Development and Implementation of a Mobile-Integrated Simulation for COVID-19 Nursing Practice: A Randomized Controlled Pretest–Posttest Experimental Design
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
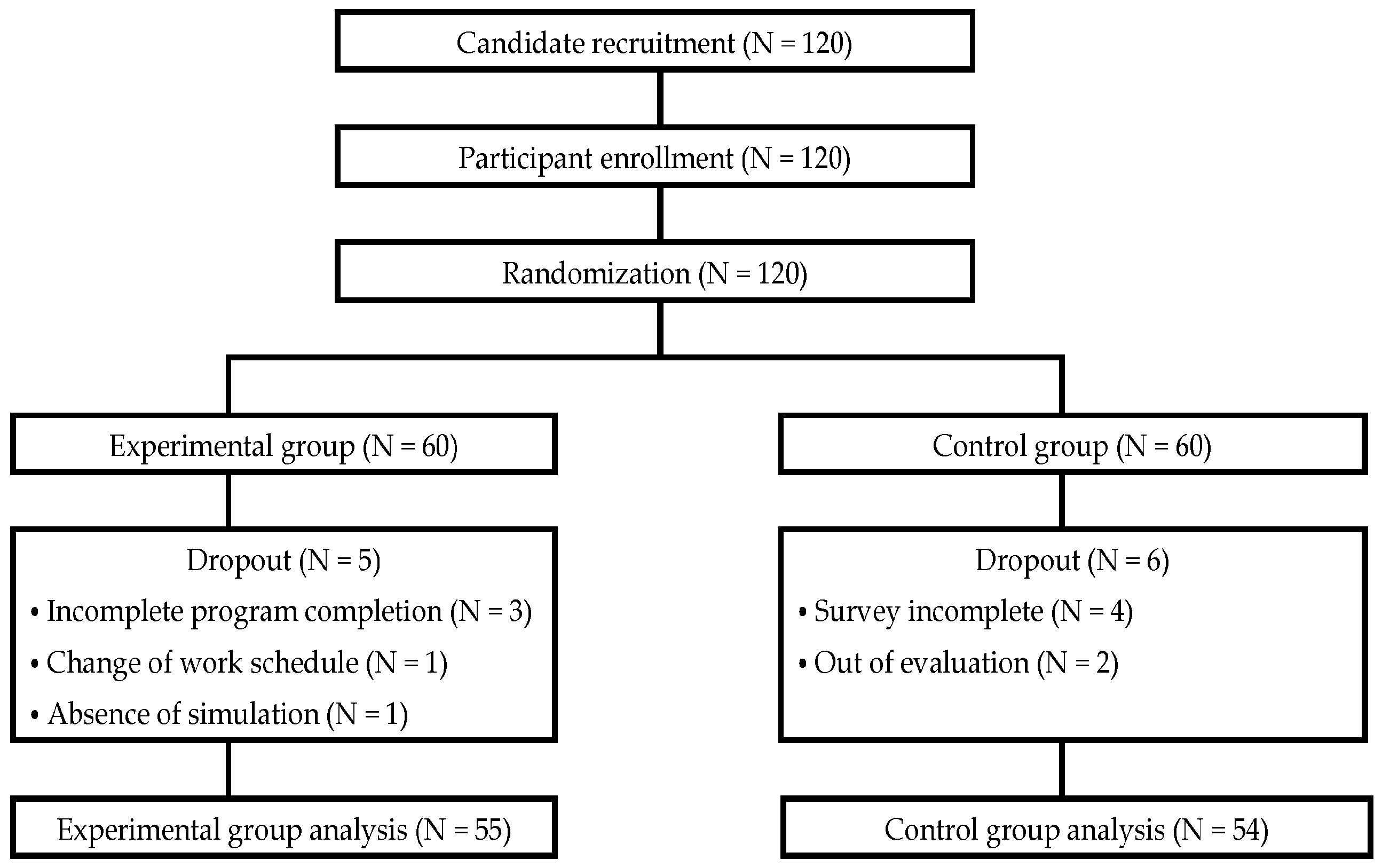
2.2. Participants and Recruitment
2.3. Randomization and Blinding
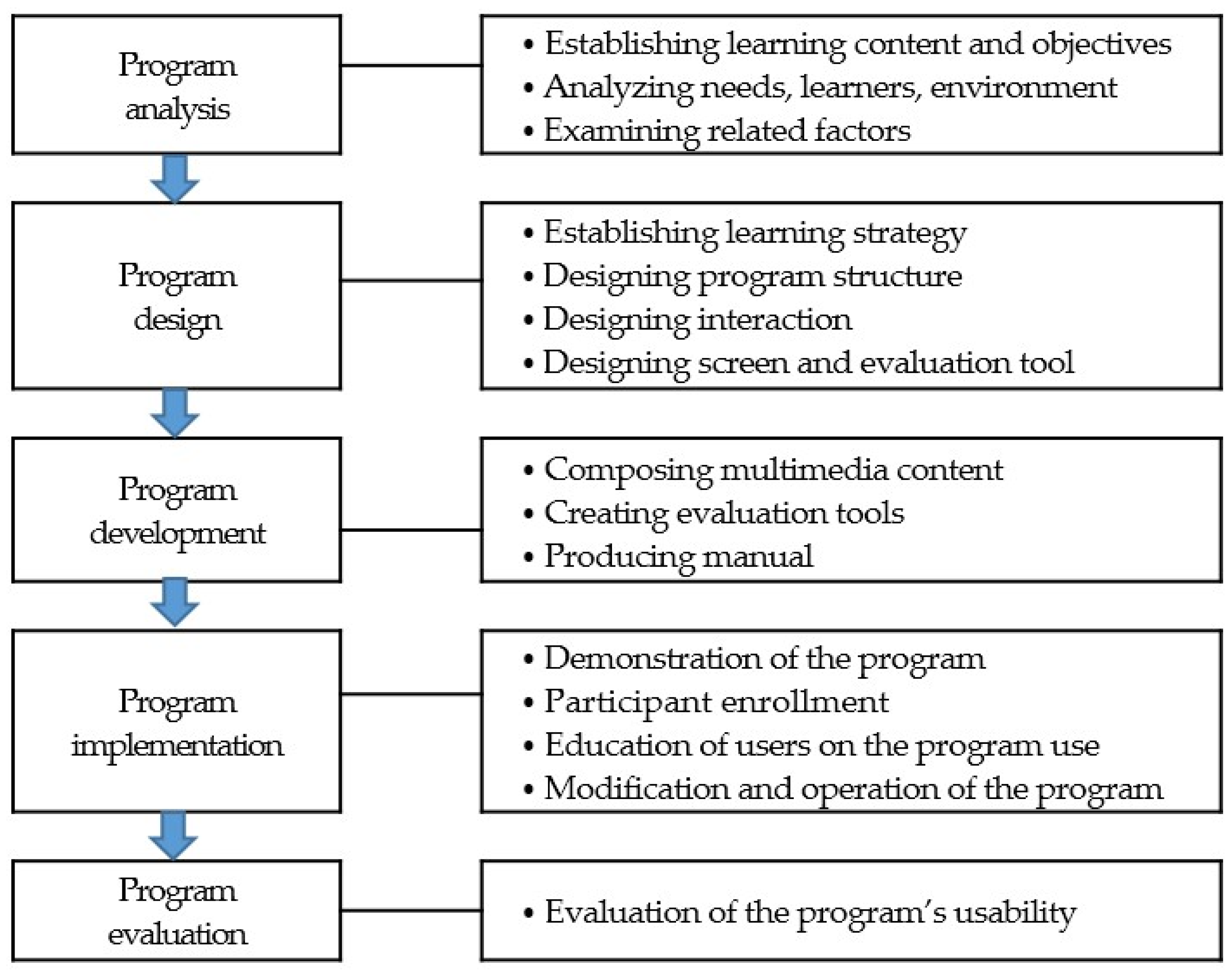
2.4. Mobile Education Program
2.5. Measurements
2.5.1. COVID-19 Knowledge
2.5.2. Infection Prevention Practice Confidence
2.5.3. Clinical Decision-Making Confidence and Anxiety
2.6. High-Fidelity Simulation Training
2.7. Statistical Approach
3. Results
3.1. General Characteristics and Baseline Homogeneity
3.2. Effectiveness of Mobile-Integrated COVID-19 Nursing Practice Simulation Program
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease (COVID-19). 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 3 April 2020).
- Lee, S.; Choi, J.S. Factors influencing COVID-19 AstraZeneca (ChAdOx1) vaccination and side effects among health care workers in an acute general hospital. J. Korean Biol. Nurs. Sci. 2021, 23, 318–329. [Google Scholar] [CrossRef]
- Central Accident Investigation Headquarters, Central Discharge Countermeasures Headquarters. Promote the Securing of COVID-19 Beds in the Metropolitan Area in Response to the Increase in Patients. (13 August 2021, Regular Briefing). Available online: https://www.mohw.go.kr/react/al/sal0301ls.jsp (accessed on 13 October 2021).
- Monesi, A.; Imbriaco, G.; Mazzoli, C.A.; Giugni, A.; Ferrari, P. In-Situ simulation for intensive care nurses during the COVID-19 pandemic in Italy: Advantages and challenges. Clin. Simul. Nurs. 2022, 62, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; De Los Santos, J.A.A. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 2020, 28, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Schwerdtle, P.N.; Connell, C.J.; Lee, S.; Plummer, V.; Russo, P.L.; Endacott, R.; Kuhn, L. Nurse expertise: A critical resource in the COVID-19 pandemic response. Ann. Glob. Health 2020, 86, 49. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.; Im, J.; Kang, H.Y. Priority analysis of needs for COVID-19 infection control education for nurses at a medium-sized hospital. J. Korean Acad. Fundam. Nurs. 2022, 29, 472–483. [Google Scholar] [CrossRef]
- Ni, J.; Wu, P.; Huang, X.; Zhang, F.; You, Z.; Chang, Q.; Liao, L. Effects of five teaching methods in clinical nursing teaching: A protocol for systematic review and network meta-analysis. PLoS ONE 2022, 17, e0273693. [Google Scholar] [CrossRef] [PubMed]
- Hwang, W.J.; Lee, J. Effectiveness of the infectious disease (COVID-19) simulation module program on nursing students: Disaster nursing scenarios. J. Korean Acad. Nurs. 2021, 51, 648–660. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.B.; Choi, J.S. Effect of an isolation-coping programme on patients isolated for colonization or infection with multi-drug-resistant organisms: A quasi-experimental study. J. Hosp. Infect. 2022, 129, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Kanaki, K.; Kalogiannakis, M. Sample design challenges: An educational research paradigm. Int. J. Technol. Enhanc. Learn. 2023, 15, 266–285. [Google Scholar] [CrossRef]
- KCDC. MERS Response Guidelines in 5-1 ed. 2018. Available online: http://www.icdc.incheon.kr/upload/20180702140219123.pdf (accessed on 2 November 2023).
- KCDC. Ebola Virus Response Guidelines in 7 ed. 2017. Available online: http://www.gbcidc.or.kr/file/download.do?file_id=246 (accessed on 2 November 2023).
- Taghrir, M.H.; Borazjani, R.; Shiraly, R. COVID-19 and Iranian medical students; a survey on their related-knowledge, preventive behaviors and risk perception. Arch. Iran. Med. 2020, 23, 249–254. [Google Scholar] [CrossRef]
- Lee, S.J.; Jin, X.L.; Lee, S. Factors influencing COVID-19 preventive behaviors in nursing students: Knowledge, risk perception, anxiety, and depression. J. Korean Biol. Nurs. Sci. 2021, 23, 110–118. [Google Scholar] [CrossRef]
- Central Accident Investigation Headquarters, Central Discharge Countermeasures Headquarters. Coronavirus Disease-19 Response Manual (for Municipal). In 10-2 ed. 2021. Available online: http://ncov.mohw.go.kr/upload/viewer/skin/doc.html?fn=1637821171779_20211125151934.pdf&rs=/upload/viewer/result/202112/ (accessed on 2 November 2023).
- Polit, D.F.; Beck, C.T. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef]
- White, K.A. Development and validation of a tool to measure self-confidence and anxiety in nursing students during clinical decision making. J. Nurs. Educ. 2014, 53, 14–22. [Google Scholar] [CrossRef]
- Yu, M.; Eun, Y.; White, K.A.; Kang, K.J. Reliability and validity of Korean version of Nursing Students’ Anxiety and Self-Confidence with Clinical Decision Making Scale. J. Korean Acad. Nurs. 2019, 49, 411–422. [Google Scholar] [CrossRef]
- Ingrassia, P.L.; Ferrari, M.; Paganini, M.; Mormando, G. Role of health simulation centres in the COVID-19 pandemic response in Italy: A national study. BMJ Simul. Technol. Enhanc. Learn. 2021, 7, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Zehler, A.; Cole, B.; Arter, S. Hyflex simulation: A case study of a creative approach to unprecedented circumstances. Clin. Simul. Nurs. 2021, 60, 64–68. [Google Scholar] [CrossRef]
- Aldekhyl, S.S.; Arabi, Y.M. Simulation role in preparing for COVID-19. Ann. Thorac. Med. 2020, 15, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Suppan, L.; Abbas, M.; Stuby, L.; Cottet, P.; Larribau, R.; Golay, E.; Iten, A.; Harbarth, S.; Gartner, B.; Suppan, M. Effect of an e-learning module on personal protective equipment proficiency among prehospital personnel: Web-based randomized controlled trial. J. Med. Internet Res. 2020, 22, e21265. [Google Scholar] [CrossRef]
- Kasai, H.; Saito, G.; Ito, S.; Kuriyama, A.; Kawame, C.; Shikino, K.; Takeda, K.; Yahaba, M.; Taniguchi, T.; Igari, H.; et al. COVID-19 infection control education for medical students undergoing clinical clerkship: A mixed-method approach. BMC Med. Educ. 2022, 22, 453. [Google Scholar] [CrossRef] [PubMed]
- Alzoubi, H.; Alnawaiseh, N.; Al-Mnayyis, A.; Abu-Lubad, M.; Aqel, A.; Al-Shagahin, H. COVID-19—Knowledge, attitude and practice among medical and non-medical University Students in Jordan. J. Pure Appl. Microbiol. 2020, 14, 17–24. [Google Scholar] [CrossRef]
- Puspitasari, I.M.; Yusuf, L.; Sinuraya, R.K.; Abdulah, R.; Koyama, H. Knowledge, attitude, and practice during the COVID-19 pandemic: A review. J. Multidiscip. Healthc. 2020, 13, 727–733. [Google Scholar] [CrossRef]
- Rojo, E.; Oruña, C.; Sierra, D.; García, G.; Del Moral, I.; Maestre, J.M. Simulation as a tool to facilitate practice changes in teams taking care of patients under investigation for Ebola virus disease in Spain. Simul. Healthc. 2016, 11, 89–93. [Google Scholar] [CrossRef]
- Jang, I.S.; Park, M.H. Effect of infection control education based on isolation room-simulation for nursing students. J. Korean Acad. Nurs. Adm. 2021, 27, 379–389. [Google Scholar] [CrossRef]
- Kang, J. Simulation results for contamination comparisons by various use protocols of personal protective equipment. Korean J. Med. 2018, 93, 41–49. [Google Scholar] [CrossRef]
- Woda, A.; Hansen, J.; Paquette, M.; Topp, R. The impact of simulation sequencing on perceived clinical decision making. Nurse Educ. Pract. 2017, 26, 33–38. [Google Scholar] [CrossRef]
- Higgs, J.; Jensen, G.M.; Loftus, S.; Christensen, N. (Eds.) Clinical Reasoning in the Health Professions E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Hoernke, K.; Djellouli, N.; Andrews, L.; Lewis-Jackson, S.; Manby, L.; Martin, S.; Vanderslott, S.; Vindrola-Padros, C. Frontline healthcare workers’ experiences with personal protective equipment during the COVID-19 pandemic in the UK: A rapid qualitative appraisal. BMJ Open 2021, 11, e046199. [Google Scholar] [CrossRef] [PubMed]
- Atthill, S.; Witmer, D.; Luctkar-Flude, M.; Tyerman, J. Exploring the impact of a virtual asynchronous debriefing method after a virtual simulation game to support clinical decision-making. Clin. Simul. Nurs. 2021, 50, 10–18. [Google Scholar] [CrossRef]

 Simulation Outline Simulation Outline | |
|---|---|
| Topic | COVID-19 Care |
| Learning objective | Adhere to infection control guidelines when caring for COVID-19 patients admitted to the hospital. |
| Outline |  Total duration of videos (43 min 13 s) Total duration of videos (43 min 13 s)  Mobile educational materials provided for pre-learning purposes Mobile educational materials provided for pre-learning purposes  Consists of 5 sessions Consists of 5 sessions  Orientation and sharing of scenarios Orientation and sharing of scenarios  Main simulation Main simulation On-site debriefing and reflection On-site debriefing and reflection Learners: nurses with at least 6 months of clinical experience but no experience in a COVID-19 unit Learners: nurses with at least 6 months of clinical experience but no experience in a COVID-19 unit |
| Supplies |  Space organization Space organization  Simulation room Simulation room PPE donning room PPE donning room PPE doffing room PPE doffing room Debriefing room Debriefing room  Equipment and supplies for education Equipment and supplies for education Simulator (Laerdal), body bag (corpse bag), negative pressure isolation chamber, ventilator, ventilator circuit, high-flow oxygen injector, ECG motoring machine, patient bed, disposable hospital bed cover, transparent film dressing roll, disinfecting wet wipes, gauze, medical stretcher cart, biomedical waste bin, hand sanitizer, HME ventilator filter, PPE (level D) Simulator (Laerdal), body bag (corpse bag), negative pressure isolation chamber, ventilator, ventilator circuit, high-flow oxygen injector, ECG motoring machine, patient bed, disposable hospital bed cover, transparent film dressing roll, disinfecting wet wipes, gauze, medical stretcher cart, biomedical waste bin, hand sanitizer, HME ventilator filter, PPE (level D) |
| Characteristic | Category | Experimental Group (n = 55) | Control Group (n = 54) | x2/t/Z | p | |
|---|---|---|---|---|---|---|
| n (%) or M ± SD | n (%) or M ± SD | |||||
| General characteristics | ||||||
| Sex | Male | 3 (5.5) | 0 | 3.001 * | 0.243 | |
| Female | 52 (94.5) | 54 (100) | ||||
| Marital status | Single | 47 (85.5) | 42 (77.8) | 1.072 | 0.332 | |
| Married | 8 (14.5) | 12 (22.2) | ||||
| CLS | None | 41 (74.5) | 36 (66.7) | 1.546 | 0.460 | |
| ≥CN1 | 14 (25.5) | 18(33.3) | ||||
| Age | M ± SD (years) | 27.74 ± 5.66 | 28.78 ± 5.5 | −0.856 | 0.395 | |
| <30 years | 41 (74.5) | 35 (64.8) | 2.159 * | 0.369 | ||
| 31 to <40 years | 10 (18.2) | 15 (27.8) | ||||
| ≥40 years | 4 (7.3) | 4 (7.4) | ||||
| Period of employment | M ± SD (months) | 57.63 ± 63.39 | 65.41 ± 62.47 | −1.044 | 0.301 | |
| 6 to <12 months | 10 (18.2) | 7 (13.0) | 2.252 | 0.532 | ||
| 1 to <2 years | 15 (27.3) | 10 (18.5) | ||||
| 2 to <5 years | 13 (23.6) | 15 (27.8) | ||||
| ≥5 years | 17 (30.9) | 22 (40.7) | ||||
| Duration of current employment | M ± SD (months) | 13.76 ± 5.31 | 13.72 ± 4.95 | −0.384 | 0.702 | |
| 6 to <12 months | 19 (34.5) | 19 (35.2) | 0.052 | 0.820 | ||
| 1 to <2 years | 36 (65.5) | 35 (64.8) | ||||
| Education level | Associate degree | 9 (16.4) | 10 (18.5)) | 0.002 | 0.996 | |
| Bachelor’s degree or higher | 46 (83.6) | 44 (81.5) | ||||
| COVID-19-related characteristics | ||||||
| PPE training | Yes | 42 (76.4) | 42 (77.8) | 0.175 | 0.861 | |
| No | 13 (23.6) | 12 (22.2) | ||||
| COVID-19 education | Yes | 41 (74.5) | 32 (59.3) | 2.878 | 0.106 | |
| No | 14 (25.5) | 22 (40.7) | ||||
| COVID-19 care experience | Yes | 44 (80) | 42 (77.8) | 0.081 | 0.776 | |
| No | 11 (11) | 12 (22.2) | ||||
| COVID-19 infection history | Yes | 30 (54.5) | 25 (46.3) | 0.742 | 0.446 | |
| No | 25 (45.5) | 29 (53.7) | ||||
| Cohabiting family COVID-19 infection history | Yes | 28 (50.9) | 30 (55.6) | 0.236 | 0.702 | |
| No | 27 (49.1) | 24 (44.4) | ||||
| Prior simulation other than COVID-19 simulation | Yes | 22 (40) | 28 (51.9) | 1.541 | 0.251 | |
| No | 33 (60) | 26 (48.1) | ||||
| Baseline homogeneity in dependent variables | ||||||
| Knowledge | 19.98 ± 2.50 | 20.65 ± 2.59 | −1.471 † | 0.141 | ||
| Practice confidence | 110.16 ± 19.63 | 117.06 ± 20.01 | −1.850 | 0.067 | ||
| Clinical decision-making anxiety | 50.40 ± 20.18 | 49.27 ± 19.58 | 0.392 | 0.696 | ||
| Clinical decision-making confidence | 74.89 ± 25.27 | 79.01 ± 27.20 | 0.957 † | 0.339 | ||
| Variable | Experimental Group (n = 55) | Control Group (n = 54) | t/Z | p | ||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Difference | Pre | Post | Difference | |||
| M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | |||
| Knowledge | 19.98 ± 2.50 | 22.88 ± 2.31 | 3.31 ± 3.20 | 20.65 ± 2.59 | 21.63 ± 2.39 | 1.33 ± 3.39 | 3.13 | 0.002 |
| Practice | 110.16 ± 19.63 | 130.91 ± 18.88 | 20.75 ± 18.36 | 117.05 ± 20.01 | 120.56 ± 21.64 | 3.5 ± 22.80 | −4.175 * | <0.001 |
| Clinical | 50.40 ± 20.18 | 47.89 ± 23.56 | −2.50 ± 25.45 | 49.27 ± 19.58 | 47.78 ± 22.13 | −1.49 ± 25.79 | −0.268 * | 0.789 |
| decision-making anxiety | ||||||||
| Clinical | 74.89 ± 25.27 | 95.20 ± 24.89 | 20.31 ± 23.66 | 79.19 ± 27.43 | 90.46 ± 26.51 | 11.28 ± 34.41 | −1.347 * | 0.178 |
| decision-making confidence | ||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-H.; Choi, J.-S. Development and Implementation of a Mobile-Integrated Simulation for COVID-19 Nursing Practice: A Randomized Controlled Pretest–Posttest Experimental Design. Healthcare 2024, 12, 419. https://doi.org/10.3390/healthcare12040419
Lee S-H, Choi J-S. Development and Implementation of a Mobile-Integrated Simulation for COVID-19 Nursing Practice: A Randomized Controlled Pretest–Posttest Experimental Design. Healthcare. 2024; 12(4):419. https://doi.org/10.3390/healthcare12040419
Chicago/Turabian StyleLee, Sun-Hwa, and Jeong-Sil Choi. 2024. "Development and Implementation of a Mobile-Integrated Simulation for COVID-19 Nursing Practice: A Randomized Controlled Pretest–Posttest Experimental Design" Healthcare 12, no. 4: 419. https://doi.org/10.3390/healthcare12040419
APA StyleLee, S.-H., & Choi, J.-S. (2024). Development and Implementation of a Mobile-Integrated Simulation for COVID-19 Nursing Practice: A Randomized Controlled Pretest–Posttest Experimental Design. Healthcare, 12(4), 419. https://doi.org/10.3390/healthcare12040419






