Personality Traits, Burnout, and Psychopathology in Healthcare Professionals in Intensive Care Units—A Moderated Analysis
Abstract
:1. Introduction
Aim of the Study
- How do personality dimensions differentiate as age increase?
- How do personality traits vary between male and female ICU personnel?
- What is the relationship between critical care experience, burnout, and psychopathology?
- Does the relationship between critical care experience, burnout, and psychopathology vary depending on the profession or the urban size of the ICU location?
- How do personality dimensions and profession interact in predicting burnout?
- Does the effect of critical care experience on burnout and psychopathology vary between nurses and intensivists or between ICU location in small and large cities?
2. Methods
2.1. Participants and Study Design
2.2. Measurements
2.3. Statistical Analysis
3. Results
3.1. Sample Demographics
3.2. Personality, Burnout, and Psychopathology Profiles
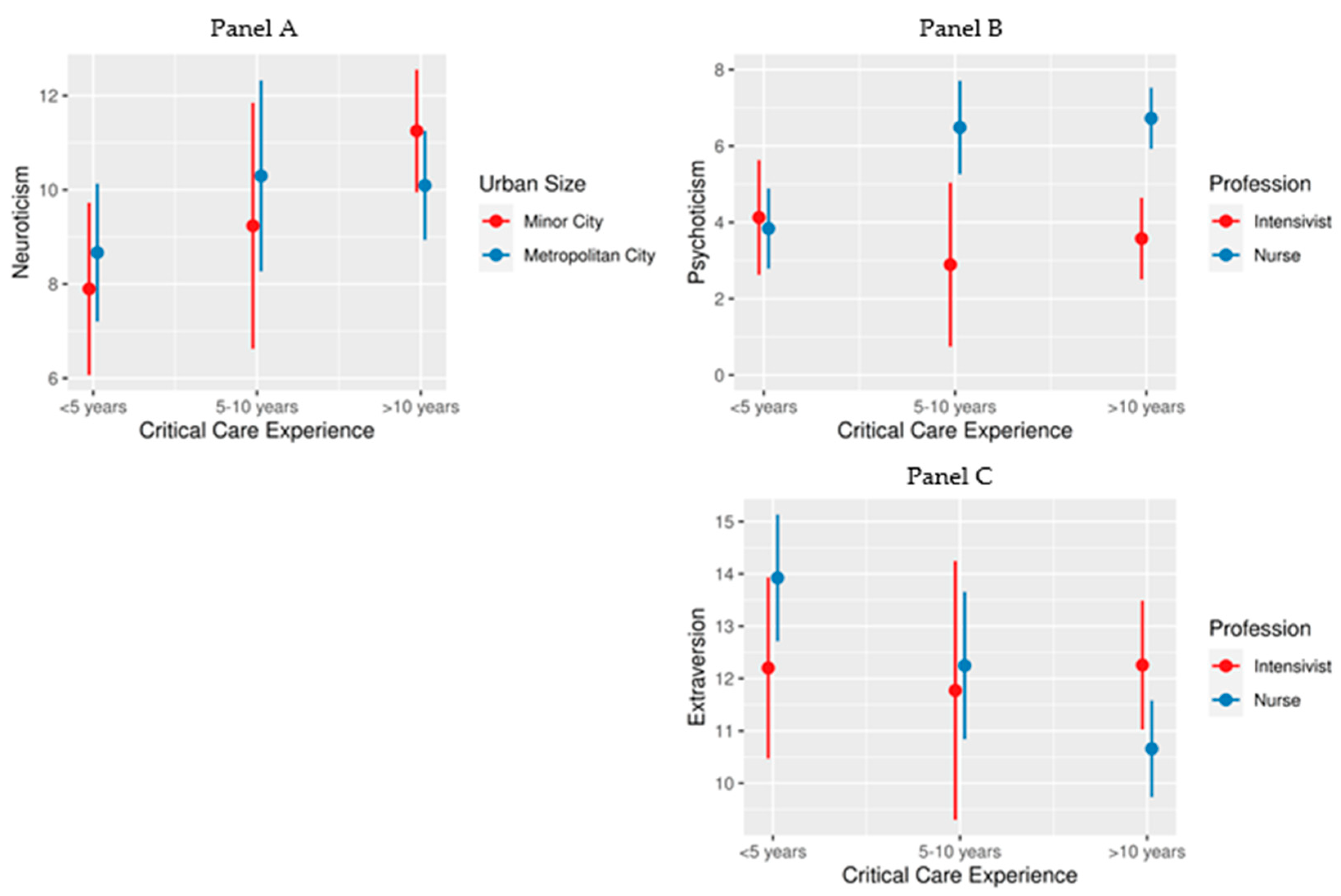
3.3. Moderation Analysis of Personality Dimensions
3.4. Moderation Analysis of Burnout Facets and Psychopathology
3.5. Indirect Effects
4. Discussion
4.1. Personality Dimensions
4.2. Burnout and Psychopathology
5. Conclusions
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Freudenberger, H.J. Staff Burn-Out. J. Soc. Issues 1974, 30, 159–165. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory. In Evaluating Stress: A Book of Resources, 3rd ed.; Scarecrow Education: Lanham, MD, USA, 1997; pp. 191–218. [Google Scholar]
- Grossi, G.; Perski, A.; Osika, W.; Savic, I. Stress-related exhaustion disorder--clinical manifestation of burnout? A review of assessment methods, sleep impairments, cognitive disturbances, and neuro-biological and physiological changes in clinical burnout. Scand. J. Psychol. 2015, 56, 626–636. [Google Scholar] [CrossRef]
- Kelly, L.A.; Gee, P.M.; Butler, R.J. Impact of nurse burnout on organizational and position turnover. Nurs. Outlook 2021, 69, 96–102. [Google Scholar] [CrossRef]
- Khatatbeh, H.; Pakai, A.; Al-Dwaikat, T.; Onchonga, D.; Amer, F.; Prémusz, V.; Oláh, A. Nurses’ burnout and quality of life: A systematic review and critical analysis of measures used. Nurs. Open 2022, 9, 1564–1574. [Google Scholar] [CrossRef] [PubMed]
- Bragard, I.; Dupuis, G.; Fleet, R. Quality of work life, burnout, and stress in emergency department physicians: A qualitative review. Eur. J. Emerg. Med. 2015, 22, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Sanfilippo, F.; Palumbo, G.J.; Noto, A.; Pennisi, S.; Mineri, M.; Vasile, F.; Dezio, V.; Busalacchi, D.; Murabito, P.; Astuto, M. Prevalence of burnout among intensive care physicians: A systematic review. Rev. Bras. Ter. Intensiv. 2020, 32, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Hasan, O.; Dyrbye, L.N.; Sinsky, C.; Satele, D.; Sloan, J.; West, C.P. Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin. Proc. 2015, 90, 1600–1613. [Google Scholar] [CrossRef]
- O’Connor, K.; Muller Neff, D.; Pitman, S. Burnout in mental health professionals: A systematic review and meta-analysis of prevalence and determinants. Eur. Psychiatry 2018, 53, 74–99. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, R.; Christensen, A.E.; Pristed, S.G.; Jepsen, I.; Telléus, G.K. Burnout in Mental Health Care Professionals Working with Inpatients in Open or Closed Wards in Psychiatric Hospitals. Issues Ment. Health Nurs. 2021, 42, 1030–1037. [Google Scholar] [CrossRef]
- Chuang, C.H.; Tseng, P.C.; Lin, C.Y.; Lin, K.H.; Chen, Y.Y. Burnout in the intensive care unit professionals: A systematic review. Medicine 2016, 95, e5629. [Google Scholar] [CrossRef]
- Fahrenkopf, A.M.; Sectish, T.C.; Barger, L.K.; Sharek, P.J.; Lewin, D.; Chiang, V.W.; Edwards, S.; Wiedermann, B.L.; Landrigan, C.P. Rates of medication errors among depressed and burnt out residents: Prospective cohort study. BMJ 2008, 336, 488–491. [Google Scholar] [CrossRef]
- Tawfik, D.S.; Profit, J.; Morgenthaler, T.I.; Satele, D.V.; Sinsky, C.A.; Dyrbye, L.N.; Tutty, M.A.; West, C.P.; Shanafelt, T.D. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin. Proc. 2018, 93, 1571–1580. [Google Scholar] [CrossRef]
- Dewa, C.S.; Loong, D.; Bonato, S.; Thanh, N.X.; Jacobs, P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv. Res. 2014, 14, 325. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Massie, F.S., Jr.; Eacker, A.; Harper, W.; Power, D.; Durning, S.J.; Thomas, M.R.; Moutier, C.; Satele, D.; Sloan, J.; et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA 2010, 304, 1173–1180. [Google Scholar] [CrossRef] [PubMed]
- Rathert, C.; Williams, E.S.; Linhart, H. Evidence for the Quadruple Aim: A Systematic Review of the Literature on Physician Burnout and Patient Outcomes. Med. Care 2018, 56, 976–984. [Google Scholar] [CrossRef] [PubMed]
- Devi, S. Doctors in distress. Lancet 2011, 377, 454–455. [Google Scholar] [CrossRef] [PubMed]
- Williams, E.S.; Skinner, A.C. Outcomes of physician job satisfaction: A narrative review, implications, and directions for future research. Health Care Manag. Rev. 2003, 28, 119–139. [Google Scholar] [CrossRef] [PubMed]
- Dall’Ora, C.; Ball, J.; Reinius, M.; Griffiths, P. Burnout in nursing: A theoretical review. Hum. Resour. Health 2020, 18, 41. [Google Scholar] [CrossRef] [PubMed]
- Flannery, R.B., Jr.; Farley, E.; Tierney, T.; Walker, A.P. Characteristics of assaultive psychiatric patients: 20-year analysis of the Assaultive Staff Action Program (ASAP). Psychiatr. Q. 2011, 82, 1–10. [Google Scholar] [CrossRef]
- Mento, C.; Silvestri, M.C.; Bruno, A.; Muscatello, M.R.A.; Cedro, C.; Pandolfo, G.; Zoccali, R.A. Workplace violence against healthcare professionals: A systematic review. Aggress. Violent Behav. 2020, 51, 101381. [Google Scholar] [CrossRef]
- Mele, F.; Buongiorno, L.; Montalbò, D.; Ferorelli, D.; Solarino, B.; Zotti, F.; Carabellese, F.F.; Catanesi, R.; Bertolino, A.; Dell’Erba, A.; et al. Reporting Incidents in the Psychiatric Intensive Care Unit: A Retrospective Study in an Italian University Hospital. J. Nerv. Ment. Dis. 2022, 210, 622–628. [Google Scholar] [CrossRef]
- Woo, T.; Ho, R.; Tang, A.; Tam, W. Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J. Psychiatr. Res. 2020, 123, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Kimo Takayesu, J.; Ramoska, E.A.; Clark, T.R.; Hansoti, B.; Dougherty, J.; Freeman, W.; Weaver, K.R.; Chang, Y.; Gross, E. Factors associated with burnout during emergency medicine residency. Acad. Emerg. Med. 2014, 21, 1031–1035. [Google Scholar] [CrossRef]
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef] [PubMed]
- Dulko, D.; Zangaro, G.A. Comparison of Factors Associated with Physician and Nurse Burnout. Nurs. Clin. N. Am. 2022, 57, 53–66. [Google Scholar] [CrossRef]
- Ntantana, A.; Matamis, D.; Savvidou, S.; Marmanidou, K.; Giannakou, M.; Gouva, Μ.; Nakos, G.; Koulouras, V. The impact of healthcare professionals’ personality and religious beliefs on the decisions to forego life sustaining treatments: An observational, multicentre, cross-sectional study in Greek intensive care units. BMJ Open 2017, 7, e013916. [Google Scholar] [CrossRef]
- Sikioti, T.; Zartaloudi, A.; Pappa, D.; Mangoulia, P.; Fradelos, E.C.; Kourti, F.E.; Koutelekos, I.; Dousis, E.; Margari, N.; Stavropoulou, A.; et al. Stress and burnout among Greek critical care nurses during the COVID-19 pandemic. AIMS Public Health 2023, 10, 755–774. [Google Scholar] [CrossRef] [PubMed]
- van Mol, M.M.; Kompanje, E.J.; Benoit, D.D.; Bakker, J.; Nijkamp, M.D. The Prevalence of Compassion Fatigue and Burnout among Healthcare Professionals in Intensive Care Units: A Systematic Review. PLoS ONE 2015, 10, e0136955. [Google Scholar] [CrossRef]
- McManus, I.C.; Keeling, A.; Paice, E. Stress, burnout and doctors’ attitudes to work are determined by personality and learning style: A twelve year longitudinal study of UK medical graduates. BMC Med. 2004, 2, 29. [Google Scholar] [CrossRef]
- Eysenck, H. Personality Psychology in Europe: Theoretical and Empirical Developments; Bonarius, H., Van Heck, G., Smid, N., Eds.; Swets & Zeitlinger: Lisse, The Netherlands, 1984. [Google Scholar]
- Maher, B.A.; Maher, W.B. Personality and psychopathology: A historical perspective. J. Abnorm. Psychol. 1994, 103, 72–77. [Google Scholar] [CrossRef]
- Eysenck, H.J.; Eysenck, S.B.G. Manual of the Eysenck Personality Questionnaire: (EPQ-R Adult); EdITS/Educational and Industrial Testing Service San Diego, Calif.: San Diego, CA, USA, 1994. [Google Scholar]
- Eysenck, H.J.; Eysenck, M.W. Personality and Individual Differences: A Natural Science Approach; Eysenck, H.J., Eysenck, M.W., Eds.; Plenum Press: New York, NY, USA, 1985. [Google Scholar]
- Eysenck, H.J.; Eysenck, S.B.G. The Orthogonality of Psychoticism and Neuroticism: A Factorial Study. Percept. Mot. Ski. 1971, 33, 461–462. [Google Scholar] [CrossRef]
- Angelini, G. Big five model personality traits and job burnout: A systematic literature review. BMC Psychol. 2023, 11, 49. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.A.; Slater, M.; Lofters, A. Personality and burnout among primary care physicians: An international study. Psychol. Res. Behav. Manag. 2019, 12, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Divinakumar, K.J.; Bhat, P.S.; Prakash, J.; Srivastava, K. Personality traits and its correlation to burnout in female nurses. Ind. Psychiatry J. 2019, 28, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Grigorescu, S.; Cazan, A.M.; Grigorescu, O.D.; Rogozea, L.M. The role of the personality traits and work characteristics in the prediction of the burnout syndrome among nurses—A new approach within predictive, preventive, and personalized medicine concept. EPMA J. 2018, 9, 355–365. [Google Scholar] [CrossRef]
- Narang, G.; Wymer, K.; Mi, L.; Wolter, C.; Humphreys, M.; Stern, K. Personality Traits and Burnout: A Survey of Practicing US Urologists. Urology 2022, 167, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Prins, D.J.; van Vendeloo, S.N.; Brand, P.L.P.; Van der Velpen, I.; de Jong, K.; van den Heijkant, F.; Van der Heijden, F.; Prins, J.T. The relationship between burnout, personality traits, and medical specialty. A national study among Dutch residents. Med. Teach. 2019, 41, 584–590. [Google Scholar] [CrossRef]
- Louwen, C.; Reidlinger, D.; Milne, N. Profiling health professionals’ personality traits, behaviour styles and emotional intelligence: A systematic review. BMC Med. Educ. 2023, 23, 120. [Google Scholar] [CrossRef]
- Atherton, O.E.; Willroth, E.C.; Graham, E.K.; Luo, J.; Mroczek, D.K.; Lewis-Thames, M.W. Rural-urban differences in personality traits and well-being in adulthood. J. Pers. 2024, 92, 73–87. [Google Scholar] [CrossRef]
- Weidmann, R.; Chopik, W.J. Explicating narrow and broad conceptualizations of environmental influences on personality. J. Pers. 2024, 92, 5–15. [Google Scholar] [CrossRef]
- Probst, J.C.; Laditka, S.B.; Moore, C.G.; Harun, N.; Powell, M.P.; Baxley, E.G. Rural-urban differences in depression prevalence: Implications for family medicine. Fam. Med. 2006, 38, 653–660. [Google Scholar]
- van den Bosch, M.; Meyer-Lindenberg, A. Environmental Exposures and Depression: Biological Mechanisms and Epidemiological Evidence. Annu. Rev. Public Health 2019, 40, 239–259. [Google Scholar] [CrossRef]
- van Os, J.; Kenis, G.; Rutten, B.P. The environment and schizophrenia. Nature 2010, 468, 203–212. [Google Scholar] [CrossRef]
- Szyszkowicz, M.; Rowe, B.H.; Colman, I. Air pollution and daily emergency department visits for depression. Int. J. Occup. Med. Environ. Health 2009, 22, 355–362. [Google Scholar] [CrossRef]
- Power, M.C.; Kioumourtzoglou, M.A.; Hart, J.E.; Okereke, O.I.; Laden, F.; Weisskopf, M.G. The relation between past exposure to fine particulate air pollution and prevalent anxiety: Observational cohort study. BMJ 2015, 350, h1111. [Google Scholar] [CrossRef] [PubMed]
- Newbury, J.B.; Arseneault, L.; Beevers, S.; Kitwiroon, N.; Roberts, S.; Pariante, C.M.; Kelly, F.J.; Fisher, H.L. Association of Air Pollution Exposure With Psychotic Experiences During Adolescence. JAMA Psychiatry 2019, 76, 614–623. [Google Scholar] [CrossRef] [PubMed]
- EEA-JRC. Environment and Human Health: Joint EEA-JRC Report; EUR-OP: Luxembourg, 2013. [Google Scholar]
- iMEdDLAB. Beds and Nursing Staff per COVID ICU. 2021. Available online: https://lab.imedd.org/ypostelexosi-meth-covid-thnitotita-plirotita-esy (accessed on 14 January 2024).
- Anagnostopoulos, F.; Papadatou, D. Factorial composition and internal consistency of the Greek version of the Maslach Burnout Inventory. Psychol. Them. 1992, 5, 183–202. [Google Scholar]
- Dimitriou, E. EPQ personality questionnaire. Greek validation in the Greek population. Engefalos 1986, 23, 41–54. [Google Scholar]
- Donias, S.; Karastergiou, A.; Manos, N. Standardization of the symptom checklist-90-R rating scale in a Greek population. Psychiatriki 1991, 2, 42–48. [Google Scholar]
- Zis, P.; Anagnostopoulos, F.; Sykioti, P. Burnout in medical residents: A study based on the job demands-resources model. Sci. World J. 2014, 2014, 673279. [Google Scholar] [CrossRef]
- Derogatis, L.R. SCL 90 R Administration, Scoring and Procedures Manual II for the Revised Version and Other Instruments of the Psychopathology Rating Scale Series; Clinical Psychometric Research: Towson, MD, USA, 1986. [Google Scholar]
- Cronbach, L.J.; Meehl, P.E. Construct validity in psychological tests. Psychol. Bull. 1955, 52, 281–302. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach (Methodology in the Social Sciences), 2nd ed.; The Guilford Press New York: New York, NY, USA, 2018. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: www.R-project.org (accessed on 14 January 2024).
- Aluja, A.; García, Ó.; García, L.F. A psychometric analysis of the revised Eysenck Personality Questionnaire short scale. Personal. Individ. Differ. 2003, 35, 449–460. [Google Scholar] [CrossRef]
- Lewis, C.A.; Francis, L.J.; Shevlin, M.; Forrest, S. Confirmatory factor analysis of the French translation of the abbreviated form of the revised Eysenck Personality Questionnaire (EPQR-A). Eur. J. Psychol. Assess. 2002, 18, 179–185. [Google Scholar] [CrossRef]
- Escorial, S.; Navas, M.J. Analysis of the Gender Variable in the Eysenck Personality Questionnaire–Revised Scales Using Differential Item Functioning Techniques. Educ. Psychol. Meas. 2007, 67, 990–1001. [Google Scholar] [CrossRef]
- Forrest, S.; Lewis, C.A.; Shevlin, M. Examining the factor structure and differential functioning of the Eysenck personality questionnaire revised–abbreviated. Personal. Individ. Differ. 2000, 29, 579–588. [Google Scholar] [CrossRef]
- Costa, P.T.; McCrae, R.R. Four ways five factors are basic. Personal. Individ. Differ. 1992, 13, 653–665. [Google Scholar] [CrossRef]
- Kennedy, B.; Curtis, K.; Waters, D. Is there a relationship between personality and choice of nursing specialty: An integrative literature review. BMC Nurs. 2014, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Levine, C.D.; Wilson, S.F.; Guido, G.W. Personality factors of critical care nurses. Heart Lung 1988, 17, 392–398. [Google Scholar] [PubMed]
- Scheepers, F.E.; de Mul, J.; Boer, F.; Hoogendijk, W.J. Psychosis as an Evolutionary Adaptive Mechanism to Changing Environments. Front. Psychiatry 2018, 9, 237. [Google Scholar] [CrossRef]
- Nyhagen, R.; Egerod, I.; Rustøen, T.; Lerdal, A.; Kirkevold, M. Unidentified communication challenges in the intensive care unit: A qualitative study using multiple triangulations. Aust. Crit. Care 2023, 36, 215–222. [Google Scholar] [CrossRef]
- Ten Hoorn, S.; Elbers, P.W.; Girbes, A.R.; Tuinman, P.R. Communicating with conscious and mechanically ventilated critically ill patients: A systematic review. Crit. Care 2016, 20, 333. [Google Scholar] [CrossRef] [PubMed]
- Baumgarten, M.; Poulsen, I. Patients’ experiences of being mechanically ventilated in an ICU: A qualitative metasynthesis. Scand. J. Caring Sci. 2015, 29, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, V.; Lindahl, B.; Bergbom, I. Patients’ statements and experiences concerning receiving mechanical ventilation: A prospective video-recorded study. Nurs. Inq. 2012, 19, 247–258. [Google Scholar] [CrossRef]
- Ayuso-Murillo, D.; Colomer-Sánchez, A.; Herrera-Peco, I. Communication skills in ICU and adult hospitalisation unit nursing staff. Enferm. Intensiv. 2017, 28, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.; Mannix, T.; Harrington, A. Nurses’ communication with families in the intensive care unit–a literature review. Nurs. Crit. Care 2017, 22, 70–80. [Google Scholar] [CrossRef]
- Ormel, J.; Jeronimus, B.F.; Kotov, R.; Riese, H.; Bos, E.H.; Hankin, B.; Rosmalen, J.G.M.; Oldehinkel, A.J. Neuroticism and common mental disorders: Meaning and utility of a complex relationship. Clin. Psychol. Rev. 2013, 33, 686–697. [Google Scholar] [CrossRef] [PubMed]
- Li, W.W.; Xie, G. Personality and job satisfaction among Chinese health practitioners: The mediating role of professional quality of life. Health Psychol. Open 2020, 7, 2055102920965053. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Zhang, F.; Tang, X.; Wang, L.; Zan, J.; Zhu, Y.; Feng, D. Do type A personality and neuroticism moderate the relationships of occupational stressors, job satisfaction and burnout among Chinese older nurses? A cross-sectional survey. BMC Nurs. 2022, 21, 88. [Google Scholar] [CrossRef]
- Myhren, H.; Ekeberg, O.; Stokland, O. Job Satisfaction and Burnout among Intensive Care Unit Nurses and Physicians. Crit. Care Res. Pract. 2013, 2013, 786176. [Google Scholar] [CrossRef] [PubMed]
- Papazian, L.; Hraiech, S.; Loundou, A.; Herridge, M.S.; Boyer, L. High-level burnout in physicians and nurses working in adult ICUs: A systematic review and meta-analysis. Intensive Care Med. 2023, 49, 387–400. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Elvira, S.; Romero-Béjar, J.L.; Suleiman-Martos, N.; Gómez-Urquiza, J.L.; Monsalve-Reyes, C.; Cañadas-De la Fuente, G.A.; Albendín-García, L. Prevalence, Risk Factors and Burnout Levels in Intensive Care Unit Nurses: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 11432. [Google Scholar] [CrossRef] [PubMed]
- Leiter, M.P.; Spence Laschinger, H.K. Relationships of work and practice environment to professional burnout: Testing a causal model. Nurs. Res. 2006, 55, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Asl, R.G.; Taghinejad, R.; Parizad, N.; Jasemi, M. The Relationship Between Professional Autonomy and Job Stress Among Intensive Care Unit Nurses: A Descriptive Correlational Study. Iran. J. Nurs. Midwifery Res. 2022, 27, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Bégat, I.; Ellefsen, B.; Severinsson, E. Nurses’ satisfaction with their work environment and the outcomes of clinical nursing supervision on nurses’ experiences of well-being—A Norwegian study. J. Nurs. Manag. 2005, 13, 221–230. [Google Scholar] [CrossRef]
- Krukowska-Sitek, H.; Krupa, S.; Grad, I. The Impact of the COVID-19 Pandemic on the Professional Autonomy of Anesthesiological Nurses and Trust in the Therapeutic Team of Intensive Therapy Units-Polish Multicentre Study. Int. J. Environ. Res. Public Health 2022, 19, 12755. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-García, C.; Solano-Ruíz Mdel, C.; Martínez-Roche, M.E.; Gómez-García, C.I. Job satisfaction among health care workers: The role of gender and age. Rev. Lat. Am. Enferm. 2013, 21, 1314–1320. [Google Scholar] [CrossRef]
- Padilla Fortunatti, C.; Palmeiro-Silva, Y.K. Effort-Reward Imbalance and Burnout Among ICU Nursing Staff: A Cross-Sectional Study. Nurs. Res. 2017, 66, 410–416. [Google Scholar] [CrossRef]
- Poncet, M.C.; Toullic, P.; Papazian, L.; Kentish-Barnes, N.; Timsit, J.F.; Pochard, F.; Chevret, S.; Schlemmer, B.; Azoulay, E. Burnout syndrome in critical care nursing staff. Am. J. Respir. Crit. Care Med. 2007, 175, 698–704. [Google Scholar] [CrossRef]
- Kashtanov, A.; Molotok, E.; Yavorovskiy, A.; Boyarkov, A.; Vasil’ev, Y.; Alsaegh, A.; Dydykin, S.; Kytko, O.; Meylanova, R.; Enina, Y.; et al. A Comparative Cross-Sectional Study Assessing the Psycho-Emotional State of Intensive Care Units’ Physicians and Nurses of COVID-19 Hospitals of a Russian Metropolis. Int. J. Environ. Res. Public Health 2022, 19, 1828. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.E.; Milward, J.; Spoiala, C.; Bhogal, J.K.; Weston, D.; Potts, H.W.W.; Caulfield, T.; Toolan, M.; Kanga, K.; El-Sheikha, S.; et al. The mental health of staff working on intensive care units over the COVID-19 winter surge of 2020 in England: A cross sectional survey. Br. J. Anaesth. 2022, 128, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Dragioti, E.; Tsartsalis, D.; Mentis, M.; Mantzoukas, S.; Gouva, M. Impact of the COVID-19 pandemic on the mental health of hospital staff: An umbrella review of 44 meta-analyses. Int. J. Nurs. Stud. 2022, 131, 104272. [Google Scholar] [CrossRef] [PubMed]
- Aslanidis, V.; Tsolaki, V.; Papadonta, M.E.; Amanatidis, T.; Parisi, K.; Makris, D.; Zakynthinos, E. The Impact of the COVID-19 Pandemic on Mental Health and Quality of Life in COVID-19 Department Healthcare Workers in Central Greece. J. Pers. Med. 2023, 13, 250. [Google Scholar] [CrossRef]
- Blekas, A.; Voitsidis, P.; Athanasiadou, M.; Parlapani, E.; Chatzigeorgiou, A.F.; Skoupra, M.; Syngelakis, M.; Holeva, V.; Diakogiannis, I. COVID-19: PTSD symptoms in Greek health care professionals. Psychol. Trauma. 2020, 12, 812–819. [Google Scholar] [CrossRef] [PubMed]
- Mavrovounis, G.; Mavrovouni, D.; Mermiri, M.; Papadaki, P.; Chalkias, A.; Zarogiannis, S.; Christodoulou, N.; Gourgoulianis, K.; Pantazopoulos, I. Watch Out for Burnout in COVID-19: A Greek Health Care Personnel Study. Inquiry 2022, 59, 469580221097829. [Google Scholar] [CrossRef]
- Milas, G.P.; Issaris, V.; Zareifopoulos, N. Burnout for medical professionals during the COVID-19 pandemic in Greece; the role of primary care. Hosp Pr. 2022, 50, 102–103. [Google Scholar] [CrossRef] [PubMed]
- Benincasa, V.; Passannante, M.; Perrini, F.; Carpinelli, L.; Moccia, G.; Marinaci, T.; Capunzo, M.; Pironti, C.; Genovese, A.; Savarese, G.; et al. Burnout and Psychological Vulnerability in First Responders: Monitoring Depersonalization and Phobic Anxiety during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 2794. [Google Scholar] [CrossRef]
- Hou, J.; Xu, B.; Zhang, J.; Luo, L.; Pen, X.; Chen, S.; Ma, G.; Hu, Z.; Kong, X. Psychological Status and Job Burnout of Nurses Working in the Frontline of the Novel Coronavirus in China During the Delta Variant Outbreak: A Cross-Sectional Survey. Psychol. Res. Behav. Manag. 2022, 15, 533–546. [Google Scholar] [CrossRef]
- Rössler, W.; Hengartner, M.P.; Ajdacic-Gross, V.; Angst, J. Predictors of burnout: Results from a prospective community study. Eur. Arch. Psychiatry Clin. Neurosci. 2015, 265, 19–25. [Google Scholar] [CrossRef]
- Saulsman, L.M.; Page, A.C. The five-factor model and personality disorder empirical literature: A meta-analytic review. Clin. Psychol. Rev. 2004, 23, 1055–1085. [Google Scholar] [CrossRef] [PubMed]
- Strickhouser, J.E.; Zell, E.; Krizan, Z. Does personality predict health and well-being? A metasynthesis. Health Psychol. 2017, 36, 797–810. [Google Scholar] [CrossRef] [PubMed]
- Lederbogen, F.; Kirsch, P.; Haddad, L.; Streit, F.; Tost, H.; Schuch, P.; Wüst, S.; Pruessner, J.C.; Rietschel, M.; Deuschle, M.; et al. City living and urban upbringing affect neural social stress processing in humans. Nature 2011, 474, 498–501. [Google Scholar] [CrossRef] [PubMed]
- Peen, J.; Schoevers, R.A.; Beekman, A.T.; Dekker, J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr. Scand. 2010, 121, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Oreskovich, M.R. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch. Intern. Med. 2012, 172, 1377–1385. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Erwin, P.J.; Shanafelt, T.D. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet 2016, 388, 2272–2281. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Sinsky, C.; Trockel, M.; Tutty, M.; Nedelec, L.; Carlasare, L.E.; Shanafelt, T.D. Resilience and Burnout Among Physicians and the General US Working Population. JAMA Netw. Open 2020, 3, e209385. [Google Scholar] [CrossRef]
- West, C.P.; Shanafelt, T.D.; Kolars, J.C. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA 2011, 306, 952–960. [Google Scholar] [CrossRef]
- Xing, J.; Sun, N.; Xu, J.; Geng, S.; Li, Y. Study of the mental health status of medical personnel dealing with new coronavirus pneumonia. PLoS ONE 2020, 15, e0233145. [Google Scholar] [CrossRef]
- Pachi, A.; Kavourgia, E.; Bratis, D.; Fytsilis, K.; Papageorgiou, S.M.; Lekka, D.; Sikaras, C.; Tselebis, A. Anger and Aggression in Relation to Psychological Resilience and Alcohol Abuse among Health Professionals during the First Pandemic Wave. Healthcare 2023, 11, 2031. [Google Scholar] [CrossRef]
- Flannery, L.; Ramjan, L.M.; Peters, K. End-of-life decisions in the Intensive Care Unit (ICU)—Exploring the experiences of ICU nurses and doctors—A critical literature review. Aust. Crit. Care 2016, 29, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Van den Bulcke, B.; Metaxa, V.; Reyners, A.K.; Rusinova, K.; Jensen, H.I.; Malmgren, J.; Darmon, M.; Talmor, D.; Meert, A.P.; Cancelliere, L.; et al. Ethical climate and intention to leave among critical care clinicians: An observational study in 68 intensive care units across Europe and the United States. Intensive Care Med. 2020, 46, 46–56. [Google Scholar] [CrossRef]
- Moss, M.; Good, V.S.; Gozal, D.; Kleinpell, R.; Sessler, C.N. An Official Critical Care Societies Collaborative Statement-Burnout Syndrome in Critical Care Health-care Professionals: A Call for Action. Chest 2016, 150, 17–26. [Google Scholar] [CrossRef] [PubMed]
- De Hert, S. Burnout in Healthcare Workers: Prevalence, Impact and Preventative Strategies. Local. Reg. Anesth. 2020, 13, 171–183. [Google Scholar] [CrossRef] [PubMed]
- Garcia, C.L.; Abreu, L.C.; Ramos, J.L.S.; Castro, C.F.D.; Smiderle, F.R.N.; Santos, J.A.D.; Bezerra, I.M.P. Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina 2019, 55, 553. [Google Scholar] [CrossRef]
- Ryu, I.S.; Shim, J. The Influence of Burnout on Patient Safety Management Activities of Shift Nurses: The Mediating Effect of Compassion Satisfaction. Int. J. Environ. Res. Public Health 2021, 18, 12210. [Google Scholar] [CrossRef]
- Welp, A.; Meier, L.L.; Manser, T. Emotional exhaustion and workload predict clinician-rated and objective patient safety. Front. Psychol. 2014, 5, 1573. [Google Scholar] [CrossRef]
- Haas, J.S.; Cook, E.F.; Puopolo, A.L.; Burstin, H.R.; Cleary, P.D.; Brennan, T.A. Is the professional satisfaction of general internists associated with patient satisfaction? J. Gen. Intern. Med. 2000, 15, 122–128. [Google Scholar] [CrossRef]


| Personality Traits | Burnout Facets | |||||||
|---|---|---|---|---|---|---|---|---|
| a | Extraversion | Neuroticism | Psychoticism | Emotional Exhaustion | Depersonalization | Personal Achievement | ||
| Personality Traits | Extraversion | 0.871 | ||||||
| Neuroticism | 0.951 | −0.127 ** | ||||||
| Psychoticism | 0.907 | −0.180 ** | 0.225 ** | |||||
| Burnout facets | Emotional exhaustion | 0.839 | −0.131 ** | 0.370 ** | 0.133 ** | |||
| Depersonalization | 0.767 | −0.078 | 0.297 ** | 0.277 ** | 0.624 ** | |||
| Personal achievement | 0.828 | 0.345 ** | −0.167 ** | −0.349 ** | −0.045 | −0.128 ** | ||
| Global severity index (GSI) | 0.99 | −0.168 ** | 0.476 ** | 0.474 ** | 0.512 ** | 0.431 ** | −0.197 ** | |
| Scale | Total (N = 503) | Profession | Sex | Critical Care Experience | Urban Size of ICU Location | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intensivist (n = 155) | Nurse (n = 348) | Male (n = 164) | Female (n = 339) | <5 Years (n = 166) | 5–10 Years (n = 105) | 10–15 Years (n = 232) | Metropolitan (n = 309) | Other (n = 194) | ||
| Age | 41.5 (8.4) | 45.7 (8.1) | 39.6 (7.8) | 43.0 (8.8) | 41.0 (8.1) | 35 (6.4) | 42 (7.0) | 46 (7.1) | 41.6 (8.5) | 41.4 (8.2) |
| Personality traits | ||||||||||
| Psychoticism | 5.8 (3.9) | 4.5 (3.2) | 6.3 (4.0) | 6.3 (4.3) | 5.5 (3.7) | 4.9 (3.1) | 6.6 (4.5) | 5.9 (4.0) | 5.8 (4) | 5.7 (3.8) |
| Extraversion | 12.2 (4.3) | 12.1 (4.26) | 12.2 (4.3) | 12.1 (4.2) | 12.2 (4.3) | 13.2 (4.2) | 12.0 (4.2) | 11.0 (4.2) | 12.2 (4.2) | 12.1 (4.4) |
| Neuroticism | 10.7 (4.5) | 9.85 (4.62) | 11.1 (4.4) | 10.2 (4.8) | 10.9 (4.4) | 9.6 (4.3) | 11.0 (4.7) | 11.0 (4.4) | 10.5 (4.3) | 10.9 (4.9) |
| Burnout facets | ||||||||||
| Emotional exhaustion | 25.6 (11.1) | 24.4 (10.8) | 26.2 (11.2) | 24.8 (11.6) | 26 (10.8) | 23.7 (10.3) | 25.0 (11.0) | 27.0 (11.0) | 26 (11.2) | 25 (10.9) |
| Depersonalization | 10.4 (6.6) | 10.1 (7.0) | 10.6 (6.4) | 10.8 (7.0) | 10.3 (6.4) | 9.5 (6.3) | 10.0 (6.5) | 11.0 (6.7) | 10.8 (6.6) | 9.9 (6.6) |
| Personal achievement | 31.2 (8.7) | 33.7 (7.1) | 30.1 (9.1) | 32.2 (8.4) | 30.7 (8.8) | 32.5 (7.7) | 30.0 (10.0) | 31.0 (8.7) | 31.7 (8.4) | 30.5 (9.1) |
| Global severity index (GSI) | 0.89 (0.72) | 0.72 (0.57) | 0.96 (0.77) | 0.84 (0.81) | 0.91 (0.67) | 0.71 (0.60) | 1.1 (0.87) | 0.93 (0.70) | 0.92 (0.73) | 0.85 (0.70) |
| Emotional Exhaustion | Depersonalization | Personal Achievement | ||
|---|---|---|---|---|
| Low (≤29) | Moderate (30–38) | High (≥39) | ||
| Low (≤16) | Low (≤4) | 20 (12/8) (1) | 16 (5/11) | 9 (4/5) |
| Moderate (5–12) | 13 (7/6) | 14 (7/7) | 27 (2/25) | |
| High (≥13) | 5 (2/3) | 1 (0/1) | 0 (0/0) | |
| Moderate (17–33) | Low (≤4) | 21 (8/13) | 25 (11/14) | 10 (2/8) |
| Moderate (5–12) | 20 (9/11) | 52 (11/41) | 48 (8/40) | |
| High (≥13) | 13 (2/11) | 34 (13/21) | 46 (14/32) | |
| High (≥34) | Low (≤4) | 2 (1/1) | 2 (1/1) | 0 (0/0) |
| Moderate (5–12) | 2 (1/1) | 11 (4/7) | 23 (3/20) | |
| High (≥13) | 19 (5/14) | 38 (13/25) | 32 (10/22) | |
| Neuroticism (1) | Psychoticism (2) | Extraversion (3) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | p | 95% C.I. | B | p | 95% C.I. | B | p | 95% C.I. | ||||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| Constant | 5.283 | 0.028 | 0.562 | 10.00 | 5.157 | 0.009 | 1.275 | 9.039 | 11.07 | 0.000 | 6.600 | 15.55 |
| Critical Care Experience | ||||||||||||
| D1: 5–10 vs. <5 | 1.364 | 0.700 | −5.598 | 8.326 | −5.543 | 0.058 | −11.27 | 0.180 | 0.522 | 0.877 | −6.073 | 7.116 |
| D2: 10–15 vs. 5–10 | 4.231 | 0.194 | −2.155 | 10.62 | 1.642 | 0.539 | −3.608 | 6.892 | 2.152 | 0.485 | −3.896 | 8.201 |
| Profession | 1.693 | 0.038 | 0.091 | 3.294 | −0.289 | 0.666 | −1.606 | 1.027 | 1.721 | 0.026 | 0.204 | 3.238 |
| Critical Care Experience × Profession | ||||||||||||
| D1 × Profess. | −0.311 | 0.824 | −3.065 | 2.442 | 3.883 | 0.001 | 1.620 | 6.147 | −1.246 | 0.348 | −3.855 | 1.362 |
| D2 × Profess. | −0.001 | 0.999 | −2.556 | 2.554 | −0.444 | 0.678 | −2.545 | 1.656 | −2.074 | 0.093 | −4.494 | 0.346 |
| Urban size of ICU Location | 0.771 | 0.287 | −0.651 | 2.194 | 0.370 | 0.534 | −0.799 | 1.540 | −0.325 | 0.636 | −1.672 | 1.022 |
| Critical Care Experience × Uban Size of ICU Location | ||||||||||||
| D1 × Urban Size of ICU Location | 0.288 | 0.808 | −2.040 | 2.615 | 0.424 | 0.663 | −1.489 | 2.337 | 0.295 | 0.793 | −1.909 | 2.499 |
| D2 × Urban Size of ICU Location | −2.216 | 0.046 | −4.392 | −0.040 | −0.515 | 0.572 | −2.304 | 1.273 | 0.406 | 0.699 | −1.655 | 2.467 |
| Age | 0.004 | 0.907 | −0.057 | 0.064 | −0.027 | 0.289 | −0.076 | 0.023 | −0.006 | 0.824 | −0.064 | 0.051 |
| Sex | −0.199 | 0.647 | −1.054 | 0.655 | 1.421 | 0.000 | 0.719 | 2.123 | −0.246 | 0.550 | −1.055 | 0.563 |
| High Emotional Exhaustion (1) | High Depersonalization (2) | Low Personal Achievement (3) | Global Severity Index (GSI) (4) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | p | 95% C.I. | B | p | 95% C.I. | B | p | 95% C.I. | B | p | 95% C.I. | |||||
| Lower | Upper | Lower | Upper | Lower | Upper | Lower | Upper | |||||||||
| Constant | −0.571 | 0.840 | −6.126 | 4.984 | −2.857 | 0.277 | −8.006 | 2.292 | 0.130 | 0.962 | −5.190 | 5.451 | −0.367 | 0.578 | −1.662 | 0.929 |
| Socio-demographics | ||||||||||||||||
| Age | 0.037 | 0.027 | 0.004 | 0.071 | 0.017 | 0.265 | −0.013 | 0.047 | −0.050 | 0.004 | −0.084 | −0.015 | 0.009 | 0.020 | 0.001 | 0.017 |
| Sex | 0.135 | 0.588 | −0.353 | 0.623 | 0.018 | 0.937 | −0.422 | 0.458 | −0.449 | 0.070 | −0.934 | 0.037 | −0.070 | 0.230 | −0.183 | 0.044 |
| Critical Care Experience | ||||||||||||||||
| D1: 5–10 vs. <5 | −1.365 | 0.532 | −5.644 | 2.914 | −2.395 | 0.249 | −6.470 | 1.681 | 0.434 | 0.832 | −3.565 | 4.432 | −0.174 | 0.712 | −1.102 | 0.753 |
| D2: 10–15 vs. 5–10 | 0.938 | 0.626 | −2.835 | 4.712 | 2.438 | 0.194 | −1.244 | 6.119 | −4.318 | 0.025 | −8.092 | −0.545 | −0.113 | 0.790 | −0.950 | 0.723 |
| Profession | −0.904 | 0.431 | −3.153 | 1.345 | 0.261 | 0.804 | −1.800 | 2.322 | 0.944 | 0.387 | −1.196 | 3.085 | 0.132 | 0.614 | −0.381 | 0.645 |
| D1 × Profession | −0.138 | 0.869 | −1.772 | 1.496 | 0.736 | 0.399 | −0.975 | 2.448 | −0.031 | 0.970 | −1.619 | 1.558 | −0.005 | 0.976 | −0.371 | 0.360 |
| D2 × Profession | 0.485 | 0.514 | −0.972 | 1.942 | −1.356 | 0.092 | −2.934 | 0.222 | 1.967 | 0.012 | 0.433 | 3.501 | 0.062 | 0.714 | −0.272 | 0.397 |
| Urban Size of ICU Location | −1.472 | 0.172 | −3.585 | 0.642 | −0.225 | 0.813 | −2.091 | 1.641 | 0.060 | 0.950 | −1.842 | 1.963 | −0.178 | 0.468 | −0.658 | 0.303 |
| D1 × Urban Size of ICU Location | 0.708 | 0.355 | −0.791 | 2.208 | 0.554 | 0.368 | −0.652 | 1.760 | −0.160 | 0.803 | −1.418 | 1.098 | 0.151 | 0.338 | −0.159 | 0.462 |
| D2 × Urban Size of ICU Location | −0.664 | 0.329 | −1.998 | 0.669 | 0.238 | 0.672 | −0.863 | 1.339 | 0.674 | 0.260 | −0.499 | 1.846 | −0.068 | 0.639 | −0.355 | 0.218 |
| Personality Traits | ||||||||||||||||
| P | 0.229 | 0.189 | −0.113 | 0.571 | 0.455 | 0.014 | 0.092 | 0.818 | 0.488 | 0.014 | 0.098 | 0.877 | 0.029 | 0.502 | −0.056 | 0.114 |
| E | −0.234 | 0.105 | −0.518 | 0.049 | −0.207 | 0.121 | −0.470 | 0.055 | −0.224 | 0.148 | −0.528 | 0.080 | −0.019 | 0.578 | −0.085 | 0.048 |
| N | −0.039 | 0.782 | −0.315 | 0.237 | 0.168 | 0.191 | −0.084 | 0.421 | 0.327 | 0.033 | 0.026 | 0.627 | 0.082 | 0.011 | 0.019 | 0.145 |
| P × Profession | −0.099 | 0.147 | −0.233 | 0.035 | −0.233 | 0.003 | −0.388 | −0.077 | −0.182 | 0.029 | −0.346 | −0.019 | −0.011 | 0.529 | −0.045 | 0.023 |
| E × Profession | 0.060 | 0.311 | −0.056 | 0.175 | 0.098 | 0.072 | −0.009 | 0.205 | 0.009 | 0.885 | −0.113 | 0.131 | −0.001 | 0.928 | −0.028 | 0.026 |
| N × Profession | 0.066 | 0.237 | −0.044 | 0.176 | −0.012 | 0.814 | −0.113 | 0.088 | −0.086 | 0.162 | −0.206 | 0.034 | −0.001 | 0.911 | −0.027 | 0.024 |
| P × Urban Size of ICU Location | −0.019 | 0.759 | −0.141 | 0.103 | 0.039 | 0.487 | −0.071 | 0.150 | 0.001 | 0.982 | −0.120 | 0.123 | 0.036 | 0.017 | 0.006 | 0.065 |
| E × Urban Size of ICU Location | 0.087 | 0.112 | −0.021 | 0.195 | 0.022 | 0.658 | −0.075 | 0.119 | 0.045 | 0.422 | −0.064 | 0.154 | 0.009 | 0.476 | −0.016 | 0.034 |
| N × Urban Size of ICU Location | 0.037 | 0.504 | −0.071 | 0.145 | −0.044 | 0.368 | −0.139 | 0.051 | −0.088 | 0.098 | −0.193 | 0.016 | −0.012 | 0.354 | −0.036 | 0.013 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pakou, V.; Tsartsalis, D.; Papathanakos, G.; Dragioti, E.; Gouva, M.; Koulouras, V. Personality Traits, Burnout, and Psychopathology in Healthcare Professionals in Intensive Care Units—A Moderated Analysis. Healthcare 2024, 12, 587. https://doi.org/10.3390/healthcare12050587
Pakou V, Tsartsalis D, Papathanakos G, Dragioti E, Gouva M, Koulouras V. Personality Traits, Burnout, and Psychopathology in Healthcare Professionals in Intensive Care Units—A Moderated Analysis. Healthcare. 2024; 12(5):587. https://doi.org/10.3390/healthcare12050587
Chicago/Turabian StylePakou, Varvara, Dimitrios Tsartsalis, Georgios Papathanakos, Elena Dragioti, Mary Gouva, and Vasilios Koulouras. 2024. "Personality Traits, Burnout, and Psychopathology in Healthcare Professionals in Intensive Care Units—A Moderated Analysis" Healthcare 12, no. 5: 587. https://doi.org/10.3390/healthcare12050587
APA StylePakou, V., Tsartsalis, D., Papathanakos, G., Dragioti, E., Gouva, M., & Koulouras, V. (2024). Personality Traits, Burnout, and Psychopathology in Healthcare Professionals in Intensive Care Units—A Moderated Analysis. Healthcare, 12(5), 587. https://doi.org/10.3390/healthcare12050587








