Abstract
Background: Dysmenorrhea and premenstrual syndrome (PMS) are common disorders in the Mexican population, but these are usually underdiagnosed and under-treated, impacting women’s quality of life. Adequate health habits have been reported as precursors of decreasing dysmenorrhea symptoms. However, few studies assess their impact on PMS. Aim: This study aims to evaluate dysmenorrhea and premenstrual syndrome in association with health habits in the Mexican population. Methods: To assess the impact of health habits on menstruation symptoms a validated survey was conducted in 1679 adult females aged ≥18 years. The survey collected data on participants’ dysmenorrhea, PMS, and their health habits. Results: The analysis showed that physical activity duration, changes in eating habits (increases in salty or sugary foods) during menstruation, and oversleeping habits predict increases in dysmenorrhea and PMS. In contrast, an active sexual life, relaxing physical activity, and adequate sleep hours during menstruation seem to decrease the symptoms. Conclusions: We conclude that adequate health habits and addressing early gynecological conditions might regulate dysmenorrhea and PMS.
1. Introduction
Dysmenorrhea is the most common gynecological disorder in reproductive age and is becoming a health problem worldwide [1] because the condition leads to absence from work or academic activities, impairing women’s quality of life and their life plans. Despite its common occurrence, dysmenorrhea is underdiagnosed and under-treated [2]. This disorder entails recurrent pain, with characteristics of deregulated somatosensory processing of the central nervous system CNS [3], severe abdominal spasms and cramps, heavy menstrual flow, nulliparity, anxiety, depression, problems in sexual functioning [4,5], headaches, backaches, dizziness, irritability, breast tenderness, swelling of extremities, diarrhea, and nausea [6].
The symptoms and signs differ for each woman; previous studies have classified these pain symptoms between 0 and 3, with 3 representing the most severe pain [7], characterized by non-responsiveness to analgesics. Moreover, the severity of symptoms of dysmenorrhea positively correlated with the age of menarche, the regularity of the menstrual period, and the duration and amount of menstrual flow [4,8].
There are two types of dysmenorrhea: primary and secondary. Primary dysmenorrhea or pain during menstruation, in the absence of pelvic pathology, is a common disease characterized by pain before and after the menstrual period; this dysmenorrhea has been reported as genetically influenced, while secondary dysmenorrhea entails a pathological condition with an anatomical problem, for example, endometriosis. The pain typically lasts from 8 to 72 h, with most severity on the 1st and 2nd days of menstruation because of the increased release of prostaglandins during this period [9]. In general, menstrual symptoms have been classified into menstrual-related diagnoses such as dysmenorrhea or PMS. Dysmenorrhea is more related to the symptoms of pain accompanying menses, while PMS is generally related to emotional or psychological concerns [4].
On the other hand, inappropriate dietary habits, low physical activity, and poor sleeping habits have been reported as precursors of menstrual disorders [1,10]. Interestingly, prior studies reported that breakfast or meal skipping predicts female gynecologic disorders [7,10]. Additionally, multiple studies reported that certain nutrient intake, such as fatty acids, antioxidants, the combination of vitamins and minerals [11], consumption of fruits, vegetables, fish, milk, and dairy products, low amounts of consumed salt [7], low frequency of drinking coffee [8], the Mediterranean diet [6], and a lower amount of consumed kilocalories [12], positively affects dysmenorrhea symptoms [6,7,8,10,11,12].
Prior studies have associated high-level physical activity with a reduction in dysmenorrhea severity [12]. They explain this association as physical activity decreasing levels of C-reactive protein (HsCRP), PGE2, and PGF2α, resulting in the amelioration of uterine contraction and inflammation [12,13]. Previous studies in the Mexican population also reported that relaxation exercises induced by physiotherapy seem to decrease symptoms of primary dysmenorrhea [14], while in other populations, relaxation exercises improve menstrual pain and quality of life [15,16,17,18].
Multiple studies reviewed the relationship between sleep and menstrual disturbances. PMS and dysmenorrhea were associated with sleep disturbances such as sleep quality, daytime sleepiness, difficulty initiating/maintaining sleep, and duration. Abnormal menstrual cycles and heavy bleeding were related to sleep quality and difficulty initiating/maintaining sleep [19], while sleeping less than five hours increased PMS [20].
In Mexico, the prevalence of dysmenorrhea is high, and 62.4% of women suffer severe pain, as measured by the Visual Analog Scale (VAS) [21]. Moreover, a high percentage of the Mexican population does not have access to formal medical care or pharmacologic treatment [21]. Therefore, women use strategies of self-medication and alternative therapies to respond to dysmenorrhea symptoms [22]. However, for between 28% and 90% of Mexican women, the pain is often not relieved despite the use of medication [21,23,24,25,26]. Therefore, the focus on health habits is a useful approach for understanding how non-medical interventions could play a role in managing dysmenorrhea symptoms.
Recent studies report that Mexican women show an inability to participate in daily activities (1–6 menstrual cycles per year), require incapacitation (6–24 h per cycle), and have school absenteeism (1–13 menstrual cycles per year) [23]. Additionally, another study suggests that menstrual pain affects Mexican women´s academic achievement due to absenteeism [27].
Although there are no previous studies assessing dysmenorrhea effect on the Mexican economy, previous studies in the US reported that absenteeism due to dysmenorrhea symptoms generates 600 million work hours resulting in a loss of 2 billion USD per year. We suggest a similar situation in the Mexican economy.
Additionally, between 78% and 90% of the Mexican population prefers sweetie beverages and fast food with high amounts of saturated fat and added sugar. Moreover, their legumes, fruits, and vegetables consumption is low, between 6.3 and 8.2% lower than that recommended by the Food and Agriculture Organization (FAO) [28]. Therefore, this exploratory study pretends to analyze retrospectively whether dietary habits, physical activity, and sleeping habits affect dysmenorrhea symptoms and PMS. We would expect more acute dysmenorrhea symptoms and more severe PMS associated with inappropriate health habits.
2. Material and Methods
2.1. Participants
This cross-sectional study was conducted on 1679 females (See Table 1), all of them were enrolled online from 2022 to 2023 (statistical power = 0.79). They were ethnic Mexican and native Spanish speakers and had at least six years of education. We included participants who completed the survey and signed the consent for participation. We excluded from our cohort those who reported suffering from endometriosis or cancer. All volunteers were informed of their rights and provided written informed consent for participation in this study. This research was carried out ethically and was approved by the Benemérita Universidad Autónoma de Puebla.

Table 1.
Demographic and anthropometric data.
2.2. Procedure
The data were obtained from a self-administered survey directed at females over 18 years, who reported at least their first menarche. The survey assesses participants’ dysmenorrhea symptoms, PMS, and health habits. This survey entails one hundred and twenty-two items distributed in five sections: (1) identification data; (2) anthropometric data; (3) symptoms of dysmenorrhea and PMS index (See Table 2); (4) health habits: dietary habits, physical activity, and sleep habits; and (5) Other habits (See Table 2).

Table 2.
Symptoms of dysmenorrhea and PMS index.
2.3. Validation
The statistical analysis for the survey’s validation was performed using a chi-square test. The factor analysis technique assessed the items with an orthogonal rotation, “Varimax”. In this analysis, the factor weight of each item was at least 0.4. We also measured the internal consistency of each item for each factor, exploring their reliability using Cronbach’s alpha (0.724). The participants reported being comfortable with all items and completion times and responded 100% to the survey (See survey in Appendix A).
2.4. Data Analysis Methods
2.4.1. Distribution Analysis of Health Habits
We compared the symptoms of dysmenorrhea and PMS index between participants with different dietary habits (adequate (AD) versus inadequate (ID)), physical activity (passive (PA) versus active (AA) during menstruation), and sleep habits (less sleep (<6 h) (LS) versus more sleep (>6 h) (MS) during menstruation) using independent t-tests.
PA was defined as unstructured daily activities, such as working, housekeeping, transportation, and leisure, while AA involved structured activities that change the capacity of the cardiorespiratory system [29].
For eating habits, a K-means clustering was performed to determine the quality of participants’ nutritional habits based on a prior Mexican study [30]. The variables included were intake of vegetables, fruits, cereals, meat, fish, dairy products, oilseeds, fats, eggs, snacks, soda, and coffee, eating habits during the menstrual period, and type of favorite foods during menstruation. The clustering analyses resulted in 827 participants in the ID group and 852 in the AD group.
Additionally, we compared the distribution of favorite food types during menstruation (salty, sweet, bitter, none in particular) with the severity of dysmenorrhea and PMS symptoms using a chi-square test. We also performed a K-means clustering analysis to classify participants into two groups based on symptom severity: more menstrual symptoms (MMSs) and fewer menstrual symptoms (LMSs). The clustering analysis resulted in 771 participants classified as having MMSs and 906 participants classified as having LMSs.
2.4.2. Predictors of Menstruation Symptoms
Regression analyses were performed to identify the association between dysmenorrhea and the PMS index and those factors that might explain the variability in menstrual symptoms. The linear regression included the index as the dependent variable and age, sex, scholarship, anthropometric data, dietary and sleep habits, physical activity, substance abuse, and sexual habits as independent variables. The linear regression analyses included multiple-linear backward regressions to find a reduced model that best explains the data.
3. Results
3.1. Distribution of Health Habits
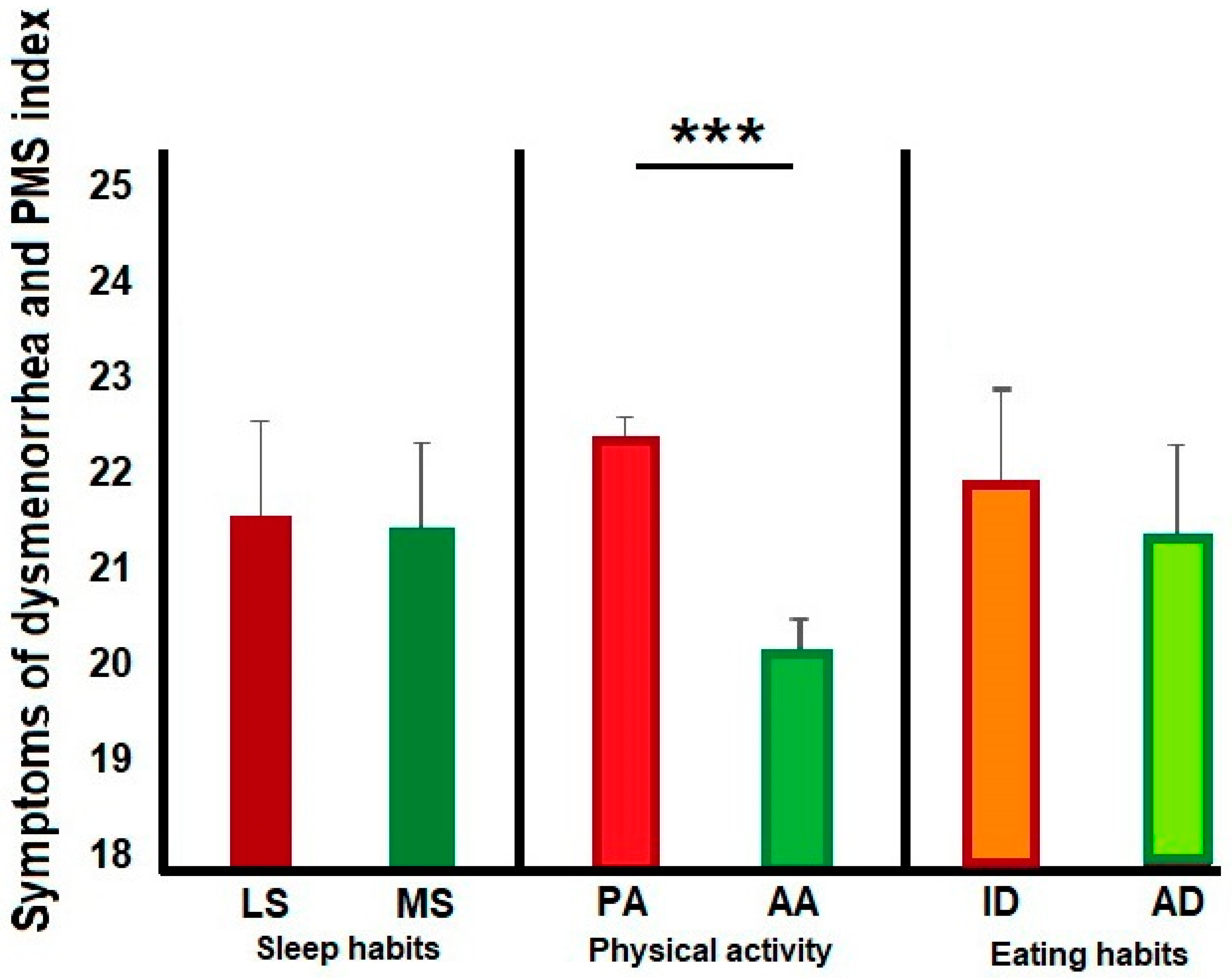
As we expected, physical activity (PA versus AA) was associated with menstrual symptoms (t(1676) 6.6, p < 0.0001). The PA group had a greater score in the index than the AA (PA, mean (M) = 22.7, SD = ±8.5; AA, M = 20.0, SD = ±7.9) during menstruation. Although menstrual symptoms did not differ between sleep and eating habits (sleep habits, LS vs. MS; t(1676) 0.2, p = 0.85; LS, M = 21.8, SD = ±8.7; MS, M = 21.7, SD = ±8.3; Eating habits ID vs. AD, t(1676) −1.6, p = 0.11; ID, M = 22.0, SD = ±8.5; AD, M = 21.4, SD = ±8.2). (See Figure 1). We found differences between the MMS and LMS groups in the type of favorite foods during menstruation (X2 (3) 45.1, p < 0.0001), with a higher count than expected for the MMS group in sweet and salty flavors compared to the LMS group.
Figure 1.
The bar graphs show differences in this cohort’s health habits distribution. We found that the participants with active physical activity (AA) exhibited a lower index score than those with passive physical activity (PA). No differences were observed in sleep and eating habits. *** Significant difference p < 0.0001.
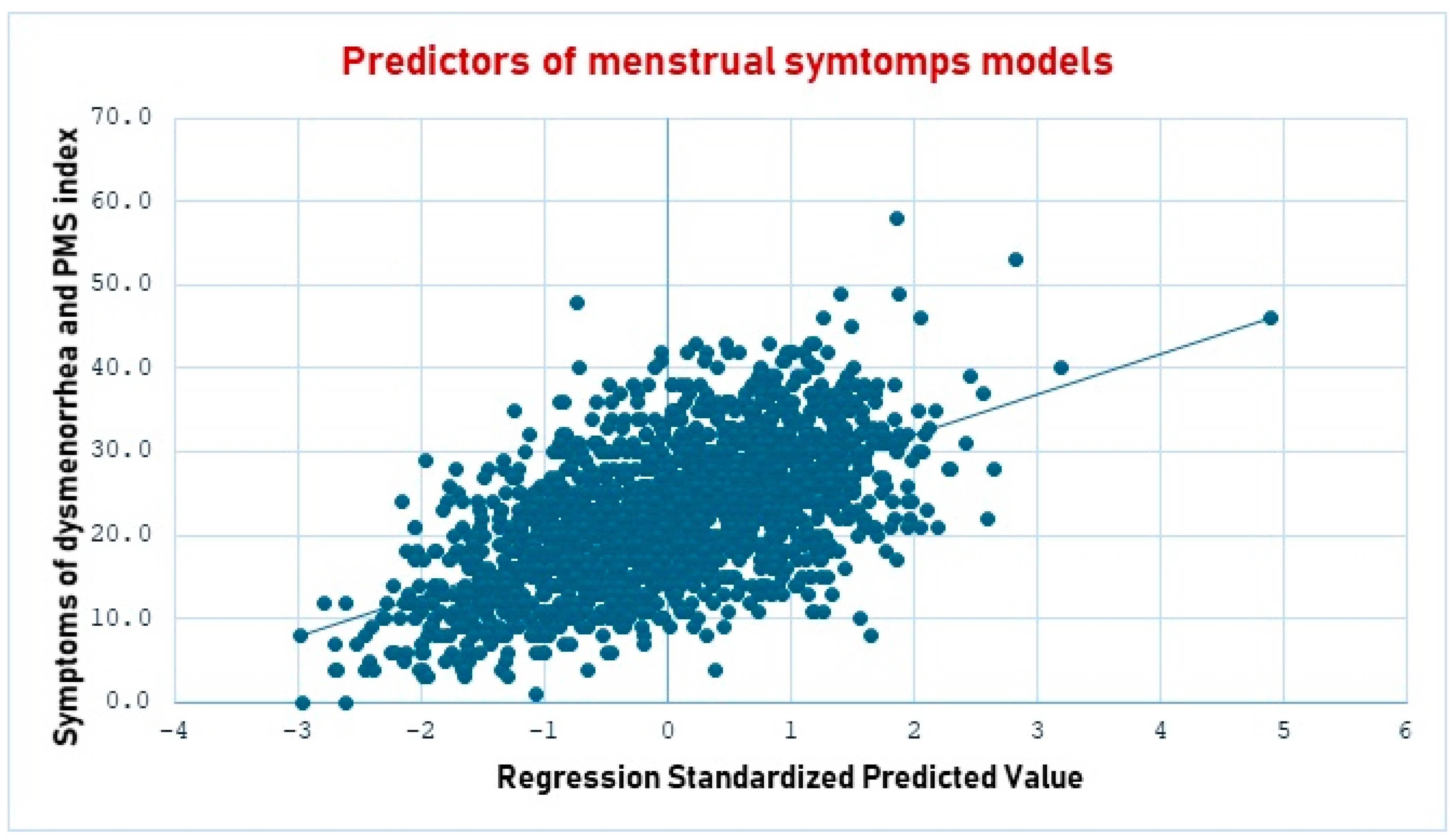
3.2. Predictors of Menstrual Symptoms
As shown in Table 3, menstrual diseases, the duration of the menstrual cycle, bleeding, pain, physical activity, change of eating habits, usual sleep duration, and frequency of vegetable intake were predictors of higher scores in the symptoms of dysmenorrhea and PMS index. In contrast, age, sex life, physical activity, and sleep hours during menstruation predicted lower scores in the symptoms of dysmenorrhea and PMS index. (See Figure 2).

Table 3.
Regression model: predictors of menstrual symptoms.
Figure 2.
The scatter plot shows the regression standardized predictive value of the statistical model to predict menstrual symptoms. The line in blue represents the expected values in the regression model.
4. Discussion
This study aimed to determine whether dietary habits, physical activity, and sleeping habits affect dysmenorrhea and PMS symptoms. As expected, participants with inappropriate health habits had higher menstrual symptoms. However, some unexpected results warrant further explanation.
4.1. Sociodemographic, Anthropometric, and Characteristics of Menstrual Cycle as Predictors
Although in our sample, age was an essential predictor for suffering from dysmenorrhea and PMS, previous studies reported that this variable depended on other factors such as earlier menarche (younger than 12 years), longer menstrual cycles, heavy menstrual flow, BMI < 20 kg/m2, and smoking habit [31,32]. This interaction between age and other factors was also observed in our sample, where most volunteers reported their first menarche between ages 11 and 13.
In our study, early menarche was associated with higher menstrual symptoms, which match multiple studies reporting that earlier menarche triggers primary dysmenorrhea; these studies also suggest that this condition is associated with hormonal immaturity and higher exposition to prostaglandins F2α (PGF2α), disturbing smooth muscle contractions of the uterus, emotional factors, and the reproductive system, increasing the chance of higher pain during menstrual cycle [5,33,34,35,36].
Recent studies also describe that longer menstrual cycles and heavy menstrual flow were good predictors of menstrual symptoms [4,8,31,32], which matches our findings.
Given that our sample represents the Mexican population, most of the participants suffered from obesity, and BMI was not a predictor variable because of its poor variability in our sample. Furthermore, smoking was not a predictor of menstrual symptoms, likely because only 10.3% of participants reported this habit.
In our findings, we also observed that gynecological medical records from the participants were associated with the severity of menstrual symptoms. Prior studies also matched our findings. They reported that dysmenorrhea is genetically influenced [3] and positively associated with its severity [31].
Interestingly, active sexual life was a significant predictor of fewer menstrual symptoms in our study, although we did not find previous research supporting this finding. We suppose that sexual life is a delicate topic worldwide, which affects the participant’s willingness to respond about their sexual habits. In Mexico, public information on female sexual activity is generally available only after the first pregnancy [37], leaving a gap in understanding sexual behavior during childhood or adolescence.
In our study, the number of days of pain during menstruation was a strong predictor of more severe menstrual symptoms. Previous studies reported that the pain appears when the female suffers from dysregulated hormonal equilibrium because of high estriol levels [38], which is also associated with uterine contraction and inflammation. Moreover, it has been reported that C-reactive protein (HsCRP), PGE2, and PGF2α levels are also involved in this inflammation process [12,13]. Therefore, the results observed in this study align with the established pathophysiology of menstrual pain.
4.2. Physical Activity Predictors
As anticipated, physical activity is associated with lower dysmenorrhea symptoms, mainly when females practice it during menstruation with a short duration. These results match prior reports describing that physical activity during menstruation reduces the incidence of dysmenorrhea [12] and increases the quality of life when the woman practices pilates [39] or relaxation exercises, such as yoga [14,15,16,17,18,40]. Other studies explain that physical activity decreases C-reactive protein (HsCRP), PGE2, and PGF2α levels, ameliorating uterine contraction and inflammation [12,13]. However, no studies explain the effect of physical activity on PMS, even when premenstrual symptoms, like anger, anxiety, depression, activity level, fatigue, and menstrual distress symptoms, such as cramps, aches, and swelling, are modulated by the same hormones: estradiol, prolactin, progesterone, and cortisol [13]. Therefore, our study contributes to the literature by demonstrating that physical activity positively affects PMS as well.
4.3. Eating Habits Predictors
We expected adequate eating habits would be associated with lower menstrual symptoms, and our findings partially matched our expectations. We found that an increased intake of sugary (55.3%) or salty (19.5%) foods during the menstrual period was associated with higher menstrual symptoms, as previous studies reported healthier food habits were not a good predictor [7,31,41]. However, no specific food influences menstrual symptoms; we suggest that we did not find any food intake as a predictor of dysmenorrhea symptoms because we did not have precise information about eating consumption during the menstrual cycle.
4.4. Sleep Habits Predictors
We expected adequate sleep habits would be associated with lower menstrual symptoms; our findings matched our expectations. We found that inadequate sleep hours (oversleeping) were associated with higher menstrual symptoms. As mentioned before, sleep disturbance is associated with higher menstrual symptoms [19,20]. Even when we did not assess sleep disturbances in our sample, our participants who tend to sleep too many hours may suffer from sleep disturbances. For example, polycystic ovary syndrome has been associated with an increased risk for sleep-disordered breathing [42], or circadian cycle dysregulation may generate an increase in morbidity risk for inflammatory diseases such as cardiovascular disorder [43,44]. Sleep disturbances mainly affect chemical substances produced during inflammation, such as energy-related molecules, nitric oxide, cytokines, and prostaglandins [45]. Therefore, our participants with habitual oversleeping (not during menstruation) might have more inflammatory symptoms and pain during menstruation than the remaining. In addition, we found that more sleep during menstruation was related to decreased menstrual symptoms, as suggested by previous studies [31].
5. Conclusions
Despite the limitations derived from the study design, we concluded that eating habits predict higher scores in the symptoms of dysmenorrhea and PMS. Sleep hours during menstruation were associated with dysmenorrhea and PMS and regular physical activity was a critical factor in managing dysmenorrhea and PMS.
6. Limitations
The present study has inherent limitations. It is cross-sectional, meaning that it may not provide sufficient evidence to make conclusions on predictors of menstrual symptoms. In addition, given that no physician examined our participants, they might suffer from other psychological and medical conditions. Additionally, we did not assess the 24 h dietary recall method during the menstrual cycle, the type or intensity of physical activity, fatigue, diurnal sleepiness, or sleep disorders. Therefore, our study’s interpretations should be carried out carefully.
Author Contributions
J.M.A.-C., G.C.A.-C. and R.C.-L. contributed to the conception and design of this study, writing—review and editing. J.M.A.-C., R.C.-L. and G.C.A.-C. organized the database and applied the survey. G.C.A.-C. and J.M.A.-C. contributed to the conception of methodology, formal analysis, and validation. V.M.-C. reviewed, performed validation, and edited this manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Ciencia de Frontera-CONAHCYT: CF-2023-I-669, R.C.L., and by CONAHCYT-Estancias Posdoctorales por México para la Formación y consolidación de las y los Investigadores por México, which awarded a postdoctoral fellowship to J.M.A.C.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Benemérita Universidad Autónoma de Puebla (project identification code: 046. April 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author. The data are not publicly available because they contain sensitive patient information.
Acknowledgments
We are especially grateful to all the participants in this study and to José Manuel Gutiérrez Cortés and José Eduardo Chávez-Jiménez for their technical support.
Conflicts of Interest
The authors declare no conflicts of interest, and the funders had no role in the design of the study; in the collection, analyses, or interpretation of the data; in the writing of the manuscript; or in the decision to publish the results.
Appendix A
Table A1 illustrates the survey of participants’ dysmenorrhea symptoms, PMS, and health habits. We included all items applied to our participants.

Table A1.
Survey of participants’ dysmenorrhea symptoms, PMS, and health habits.
Table A1.
Survey of participants’ dysmenorrhea symptoms, PMS, and health habits.
| Identification Data (Datos de Identificación) | Possible Responses |
|---|---|
| Age/(Edad) | Years (años) |
| Marital status/(Estado civil) | Single/Married/Common union/Divorced/Widowed (Soltero (a)/Casado (a)/Unión libre (a)/Divorciado (a)/Viudo (a)) |
| Occupation/(Ocupación) | Open (Abierta) |
| Education /(Escolaridad) | None/Primary/Secondary/High School/Undergraduate/Graduate (Ninguno/Primaria/Secundaria/Preparatoria/Licenciatura/Posgrado) |
| Residencie’ place/(Lugar de residencia) | Open (Abierta) |
| Nationality/(Nacionalidad) | Open (Abierta) |
| Anthropometric data (Datos antropométricos) | |
| Height(m)/(Estatura) | Meters (mts) |
| Weight (kg)/(Peso) | kilograms (kg) |
| Medical records (Datos clínicos) | |
| Pathological family history (Antecedentes familiares patológicos) | |
| Did your family have ever had Dysmenorrhea?/ (En tu familia, han padecido dismenorrea?) | Yes/No (Sí/No) |
| Did your family have ever had difficulty getting pregnant?/(En tu familia, han tenido dificultad para embarazarse?) | Yes/No (Sí/No) |
| Did your family have ever had fibroids?/(En tu familia, han padecido miomas (tumores beningnos)?) | Yes/No (Sí/No) |
| Did your family have ever had cancer?/(En tu familia, han padecido cancer?) | Yes/No (Sí/No) |
| Did your family have ever had endometriosis?/(En tu familia, han padecido endometriosos?) | Yes/No (Sí/No) |
| Did you family have ever had a hysterectomy?/(En tu familia, le han hecho histerectomía?) | Yes/No (Sí/No) |
| Pathological personal history (Antecedentes personales patológicos) | |
| Did you have ever had polycystic ovary syndrome disease?/(¿Usted padece Sindrome de Ovario Poliquístico?) | Yes/No/I have not checked myself (Si/No/No me he checado) |
| Did you have ever had diabetes?/(¿Usted padece Diabetes?) | Yes/No/I have not checked myself (Si/No/No me he checado) |
| Did you have ever had hypertension (high blood pressure)?/(¿Usted padece Hipertensión (presión alta)?) | Yes/No/I have not checked myself (Si/No/No me he checado) |
| Did you have ever had anemia?/(¿Usted padece anemia?) | Yes/No/I have not checked myself (Si/No/No me he checado) |
| Did you have ever had Autoimmune diseases (arthritis, ankylosing spondylitis, lupus erythematosus, antiphospholipid syndrome)?/Usted, padece enfermedades autoinmunes (artritis, espondilitis anquilosante, lupus eritematoso, Síndrome antifosfolípidos)? | Yes/No/I have not checked myself (Si/No/No me he checado) |
| Did you have ever had cholesterolemia?/(¿Usted padece hipercolesterolemia o colesterol alto?) | Yes/No/I have not checked myself (Si/No/No me he checado) |
| Did you have ever had hypertriglyceridemia?/(¿Usted padece hipertrigliceridemia o triglicéridos altos?) | Yes/No/I have not checked myself (Si/No/No me he checado) |
| Did you have ever had difficulty getting pregnant?/(Usted, ha tenido dificultad para embarazarse?) | Yes /No (Sí/No) |
| Did you have ever suffered from infertility?/(Usted, ha sufrido de infertilidad?) | Yes /No (Sí/No) |
| Have you ever have had abortions?/(Usted, ha tenido abortos?) | Yes /No (Sí/No) |
| Did you have ever had endometriosis?/(Usted padece de endometriosis?) | Yes /No (Sí/No) |
| Did you have ever had fibroids? /(Usted padece de miomas (tumores benignos)?) | Yes /No (Sí/No) |
| Did you have ever had hormonal imbalances? /(Usted padece de alteraciones hormonales?) | Yes /No (Sí/No) |
| Did you have ever had cancer? /(Usted padece de cancer?) | Yes /No (Sí/No) |
| Have you ever had a hysterectomy? /(Usted tuvo una histerectomía (quitar la matriz)?) | Yes /No (Sí/No) |
| Have you ever had vaginal infecctions? (Usted ha tenido infecciones vaginales?) | Yes /No (Sí/No) |
| Premenstrual syndrome (Síndrome premenstrual) | |
| Have you ever had abdominal inflammation?/(En su período menstrual, usted padece dolor abdominal?) | Never, rarely, frequently, always (Nunca, rara vez, frecuentemente, siempre) |
| Have you ever had chills?/(En su período menstrual, usted tiene escalofríos?) | Never, rarely, frequently, always (Nunca, rara vez, frecuentemente, siempre) |
| Have you ever had edema or inflammation in your legs?/(En su período menstrual, usted tiene edema o inflamación en sus piernas?) | Never, rarely, frequently, always (Nunca, rara vez, frecuentemente, siempre) |
| Have you ever had a headache?/(En su período menstrual, usted padece de dolores de cabeza?) | Never, rarely, frequently, always (Nunca, rara vez, frecuentemente, siempre) |
| Did you experience sadness?/(En su período menstrual, usted experimenta tristeza?) | Never, rarely, frequently, always (Nunca, rara vez, frecuentemente, siempre) |
| Did you experience anger or annoyance?/(En su período menstrual, usted experimenta enojo?) | Never, rarely, frequently, always (Nunca, rara vez, frecuentemente, siempre) |
| Did you experience anxiety?/(En su período menstrual, usted experimenta ansiedad?) | Never, rarely, frequently, always (Nunca, rara vez, frecuentemente, siempre) |
| Did you experience aggressiveness?/(En su período menstrual, usted experimenta agresividad?) | Never, rarely, frequently, always (Nunca, rara vez, frecuentemente, siempre) |
| Indicate level of bleeding in the first days of menstruation (Indique nivel de sangrado en los primeros días de la menstruación) | No menstruation/Light/Normal/Abundant/Very abundant (No menstruo/Ligero/ Normal/Abundante /Muy abundante) |
| Indicate level of bleeding in the last days of menstruation. (Indique nivel de sangrado en los últimos días de la menstruación.) | No menstruation/Light/Normal/Abundant/Very abundant (No menstruo/Ligero/ Normal/Abundante /Muy abundante) |
| Bleeding duration (days): (Duración de sangrado (días):) | 0–7 days (días) |
| Have you stopped working, studying or doing your activities because of colic pain? (¿Has dejado de trabajar, estudiar o hacer tus actividades por el dolor de cólico?) | Yes/No/Sometimes (Si/No/A veces) |
| From 0 to 10, how much it hurts in the first days of your menstrual period (Del 0 al 10 que tanto te duele en los primeros días en tu período menstrual) | 0–10 |
| From 0 to 10, how much it hurts you in the last days of your menstrual period (Del 0 al 10 que tanto te duele en los últimos días en tu período menstrual) | 0–10 |
| From 0 to 10, how much anxiety (fear and restlessness) you have in the first days of your menstrual period (Del 0 al 10 que tanta ansiedad (miedo, temor e inquietud) presentas en los primeros días de tu período menstrual) | 0–10 |
| From 0 to 10, how much stress (physical or emotional tension) you experience in the first days of your menstrual period (Del 0 al 10 que tanto estrés (tensión física o emocional) presentas en primeros días de tu período menstrual) | 0–10 |
| From 0 to 10, how much energy or spirit you have in the first days of your menstrual period (Del 0 al 10 que tanta energía o ánimo presentas en los primeros días de tu período menstrual) | 0–10 |
| Do you use medication for colic pain? (¿Usas medicamentos para el dolor de cólico?) | Yes /No (Sí/No) |
| What medication do you take for colic and how many pills per day? (¿Cuál medicamento tomas para el cólico y cuántas pastillas por día?) | Open (Abierta) |
| Do you use hormonal treatment or contraceptives? (¿Usas tratamiento hormonal o anticonceptivos?) | Yes/No (Sí/No) |
| If so, what contraceptive method do you use? (¿De ser así, cual método anticonceptivo usas?) | Open (Abierta) |
| Gynecobstetric data (Datos gineco-obstétricos) | |
| How often do you go to the gynecologist? (¿Con que frecuencia acudes a la ginecóloga (o)?) | Never/Once a year/Once every 6 months/More than once every 6 months (Nunca/1 vez al año/1 vez cada 6 meses/Más de 1 vez cada 6 meses) |
| How often have you had a pap smear? (¿Con que frecuencia te has hecho el papanicolaou?) | Never/Once a year/Once every 6 months/More than once every 6 months (Nunca /1 vez al año/1 vez cada 6 meses/ Más de 1 vez cada 6 meses) |
| Sex life: (Vida sexual:) | Active/Inactive (Activa/Inactiva) |
| Age of menarche (Edad de la primera menstruación) | Years (años) |
| Indicate what is the time of your menstrual cycle (Indicar cual es el tiempo de su ciclo menstrual) | Less than 21 days/From 21–35 days/Greater than 35 days/No Menstruation (Menos de 21 días/ De 21–35 días/Mayor a 35 días /No Menstruo) |
| Please indicate if you are currently: (Indique si usted está:) | None/Pregnant/Breastfeeding/Menopause (Ninguno/ Embarazada/Lactando /Menopausia) |
| Eating habits data (Datos de hábitos alimentarios) | |
| Have you noticed that your eating habits change during your menstrual period? (¿Usted ha notado que cambia hábitos alimentarios en el período menstrual?) | Yes/No (Sí/No) |
| What do you prefer to eat during your period? (¿Qué prefiere comer en tu menstruación?) | Salty/Sweet/Bitter/None (Salado/Dulce/Amargo/Ninguno en particular) |
| How many liters of water do you drink a day? (¿Cuántos litros toma de agua simple al día?) | Liters (Litros) |
| Do you consume alcoholic beverages? (¿Consume usted bebidas alcohólicas ?) | Yes /No (Sí/No) |
| Do you smoke? (¿ Usted fuma ?) | Yes /No (Sí/No) |
| Do you consume drugs? (¿Consume usted grogas ?) | Yes /No (Sí/No) |
| Do you drink coffee? (¿Consume usted café?) | Yes /No (Sí/No) |
| How often do you eat fruits? (¿Qué tan frecuente consume frutas?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you eat vegetables? (¿Qué tan frecuente consume verduras?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you eat red meat? (¿Qué tan frecuente consume carne roja?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you eat fish? (¿Qué tan frecuente consume pescado?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you eat chicken? (¿Qué tan frecuente consume pollo?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume milk? (¿Qué tan frecuente consume leche?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume eggs? (¿Qué tan frecuente consume huevo?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you eat tortilla? (¿Qué tan frecuente consume tortilla?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you eat sweet bread? (¿Qué tan frecuente consume pan dulce?) | (Never/By season/once a month/once or twice a week/three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume oil? (¿Qué tan frecuente consume aceite?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume butter? How often do you consume lard? (¿Qué tan frecuente consume manteca?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume nuts, almonds, seeds, peanuts? (¿Qué tan frecuente consume nueces, almendras, semillas, cacahuates?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume sugar? (¿Qué tan frecuente consume azúcar?) | (Never/ By season/once a month/once or twice a week/three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you eat sweets? (¿Qué tan frecuente consume dulces?) | (Never/ By season/once a month/once or twice a week/three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume soda? (¿Qué tan frecuente consume refresco?) | (Never/ By season/once a month/once or twice a week/three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you drink beer? (¿Qué tan frecuente consume cerveza?) | (Never/ By season/once a month/once or twice a week/ three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume wine? (¿Qué tan frecuente consume vino?) | (Never/ By season/once a month/once or twice a week/three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume Vodka, rum, tequila, etc.? (¿Qué tan frecuente consume Vodka, ron, tequila, etc.?) | (Never/By season/once a month/once or twice a week/three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume chocolate? (¿Qué tan frecuente consume chocolate?) | (Never/ By season/once a month/once or twice a week/three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| How often do you consume ice cream? (¿Qué tan frecuente consume helado?) | (Never/ By season/once a month/once or twice a week/three or five times a week/ every day) (Nunca/Por temporada/1 vez por mes/1–2 veces por sem/3–5 veces por sem/Diario) |
| Physical activity data (Datos de actividad física) | |
| How long does it last to exercise? (¿Cuánto dura haciendo ejercicio?) | I don’t do it/Less than 20 min/Half an hour/More than 1 h (No hago/Menos de 20 min/Media hora/Más de 1 hora) |
| Do you exercise during menstruation? (¿Durante la menstruación realiza ejercicio?) | Yes /No (Sí/No) |
| Sleep habits data (Datos de hábitos de sueño) | |
| In the last 3 months, how long do you usually sleep? (En los últimos 3 meses, ¿Cuánto tiempo duermes generalmente?) | Less than 6 h/From 6 to 9 h/More than 9 h (Menos de 6 horas/De 6 a 9 horas/Más de 9 horas) |
| How long do you sleep during your menstruation? (¿Cuánto tiempo duermes durante tu menstruación?) | Less than 6 h/From 6 to 9 h/More than 9 h (Menos de 6 horas/De 6 a 9 horas/Más de 9 horas) |
References
- Qin, L.L.; Hu, Z.; Kaminga, A.C.; Luo, B.A.; Xu, H.L.; Feng, X.L.; Liu, J.H. Association between Cigarette Smoking and the Risk of Dysmenorrhea: A Meta-Analysis of Observational Studies. PLoS ONE 2020, 15, e231201. [Google Scholar] [CrossRef] [PubMed]
- Iacovides, S.; Avidon, I.; Baker, F.C. What We Know about Primary Dysmenorrhea Today: A Critical Review. Hum. Reprod. Update 2015, 21, 762–778. [Google Scholar] [CrossRef] [PubMed]
- Aouad, P.; Bui, M.; Sarraf, S.; Donnelly, T.; Chen, Y.; Jaaniste, T.; Eden, J.; Champion, G.D. Primary Dysmenorrhoea in Adolescents and Young Women: A Twin Family Study of Maternal Transmission, Genetic Influence and Associations. Aust. N. Z. J. Obstet. Gynaecol. 2022, 62, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Negriff, S.; Dorn, L.D.; Hillman, J.B.; Huang, B. The Measurement of Menstrual Symptoms. J. Health Psychol. 2009, 14, 899–908. [Google Scholar] [CrossRef]
- French, L. Dysmenorrhea. Am. Fam. Physician 2005, 71, 286–291. [Google Scholar]
- Onieva-Zafra, M.D.; Fernández-Martínez, E.; Abreu-Sánchez, A.; Iglesias-López, M.T.; García-Padilla, F.M.; Pedregal-González, M.; Parra-Fernández, M.L. Relationship Between Diet, Menstrual Pain and Other Menstrual Characteristics among Spanish Students. Nutrients 2020, 12, 1759. [Google Scholar] [CrossRef]
- Bajalan, Z.; Alimoradi, Z.; Moafi, F. Nutrition as a Potential Factor of Primary Dysmenorrhea: A Systematic Review of Observational Studies. Gynecol. Obstet. Investig. 2019, 84, 209–224. [Google Scholar] [CrossRef]
- Al-Matouq, S.; Al-Mutairi, H.; Al-Mutairi, O.; Abdulaziz, F.; Al-Basri, D.; Al-Enzi, M.; Al-Taiar, A. Dysmenorrhea among High-School Students and Its Associated Factors in Kuwait. BMC Pediatr. 2019, 19, 80. [Google Scholar] [CrossRef]
- Guimarães, I.; Póvoa, A.M. Primary Dysmenorrhea: Assessment and Treatment. Rev. Bras. Ginecol. Obstet. 2020, 42, 501–507. [Google Scholar] [CrossRef]
- Fujiwara, T.; Ono, M.; Iizuka, T.; Sekizuka-Kagami, N.; Maida, Y.; Adachi, Y.; Fujiwara, H.; Yoshikawa, H. Breakfast Skipping in Female College Students Is a Potential and Preventable Predictor of Gynecologic Disorders at Health Service Centers. Diagnostics 2020, 10, 476. [Google Scholar] [CrossRef]
- Gutke, A.; Sundfeldt, K.; De Baets, L. Lifestyle and Chronic Pain in the Pelvis: State of the Art and Future Directions. J. Clin. Med. 2021, 10, 5397. [Google Scholar] [CrossRef]
- Bavil, D.A.; Dolatian, M.; Mahmoodi, Z.; Baghban, A.A. A Comparison of Physical Activity and Nutrition in Young Women with and without Primary Dysmenorrhea. F1000Research 2018, 7, 59. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.C.; Chiu, P.C.; Ho, C.H. The Sprint-Interval Exercise Using a Spinning Bike Improves Physical Fitness and Ameliorates Primary Dysmenorrhea Symptoms Through Hormone and Inflammation Modulations: A Randomized Controlled Trial. J. Sport. Sci. Med. 2022, 21, 595–607. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, M.I.; Cortés-Márquez, S.K.; Romero-Quezada, L.C.; Murguía-Cánovas, G.; Jaramillo-Díaz, A.P. Effect of a Physiotherapy Program in Women with Primary Dysmenorrhea. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 194, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Yonglitthipagon, P.; Muansiangsai, S.; Wongkhumngern, W.; Donpunha, W.; Chanavirut, R.; Siritaratiwat, W.; Mato, L.; Eungpinichpong, W.; Janyacharoen, T. Effect of Yoga on the Menstrual Pain, Physical Fitness, and Quality of Life of Young Women with Primary Dysmenorrhea. J. Bodyw. Mov. Ther. 2017, 21, 840–846. [Google Scholar] [CrossRef] [PubMed]
- Matthewman, G.; Lee, A.; Kaur, J.G.; Daley, A.J. Physical Activity for Primary Dysmenorrhea: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Am. J. Obstet. Gynecol. 2018, 219, 255.e1–255.e20. [Google Scholar] [CrossRef]
- Kirmizigil, B.; Demiralp, C. Effectiveness of Functional Exercises on Pain and Sleep Quality in Patients with Primary Dysmenorrhea: A Randomized Clinical Trial. Arch. Gynecol. Obstet. 2020, 302, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Wildayani, D.; Lestari, W.; Ningsih, W.L.; Sujendri, S. The Relationship Between Physical Activity Level and Dysmenorrhoea in Young Women. Med. J. Malays. 2023, 78, 495–499. [Google Scholar]
- Jeon, B.; Baek, J. Menstrual Disturbances and Its Association with Sleep Disturbances: A Systematic Review. BMC Women’s Health 2023, 23, 470. [Google Scholar] [CrossRef]
- Jeong, D.; Lee, H.; Kim, J. Effects of Sleep Pattern, Duration, and Quality on Premenstrual Syndrome and Primary Dysmenorrhea in Korean High School Girls. BMC Women’s Health 2023, 23, 456. [Google Scholar] [CrossRef]
- Ortiz, M.I. Primary Dysmenorrhea among Mexican University Students: Prevalence, Impact and Treatment. Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 152, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Lifshitz, A.; Arrieta, O.; Burgos, R.; Campillo Serrano, C.; Celis, M.Á.; De la Llata, M.; Domínguez, J.; Halabe, J.; Islas-Andrade, S.; Jasso, L.; et al. Automedicación y Autoprescripción. Gac. Med. Mex. 2020, 156, 612–614. [Google Scholar] [CrossRef]
- Ortiz, M.I. The Trend of Increasing Primary Dysmenorrhea Prevalence in Mexican University Students. Clin. Exp. Obstet. Gynecol. 2023, 50, 58. [Google Scholar] [CrossRef]
- Bayley, N. Bayley Scales of Infant Development Manual 2; The Psychological Corporation: San Antonio, TX, USA, 1993. [Google Scholar]
- Pawłowski, B. Prevalence of Menstrual Pain in Relation to the Reproductive Life History of Women from the Mayan Rural Community. Ann. Hum. Biol. 2004, 31, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pedrón-Nuevo, N.; González-Unzaga, L.N.; De Celis-Carrillo, R.; Reynoso-Isla, M.; de la Torre-Romeral, L. Incidence of Dysmenorrhea and Associated Symptoms in Women Aged 12–24 Years. Ginecol. Obstet. Mex. 1998, 66, 492–494. [Google Scholar]
- Ortiz, M.I.; Espinoza-Ramírez, A.L.; Cariño-Cortés, R.; Moya-Escalera, A. Impacto de La Dismenorrea Primaria En El Rendimiento Académico de Estudiantes Universitarios. Enfermería Clínica (Engl. Ed.) 2022, 32, 351–357. [Google Scholar] [CrossRef]
- Aburto, T.C.; Batis, C.; Pedroza-Tobías, A.; Pedraza, L.S.; Ramírez-Silva, I.; Rivera, J.A. Dietary Intake of the Mexican Population: Comparing Food Group Contribution to Recommendations, 2012–2016. Salud Publica Mex. 2022, 64, 267–279. [Google Scholar] [CrossRef]
- Strath, S.J.; Kaminsky, L.A.; Ainsworth, B.E.; Ekelund, U.; Freedson, P.S.; Gary, R.A.; Richardson, C.R.; Smith, D.T.; Swartz, A.M.; American Heart Association Physical Activity Committee of the Council on Lifestyle and Cardiometabolic Health and Cardiovascular, Exercise, Cardiac Rehabilitation and Prevention Committee of the Council on Clinical Cardiology, and Council on Cardiovascular and Stroke Nursing. Guide to the Assessment of Physical Activity: Clinical and Research Applications: A Scientific Statement from the American Heart Association. Circulation 2013, 128, 2259–2279. [Google Scholar] [CrossRef]
- UNICEF. Guías Alimentarias Saludables y Sostenibles Para La Población Mexicana 2023; Secretaría de Salud: Mexico City, Mexico, 2023.
- Al-Husban, N.; Odeh, O.; Dabit, T.; Masadeh, A. The Influence of Lifestyle Variables on Primary Dysmenorrhea: A Cross-Sectional Study. Int. J. Women’s Health 2022, 14, 545–553. [Google Scholar] [CrossRef]
- McKenna, K.A.; Fogleman, C.D. Dysmenorrhea. Am. Fam. Physician 2021, 104, 164–170. [Google Scholar] [CrossRef]
- Barcikowska, Z.; Rajkowska-Labon, E.; Grzybowska, M.E.; Hansdorfer-Korzon, R.; Zorena, K. Inflammatory Markers in Dysmenorrhea and Therapeutic Options. Int. J. Environ. Res. Public Health 2020, 17, 1191. [Google Scholar] [CrossRef] [PubMed]
- Barcikowska, Z.; Wójcik-Bilkiewicz, K.; Sobierajska-Rek, A.; Grzybowska, M.E.; Wąż, P.; Zorena, K. Dysmenorrhea and Associated Factors among Polish Women: A Cross-Sectional Study. Pain Res. Manag. 2020, 2020, 6161536. [Google Scholar] [CrossRef] [PubMed]
- Bernardi, M.; Lazzeri, L.; Perelli, F.; Reis, F.M.; Petraglia, F. Dysmenorrhea and Related Disorders. F1000Research 2017, 6, 1645. [Google Scholar] [CrossRef] [PubMed]
- Ju, H.; Jones, M.; Mishra, G. The Prevalence and Risk Factors of Dysmenorrhea. Epidemiol. Rev. 2014, 36, 104–113. [Google Scholar] [CrossRef]
- Cuenca, L.C.; Atienzo, E.E.; López, L.S.; Prado, B.H. Salud Sexual y Reproductiva de Los Adolescentes En México: Evidencias y Propuestas. Gac. Médica México 2013, 149, 299–307. [Google Scholar]
- Jiang, J.; Zhuang, Y.; Si, S.; Cheng, H.; Alifu, X.; Mo, M.; Zhou, H.; Liu, H.; Yu, Y. The Association of Reproductive Hormones During the Menstrual Period with Primary Dysmenorrhea. Int. J. Women’s Health 2023, 15, 1501–1514. [Google Scholar] [CrossRef]
- Kirthika, S.V.; Sudhakar, S.; Mohan Kumar, G.; Ramachandran, S.; Deepthi, R.N.V.; Senthil Selvam, P. Comparing Pilates and Gym Ball Exercises for Primary Dysmenorrhea Management: An Empirical Study. Cureus 2024, 16, e59184. [Google Scholar] [CrossRef]
- Tsai, I.C.; Hsu, C.W.; Chang, C.H.; Lei, W.T.; Tseng, P.T.; Chang, K.V. Comparative Effectiveness of Different Exercises for Reducing Pain Intensity in Primary Dysmenorrhea: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. Sport. Med.-Open 2024, 10, 63. [Google Scholar] [CrossRef]
- Hirschberg, A.L. Sex Hormones, Appetite and Eating Behaviour in Women. Maturitas 2012, 71, 248–256. [Google Scholar] [CrossRef]
- Baker, F.C.; Lee, K.A. Menstrual Cycle Effects on Sleep. Sleep Med. Clin. 2022, 17, 283–294. [Google Scholar] [CrossRef]
- Huang, B.H.; Duncan, M.J.; Cistulli, P.A.; Nassar, N.; Hamer, M.; Stamatakis, E. Sleep and Physical Activity in Relation to All-Cause, Cardiovascular Disease and Cancer Mortality Risk. Br. J. Sports Med. 2022, 56, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Chaix, A.; Zarrinpar, A.; Panda, S. The Circadian Coordination of Cell Biology. J. Cell Biol. 2016, 215, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Cui, J.; Chen, Y.; Wang, H.Y.; Wang, R.-F. Mechanisms and Pathways of Innate Immune Activation and Regulation in Health and Cancer. Hum. Vaccines Immunother. 2014, 10, 3270–3285. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).