Lower Jaw Full-Arch Restoration: A Completely Digital Approach to Immediate Load
Abstract
:1. Introduction
2. Materials and Methods
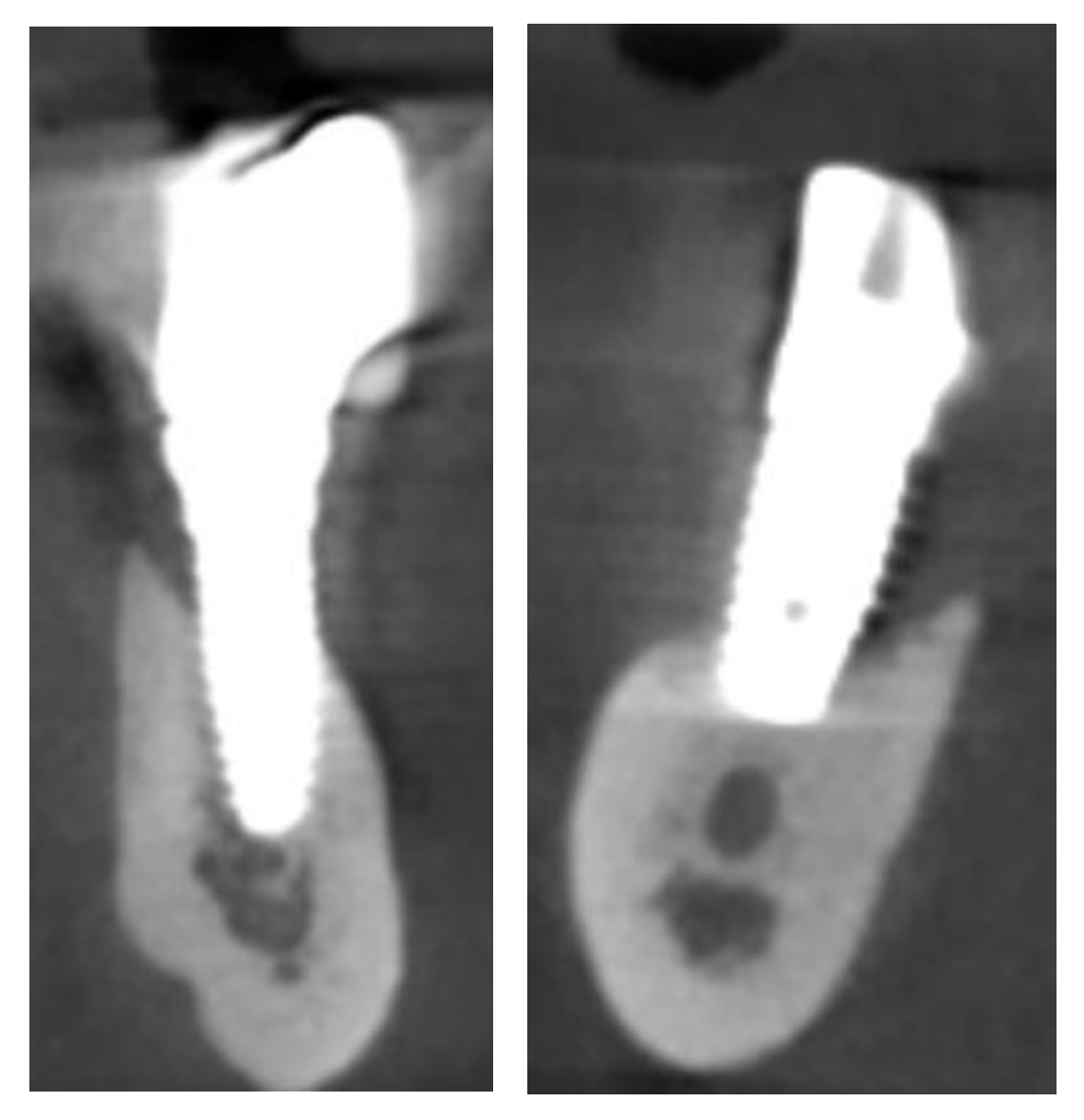
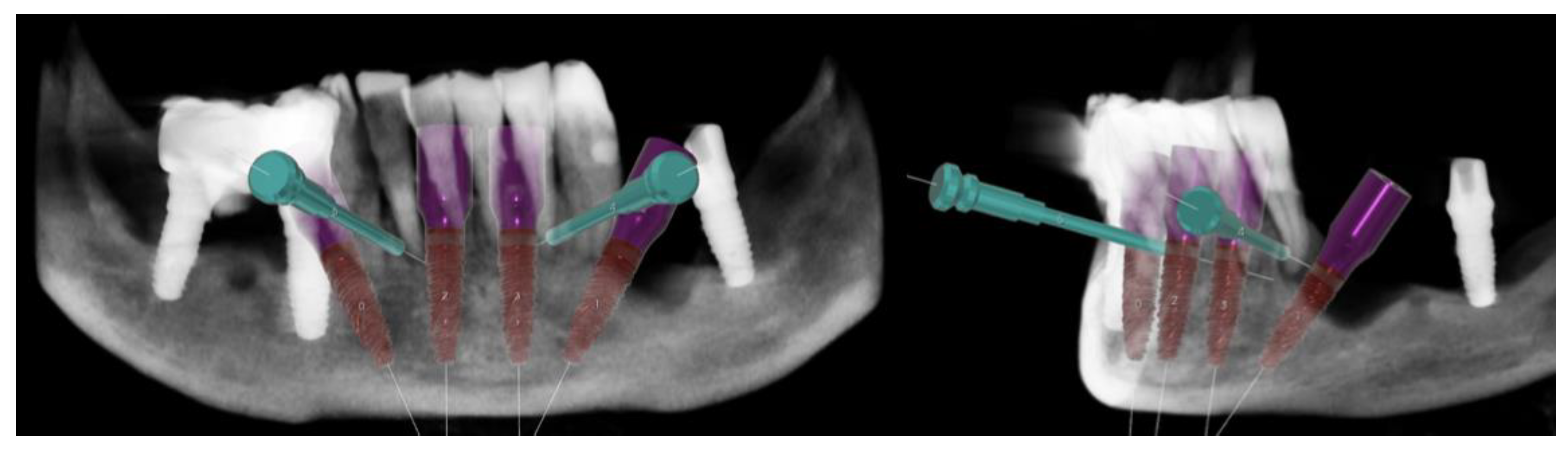
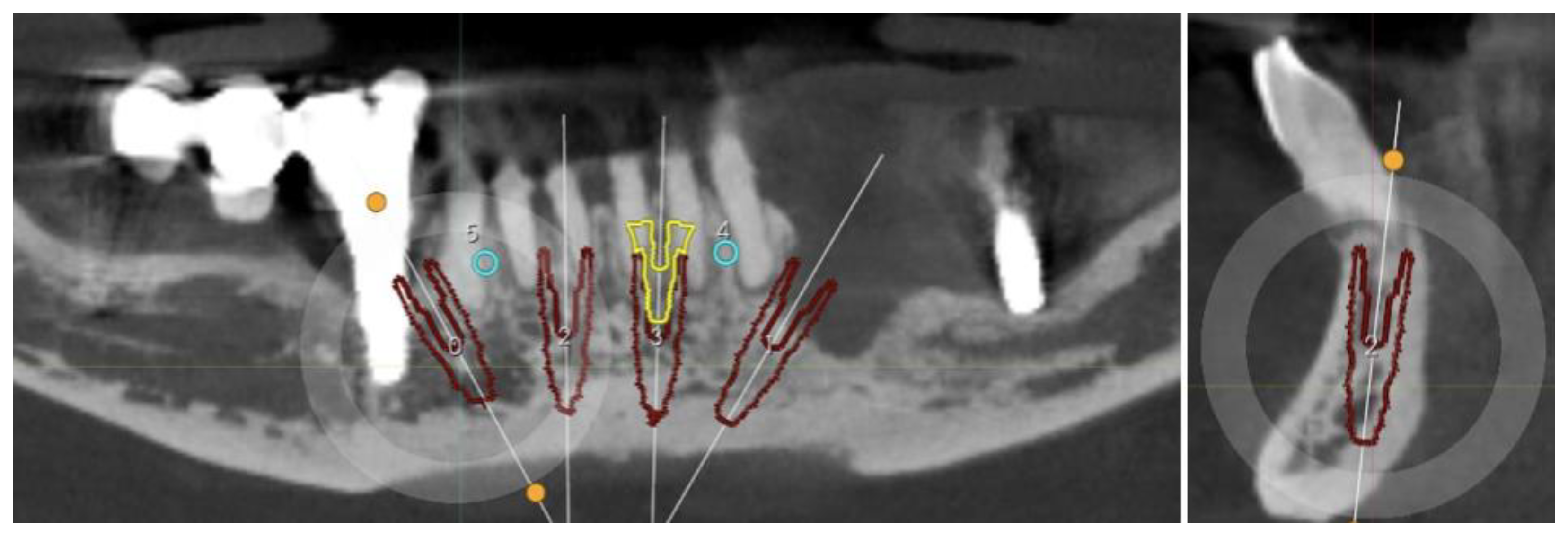
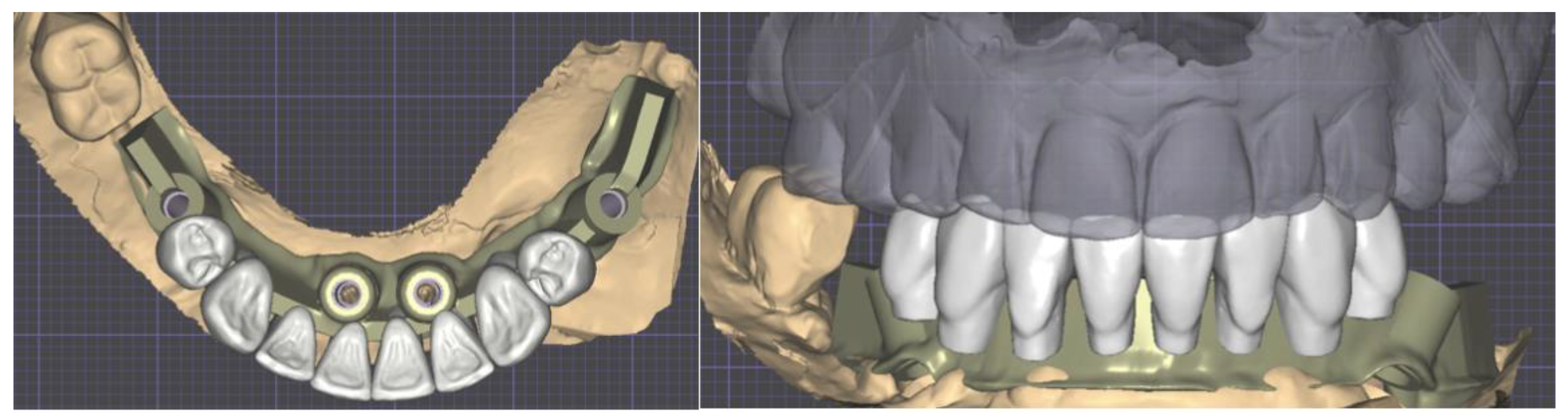
2.1. Planning
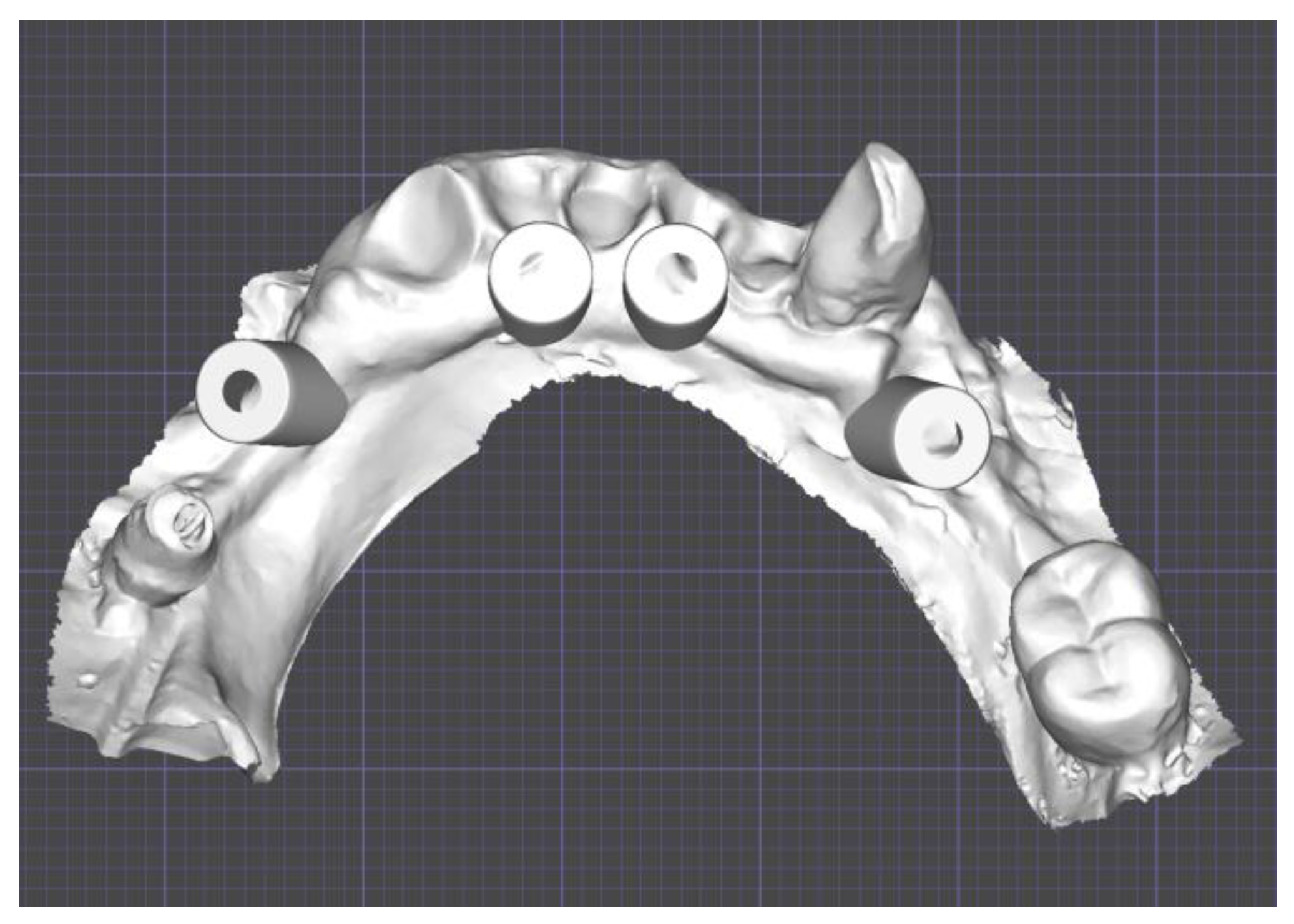
Surgical Guide
2.2. Provisional Prosthesis
2.3. Three-Dimensional Printing
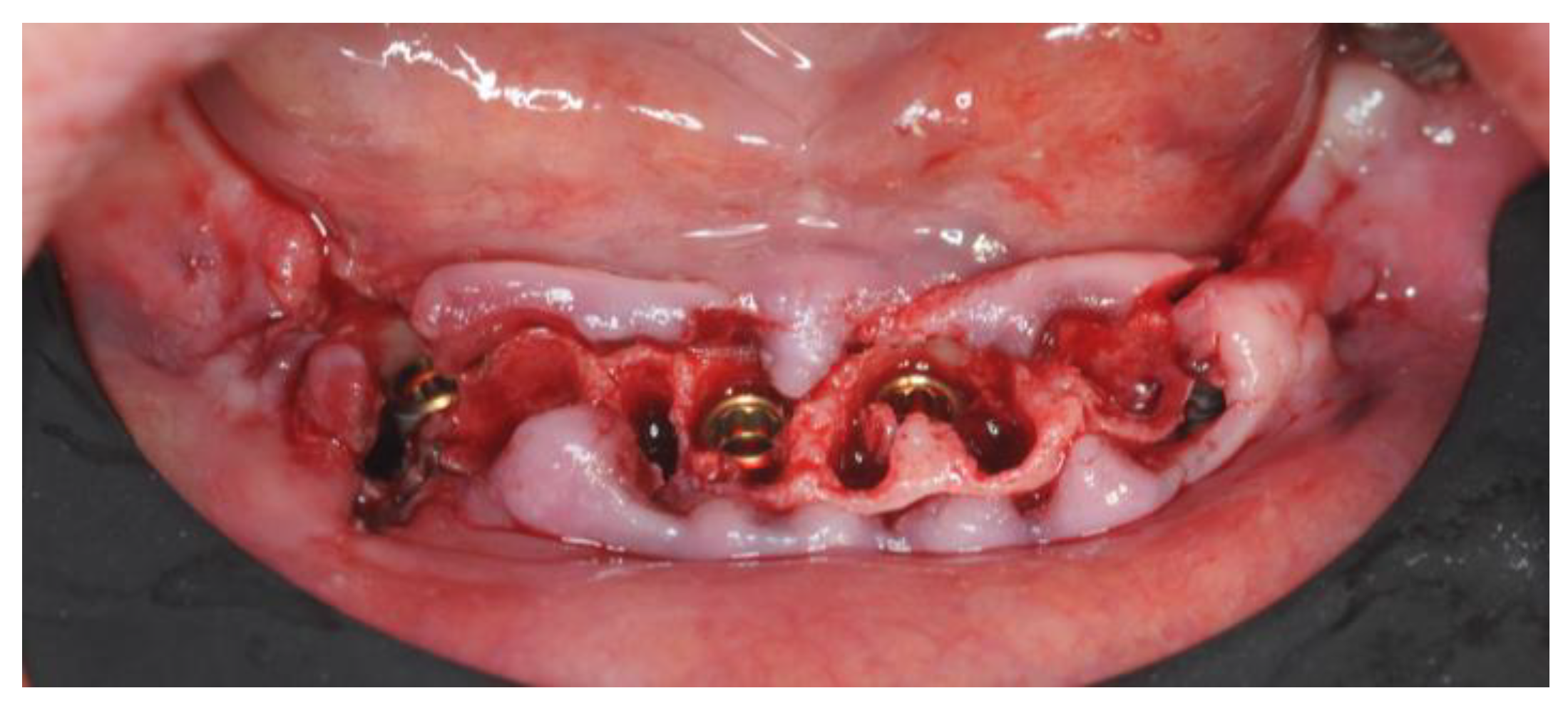
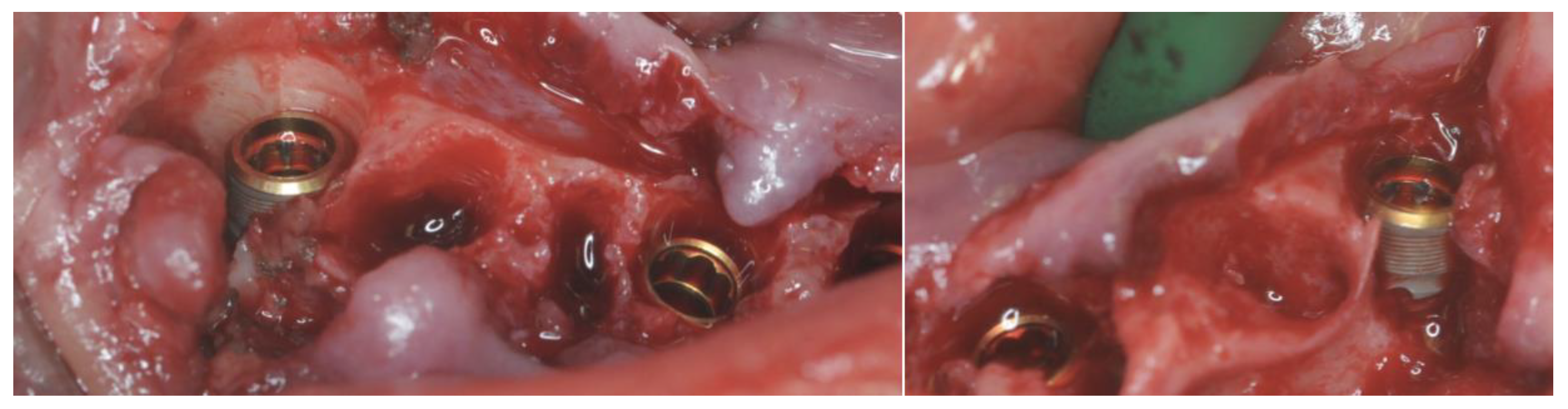
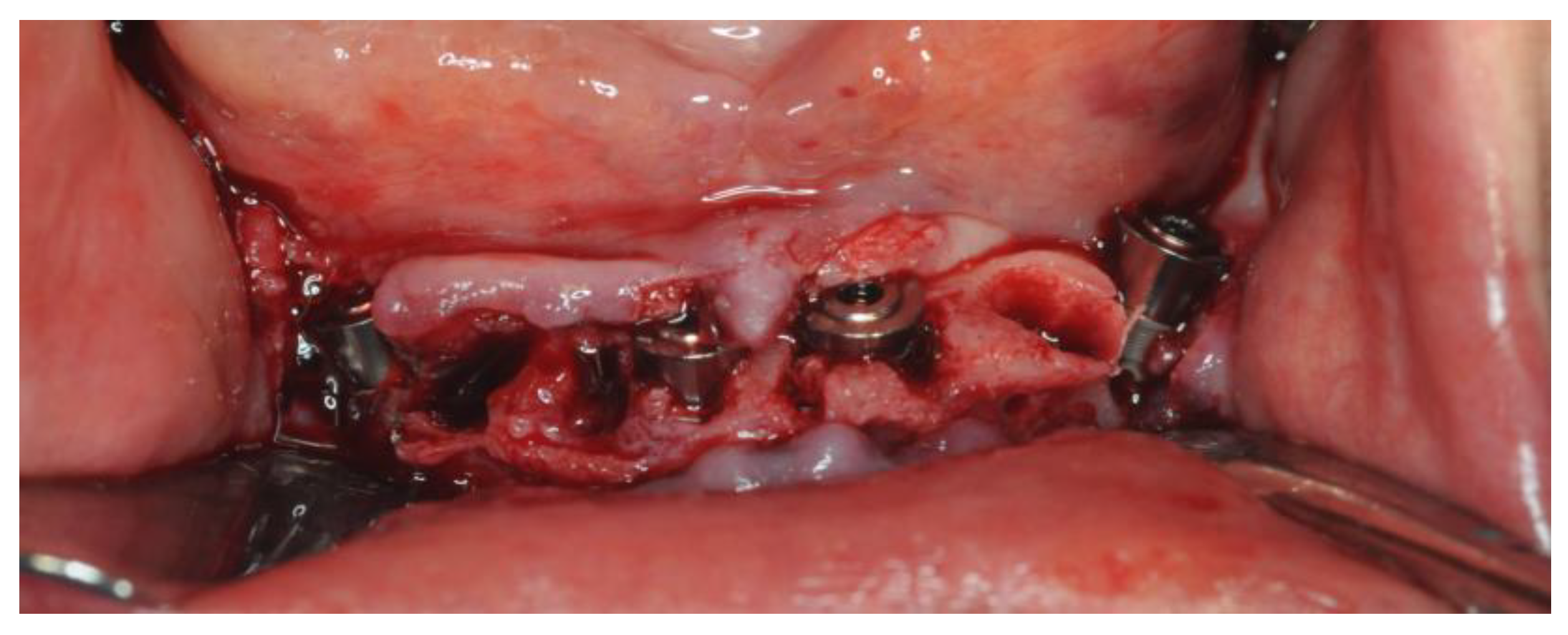
2.4. Surgery
2.5. Definitive Prosthesis
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alauddin, M.S.; Baharuddin, A.S.; Mohd Ghazali, M.I. The Modern and Digital Transformation of Oral Health Care: A Mini Review. Healthcare 2021, 9, 118. [Google Scholar] [CrossRef]
- Joda, T.; Yeung, A.W.K.; Hung, K.; Zitzmann, N.U.; Bornstein, M.M. Disruptive Innovation in Dentistry: What It Is and What Could Be Next. J. Dent. Res. 2021, 100, 448–453. [Google Scholar] [CrossRef]
- Joda, T.; Bornstein, M.M.; Jung, R.E.; Ferrari, M.; Waltimo, T.; Zitzmann, N.U. Recent Trends and Future Direction of Dental Research in the Digital Era. Int. J. Environ. Res. Public Health 2020, 17, 1987. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M. Computerization and Digital Workflow in Medicine: Focus on Digital Dentistry. Materials 2020, 13, 2172. [Google Scholar] [CrossRef]
- Todaro, C.; Cerri, M.; Isola, G.; Manazza, A.; Storelli, S.; Baena, R.R.Y.; Lupi, S.M. Computer-Guided Osteotomy with Simultaneous Implant Placement and Immediately Loaded Full-Arch Fixed Restoration: A Case Report. Prosthesis 2023, 5, 221–233. [Google Scholar] [CrossRef]
- Todaro, C.; Cerri, M.; Rodriguez y Baena, R.; Lupi, S.M. Full-Arch Guided Restoration and Bone Regeneration: A Complete Digital Workflow Case Report. Healthcare 2023, 11, 1301. [Google Scholar] [CrossRef] [PubMed]
- Pesce, P.; Pera, F.; Setti, P.; Menini, M. Precision and Accuracy of a Digital Impression Scanner in Full-Arch Implant Rehabilitation. Int. J. Prosthodont. 2018, 31, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Velasco-Ortega, E.; Cracel-Lopes, J.L.; Matos-Garrido, N.; Jiménez-Guerra, A.; Ortiz-Garcia, I.; Moreno-Muñoz, J.; Núñez-Márquez, E.; Rondón-Romero, J.L.; López-López, J.; Monsalve-Guil, L. Immediate Functional Loading with Full-Arch Fixed Implant-Retained Rehabilitation in Periodontal Patients: Clinical Study. Int. J. Environ. Res. Public Health 2022, 19, 13162. [Google Scholar] [CrossRef] [PubMed]
- Bassir, S.H.; El Kholy, K.; Chen, C.-Y.; Lee, K.H.; Intini, G. Outcome of early dental implant placement versus other dental implant placement protocols: A systematic review and meta-analysis. J. Periodontol. 2019, 90, 493–506. [Google Scholar] [CrossRef]
- Chatzopoulos, G.S.; Wolff, L.F. Survival Rates and Factors Affecting the Outcome Following Immediate and Delayed Implant Placement: A Retrospective Study. J. Clin. Med. 2022, 11, 4598. [Google Scholar] [CrossRef]
- Chen, J.; Cai, M.; Yang, J.; Aldhohrah, T.; Wang, Y. Immediate versus early or conventional loading dental implants with fixed prostheses: A systematic review and meta-analysis of randomized controlled clinical trials. J. Prosthet. Dent. 2019, 122, 516–536. [Google Scholar] [CrossRef]
- Velasco-Ortega, E.; Jiménez-Guerra, A.; Ortiz-Garcia, I.; Moreno-Muñoz, J.; Núñez-Márquez, E.; Cabanillas-Balsera, D.; López-López, J.; Monsalve-Guil, L. Immediate Loading of Implants Placed by Guided Surgery in Geriatric Edentulous Mandible Patients. Int. J. Environ. Res. Public Health 2021, 18, 4125. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef]
- La Monaca, G.; Pranno, N.; Annibali, S.; Di Carlo, S.; Pompa, G.; Cristalli, M.P. Immediate flapless full-arch rehabilitation of edentulous jaws on 4 or 6 implants according to the prosthetic-driven planning and guided implant surgery: A retrospective study on clinical and radiographic outcomes up to 10 years of follow-up. Clin. Implant. Dent. Relat. Res. 2022, 24, 831–844. [Google Scholar] [CrossRef]
- Spagnuolo, G.; Sorrentino, R. The Role of Digital Devices in Dentistry: Clinical Trends and Scientific Evidences. J. Clin. Med. 2020, 9, 1692. [Google Scholar] [CrossRef]
- Huang, S.; Wei, H.; Li, D. Additive manufacturing technologies in the oral implant clinic: A review of current applications and progress. Front. Bioeng. Biotechnol. 2023, 11, 1100155. [Google Scholar] [CrossRef] [PubMed]
- Goguta, L.; Lungeanu, D.; Negru, R.; Birdeanu, M.; Jivanescu, A.; Sinescu, C. Selective Laser Sintering versus Selective Laser Melting and Computer Aided Design—Computer Aided Manufacturing in Double Crowns Retention. J. Prosthodont. Res. 2021, 65, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Doyle, D.J.; Hendrix, J.M.; Garmon, E.H. American Society of Anesthesiologists Classification. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Aminoshariae, A.; Mackey, S.A.; Palomo, L.; Kulild, J.C. Declassifying Mobility Classification. J. Endod. 2020, 46, 1539–1544. [Google Scholar] [CrossRef] [PubMed]
- Del Giudice, R.; Piattelli, A.; Grande, N.; Cataneo, E.; Crispino, A.; Petrini, M. Implant insertion torque value in immediate loading: A retrospective study. Med. Oral Patol. Oral Cirugia Bucal 2019, 24, e398–e403. [Google Scholar] [CrossRef] [PubMed]
- Comuzzi, L.; Tumedei, M.; Di Pietro, N.; Romasco, T.; Hossein, H.H.S.; Montesani, L.; Inchingolo, F.; Piattelli, A.; Covani, U. A Comparison of Conical and Cylindrical Implants Inserted in an in Vitro Post-Extraction Model Using Low-Density Polyurethane Foam Blocks. Materials 2023, 16, 5064. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.-S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef]
- Gong, G.; Ye, J.; Chi, Y.; Zhao, Z.; Wang, Z.; Xia, G.; Du, X.; Tian, H.; Yu, H.; Chen, C. Research status of laser additive manufacturing for metal: A review. J. Mater. Res. Technol. 2021, 15, 855–884. [Google Scholar] [CrossRef]
- Konieczny, B.; Szczesio-Wlodarczyk, A.; Sokolowski, J.; Bociong, K. Challenges of Co–Cr Alloy Additive Manufacturing Methods in Dentistry—The Current State of Knowledge (Systematic Review). Materials 2020, 13, 3524. [Google Scholar] [CrossRef]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review. Int. J. Environ. Res. Public Health 2022, 19, 3331. [Google Scholar] [CrossRef] [PubMed]
- Stamenković, D.; Popović, M.; Rudolf, R.; Zrilić, M.; Raić, K.; Đuričić, K.O.; Stamenković, D. Comparative Study of the Microstructure and Properties of Cast-Fabricated and 3D-Printed Laser-Sintered Co–Cr Alloys for Removable Partial Denture Frameworks. Materials 2023, 16, 3267. [Google Scholar] [CrossRef] [PubMed]
- Svanborg, P.; Eliasson, A.; Stenport, V. Additively Manufactured Titanium and Cobalt-Chromium Implant Frameworks: Fit and Effect of Ceramic Veneering. Int. J. Oral Maxillofac. Implant. 2018, 33, 590–596. [Google Scholar] [CrossRef] [PubMed]
- Ucar, Y.; Akova, T.; Akyil, M.S.; Brantley, W.A. Internal fit evaluation of crowns prepared using a new dental crown fabrication technique: Laser-sintered Co-Cr crowns. J. Prosthet. Dent. 2009, 102, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Altintas, M.A.; Akin, H. Effect of repetitive firing on passive fit of metal substructure produced by the laser sintering in implant-supported fixed prosthesis. J. Adv. Prosthodont. 2020, 12, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Kligman, S.; Ren, Z.; Chung, C.-H.; Perillo, M.A.; Chang, Y.-C.; Koo, H.; Zheng, Z.; Li, C. The Impact of Dental Implant Surface Modifications on Osseointegration and Biofilm Formation. J. Clin. Med. 2021, 10, 1641. [Google Scholar] [CrossRef] [PubMed]
- Pandey, C.; Rokaya, D.; Bhattarai, B.P. Contemporary Concepts in Osseointegration of Dental Implants: A Review. BioMed Res. Int. 2022, 2022, 6170452. [Google Scholar] [CrossRef] [PubMed]
- Accioni, F.; Vázquez, J.; Merinero, M.; Begines, B.; Alcudia, A. Latest Trends in Surface Modification for Dental Implantology: Innovative Developments and Analytical Applications. Pharmaceutics 2022, 14, 455. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry—State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef]
- Wersényi, G.; Scheper, V.; Spagnol, S.; Eixelberger, T.; Wittenberg, T. Cost-effective 3D scanning and printing technologies for outer ear reconstruction: Current status. Head Face Med. 2023, 19, 46. [Google Scholar] [CrossRef]
- Lupi, S.M.; Todaro, C.; De Martis, D.; Blasi, P.; Baena, R.R.Y.; Storelli, S. The Conometric Connection for the Implant-Supported Fixed Prosthesis: A Narrative Review. Prosthesis 2022, 4, 458–467. [Google Scholar] [CrossRef]
- Ahmed, N.; Abbasi, M.S.; Zuberi, F.; Qamar, W.; Bin Halim, M.S.; Maqsood, A.; Alam, M.K. Artificial Intelligence Techniques: Analysis, Application, and Outcome in Dentistry—A Systematic Review. BioMed Res. Int. 2021, 2021, 9751564. [Google Scholar] [CrossRef] [PubMed]
- Di Giacomo, G.d.A.; Cury, P.R.; da Silva, A.M.; da Silva, J.V.; Ajzen, S.A. Surgical guides for flapless dental implant placement and immediate definitive prosthesis installation by using selective laser melting and sintering for 3D metal and polymer printing: A clinical report. J. Prosthet. Dent. 2022. [Google Scholar] [CrossRef]
- Venezia, P.; Torsello, F.; Santomauro, V.; Dibello, V.; Cavalcanti, R. Full Digital Workflow for the Treatment of an Edentulous Patient with Guided Surgery, Immediate Loading and 3D-Printed Hybrid Prosthesis: The BARI Technique 2.0. A Case Report. Int. J. Environ. Res. Public Health 2019, 16, 5160. [Google Scholar] [CrossRef] [PubMed]












Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Todaro, C.; Cerri, M.; Rodriguez y Baena, R.; Lupi, S.M. Lower Jaw Full-Arch Restoration: A Completely Digital Approach to Immediate Load. Healthcare 2024, 12, 332. https://doi.org/10.3390/healthcare12030332
Todaro C, Cerri M, Rodriguez y Baena R, Lupi SM. Lower Jaw Full-Arch Restoration: A Completely Digital Approach to Immediate Load. Healthcare. 2024; 12(3):332. https://doi.org/10.3390/healthcare12030332
Chicago/Turabian StyleTodaro, Claudia, Michael Cerri, Ruggero Rodriguez y Baena, and Saturnino Marco Lupi. 2024. "Lower Jaw Full-Arch Restoration: A Completely Digital Approach to Immediate Load" Healthcare 12, no. 3: 332. https://doi.org/10.3390/healthcare12030332
APA StyleTodaro, C., Cerri, M., Rodriguez y Baena, R., & Lupi, S. M. (2024). Lower Jaw Full-Arch Restoration: A Completely Digital Approach to Immediate Load. Healthcare, 12(3), 332. https://doi.org/10.3390/healthcare12030332








