Comparison of UESCOPE VL 400, I-View, Non-Channeled Airtraq Videolaryngoscopes and Macintosh Laryngoscope for Tracheal Intubation in Simulated Out-of-Hospital Conditions: A Randomized Crossover Manikin Study
Abstract
:1. Introduction
2. Methods
2.1. Pre-Study Preparation
2.2. Simulation Model
2.3. Outcomes
2.4. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Primary Endpoints
3.3. Secondary Endpoints
4. Discussion
5. Conclusions
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pirotte, A.; Panchananam, V.; Finley, M.; Petz, A.; Herrmann, T. Current Considerations in Emergency Airway Management. Curr. Emerg. Hosp. Med. Rep. 2022, 10, 73–86. [Google Scholar] [CrossRef]
- Joffe, A.M.; Aziz, M.F.; Posner, K.L.; Duggan, L.V.; Mincer, S.L.; Domino, K.B. Management of Difficult Tracheal Intubation: A Closed Claims Analysis. Anesthesiology 2019, 131, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Gaszyński, T.; Jakubiak, J. Muscle activity during endotracheal intubation using 4 laryngoscopes (Macintosh laryngoscope, Intubrite, TruView Evo2 and King Vision)—A comparative study. Med. Pr. 2016, 67, 155–162. [Google Scholar] [CrossRef]
- Amalric, M.; Larcher, R.; Brunot, V.; Garnier, F.; De Jong, A.; Moulaire Rigollet, V.; Corne, P.; Klouche, K.; Jung, B. Impact of Videolaryngoscopy Expertise on First-Attempt Intubation Success in Critically Ill Patients. Crit. Care Med. 2020, 48, e889–e896. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M.; Woodall, N.; Harper, J.; Benger, J. Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2, intensive care and emergency departments. Br. J. Anaesth. 2011, 106, 632–642. [Google Scholar] [CrossRef]
- Morton, S.; Dawson, J.; Wareham, G.; Broomhead, R.; Sherren, P. The Prehospital Emergency Anaesthetic in 2022. Air Med. J. 2022, 41, 530–535. [Google Scholar] [CrossRef]
- Pourmand, A.; Terrebonne, E.; Gerber, S.; Shipley, J.; Tran, Q.K. Efficacy of Video Laryngoscopy versus Direct Laryngoscopy in the Prehospital Setting: A Systematic Review and Meta-Analysis. Prehosp. Disaster Med. 2022, 38, 111–121. [Google Scholar] [CrossRef]
- Xue, F.S.; Yang, B.Q.; Liu, Y.Y.; Li, H.X.; Yang, G.Z. Current Evidences for the Use of UEscope in Airway Management. Chin. Med. J. 2017, 130, 1867–1875. [Google Scholar] [CrossRef] [PubMed]
- Sampankanpanich Soria, C.; Lee, D.E.; Manecke, G.R. (Eds.) Intubating on the Ground. In Anesthesiology Resident Manual of Procedures: A Step-by-Step Guide; Springer International Publishing: Cham, Switzerland, 2021; pp. 83–84. [Google Scholar]
- Toshiyuki Nakanishi, T.; Sento, Y.; Kamimura, Y.; Sobue, K. Macintosh laryngoscope and i-view™ and C-MAC® video laryngoscopes for tracheal intubation with an aerosol box: A randomized crossover manikin study. JA Clin. Rep. 2021, 7, 52. [Google Scholar] [CrossRef]
- Wakabayashi, R.; Ishida, T.; Yamada, T.; Kawamata, M. Effect of an aerosol box on tracheal intubation difficulty. J. Anesth. 2020, 34, 790–793. [Google Scholar] [CrossRef]
- Taylor, D.H.; Wagner, E.M.; Hu, J.S.; Tobin, M.R.; Cronin, A.J.; Couperus, K.S.; April, M.D.; Schauer, S.G.; Jason FNaylor, J.F. New Versus Old, The i-View Video Laryngoscope Versus the GlideScope: A Prospective, Randomized, Crossover Trial. Med. J. (Ft Sam Houst Tex) 2021, PB 8-21-07/08/09, 81–89. [Google Scholar]
- Moritz, A.; Leonhardt, V.; Prottengeier, J.; Birkholz, T.; Schmidt, J.; Irouschek, A. Comparison of Glidescope® Go™, King Vision™, Dahlhausen VL, I-View™ and Macintosh laryngoscope use during difficult airway management simulation by experienced and inexperienced emergency medical staff: A randomized crossover manikin study. PLoS ONE 2020, 15, e0236474. [Google Scholar] [CrossRef]
- Gaszyński, T. A randomized controlled study on the visual grading of the glottis and the hemodynamics response to laryngoscopy when using I-View and MacGrath Mac videolaryngoscopes in super obese patients. J. Clin. Monit. Comput. 2021, 35, 279–283. [Google Scholar] [CrossRef]
- Wang, Y.L.; Qiu, Y.Q.; Huang, M.; Chen, Y.; He, J.L.; Chen, A. Application of HC videolaryngoscope in endotracheal intubation under general anesthesia. China Med. Pharm. 2015, 5, 84–87. (In Chinese) [Google Scholar]
- Higashizawa, T.; Bioto, H.; Nishiyama, T.; Sakai, T.; Konishi, A. Assessment of practice of endotracheal intubation bu levering Laryngoscope in teaching of undergraduate medical students. Masui 1997, 46, 1255–1258. [Google Scholar] [PubMed]
- Gaszyński, T. A comparison of Standard Macintosh Blade Laryngoscope, Pentax-AWS Videolaryngoscope and Intubrite Videolaryngoscope for Tracheal Intubation in Manikins in Sitting and Prone Positions: A Randomized Cross-Over Study. Diagnostics 2020, 10, 603. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y. The clinical application of HC videolaryngoscope in tracheal intubation with general anesthesia. Guide China Med. 2015, 13, 65–66. (In Chinese) [Google Scholar]
- Sun, Z.; Gong, S.K.; Han, X.P.; Li, P.H. Clinical observation of HC videolaryngoscope and Macintosh laryngoscope for orotracheal intubation. J. Pract. Med. 2013, 29, 1161–1163. [Google Scholar]
- Wang, W.L.; Wang, L.; Wang, Z.H.; Li, X.F.; Wang, S.L. Comparative performance of HC videolaryngoscope and direct laryngoscope for tracheal intubation. Shandong Med. J. 2015, 55, 39–40. (In Chinese) [Google Scholar] [CrossRef]
- Wang, H.; Zhang, M.F. The observation of tracheal intubation with UE videolaryngoscope in obese patients. Zhejiang Med. J. 2013, 35, 1282–1283. (In Chinese) [Google Scholar]
- Li, Z.; Meng, J.S.; Hu, Y. Application of HC videolaryngoscope for endotracheal intubation in patients with difficult airways by burn scar. Pract. J. Med. Pharm. 2013, 30, 397–398. [Google Scholar] [CrossRef]
- Pan, L.; Yu, L.; Pei, H.; Fan, Y.; Wang, X.; Su, L.; Huang, W. The usage of HC videolaryngoscope for emergency tracheal intubation by unskilled junior emergency resident doctors. Chin. J. Emerg. Med. 2016, 25, 910–914. (In Chinese) [Google Scholar] [CrossRef]
- Saracoglu, K.T.; Eti, Z.; Gogus, F.Y. Airtraq optical laryngoscope: Advantages and disadvantages. Middle East J. Anaesthesiol. 2013, 22, 135–141. [Google Scholar]
- Giquello, J.A.; Humbert, S.; Duc, F.; Monrigal, J.P.; Granry, J.C. Use of the Airtraq by inexperienced physicians supervised during a series of tracheal intubation in adult patient with anticipated difficult airway. Ann. Fr. Anesth. Reanim. 2011, 30, 804–808. [Google Scholar] [CrossRef]
- Kleine-Brueggeney, M.; Greif, R.; Schoettker, G.L.; SNabecker, S.; Theiler, L.G. Evaluation of six videolaryngoscopes in 720 patients with a simulated difficult airway: A multicentre randomized controlled trial. Br. J. Anaesth. 2016, 116, 670–679. [Google Scholar] [CrossRef]
- Lu, Y.; Jiang, H.; Zhu, Y.S. Airtraq laryngoscope versus conventional Macintosh laryngoscope: A systematic review and meta-analysis. Anaesthesia 2011, 66, 1160–1167. [Google Scholar] [CrossRef]
- Nowicki, T.A.; Suozzi, J.S.; Dziedzic, M.; Kamin, R.; Donahue, S.; Robinson, K. Comparison of use of the the Airtraq with direct laryngoscopy by paramedics in the simulated airway. Prehosp. Emerg. Care 2009, 13, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Trimmel, H.; Kreutziger, J.; Fertsak, G.; Fitzka, R.; Dittrich, M.; Voelckel, W.G. Use of the Airtraq laryngoscope for emergency intubation in the prehospital setting: A randomized control trial. Crit. Care Med. 2011, 39, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Wetsch, W.A.; Spelten, O.; Hellmich, M.; Carlitscheck, M.; Padosch, S.A.; Lier, H.; Böttiger, B.W.; Hinkelbein, J. Comparison of different video laryngoscopes for emergency intubation in a standardized airway manikin with immobilized cervical spine by experienced anaesthetists. A randomized, controlled crossover trial. Resuscitation 2012, 83, 740–745. [Google Scholar] [CrossRef] [PubMed]
- Maharaj, C.H.; McDonnell, J.G.; Harte, B.H.; Laffey, J.G. A comparison of direct and indirect laryngoscopes and the ILMA in novoces users: A manikin study. Anaesthesia 2007, 62, 1161–1166. [Google Scholar] [CrossRef] [PubMed]
- Nandakumar, K.P.; Bhalla, A.P.; Pandey, R.K.; Baidya, D.K.; Subramaniam, R.; Kashyap, L. Comparison of Macintosh, McCoy, and Glidescope video laryngoscope for intubation in morbidly obese patients: Randomized controlled trial. Saudi J. Anaesth. 2018, 12, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Akbarzadeh, S.R.; Gillani, M.T.; Tabari, M.; Morovatdar, N. Comparison analysis of the Usefulness of the GlideScope®, Macintosh, and McCoy Laryngoscopes for Endotracheal Intubation in Patients with Obesity: A Randomized, Clinical Trial. Anesth. Pain Med. 2017, 7, e57913. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M.; Tuckey, J.P. A comparison between the Macintosh and the McCoy laryngoscope blades. Anaesthesia 1996, 51, 977–980. [Google Scholar] [CrossRef] [PubMed]
- Hansel, J.; Rogers, A.M.; Lewis, S.R.; Cook, T.M.; Smith, A.F. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst. Rev. 2022, 4, CD011136. [Google Scholar] [CrossRef] [PubMed]
- Pieters, B.M.; Wilbers, N.E.; Huijzer, M.; Winkens, B.; van Zundert, A.A. Comparison of seven videolaryngoscopes with the Macintosh laryngoscope in manikins by experienced and novice personnel. Anaesthesia 2016, 71, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Pieters, B.M.A.; Maas, E.H.A.; Knape, J.T.A.; van Zundert, A.A.J. Videolaryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: A systematic review and meta-analysis. Anaesthesia 2017, 72, 1532–1541. [Google Scholar] [CrossRef] [PubMed]
- Maassen, R.; van Zundert, A. Comparison of the C-MAC® vidolaryngoscope with the Macintosh, Glidescope® and Airtraq® laryngoscopes in easy and difficult laryngoscopy senarios in manikins. Anaesthesia 2010, 65, 955–956. [Google Scholar] [CrossRef]
- Van Zundert, A.; Maassen, R.; Lee, R.; Willems, R.; Timmerman, M.; Siemonsma, M.; Buise, M.; Wiepking, M. A Macintosh laryngoscope blade for videolaryngoscopy reduces stylet use in patients with normal airways. Anesth. Analg. 2009, 109, 825–831. [Google Scholar] [CrossRef]
- Maassen, R.; Lee, R.; Hermans, B.; Marcus, M.; van Zundert, A. A comparison of three videolaryngoscopes: The Macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesth. Analg. 2009, 109, 1560–1565. [Google Scholar] [CrossRef]
- Vidhya, S.; Prakash, N.; Swain, A.; Kumar, S.; Shukla, R. An Inquiry on Airway Management by McCoy Blade with Elevated Tip and Miller Straight Blade with Paraglossal Technique: Relevance for difficult airway Management in Current Infectious Times. Anesth Essays Res. 2021, 15, 401–407. [Google Scholar] [CrossRef]

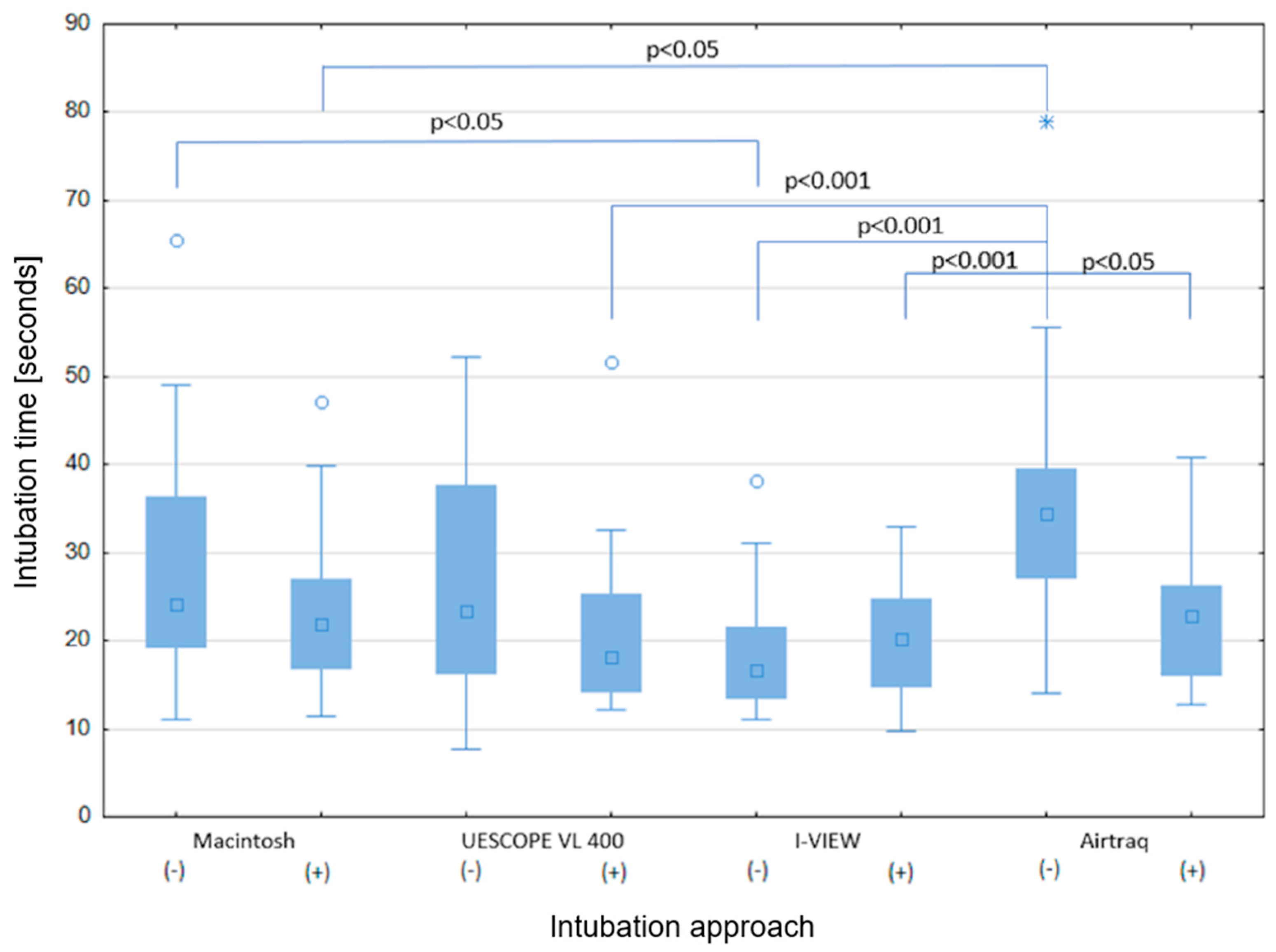

| UESCOPE VL 400 (n = 30) | I-View (n = 30) | Airtraq (n = 30) | Macintosh (n = 30) | p-Value | |
|---|---|---|---|---|---|
| Primary Outcome | |||||
| Time to TI; s | |||||
| without stylet | 23.31 (IQR: 17–31) | 16.6 (IQR:13–22) | 34.5 (IQR: 28–39) | 24.1 (IQR:19–37) | <0.05 |
| with stylet | 18.18 (IQR: 14–25) | 20.3 (IQR:15–24) | 22.7 (IQR: 17–27) | 18.5 (IQR:17–28) | >0.05 |
| Secondary Outcomes | |||||
| Cormack-Lehane grading | |||||
| without and with stylet | |||||
| 1 | 31 (51.7%) | 31 (51.7%) | 27 (45%) | 26 (43%) | >0.05 |
| 2 | 26 (43.7% | 27 (45%) | 28 (46.7%) | 24 (40%) | >0.05 |
| 3 | 3 (5%) | 2 (3.3%) | 5 (8.3) | 9 (15%) | <0.05 |
| 4 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1.7%) | >0.05 |
| Successful TI rate | |||||
| without stylet | 29 (96.7%) | 30 (100%) | 26 (86.7%) | 30 (100%) | >0.05 |
| with stylet | 30 (100%) | 30 (100%) | 30 (100%) | 30 (100%) | >0.05 |
| Dental clicks | |||||
| without stylet | 4 (13.3%) | 4 (13.3%) | 8 (26.7%) | 9 (30%) | <0.05 |
| with stylet | 1 (3.3%) | 4 (13.3%) | 2 (6.7%) | 6 (20%) | <0.05 |
| Effort | |||||
| without stylet | 2 (IQR: 1–3) | 2 (IQR: 1–3) | 3 (IQR: 3–4) | 3 (IQR: 2–4) | >0.05 |
| with stylet | 2.5 (IQR: 1–3) | 2 (IQR: 1–2) | 3 (IQR: 2–4) | 2.5(IQR:1–3) | >0.05 |
| Comfort | |||||
| without stylet | 2 (IQR: 2–3) | 3 (IQR: 2–3) | 2 (IQR:1.25–3) | 2.5(IQR:2–3) | >0.05 |
| with stylet | 3 (IQR: 2–3) | 3 (IQR: 2–3) | 2 (IQR:2–3) | 3 (IQR: 2–3) | >0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ratajczyk, P.; Dolder, P.; Szmyd, B.; Gomez-Rios, M.A.; Hogendorf, P.; Durczyński, A.; Gaszyński, T. Comparison of UESCOPE VL 400, I-View, Non-Channeled Airtraq Videolaryngoscopes and Macintosh Laryngoscope for Tracheal Intubation in Simulated Out-of-Hospital Conditions: A Randomized Crossover Manikin Study. Healthcare 2024, 12, 452. https://doi.org/10.3390/healthcare12040452
Ratajczyk P, Dolder P, Szmyd B, Gomez-Rios MA, Hogendorf P, Durczyński A, Gaszyński T. Comparison of UESCOPE VL 400, I-View, Non-Channeled Airtraq Videolaryngoscopes and Macintosh Laryngoscope for Tracheal Intubation in Simulated Out-of-Hospital Conditions: A Randomized Crossover Manikin Study. Healthcare. 2024; 12(4):452. https://doi.org/10.3390/healthcare12040452
Chicago/Turabian StyleRatajczyk, Paweł, Przemyslaw Dolder, Bartosz Szmyd, Manuel A. Gomez-Rios, Piotr Hogendorf, Adam Durczyński, and Tomasz Gaszyński. 2024. "Comparison of UESCOPE VL 400, I-View, Non-Channeled Airtraq Videolaryngoscopes and Macintosh Laryngoscope for Tracheal Intubation in Simulated Out-of-Hospital Conditions: A Randomized Crossover Manikin Study" Healthcare 12, no. 4: 452. https://doi.org/10.3390/healthcare12040452
APA StyleRatajczyk, P., Dolder, P., Szmyd, B., Gomez-Rios, M. A., Hogendorf, P., Durczyński, A., & Gaszyński, T. (2024). Comparison of UESCOPE VL 400, I-View, Non-Channeled Airtraq Videolaryngoscopes and Macintosh Laryngoscope for Tracheal Intubation in Simulated Out-of-Hospital Conditions: A Randomized Crossover Manikin Study. Healthcare, 12(4), 452. https://doi.org/10.3390/healthcare12040452









