.; Rothberg, J.M.; Koshes, R.J. Witnessed suicides. Suicide Life Threat. Behav. 1994, 24, 213–223. [Google Scholar] [CrossRef]
- Padosch, S.A.; Schmidt, P.H.; Madea, B. Planned complex suicide by self-poisoning and a manipulated blank revolver: Remarkable findings due to multiple gunshot wounds and self-made wooden projectiles. J. Forensic Sci. 2003, 48, 1371–1378. [Google Scholar] [CrossRef]
- Zhao, C.; Zou, Y.; Cao, L. Traumatic stress disorder in witnesses to a suicide. Chin. Ment. Health J. 2006, 20, 252–255. [Google Scholar]
- Limosin, F.; Loze, J.; Cothereau, C.; Beaurepaire, C.D.; Payan, C.; Conso, F.; Hautecouverture, S.; Rouillon, F. A prospective study of the psychological effects of “person under train” incident on drivers. J. Psychiatr. Res. 2006, 40, 755–761. [Google Scholar] [CrossRef]
- Cothereau, C.; Beaurepaire, C.D.; Payan, C.; Cambou, J.P.; Rouillon, F.; Conso, F. Professional and medical outcomes for French train drivers after “person under train” accidents: Three-year follow up study. Occup. Environ. Med. 2004, 61, 488–494. [Google Scholar] [CrossRef] [PubMed]
- PTSD, UK. Causes of PTSD: Witnessing a Suicide. n.d. Available online: https://www.ptsduk.org/causes-of-ptsd-witnessing-a-suicide/ (accessed on 10 January 2023).
- Van Hooff, M.; McFarlane, A.C.; Baur, J.; Abraham, M.; Barnes, D.J. The stressor Criterion-A1 and PTSD: A matter of opinion? J. Anxiety Disord. 2009, 23, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Shneidman, E.S. Postvention and the Survivor-Victim. In Deaths of Man; The New York Times Book Quadrangle: New York, NY, USA, 1973; pp. 33–41. [Google Scholar]
- Blaustein, M.; Fleming, A. Suicide from the Golden Gate Bridge. Am. J. Psychiatry 2009, 166, 1111–1116. [Google Scholar] [CrossRef] [PubMed]
- Cantor, C.H.; Hill, M.A.; McLachlan, E.K. Suicide and related behaviour from river bridges. Br. J. Psychiatry 1989, 155, 829–835. [Google Scholar] [CrossRef] [PubMed]
- de Moore, G.M.; Robertson, A.R. Suicide attempts by firearms and by leaping from heights: A comparative study of survivors. Am. J. Psychiatry 1999, 156, 1425–1431. [Google Scholar] [CrossRef]
- San Too, L.; Milner, A.; Bugeja, L.; McClure, R. The socio-environmental determinants of railway suicide: A systematic review. BMC Public Health 2014, 14, 20. [Google Scholar] [CrossRef]
- Guggenheim, F.G.; Weisman, A.D. Suicide in the subway: Publicly witnessed attempts of 50 cases. J. Nerv. Ment. Dis. 1972, 155, 404–409. [Google Scholar] [CrossRef]
- Mishara, B.L.; Bardon, C.; Dupont, S. Can CCTV identify people in public transit stations who are at risk of attempting suicide? An analysis of CCTV video recordings of attempters and a comparative investigation. BMC Public Health 2016, 16, 1245. [Google Scholar] [CrossRef]
- Lukaschek, K.; Baumert, J.; Ladwig, K.H. Behaviour patterns preceding a railway suicide: Explorative study of German federal police officers’ experiences. BMC Public Health 2011, 11, 620. [Google Scholar] [CrossRef]
- Mackenzie, J.; Borrill, J.; Hawkins, E.; Fields, B.; Kruger, I.; Noonan, I.; Marzano, L. Behaviours preceding suicides at railway and underground locations: A multimethodological qualitative approach. BMJ Open 2018, 8, e021076. [Google Scholar] [CrossRef]
- Lyons, B.H.; Walters, M.L.; Jack, S.P.D.; Petrosky, E.; Blair, J.M.; Ivey-Stephenson, A.Z. Suicides among lesbian and gay male individuals: Findings from the National Violent Death Reporting System. Am. J. Prev. Med. 2019, 56, 512–521. [Google Scholar] [CrossRef]
- Arseniev-Koehler, A.; Cochran, S.; Mays, V.; Chang, K.; Foster, J.G. Integrating topic modeling and word embedding to characterize violent deaths. Proc. Natl. Acad. Sci. USA 2022, 119, e2108801119. [Google Scholar] [CrossRef] [PubMed]
- Paulozzi, L.J.; Mercy, J.; Frazier, L.; Annest, J.L. CDC’s National Violent Death Reporting System: Background and methodology. Inj. Prev. 2004, 10, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. National Violent Death Reporting System (NVDRS). CDC. 2021. Available online: https://www.cdc.gov/violenceprevention/datasources/nvdrs/index.html (accessed on 10 January 2023).
- Blair, J.P.; Schweit, K.W. A Study of Active Shooter Incidents, 2000–2013; Texas State University; Federal Bureau of Investigation, U.S. Department of Justice: Washington, DC, UA, 2014. Available online: https://www.fbi.gov/file-repository/active-shooter-study-2000-2013-1.pdf/view (accessed on 10 January 2023).
- Fleiss, J.L.; Cohen, J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ. Psychol. Meas. 1973, 33, 613–619. [Google Scholar] [CrossRef]
- Gamer, M.; Lemon, J.; Fellows, I.; Singh, P. irr: Various Coefficients of Inter-rater Reliability and Agreement. R Package Version 0.84.1. 2019. Available online: https://CRAN.R-project.org/package=irr (accessed on 24 August 2023).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 10 December 2022).
- Jakab, I.; Howard, M.C. Art therapy with a 12-year-old girl who witnessed suicide and developed school phobia. Psychother. Psychosom. 1969, 17, 309–324. [Google Scholar] [CrossRef] [PubMed]
- Van Orden, K.A.; Witte, T.K.; Cukrowicz, K.C.; Braithwaite, S.; Selby, E.A.; Joiner, T.E. The Interpersonal Theory of Suicide. Psychol. Rev. 2010, 117, 575–600. [Google Scholar] [CrossRef] [PubMed]
- Aparicio-Garcia, M.E.; Diaz-Ramiro, E.M.; Rubio-Valdehita, S.; Lopez-Nunez, M.I.; Garcia-Nieto, I. Protective factors, risk of violence and discrimination and mental health indicators of young LGB people. Int. J. Environ. Res. Public Health 2022, 19, 14401. [Google Scholar] [CrossRef]
- Fraser, B.; Pierse, N.; Chisholm, E.; Cook, H. LGBTIQ+ Homelessness: A Review of the Literature. Int. J. Environ. Res. Public Health 2019, 16, 2677. [Google Scholar] [CrossRef]
- Ormiston, C.K. LGBTQ Youth Homelessness: Why We Need to Protect Our LGBTQ Youth. LGBT Health 2022, 9, 217–221. [Google Scholar] [CrossRef]
- Mays, V.M.; Cochran, S.D. Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. AJPH 2001, 91, 1869–1876. [Google Scholar] [CrossRef]
- Gmelin, J.H.; Vries, Y.A.D.; Baams, L.; Aguilar-Gaxiola, S.; Alonso, J.; Borges, G.; Bunting, B.; Cardoso, G.; Florescu, S.; Gureje, O.; et al. Increased risks for mental disorders among LGB individuals: Cross-national evidence from the World Mental Health Surveys. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 2319–2332. [Google Scholar] [CrossRef] [PubMed]
- Hedegaard, H.; Curtin, S.C.; Warner, M. Suicide rates in the United States continue to increase. In NCHS Data Brief; National Center for Health Statistics: Hyattsville, MD, USA, 2018. [Google Scholar]
- Pettrone, K.; Curtin, S.C. Urban-rural differences in suicide rates, by sex and three leading methods: United States, 2000–2018. In NCHS Data Brief; National Center for Health Statistics: Hyattsville, MD, USA, 2020; pp. 1–8. [Google Scholar] [PubMed]
- Wasserman, I.M.; Stack, S. Lethal locations: An application of opportunity theory to motel suicide, a research note. Death Stud. 2008, 32, 757–767. [Google Scholar] [CrossRef] [PubMed]
- Mishara, B.L. Railway and metro suicides: Understanding the problem and prevention potential. Crisis 2007, 28, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Weisman, A.D.; Worden, W. Risk-rescue rating in suicide assessment. Arch. Gen. Psychiatry 1972, 26, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Zarkowski, P.; Avery, D. Hotel room suicide. Suicide Life Threat. Behav. 2011, 36, 578–581. [Google Scholar] [CrossRef]
- Lyra, R.L.; McKenzie, S.K.; Every-Palmer, S.; Jenkin, G. Occupational exposure to suicide: A review of research on the experiences of mental health professionals and first responders. PLoS ONE 2021, 16, e0251038. [Google Scholar] [CrossRef] [PubMed]
- Hom, M.A.; Stanley, I.H.; Spencer-Thomas, S.; Joiner, T.E. Exposure to suicide and suicide bereavement among women firefighters: Associated suicidality and psychiatric symptoms. J. Clin. Psychol. 2018, 74, 2219–2237. [Google Scholar] [CrossRef]
- Greenleaf, C. New Approaches to Helping the Witness to A Suicide: The Suicide Witness Survivor Outreach Program of NAMI New Hampshire. Available online: https://theconnectprogram.org/wp-content/uploads/2018/11/witnesssurvivor-final.pdf (accessed on 23 August 2023).
- Witnesses—Support after Suicide. Available online: https://supportaftersuicide.org.uk/i-didnt-know-the-person/ (accessed on 23 August 2023).
- Cerel, J.; Maple, M.; van de Venne, J.; Moore, M.; Flaherty, C.; Brown, M. Exposure to Suicide in the Community: Prevalence and Correlates in One U.S. State. Public Health Rep. 2016, 131, 100–107. [Google Scholar] [CrossRef]
- Harper, C.R. Witnessing Community Violence, Gun Carrying, and Associations with Substance Use and Suicide Risk Among High School Students—Youth Risk Behavior Survey, United States, 2021. MMWR Suppl. 2023, 72, 22–28. [Google Scholar] [CrossRef]
- Robb, A. How A Public Suicide Harms the People Who See It. Available online: https://www.theatlantic.com/health/archive/2018/05/witnessing-stranger-suicide/561257/ (accessed on 23 August 2023).
- Bardon, C.; Dargis, L.; Mishara, B. Evaluation of the implementation of a railway critical incident management and support protocol to help train drivers cope with accidents and suicides. J. Occup. Environ. Med. 2021, 63, e495–e504. [Google Scholar] [CrossRef]
| [Witnessed/Non-Witnessed Suicide] | |
|---|---|
| Code type | (1, Witnessed Suicide) (0, Non-Witnessed Suicide) |
| Definition | A witnessed suicide occurs when the victim (V) suicides in a location where an individual or individuals see(s), or is highly likely to see, the V suicide. |
| When to code presence of [witnessed suicide] | Suicide was mentioned to be observed by others. Location/manner of death suggests that one or more people had a high probability of observing the V suicide. |
| Examples of PRESENCE of [witnessed suicide] |
|
| When to code absence of [witnessed suicide—case of non-witnessed] | Mention of finding the V after a prolonged period of time after suicide. Any mention of hearing the act or being in close proximity without actually observing the V commit suicide. |
| Examples of ABSENCE of [witnessed suicide—case of non-witnessed] | Decedent was already deceased:
|
| Specific notes: Non-witnessed: Suicide occurs where another individual cannot, or has a low likelihood, of seeing the event take place, regardless of whether or not others can hear the suicide. Witnessed suicide does not have to be an abrupt death like jumping off a building, walking into traffic, or self-inflicted gunshot wounds. Overdosing, drinking poison, etc., in front of another person qualifies as a witnessed suicide. When coding for witnessed suicide, ask: “Did the V suicide in a location where there is a high possibility of being seen by another individual(s)?” regardless of whether the narrative states the suicide was unwitnessed. Witnessed Suicide Location Criteria Commerce Presence: Areas open to the public Absence: Areas open only to employees Education Presence: Areas open to the public Absence: Private rooms House of Worship Presence: Areas open to the public Absence: Areas only open to employees Open Space Presence: High exposure/unobstructed Absence: Low exposure/obstructed Government Buildings Presence: Areas open to the public Absence: Areas only open to employees Residence Non-communal space Presence: Another person is reported to have seen the suicide Absence: No witnesses reported Communal space Presence: Location exposed to shared areas Absence: Unexposed to shared areas Healthcare Presence: Areas open to the public Absence: Private rooms | |
| Witnessed Suicide (n = 125) | Non-Witnessed Suicide (n = 1075) | Cramer’s V | Chi-Squared Statistic | p-Value | |||
|---|---|---|---|---|---|---|---|
| Frequency | Percent (%) | Frequency | Percent (%) | ||||
| Sex | |||||||
| Male | 92 | 73.6 | 782 | 72.7 | 0.006 | 0.009 | 0.922 |
| Female | 33 | 26.4 | 293 | 27.3 | |||
| Age *** | |||||||
| 0–17 | 7 | 5.6 | 60 | 5.6 | 0.128 | 19.503 | <0.001 |
| 18–25 | 24 | 19.2 | 172 | 16.0 | |||
| 26–44 | 62 | 49.6 | 356 | 33.1 | |||
| 45–64 | 24 | 19.2 | 359 | 33.4 | |||
| 65+ | 8 | 6.4 | 128 | 11.9 | |||
| Sexual orientation | |||||||
| Straight/heterosexual | 6 | 4.8 | 47 | 4.4 | 0.069 | 5.741 | 0.057 |
| Gay/lesbian/bisexual | 47 | 37.6 | 297 | 27.6 | |||
| Unknown | 72 | 57.6 | 731 | 68.0 | |||
| Transgender | |||||||
| Yes | 5 | 4.0 | 48 | 4.5 | 0.007 | < 0.001 | 0.992 |
| No | 120 | 96.0 | 1027 | 95.5 | |||
| Race and ethnicity * | |||||||
| White, non-Hispanic | 92 | 73.6 | 888 | 82.6 | 0.081 | 7.927 | 0.048 |
| Black or African American, non-Hispanic | 12 | 9.6 | 63 | 5.9 | |||
| Hispanic | 14 | 11.2 | 66 | 6.1 | |||
| Other | 7 | 5.6 | 58 | 5.4 | |||
| Highest level of education | |||||||
| High school or less | 56 | 44.8 | 420 | 39.1 | 0.057 | 3.881 | 0.422 |
| Some college | 25 | 20.0 | 223 | 20.7 | |||
| Four-year college degree | 7 | 5.6 | 104 | 9.7 | |||
| Graduate study | 8 | 6.4 | 51 | 4.7 | |||
| Unknown | 29 | 23.2 | 277 | 25.8 | |||
| Marital status | |||||||
| Never married | 74 | 59.2 | 522 | 48.6 | - | - | 0.158 |
| Married/civil union/domestic partnership | 25 | 20.0 | 268 | 24.9 | |||
| Formerly married (Widowed/divorced/married, but separated) | 24 | 19.2 | 247 | 23.0 | |||
| Unknown/single not otherwise specified | 2 | 1.6 | 38 | 3.5 | |||
| Ever served in the U.S. armed forces | |||||||
| Yes | 10 | 8.0 | 156 | 14.5 | 0.058 | 3.456 | 0.063 |
| No/unknown | 115 | 92.0 | 919 | 85.5 | |||
| Homeless ** | |||||||
| Yes | 5 | 4.0 | 8 | 0.7 | 0.096 | 8.247 | 0.004 |
| No/unknown | 120 | 96.0 | 1067 | 99.3 | |||
| Recently released from or admitted to an institutional setting (added to NVDRS in August 2013) | |||||||
| Yes | 8 | 6.4 | 50 | 4.6 | 0.025 | 0.413 | 0.521 |
| No/unknown | 117 | 93.6 | 1025 | 95.4 | |||
| Primary weapon type/means *** | |||||||
| Various methods | 40 | 32.0 | 408 | 38.0 | - | - | <0.001 |
| Fall | 29 | 23.2 | 2 | 0.2 | |||
| Gun-related | 53 | 42.4 | 452 | 42.0 | |||
| Poisoning | 3 | 2.4 | 213 | 19.8 | |||
| Location type *** | |||||||
| Commercial space of businesses | 4 | 3.2 | 45 | 4.2 | - | - | <0.001 |
| Living space | 56 | 44.8 | 827 | 76.9 | |||
| Public, open space | 42 | 33.6 | 87 | 8.1 | |||
| Supervised public space | 5 | 4.0 | 23 | 2.1 | |||
| Transportation | 14 | 11.2 | 40 | 3.7 | |||
| Other/unknown | 4 | 3.2 | 53 | 4.9 | |||
| Alcohol use suspected | |||||||
| Yes | 31 | 24.8 | 236 | 22.0 | 0.021 | 0.373 | 0.542 |
| No/not applicable/unknown | 94 | 75.2 | 839 | 78.0 | |||
| Blood alcohol content | |||||||
| 0.08% or above | 21 | 16.8 | 139 | 12.9 | 0.045 | 2.389 | 0.303 |
| Between 0.01% & 0.08% | 11 | 8.8 | 73 | 6.8 | |||
| Below the detection limit of the test (<0.01% or non-detectable/not applicable, no testing/unknown | 93 | 74.4 | 863 | 80.28 | |||
| Marijuana result * | |||||||
| Present | 14 | 11.2 | 63 | 5.9 | 0.067 | 4.465 | 0.035 |
| Not present/not applicable/unknown | 111 | 88.8 | 1012 | 94.1 | |||
| Opiate result | |||||||
| Present | 9 | 7.2 | 134 | 12.5 | 0.050 | 2.477 | 0.116 |
| Not present/not applicable/unknown | 116 | 92.8 | 941 | 87.5 | |||
| Financial problems appear to have contributed to the death | |||||||
| Yes | 8 | 6.4 | 120 | 11.2 | 0.047 | 2.189 | 0.139 |
| No | 117 | 93.6 | 955 | 88.8 | |||
| Predictor | AOR | 95% CI |
|---|---|---|
| Sex | ||
| Male | - | - |
| Female | 0.95 | 0.55–1.66 |
| Age * | ||
| 0–17 | - | - |
| 18–25 | 0.73 | 0.25–2.11 |
| 26–44 | 1.06 | 0.38–3.00 |
| 45–64 | 0.35 | 0.11–1.15 |
| 65+ | 0.54 | 0.14–2.15 |
| Sexual orientation ** | ||
| Unknown/not coded | - | - |
| Gay/lesbian/bisexual | 2.27 | 1.30–3.97 |
| Straight/heterosexual | 2.51 | 0.89–7.05 |
| Transgender | ||
| No | - | - |
| Yes | 0.61 | 0.17–2.12 |
| Race and ethnicity | ||
| White, non-Hispanic | - | - |
| Black or African American, non-Hispanic | 1.51 | 0.67–3.42 |
| Hispanic | 1.51 | 0.68–3.37 |
| Other | 0.89 | 0.31–2.55 |
| Highest level of education | ||
| High school or less | - | - |
| Some college | 0.49 | 0.24–0.99 |
| Four-year college degree | 0.36 | 0.12–1.08 |
| Graduate study | 1.55 | 0.57–4.22 |
| Unknown | 0.87 | 0.48–1.59 |
| Marital status | ||
| Never married | - | - |
| Married/civil union/domestic partnership | 1.48 | 0.75–2.92 |
| Formerly married (widowed/divorced/married, but separated) | 1.45 | 0.73–2.90 |
| Unknown/single not otherwise specified | 0.46 | 0.09–2.33 |
| Ever served in the U.S. Armed Forces | ||
| No/unknown | - | - |
| Yes | 0.74 | 0.33–1.67 |
| Homeless ** | ||
| No/unknown | - | - |
| Yes | 8.01 | 1.94–33.09 |
| Recently released from or admitted to an institutional setting (added August 2013) | ||
| No/unknown | - | - |
| Yes | 1.05 | 0.37–2.97 |
| Primary weapon type/means *** | ||
| Various methods | - | - |
| Fall | 323.04 | 62.08–1680.83 |
| Gun-related | 1.61 | 0.95–2.74 |
| Poisoning | 0.15 | 0.04–0.54 |
| Location type *** | ||
| Commercial space of businesses | ||
| Living space | 0.93 | 0.22–3.99 |
| Public, open space | 8.41 | 1.88–37.62 |
| Supervised public space | 3.72 | 0.56–24.87 |
| Transportation | 6.60 | 1.28–33.99 |
| Other/unknown | 0.87 | 0.13–5.97 |
| Alcohol use suspected | ||
| No/not applicable/unknown | - | - |
| Yes | 1.45 | 0.74–2.82 |
| Blood alcohol content | ||
| Below the detection limit of the test (<0.01% or Non-detectable/not applicable, no testing/unknown | - | - |
| Between 0.01–0.08% | 1.53 | 0.62–3.73 |
| 0.08% or above | 1.75 | 0.80–3.81 |
| Marijuana result ** | ||
| Not present/not applicable/unknown | - | - |
| Present | 3.41 | 1.58–7.36 |
| Opiate result | ||
| Not present/not applicable/unknown | - | - |
| Present | 0.78 | 0.29–2.06 |
| Financial problems appear to have contributed to the death | ||
| No | - | - |
| Yes | 0.55 | 0.22–1.34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mays, V.M.; Gareeb, M.; Zhang, X.; Nguyen, V.; Rosenberg, J.; Lin, Y.; Arseniev-Koehler, A.; Eliav, A.; Foster, J.G.; Baumgardner, M.; et al. Identifying Witnessed Suicides in National Violent Death Reporting System Narratives. Healthcare 2024, 12, 209. https://doi.org/10.3390/healthcare12020209
Mays VM, Gareeb M, Zhang X, Nguyen V, Rosenberg J, Lin Y, Arseniev-Koehler A, Eliav A, Foster JG, Baumgardner M, et al. Identifying Witnessed Suicides in National Violent Death Reporting System Narratives. Healthcare. 2024; 12(2):209. https://doi.org/10.3390/healthcare12020209
Chicago/Turabian StyleMays, Vickie M., Mikaela Gareeb, Xingruo Zhang, Vivian Nguyen, Joelle Rosenberg, Yuri Lin, Alina Arseniev-Koehler, Adam Eliav, Jacob Gates Foster, Mika Baumgardner, and et al. 2024. "Identifying Witnessed Suicides in National Violent Death Reporting System Narratives" Healthcare 12, no. 2: 209. https://doi.org/10.3390/healthcare12020209
APA StyleMays, V. M., Gareeb, M., Zhang, X., Nguyen, V., Rosenberg, J., Lin, Y., Arseniev-Koehler, A., Eliav, A., Foster, J. G., Baumgardner, M., & Cochran, S. D. (2024). Identifying Witnessed Suicides in National Violent Death Reporting System Narratives. Healthcare, 12(2), 209. https://doi.org/10.3390/healthcare12020209







