Development and Effect Evaluation of an Action-Oriented Interdisciplinary Weaning Protocol for Cuffed Tracheostomy Tubes in Patients with Acquired Brain Injury
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Development of the Action Oriented IWP
2.3. Search Strategy
2.4. Patient Population for Effect Evaluation of the IWP
3. Results
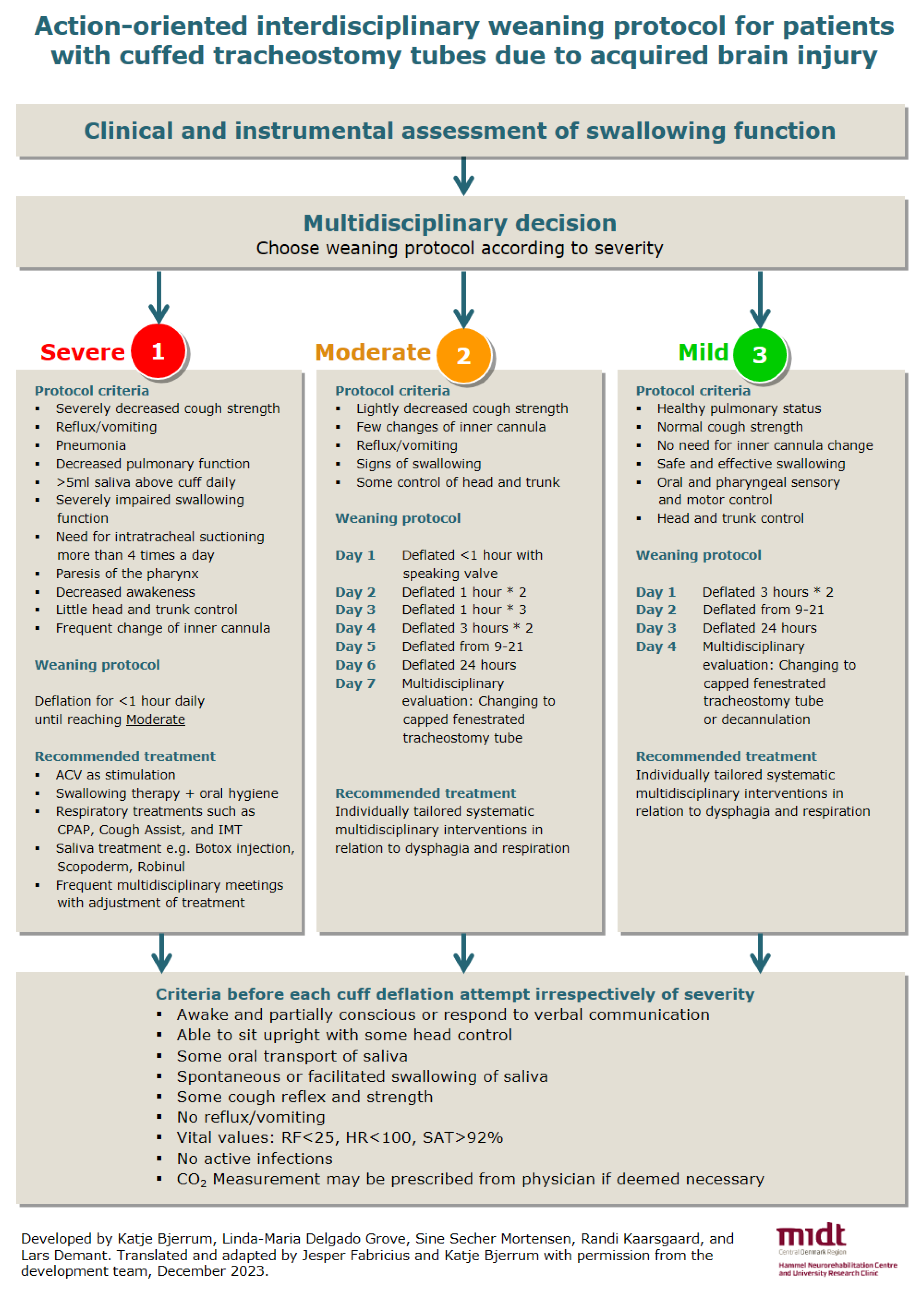
3.1. Action-Oriented IWP
- Each of the three protocols provide the interdisciplinary team with guidance on the weaning process, which must be adapted to the individual patient [8,12]. The IWP present both suggestions for cuff-deflation intervals and for treatment and therapy [10,27]. Treatment and therapy [5,28] encompass, e.g., interventions related to meal situations and oral hygiene [29,30,31], tactile stimulation [15,30,31,32], mobilization of the tongue [30,32], facilitation of swallowing [30,31], ACV [7,27], neuromuscular electrical stimulation, chin-tuck, effortful swallow, supraglottic swallow, the Mendelsohn maneuver [33], and pharmacological agents to reduce the production of saliva [5].
| Protocol Criteria | Description | Comment | References |
|---|---|---|---|
| Conscious/verbal address | Some consciousness and/or response to verbal address. | There is no consensus on whether consciousness has an impact in relation to a successful weaning from the tracheostomy tube. | [5,10,14,15] |
| Postural control | Able to sit upright with some degree of head control. | This is also a prerequisite for oral intake of food and liquids. | [10,15] |
| Saliva management | Some oral transport of saliva. | The literature indicates that some oral transport of saliva increases the chance of a successful decannulation. | [5,10,15] |
| Swallowing of saliva | Spontaneous or facilitated swallowing of saliva. | It has been suggested that spontaneous or facilitated swallowing of saliva has an impact on weaning from tracheostomy tubes. | [5,10,14,15] |
| Cough reflex and strength | Spontaneous and effective cough reflex and strength. | It is suggested that cough reflex and strength are important criteria to assess, but without having consensus on how to measure it. | [5,10,14,25,34] |
| Reflux/vomiting | No or little problems with reflux and vomiting. | Patients that cannot protect their lower airways are at higher risk of pneumonia if they have issues with reflux and vomiting. | [5,34] |
| Saliva above the cuff | Saliva above the cuff measured several times a day. | Cuffed tracheostomy tubes with a suction aid is preferred. However, there is no consensus on cutoff value on the amount of saliva above the cuff. | [35] |
| Respiratory frequency | <25 | No obstruction of the upper respiratory tract. | [5,14,34] |
| Heart rate | <100 | A normal resting heart rate for adults ranges 60–100 beats per minute. | [36] |
| Saturation | >92% | Breathing room air or with supplemented oxygen. | [5,10,34] |
| Infections | No active infection. | Recommended before proceeding with weaning and decannulation. | [5,37,38,39] |
| CO2 Measurement | PaCO2 < 60 mmHg | If deemed necessary. | [14] |
3.2. Effect Evaluation of the IWP
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bosel, J. Tracheostomy in stroke patients. Curr. Treat. Options Neurol. 2014, 16, 274. [Google Scholar] [CrossRef] [PubMed]
- Elman, L.B.; Dubin, R.M.; Kelley, M.; McCluskey, L. Management of oropharyngeal and tracheobronchial secretions in patients with neurologic disease. J. Palliat. Med. 2005, 8, 1150–1159. [Google Scholar] [CrossRef] [PubMed]
- Zielske, J.; Bohne, S.; Brunkhoste, F.M.; Axer, H.; Guntinas-Lichius, O. Acute and long-term dysphagia in critically ill patients with severe sepsis: Results of a prospective controlled observational study. Eur. Arch. Oto-Rhino-Laryngol. 2014, 271, 3085–3093. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, H.H.; Kirby, K.J.; Terrin, N.; Hill, N.S.; White, A.C. Decannulation following tracheostomy for prolonged mechanical ventilation. J. Intensive Care Med. 2009, 24, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Garuti, G.; Reverberi, C.; Briganti, A.; Massobrio, M.; Lombardi, F.; Lusuardi, M. Swallowing disorders in tracheostomised patients: A multidisciplinary/multiprofessional approach in decannulation protocols. Multidiscip. Respir. Med. 2014, 9, 36. [Google Scholar] [CrossRef] [PubMed]
- Checklin, M.; Etty-Leal, M.; Iseli, T.A.; Potter, N.; Fisher, S.; Chapman, L. Saliva management options for difficult-to-wean people with tracheostomy following severe acquired brain injury (ABI): A review of the literature. Brain Inj. 2015, 29, 1–10. [Google Scholar] [CrossRef]
- McGrath, B.; Lynch, J.; Wilson, M.; Nicholson, L.; Wallace, S. Above cuff vocalisation: A novel technique for communication in the ventilator-dependent tracheostomy patient. J. Intensive Care Soc. 2016, 17, 19–26. [Google Scholar] [CrossRef]
- Heffner, J.E. The technique of weaning from tracheostomy. Criteria for weaning; practical measures to prevent failure. J. Crit. Illn. 1995, 10, 729–733. [Google Scholar]
- Roth, E.J.; Lovell, L.; Harvey, R.L.; Bode, R.K.; Heinemann, A.W. Stroke rehabilitation: Indwelling urinary catheters, enteral feeding tubes, and tracheostomies are associated with resource use and functional outcomes. Stroke 2002, 33, 1845–1850. [Google Scholar] [CrossRef][Green Version]
- Frank, U.; Mader, M.; Sticher, H. Dysphagic patients with tracheotomies: A multidisciplinary approach to treatment and decannulation management. Dysphagia 2007, 22, 20–29. [Google Scholar] [CrossRef]
- Warnecke, T.; Suntrup, S.; Teismann, I.K.; Hamacher, C.; Oelenberg, S.; Dziewas, R. Standardized endoscopic swallowing evaluation for tracheostomy decannulation in critically ill neurologic patients. Crit. Care Med. 2013, 41, 1728–1732. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Saran, S.; Baronia, A.K. The practice of tracheostomy decannulation-a systematic review. J. Intensive Care 2017, 5, 38. [Google Scholar] [CrossRef] [PubMed]
- Sticher, H.; Gratz, C. Trachealkanülen-Management in der F.O.T.T.: Der Weg zurück zur Physiologie. In Die Therapie des Facio-Oralen Trakts; Nusser-Müller-Busch, R., Ed.; Springer: Berlin/Heidelberg, Germany, 2004. [Google Scholar]
- Santus, P.; Gramegna, A.; Radovanovic, D.; Raccanelli, R.; Valenti, V.; Rabbiosi, D.; Vitacca, M.; Nava, S. A systematic review on tracheostomy decannulation: A proposal of a quantitative semiquantitative clinical score. BMC Pulm. Med. 2014, 14, 201. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, J.; Jensen, D.; Kjaersgaard, A. A validation study of the Facial-Oral Tract Therapy Swallowing Assessment of Saliva. Clin. Rehabil. 2016, 30, 410–415. [Google Scholar] [CrossRef]
- Robbins, J.; Coyle, J.; Rosenbek, J.; Roecker, E.; Wood, J. Differentiation of Normal and Abnormal Airway Protection during Swallowing Using the Penetration–Aspiration Scale. Dysphagia 1999, 14, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Rosenbek, J.C.; Robbins, J.A.; Roecker, E.B.; Coyle, J.L.; Wood, J.L. A penetration-aspiration scale. Dysphagia 1996, 11, 93–98. [Google Scholar] [CrossRef]
- Neubauer, P.D.; Rademaker, A.W.; Leder, S.B. The Yale Pharyngeal Residue Severity Rating Scale: An Anatomically Defined and Image-Based Tool. Dysphagia 2015, 30, 521–528. [Google Scholar] [CrossRef]
- Warnecke, T.; Ritter, M.A.; Kroger, B.; Oelenberg, S.; Teismann, I.; Heuschmann, P.U.; Ringelstein, E.B.; Nabavi, D.G.; Dziewas, R. Fiberoptic endoscopic Dysphagia severity scale predicts outcome after acute stroke. Cerebrovasc. Dis. 2009, 28, 283–289. [Google Scholar] [CrossRef]
- Pedersen, A.R.; Stubbs, P.W.; Nielsen, J.F. Reducing redundant testing using the Functional Independence Measure and Early Functional Abilities scale during rehabilitation in patients with brain injury. Brain Inj. 2018, 32, 1090–1095. [Google Scholar] [CrossRef]
- Hankemeier, A.; Rollnik, J.D. The Early Functional Abilities (EFA) scale to assess neurological and neurosurgical early rehabilitation patients. BMC Neurol. 2015, 15, 207. [Google Scholar] [CrossRef]
- Poulsen, I.; Kreiner, S.; Engberg, A. Validation of the Early Functional Abilities scale: An assessment of four dimensions in early recovery after traumatic brain injury. J. Rehabil. Med. 2018, 50, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Boltzmann, M.; Schmidt, S.B.; Gutenbrunner, C.; Krauss, J.K.; Höglinger, G.U.; Weimar, C.; Rollnik, J.D. Validity of the Early Functional Ability scale (EFA) among critically ill patients undergoing early neurological rehabilitation. BMC Neurol. 2022, 22, 333. [Google Scholar] [CrossRef] [PubMed]
- Enrichi, C.; Battel, I.; Zanetti, C.; Koch, I.; Ventura, L.; Palmer, K.; Meneghello, F.; Piccione, F.; Rossi, S.; Lazzeri, M.; et al. Clinical Criteria for Tracheostomy Decannulation in Subjects with Acquired Brain Injury. Respir. Care 2017, 62, 1255–1263. [Google Scholar] [CrossRef] [PubMed]
- Perin, C.; Meroni, R.; Rega, V.; Braghetto, G.; Cerri, C.G. Parameters Influencing Tracheostomy Decannulation in Patients Undergoing Rehabilitation after severe Acquired Brain Injury (sABI). Int. Arch. Otorhinolaryngol. 2017, 21, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Hiss, S.G.; Postma, G.N. Fiberoptic Endoscopic Evaluation of Swallowing. Laryngoscope 2003, 113, 1386–1393. [Google Scholar] [CrossRef] [PubMed]
- Kothari, M.; Bjerrum, K.; Nielsen, L.H.; Jensen, J.; Nielsen, J.F. Influence of external subglottic air flow on dysphagic tracheotomized patients with severe brain injury: Preliminary findings. Ann. Otol. Rhinol. Laryngol. 2017, 126, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, H.; Pallesen, H. Personcentreret Neurorehabilitering—Viden og Praksis, 1st ed.; Gads forlag: Copenhagen, Denmark, 2022; Volume 272. [Google Scholar]
- Kothari, M.; Pillai, R.S.; Kothari, S.F.; Spin-Neto, R.; Kumar, A.; Nielsen, J.F. Oral health status in patients with acquired brain injury: A systematic review. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2017, 123, 205–219.e7. [Google Scholar] [CrossRef]
- Nusser-Müller-Busch, R.; Gampp Lehmann, K. Facial-Oral Tract Therapy (F.O.T.T.) for Eating, Swallowing, Nonverbal Communication and Speech, 1st ed.; Springer: Berlin/Heidelberg, Germany, 2021; Volume XIV, p. 324. [Google Scholar]
- Kjærsgaard, A. Ansigt, Mund og Svælg: Undersøgelse og Behandling af Dysfagi og Tilgrænsende Problemer, 2nd ed.; Munksgaard: Copenhagen, Denmark, 2020; p. 224. [Google Scholar]
- Hansen, T.S.; Jakobsen, D. A decision-algorithm defining the rehabilitation approach: ‘Facial oral tract therapy’. Disabil. Rehabil. 2010, 32, 1447–1460. [Google Scholar] [CrossRef]
- Warnecke, T.D.; Langmore, R. Neurogenic Dysphagia, 1st ed.; Springer: Cham, Switzerland, 2021; p. 399. [Google Scholar]
- Braine, M.E.; Sweby, C. A systematic approach to weaning and decannulation of tracheostomy tubes. Br. J. Neurosci. Nurs. 2006, 2, 124–132. [Google Scholar] [CrossRef]
- Greene, R.; Thompson, S.; Jantsch, H.S.; Teplick, R.; Cullen, D.J.; Greene, E.M.; Whitman, G.J.; Hulka, C.A.; Llewellyn, H.J. Detection of pooled secretions above endotracheal-tube cuffs: Value of plain radiographs in sheep cadavers and patients. AJR Am. J. Roentgenol. 1994, 163, 1333–1337. [Google Scholar] [CrossRef]
- All about Heart Rate (Pulse). Available online: https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/all-about-heart-rate-pulse (accessed on 1 February 2024).
- Schow, T.; Larsen, K.; Engberg, A.W. The Association of Functional Oral Intake and Pneumonia in Patients With Severe Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2008, 89, 2114–2120. [Google Scholar]
- Coelho, L.; Póvoa, P.; Almeida, E.; Fernandes, A.; Mealha, R.; Moreira, P.; Sabino, H. Usefulness of C-reactive protein in monitoring the severe community-acquired pneumonia clinical course. Crit. Care 2007, 11, R92. [Google Scholar] [CrossRef] [PubMed]
- Kutz, A.; Grolimund, E.; Christ-Crain, M.; Thomann, R.; Falconnier, C.; Hoess, C.; Henzen, C.; Zimmerli, W.; Mueller, B.; Schuetz, P.; et al. Pre-analytic factors and initial biomarker levels in community-acquired pneumonia patients. BMC Anesthesiol. 2014, 14, 102. [Google Scholar] [CrossRef]
- E-dok. Available online: https://e-dok.rm.dk/edok/admin/GUI.nsf/Desktop.html?Open&login (accessed on 1 February 2024).
- Mortensen, J.; Kjeldsen, S.S.; Honoré, H.; Pedersen, A.R. Using Routinely Gathered Clinical Data to Develop a Prognostic Online Tool for Decannulation in Subjects With Acquired Brain Injury. Respir. Care 2020, 65, 1678–1686. [Google Scholar] [CrossRef] [PubMed]
- Okamura, K. Glasgow Coma Scale flow chart: A beginner’s guide. Br. J. Nurs. 2014, 23, 1068–1073. [Google Scholar] [CrossRef] [PubMed]
- de Lima Zanata, I.; Santos, R.S.; Hirata, G.C. Tracheal decannulation protocol in patients affected by traumatic brain injury. Int. Arch. Otorhinolaryngol. 2014, 18, 108–114. [Google Scholar]
- Steidl, C.; Boesel, J.; Suntrup-Krueger, S.; Schoenenberger, S.; Al-Suwaidan, F.; Warnecke, T.; Minnerup, J.; Dziewas, R. Tracheostomy, Extubation, Reintubation: Airway Management Decisions in Intubated Stroke Patients. Cerebrovasc. Dis. 2017, 44, 1–9. [Google Scholar] [CrossRef]
- Kjaersgaard, A.; Nielsen, L.H.; Sjölund, B.H. Randomized trial of two swallowing assessment approaches in patients with acquired brain injury: Facial-Oral Tract Therapy versus Fibreoptic Endoscopic Evaluation of Swallowing. Clin. Rehabil. 2014, 28, 243–253. [Google Scholar] [CrossRef]
- Medeiros, G.C.D.; Sassi, F.C.; Lirani-Silva, C.; Andrade, C.R.F.D. Criteria for tracheostomy decannulation: Literature review. CoDAS 2019, 31, e20180228. [Google Scholar] [CrossRef]
- Enrichi, C.; Zanetti, C.; Gregorio, C.; Koch, I.; Vio, A.; Palmer, K.; Meneghello, F.; Piccione, F.; Battel, I. The assessment of the peak of reflex cough in subjects with acquired brain injury and tracheostomy and healthy controls. Respir. Physiol. Neurobiol. 2020, 274, 103356. [Google Scholar] [CrossRef]
- Gallice, T.; Cugy, E.; Branchard, O.; Dehail, P.; Moucheboeuf, G. Predictive Factors for Successful Decannulation in Patients with Tracheostomies and Brain Injuries: A Systematic Review. Dysphagia 2024. Epub ahead of print. [Google Scholar] [CrossRef]
- Gallice, T.; Cugy, E.; Germain, C.; Barthélemy, C.; Laimay, J.; Gaube, J.; Engelhardt, M.; Branchard, O.; Maloizel, E.; Frison, E.; et al. A Pluridisciplinary Tracheostomy Weaning Protocol for Brain-Injured Patients, Outside of the Intensive Care Unit and Without Instrumental Assessment: Results of Pilot Study. Dysphagia 2023. Epub ahead of print. [Google Scholar] [CrossRef]
- Choi, B.C.; Pak, A.W. Multidisciplinarity, interdisciplinarity and transdisciplinarity in health research, services, education and policy: 1. Definitions, objectives, and evidence of effectiveness. Clin. Investig. Med. 2006, 29, 351–364. [Google Scholar]
- Speyer, R.; Cordier, R.; Farneti, D.; Nascimento, W.; Pilz, W.; Verin, E.; Walshe, M.; Woisard, V. White Paper by the European Society for Swallowing Disorders: Screening and Non-instrumental Assessment for Dysphagia in Adults. Dysphagia 2022, 37, 333–349. [Google Scholar] [CrossRef] [PubMed]


| Before IWP, n = 161 | After IWP, n = 176 | p-Value | |
|---|---|---|---|
| Age | 56 (45–66) | 55 (44–64) | 0.338 |
| Sex | 0.133 | ||
| • Women | 29% | 36% | |
| • Men | 71% | 64% | |
| Diagnosis | 0.389 | ||
| • Ischemic stroke | 15% | 11% | |
| • Hemorrhagic stroke | 22% | 18% | |
| • SAH | 15% | 17% | |
| • Stroke NOS # | 4% | 12% | |
| • TBI | 27% | 28% | |
| • Anoxic brain injury | 10% | 4% | |
| • Brain tumor | 1% | 3% | |
| • Encephalopathy NOS | 7% | 7% | |
| Day from injury until admission | 31 (22–40) | 31 (21–41) | 0.868 |
| FIM at admission | 18 (18–21) | 18 (18–20) | 0.581 |
| EFA at admission | 42 (34–50) | 40 (32–50) | 0.324 |
| • No aspiration risk | 1% | 1% | 1.000 |
| • Stable yes/no communication | 20% | 17% | 0.571 |
| • Head control ¤ | 28% | 21% | 0.158 |
| • Postural control § | 10% | 9% | 0.851 |
| Variable | Cases/Subjects | Unadjusted HR (95%CI) | Adjusted HR (95%CI) |
|---|---|---|---|
| Weaning protocol | |||
| • Following IWP | 131/176 | 1.341 (1.038; 1.731) | 1.309 (1.013; 1.693) |
| • Before IWP | 111/161 | Ref. | Ref. |
| Sex | |||
| • Men | 158/227 | 0.733 (0.562; 0.957) | 0.753 (0.576; 0.983) |
| • Women | 84/110 | Ref. | Ref. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bjerrum, K.; Grove, L.-M.D.; Mortensen, S.S.; Fabricius, J. Development and Effect Evaluation of an Action-Oriented Interdisciplinary Weaning Protocol for Cuffed Tracheostomy Tubes in Patients with Acquired Brain Injury. Healthcare 2024, 12, 480. https://doi.org/10.3390/healthcare12040480
Bjerrum K, Grove L-MD, Mortensen SS, Fabricius J. Development and Effect Evaluation of an Action-Oriented Interdisciplinary Weaning Protocol for Cuffed Tracheostomy Tubes in Patients with Acquired Brain Injury. Healthcare. 2024; 12(4):480. https://doi.org/10.3390/healthcare12040480
Chicago/Turabian StyleBjerrum, Katje, Linda-Maria Delgado Grove, Sine Secher Mortensen, and Jesper Fabricius. 2024. "Development and Effect Evaluation of an Action-Oriented Interdisciplinary Weaning Protocol for Cuffed Tracheostomy Tubes in Patients with Acquired Brain Injury" Healthcare 12, no. 4: 480. https://doi.org/10.3390/healthcare12040480
APA StyleBjerrum, K., Grove, L.-M. D., Mortensen, S. S., & Fabricius, J. (2024). Development and Effect Evaluation of an Action-Oriented Interdisciplinary Weaning Protocol for Cuffed Tracheostomy Tubes in Patients with Acquired Brain Injury. Healthcare, 12(4), 480. https://doi.org/10.3390/healthcare12040480




