Impact of COVID-19 on Perinatal Outcomes and Birth Locations in a Large US Metropolitan Area
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Sources
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Maternal Delivery Indication and Outcomes
3.2. Changes in Birth Location by Hospital Designation
3.3. Hospital Length of Stay
4. Discussion
4.1. Shifts in Birth Location by Hospital Designation
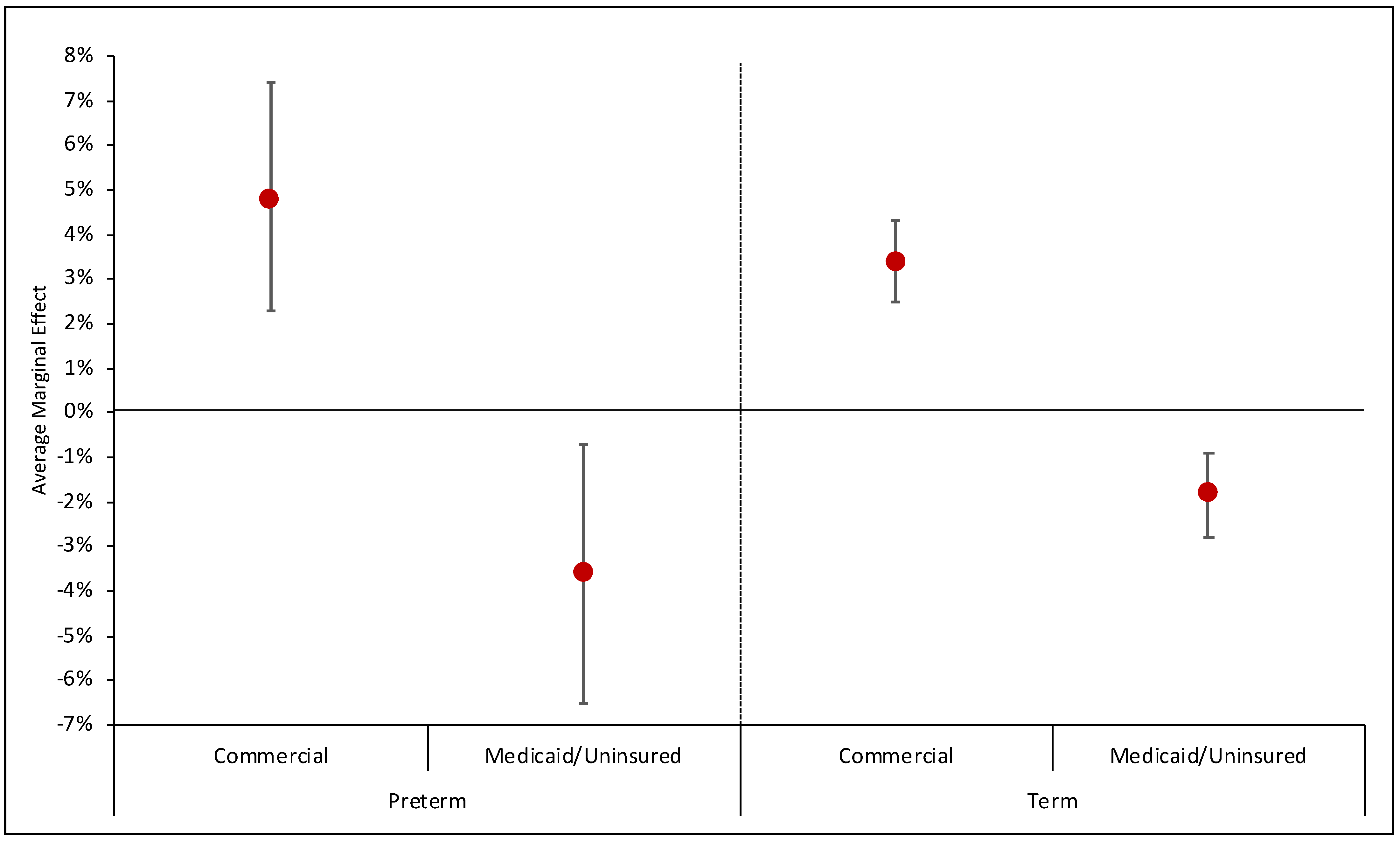
4.2. Inequity
4.3. Hospital Length of Stay
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hedley, P.L.; Hedermann, G.; Hagen, C.M.; Bækvad-Hansen, M.; Hjalgrim, H.; Rostgaard, K.; Laksafoss, A.D.; Hoffmann, S.; Jensen, J.S.; Breindahl, M.; et al. Preterm birth, stillbirth and early neonatal mortality during the Danish COVID-19 lockdown. Eur. J. Pediatr. 2022, 181, 1175–1184. [Google Scholar] [CrossRef]
- Hedermann, G.; Hedley, P.L.; Bækvad-Hansen, M.; Hjalgrim, H.; Rostgaard, K.; Poorisrisak, P.; Breindahl, M.; Melbye, M.; Hougaard, D.M.; Christiansen, M.; et al. Danish premature birth rates during the COVID-19 lockdown. Arch. Dis. Child. Fetal Neonatal Ed. 2021, 106, 93–95. [Google Scholar] [CrossRef] [PubMed]
- Leibovitch, L.; Reichman, B.; Mimouni, F.; Zaslavsky-Paltiel, I.; Lerner-Geva, L.; Wasserteil, N.; Sagiv, N.; Daas, S.; Almashanu, S.; Strauss, T. Preterm singleton birth rate during the COVID-19 lockdown: A population-based study. Am. J. Perinatol. 2022, 39, 1020–1026. [Google Scholar] [CrossRef] [PubMed]
- Mølholm Hansen, B.; Cueto, H.; Padkaer Petersen, J.; Zachariassen, G.; Sønderby Christensen, P.; Breindahl, M.; Schiøler Kesmodel, U.; Brink Henriksen, T. Preterm birth rates were slightly lower in Denmark during the first year of the COVID-19 pandemic compared with the previous 4 years. Acta Paediatr. 2022, 111, 1695–1700. [Google Scholar] [CrossRef] [PubMed]
- Been, J.V.; Ochoa, L.B.; Bertens, L.C.M.; Schoenmakers, S.; Steegers, E.A.P.; Reiss, I.K.M. Impact of COVID-19 mitigation measures on the incidence of preterm birth: A national quasi-experimental study. Lancet Public Health 2020, 5, e604–e611. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.; Moon, S.; Cho, K.D.; Oh, M.J.; Hong, S.J.; Cho, G.J. Changes in preterm birth and birthweight during the SARS-CoV-2 pandemic: A nationwide study in South Korea. Sci. Rep. 2022, 12, 16288. [Google Scholar] [CrossRef] [PubMed]
- Oakley, L.L.; Örtqvist, A.K.; Kinge, J.; Hansen, A.V.; Petersen, T.G.; Söderling, J.; Telle, K.E.; Magnus, M.C.; Mortensen, L.H.; Andersen, A.-M.N.; et al. Preterm birth after the introduction of COVID-19 mitigation measures in Norway, Sweden, and Denmark: A registry-based difference-in-differences study. Am. J. Obstet. Gynecol. 2022, 226, 550.e1–550.e22. [Google Scholar] [CrossRef] [PubMed]
- Pasternak, B.; Neovius, M.; Söderling, J.; Ahlberg, M.; Norman, M.; Ludvigsson, J.F.; Stephansson, O. Preterm birth and stillbirth during the COVID-19 pandemic in Sweden: A nationwide cohort study. Ann. Intern. Med. 2021, 174, 873–875. [Google Scholar] [CrossRef]
- Simpson, A.N.; Snelgrove, J.W.; Sutradhar, R.; Everett, K.; Liu, N.; Baxter, N.N. Perinatal outcomes during the COVID-19 pandemic in Ontario, Canada. JAMA Netw. Open 2021, 4, e2110104. [Google Scholar] [CrossRef] [PubMed]
- Mullin, A.M.; Handley, S.C.; Lundsberg, L.; Elovitz, M.A.; Lorch, S.A.; McComb, E.J.; Montoya-Williams, D.; Yang, N.; Dysart, K.; Son, M.; et al. Changes in preterm birth during the COVID-19 pandemic by duration of exposure and race and ethnicity. J. Perinatol. 2022, 42, 1346–1352. [Google Scholar] [CrossRef]
- Handley, S.C.; Mullin, A.M.; Elovitz, M.A.; Gerson, K.D.; Montoya-Williams, D.; Lorch, S.A.; Burris, H.H. Changes in Preterm Birth Phenotypes and Stillbirth at 2 Philadelphia Hospitals During the SARS-CoV-2 Pandemic, March–June 2020. JAMA 2021, 325, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Wood, R.; Sinnott, C.; Goldfarb, I.; Clapp, M.; McElrath, T.; Little, S. Preterm birth during the Coronavirus Disease 2019 (COVID-19) pandemic in a large hospital system in the United States. Obstet. Gynecol. 2021, 137, 403–404. [Google Scholar] [CrossRef] [PubMed]
- Berghella, V.; Boelig, R.; Roman, A.; Burd, J.; Anderson, K. Decreased incidence of preterm birth during coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. MFM 2020, 2, 100258. [Google Scholar] [CrossRef] [PubMed]
- Molina, R.L.; Tsai, T.C.; Dai, D.; Soto, M.; Rosenthal, N.; Orav, E.J.; Figueroa, J.F. Comparison of pregnancy and birth outcomes before vs during the COVID-19 pandemic. JAMA Netw. Open 2022, 5, e2226531. [Google Scholar] [CrossRef] [PubMed]
- Simeone, R.M.; Downing, K.F.; Wallace, B.; Galang, R.R.; DeSisto, C.L.; Tong, V.T.; Zapata, L.B.; Ko, J.Y.; Ellington, S.R. Changes in rates of adverse pregnancy outcomes during the COVID-19 pandemic: A cross-sectional study in the United States, 2019–2020. J. Perinatol. 2022, 42, 617–623. [Google Scholar] [CrossRef]
- Chen, J.; Ferre, C.; Ouyang, L.; Mohamoud, Y.; Barfield, W.; Cox, S. Changes and geographic variation in rates of preterm birth and stillbirth during the prepandemic period and COVID-19 pandemic, according to health insurance claims in the United States, April–June 2019 and April–June 2020. Am. J. Obstet. Gynecol. MFM 2022, 4, 100508. [Google Scholar] [CrossRef]
- Dench, D.; Joyce, T.; Minkoff, H. United States Preterm Birth Rate and COVID-19. Pediatrics 2022, 149, e2021055495. [Google Scholar] [CrossRef]
- Hwang, S.S.; Weikel, B.W.; Hannan, K.E.; Bourque, S.L. Impact of Coronavirus Disease-19 “stay-at-home” orders on preterm birth in Colorado. J. Pediatr. 2022, 242, 238–241.e1. [Google Scholar] [CrossRef]
- Harvey, E.M.; McNeer, E.; McDonald, M.F.; Shapiro-Mendoza, C.K.; Dupont, W.D.; Barfield, W.; Patrick, S.W. Association of preterm birth rate with COVID-19 statewide stay-at-home orders in Tennessee. JAMA Pediatr. 2021, 175, 635–637. [Google Scholar] [CrossRef] [PubMed]
- Gemmill, A.; Casey, J.A.; Catalano, R.; Karasek, D.; Margerison, C.E.; Bruckner, T. Changes in preterm birth and caesarean deliveries in the United States during the SARS-CoV-2 pandemic. Paediatr. Perinat. Epidemiol. 2022, 36, 485–489. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau. American Community Survey 5-Year Estimates Data Profiles. 2019. Available online: https://data.census.gov/cedsci/table?tid=ACSDP5Y2019.DP05&g=310XX00US35620 (accessed on 10 December 2021).
- Walani, S.R. Global burden of preterm birth. Int. J. Gynaecol. Obstet. 2020, 150, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Khalil, A.; von Dadelszen, P.; Draycott, T.; Ugwumadu, A.; O’brien, P.; Magee, L. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA 2020, 324, 705–706. [Google Scholar] [CrossRef] [PubMed]
- Philip, R.K.; Purtill, H.; Reidy, E.; Daly, M.; Imcha, M.; McGrath, D.; O’Connell, N.H.; Dunne, C.P. Unprecedented reduction in births of very low birthweight (VLBW) and extremely low birthweight (ELBW) infants during the COVID-19 lockdown in Ireland: A ‘natural experiment’ allowing analysis of data from the prior two decades. BMJ Glob. Health 2020, 5, e003075. [Google Scholar] [CrossRef] [PubMed]
- Calvert, C.; Brockway, M.; Zoega, H.; Miller, J.E.; Been, J.V.; Amegah, A.K.; Racine-Poon, A.; Oskoui, S.E.; Abok, I.I.; Aghaeepour, N.; et al. Changes in preterm birth and stillbirth during COVID-19 lockdowns in 26 countries. Nat. Hum. Behav. 2023, 7, 529–544. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, N.N.; Pednekar, R.; Gaikwad, C.; More, P.; Pophalkar, M.; Kesarwani, S.; Jnanananda, B.; Mahale, S.D.; Gajbhiye, R.K. Increased spontaneous preterm births during the second wave of the coronavirus disease 2019 pandemic in India. Int. J. Gynecol. Obstet. 2022, 157, 115–120. [Google Scholar] [CrossRef]
- Fresson, J.; Bruckner, T.A.; Le Ray, C.; Goffinet, F.; Rey, S.; Blondel, B.; Deneux-Tharaux, C.; Ancel, P.-Y.; Zeitlin, J. Decreases in preterm birth during the first COVID-19 lockdown in France by gestational age sub-groups and regional COVID-19 incidence. Ann. Epidemiol. 2022, 72, 74–81. [Google Scholar] [CrossRef]
- De Curtis, M.; Villani, L.; Polo, A. Increase of stillbirth and decrease of late preterm infants during the COVID-19 pandemic lockdown. Arch. Dis. Child. Fetal Neonatal Ed. 2021, 106, 456. [Google Scholar] [CrossRef]
- Hui, L.; Marzan, M.B.; Potenza, S.; Rolnik, D.L.; Pritchard, N.; Said, J.M.; Palmer, K.R.; Whitehead, C.L.; Sheehan, P.M.; Ford, J.; et al. Increase in preterm stillbirths in association with reduction in iatrogenic preterm births during COVID-19 lockdown in Australia: A multicenter cohort study. Am. J. Obstet. Gynecol. 2022, 227, 491.e1–491.e17. [Google Scholar] [CrossRef]
- Thoma, M.E.; Drew, L.B.; Hirai, A.H.; Kim, T.Y.; Fenelon, A.; Shenassa, E.D. Black-White Disparities in Preterm Birth: Geographic, Social, and Health Determinants. Am. J. Prev. Med. 2019, 57, 675–686. [Google Scholar] [CrossRef]
- DeFranco, E.A.; Hall, E.S.; Muglia, L.J. Racial disparity in previable birth. Am. J. Obstet. Gynecol. 2016, 214, 394.e1–394.e7. [Google Scholar] [CrossRef]
- Manuck, T.A. Racial and ethnic differences in preterm birth: A complex, multifactorial problem. Semin. Perinatol. 2017, 41, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Magesh, S.; John, D.; Li, W.T.; Li, Y.; Mattingly-App, A.; Jain, S.; Chang, E.Y.; Ongkeko, W.M. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: A systematic-review and meta-analysis. JAMA Netw. Open 2021, 4, e2134147. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, E.; Gulersen, M.; Husk, G.; Grunebaum, A.; Blitz, M.J.; Rafael, T.J.; Rochelson, B.L.; Schwartz, B.; Nimaroff, M.; Chervenak, F.A. Early postpartum discharge during the COVID-19 pandemic. J. Perinat. Med. 2020, 48, 1008–1012. [Google Scholar] [CrossRef] [PubMed]
- Gulersen, M.; Husk, G.; Lenchner, E.; Blitz, M.J.; Rafael, T.J.; Rochelson, B.; Chakravarthy, S.; Grunebaum, A.; Chervenak, F.A.; Fruhman, G.; et al. The risk of readmission after early postpartum discharge during the COVID-19 pandemic. Am. J. Perinatol. 2022, 39, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Handley, S.C.; Gallagher, K.; Breden, A.; Lindgren, E.; Lo, J.Y.; Son, M.; Murosko, D.; Dysart, K.; Lorch, S.A.; Greenspan, J.; et al. Birth hospital length of stay and rehospitalization during COVID-19. Pediatrics 2022, 149, e2021053498. [Google Scholar] [CrossRef]
- Mollard, E.; Wittmaack, A. Experiences of Women Who Gave Birth in US Hospitals During the COVID-19 Pandemic. J. Patient Exp. 2021, 8, 2374373520981492. [Google Scholar] [CrossRef] [PubMed]
- Marino, L.V.; Collaço, N.; Johnson, M.J.; Darlington, A. Preterm birth during the COVID-19 pandemic: Parental experience. Acta Paediatr. 2022, 111, 772–773. [Google Scholar] [CrossRef]
- Shuman, C.J.; Morgan, M.E.; Chiangong, J.; Pareddy, N.; Veliz, P.; Peahl, A.F.; Dalton, V.K. “Mourning the experience of what should have been”: Experiences of peripartum women during the COVID-19 pandemic. Matern. Child Health J. 2022, 26, 102–109. [Google Scholar] [CrossRef]
- Jones, E.; Stewart, F.; Taylor, B.; Davis, P.G.; Brown, S.J. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database Syst. Rev. 2021, 6, CD002958. [Google Scholar] [CrossRef]
- Gregory, E.C.W.; Osterman, M.J.K.; Valenzuela, C.P. Changes in home births by race and hispanic origin and state of residence of mother: United States, 2018–2019 and 2019–2020. Natl. Vital. Stat. Rep. 2021, 70, 1–10. [Google Scholar] [PubMed]
- MacDorman, M.F.; Declercq, E. Trends and state variations in out-of-hospital births in the United States, 2004–2017. Birth 2019, 46, 279–288. [Google Scholar] [CrossRef] [PubMed]


| Pre-COVID-19 April–September 2019 N = 47,068 | During COVID-19 April–September 2020 N = 43,270 | p-Value | |
|---|---|---|---|
| Male, n (%) | 24,212 (51.4) | 22,165 (51.2) | 0.517 |
| Primary payer, n (%) | <0.001 | ||
| Commercial | 26,888 (57.1) | 23,516 (54.4) | |
| Medicaid/uninsured | 19,803 (42.1) | 19,476 (45.0) | |
| Other | 377 (0.8) | 278 (0.6) | |
| Race/ethnicity, n (%) | <0.001 | ||
| Asian | 2772 (5.9) | 2657 (6.1) | |
| Black | 7062 (14.9) | 6329 (14.5) | |
| Hispanic | 9147 (19.3) | 9115 (20.9) | |
| White | 17,907 (37.8) | 17,698 (40.6) | |
| Other | 10,488 (22.1) | 7756 (17.8) | |
| Gestational age, n (%) | 0.263 | ||
| <28 weeks | 270 (0.6) | 215 (0.5) | |
| 28–<32 weeks | 352 (0.8) | 333 (0.8) | |
| 32–<37 weeks | 3758 (8.0) | 3365 (7.8) | |
| 37 weeks or older | 42,679 (90.7) | 39,338 (91.0) | |
| <32 weeks gestational age born at hospital with inappropriate level of NICU care, n (%) | 62/622 (10.0) | 57/548 (10.4) | 0.807 |
| All infants transferred to another facility, n (%) | 479 (1.0) | 388 (0.9) | 0.062 |
| In-hospital death, n (%) | 125 (0.3) | 103 (0.2) | 0.410 |
| Neighborhood characteristics | |||
| Concentrated poverty, >20% below federal poverty level, n (%) | 7272 (15.5) | 6696 (15.5) | 0.918 |
| % population working, mean (sd) | 67.3 (6.6) | 67.4 (6.6) | 0.052 |
| % housing units crowded (more than 1 person per room), mean (sd) | 3.2 (2.4) | 3.2 (2.4) | 0.042 |
| % households without a computer, mean (sd) | 9.4 (5.6) | 9.3 (5.5) | 0.054 |
| % population age 25 and older with high school degree or more, mean (sd) | 87.3 (9.3) | 87.4 (9.3) | 0.139 |
| N (%) | Adjusted | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Pre-COVID-19 n (%) | During COVID-19 n (%) | p-Value * | OR (95% CI) | p-Value ** | Marginal Effect | |||
| Predictive Margin | Average Marginal Effect (%) (95% CI) | ||||||||
| Pre-COVID-19 Prob (95% CI) | During COVID-19 Prob (95% CI) | ||||||||
| Stillbirth/IUFD | 90,931 | 308 (0.7) | 285 (0.7) | 0.937 | 1.00 (0.85, 1.18) | 0.971 | 0.7 (0.6, 0.7) | 0.7 (0.6, 0.7) | 0.0 (−0.1 to 0.1) |
| Preterm Birth | 90,338 | 4389 (9.3) | 3932 (9.1) | 0.217 | 0.98 (0.94, 1.03) | 0.442 | 9.3 (9.0, 9.6) | 9.1 (8.8, 9.4) | −0.1 (−0.5, 0.2) |
| Birth Category | 90,051 | 0.502 | |||||||
| Indicated Preterm | 2465 | 1288 (2.8) | 1177 (2.7) | 0.99 (0.92, 1.07) | 0.761 | 2.7 (2.6, 2.9) | 2.7 (2.6, 2.9) | −0.0 (−0.2 to 0.2) | |
| Spontaneous Preterm | 4445 | 2341 (5.0) | 2104 (4.9) | 0.97 (0.91, 1.03) | 0.268 | 5.0 (4.8, 5.2) | 4.9 (4.7, 5.1) | −0.2 (−0.4 to 0.1) | |
| Unspecified Preterm | 1583 | 841 (1.8) | 742 (1.7) | 0.95 (0.86, 1.04) | 0.277 | 1.8 (1.7, 1.9) | 1.7 (1.6, 1.8) | −0.1 (−0.3 to 0.1) | |
| Term | 81,558 | 42,259 (90.4) | 39,299 (90.7) | REF | 90.4 (90.2, 90.7) | 90.7 (90.5, 91.0) | −0.2 (−0.7 to 0.6) | ||
| AMC Birth Location | 90,338 | 9997 (21.2) | 9791 (22.6) | <0.001 | 1.07 (1.03, 1.12) | 0.002 | 21.4 (18.8, 24.1) | 22.4 (19.7, 25.1) | 1.0 (0.4, 1.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, E.G.; Perez, A.; Patel, A.; Patel, A.L.; Waters, T.; Fricchione, M.; Johnson, T.J. Impact of COVID-19 on Perinatal Outcomes and Birth Locations in a Large US Metropolitan Area. Healthcare 2024, 12, 340. https://doi.org/10.3390/healthcare12030340
Lee EG, Perez A, Patel A, Patel AL, Waters T, Fricchione M, Johnson TJ. Impact of COVID-19 on Perinatal Outcomes and Birth Locations in a Large US Metropolitan Area. Healthcare. 2024; 12(3):340. https://doi.org/10.3390/healthcare12030340
Chicago/Turabian StyleLee, Esther G., Alejandra Perez, Arth Patel, Aloka L. Patel, Thaddeus Waters, Marielle Fricchione, and Tricia J. Johnson. 2024. "Impact of COVID-19 on Perinatal Outcomes and Birth Locations in a Large US Metropolitan Area" Healthcare 12, no. 3: 340. https://doi.org/10.3390/healthcare12030340






