Biopsychosocial Predictors of Postpartum Depression: Protocol for Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Objectives
- Identify biological peripartum risk factors and calculate pooled prevalence of PPD for each of them.
- Explore associations between biological peripartum risk factors and PPD.
- Rank the predictors by their prevalence and strength.
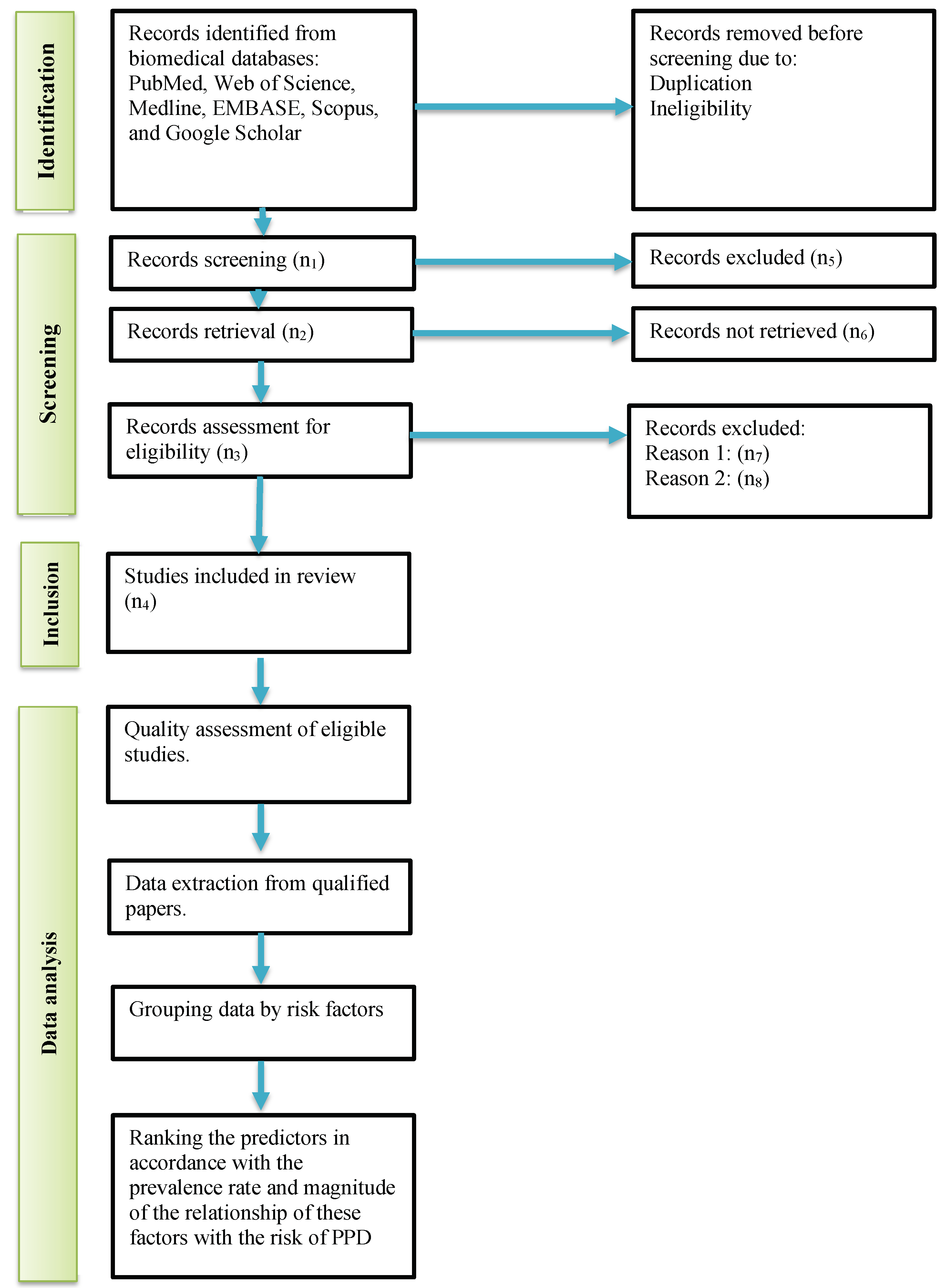
3. Materials and Methods
3.1. Study Design and Data Source
3.2. Eligibility Criteria
3.3. Study Records
3.4. Study Methodology
4. Discussion
4.1. Pathogenesis of Postpartum Depression
4.2. Biological Risks of Postpartum Depression
4.3. Socioeconomic and Demographic Confounders
5. Conclusions
6. Strength and Limitations
- The protocol is prepared in accordance with the PRISMA-P checklist for systematic reviews; the protocol is registered with the international database for systematic reviews PROSPERO.
- The study will focus on the biological peripartum risk factors for PPD, which are not studied well.
- The socioeconomic and demographic risks will also be included in the analysis as confounders.
- We will perform subgroup analysis to evaluate the consistency of findings across multiple observational groups. If the risk of PPD varies markedly among different categories of patients, we will check whether studies replicate and add confidence to the findings. If not, we will not derive conclusions from such data.
- A notable limitation of the proposed study is scarcity of findings on biological peripartum risk factors for PPD. If we fail to perform the meta-analysis, a narrative systematic review will be conducted.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, X.; Wang, S.; Wang, G. Prevalence and risk factors of postpartum depression in women: A systematic review and meta-analysis. J. Clin. Nurs. 2022, 31, 2665–2677. [Google Scholar] [CrossRef] [PubMed]
- Yim, I.S.; Tanner Stapleton, L.R.; Guardino, C.M.; Hahn-Holbrook, J.; Dunkel Schetter, C. Biological and psychosocial predictors of postpartum depression: Systematic review and call for integration. Annu. Rev. Clin. Psychol. 2015, 11, 99–137. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, J.; Shuai, H.; Cai, Z.; Fu, X.; Liu, Y.; Xiao, X.; Zhang, W.; Krabbendam, E.; Liu, S.; et al. Mapping global prevalence of depression among postpartum women. Transl. Psychiatry 2021, 11, 543. [Google Scholar] [CrossRef] [PubMed]
- Shorey, S.; Chee, C.Y.I.; Ng, E.D.; Chan, Y.H.; San Tam, W.W.; Chong, Y.S. Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. J. Psychiatr. Res. 2018, 104, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Affonso, D.D.; De, A.K.; Horowitz, J.A.; Mayberry, L.J. An international study exploring levels of postpartum depressive symptomatology. J. Psychosom. Res. 2000, 49, 207–216. [Google Scholar] [CrossRef]
- Alshikh Ahmad, H.; Alkhatib, A.; Luo, J. Prevalence and risk factors of postpartum depression in the Middle East: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2021, 21, 542. [Google Scholar] [CrossRef]
- Haque, A.; Namavar, A.; Breene, K.A. Prevalence and risk factors of postpartum depression in Middle Eastern/Arab women. J. Muslim Ment. Health 2015, 9, 65–84. [Google Scholar] [CrossRef]
- Al Rehaili, B.O.; Al-Raddadi, R.; ALEnezi, N.K.; ALYami, A.H. Postpartum quality of life and associated factors: A cross-sectional study. Qual. Life Res. 2023, 32, 2099–2106. [Google Scholar] [CrossRef]
- Jeong, Y.J.; Nho, J.H.; Kim, H.Y.; Kim, J.Y. Factors influencing quality of life in early postpartum women. Int. J. Environ. Res. Public Health 2021, 18, 2988. [Google Scholar] [CrossRef]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.Y.; Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Health 2019, 15, 1745506519844044. [Google Scholar] [CrossRef]
- Faisal-Cury, A.; Bertazzi Levy, R.; Kontos, A.; Tabb, K.; Matijasevich, A. Postpartum bonding at the beginning of the second year of child’s life: The role of postpartum depression and early bonding impairment. J. Psychosom. Obstet. Gynecol. 2020, 41, 224–230. [Google Scholar] [CrossRef]
- Netsi, E.; Pearson, R.M.; Murray, L.; Cooper, P.; Craske, M.G.; Stein, A. Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry 2018, 75, 247–253. [Google Scholar] [CrossRef]
- Mughal, S.; Azhar, Y.; Siddiqui, W.; May, K. Postpartum depression (nursing). In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Naviaux, A.F.; Janne, P.; Gourdin, M. Psychiatric considerations on infanticide: Throwing the baby out with the bathwater. Psychiatr. Danub. 2020, 32, 24–28. [Google Scholar] [PubMed]
- Barooj-Kiakalaee, O.; Hosseini, S.H.; Mohammadpour-Tahmtan, R.A.; Hosseini-Tabaghdehi, M.; Jahanfar, S.; Esmaeili-Douki, Z.; Shahhosseini, Z. Paternal postpartum depression’s relationship to maternal pre and postpartum depression, and father-mother dyads marital satisfaction: A structural equation model analysis of a longitudinal study. J. Affect. Disord. 2022, 297, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Salm Ward, T.; Kanu, F.A.; Robb, S.W. Prevalence of stressful life events during pregnancy and its association with postpartum depressive symptoms. Arch. Women’s Ment. Health 2017, 20, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Johannsen, B.M.; Mægbæk, M.L.; Bech, B.H.; Laursen, T.M.; Munk-Olsen, T. Divorce or Separation Following Postpartum Psychiatric Episodes: A Population-Based Cohort Study. J. Clin. Psychiatry 2021, 82, 29461. [Google Scholar] [CrossRef]
- Lindahl, V.; Pearson, J.L.; Colpe, L. Prevalence of suicidality during pregnancy and the postpartum. Arch. Women’s Ment. Health 2005, 8, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, P.; Rostami, M. Postpartum depression and suicide in Iran. Women’s Health 2021, 17, 17455065211043994. [Google Scholar] [CrossRef] [PubMed]
- Hanach, N.; Radwan, H.; Fakhry, R.; Dennis, C.L.; Issa, W.B.; Faris, M.E.; Obaid, R.S.; Al Marzooqi, S.; Tabet, C.; De Vries, N. Prevalence and risk factors of postpartum depression among women living in the United Arab Emirates. Soc. Psychiatry Psychiatr. Epidemiol. 2023, 58, 395–407. [Google Scholar] [CrossRef]
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef]
- de Avila Quevedo, L.; Scholl, C.C.; de Matos, M.B.; da Silva, R.A.; da Cunha Coelho, F.M.; Pinheiro, K.A.T.; Pinheiro, R.T. Suicide risk and mood disorders in women in the postpartum period: A longitudinal study. Psychiatr. Q. 2021, 92, 513–522. [Google Scholar] [CrossRef]
- Lee, Y.L.; Tien, Y.; Bai, Y.S.; Lin, C.K.; Yin, C.S.; Chung, C.H.; Sun, C.A.; Huang, S.H.; Huang, Y.C.; Chien, W.C.; et al. Association of postpartum depression with maternal suicide: A nationwide population-based study. Int. J. Environ. Res. Public Health 2022, 19, 5118. [Google Scholar] [CrossRef] [PubMed]
- Moraes, I.G.d.S.; Pinheiro, R.T.; Silva, R.A.d.; Horta, B.L.; Sousa, P.L.R.; Faria, A.D. Prevalence of postpartum depression and associated factors. Rev. Saúde Pública 2006, 40, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Park, J.h.; Karmaus, W.; Zhang, H. Prevalence of and risk factors for depressive symptoms in Korean women throughout pregnancy and in postpartum period. Asian Nurs. Res. 2015, 9, 219–225. [Google Scholar] [CrossRef]
- Drozd, F.; Haga, S.M.; Valla, L.; Slinning, K. Latent trajectory classes of postpartum depressive symptoms: A regional population-based longitudinal study. J. Affect. Disord. 2018, 241, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Selcuki, N.F.T.; Bahat, P.Y.; Turan, G.; Aksoy, U.; Bagci, K.; Ozdemir, I. Postpartum evaluation of the role of maternal characteristics and mode of delivery on maternal attachment, anxiety and depression; a study conducted in Turkey. Acta Bio Med. Atenei Parm. 2022, 93, e2022011. [Google Scholar]
- Goyal, D.; Gay, C.; Lee, K.A. How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first-time mothers? Women’s Health Issues 2010, 20, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Rupanagunta, G.P.; Nandave, M.; Rawat, D.; Upadhyay, J.; Rashid, S.; Ansari, M.N. Postpartum depression: Aetiology, pathogenesis and the role of nutrients and dietary supplements in prevention and management. Saudi Pharm. J. SPJ 2023, 31, 1274. [Google Scholar] [CrossRef]
- Worthen, R.J.; Beurel, E. Inflammatory and neurodegenerative pathophysiology implicated in postpartum depression. Neurobiol. Dis. 2022, 165, 105646. [Google Scholar] [CrossRef]
- Schiller, C.E.; Meltzer-Brody, S.; Rubinow, D.R. The role of reproductive hormones in postpartum depression. CNS Spectrums 2015, 20, 48–59. [Google Scholar] [CrossRef]
- Wu, D.; Jiang, L.; Zhao, G. Additional evidence on prevalence and predictors of postpartum depression in China: A study of 300,000 puerperal women covered by a community-based routine screening programme. J. Affect. Disord. 2022, 307, 264–270. [Google Scholar] [CrossRef]
- Zejnullahu, V.A.; Ukella-Lleshi, D.; Zejnullahu, V.A.; Miftari, E.; Govori, V. Prevalence of postpartum depression at the clinic for obstetrics and gynecology in Kosovo teaching hospital: Demographic, obstetric and psychosocial risk factors. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 256, 215–220. [Google Scholar] [CrossRef]
- Werner, E.; Miller, M.; Osborne, L.M.; Kuzava, S.; Monk, C. Preventing postpartum depression: Review and recommendations. Arch. Women’s Ment. Health 2015, 18, 41–60. [Google Scholar] [CrossRef] [PubMed]
- Sangsawang, B.; Wacharasin, C.; Sangsawang, N. Interventions for the prevention of postpartum depression in adolescent mothers: A systematic review. Arch. Women’s Ment. Health 2019, 22, 215–228. [Google Scholar] [CrossRef] [PubMed]
- Acharya, V. Preparing for motherhood: A role for occupational therapy. World Fed. Occup. Ther. Bull. 2014, 70, 16–17. [Google Scholar] [CrossRef]
- Osorio-Castaño, J.H.; Carvajal-Carrascal, G.; Rodríguez-Gázquez, M. Preparation for motherhood during Pregnancy: A Concept Analysis. Investig. Educ. Enferm. 2017, 35, 295–305. [Google Scholar] [CrossRef]
- Cox, E.Q.; Sowa, N.A.; Meltzer-Brody, S.E.; Gaynes, B.N. The perinatal depression treatment cascade: Baby steps toward improving outcomes. J. Clin. Psychiatry 2016, 77, 20901. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Yang, S.; Xie, M.; Wu, X.; Huang, L.; Ruan, W.; Liu, Y. Impact of some social and clinical factors on the development of postpartum depression in Chinese women. BMC Pregnancy Childbirth 2020, 20, 226. [Google Scholar] [CrossRef]
- Guintivano, J.; Sullivan, P.; Stuebe, A.; Penders, T.; Thorp, J.; Rubinow, D.; Meltzer-Brody, S. Adverse life events, psychiatric history, and biological predictors of postpartum depression in an ethnically diverse sample of postpartum women. Psychol. Med. 2018, 48, 1190–1200. [Google Scholar] [CrossRef]
- Marín-Morales, D.; Toro-Molina, S.; Peñacoba-Puente, C.; Losa-Iglesias, M.; Carmona-Monge, F.J. Relationship between postpartum depression and psychological and biological variables in the initial postpartum period. Matern. Child Health J. 2018, 22, 866–873. [Google Scholar] [CrossRef]
- Ostacoli, L.; Cosma, S.; Bevilacqua, F.; Berchialla, P.; Bovetti, M.; Carosso, A.R.; Malandrone, F.; Carletto, S.; Benedetto, C. Psychosocial factors associated with postpartum psychological distress during the COVID-19 pandemic: A cross-sectional study. BMC Pregnancy Childbirth 2020, 20, 703. [Google Scholar] [CrossRef] [PubMed]
- Qi, W.; Zhao, F.; Liu, Y.; Li, Q.; Hu, J. Psychosocial risk factors for postpartum depression in Chinese women: A meta-analysis. BMC Pregnancy Childbirth 2021, 21, 174. [Google Scholar] [CrossRef] [PubMed]
- Loudon, H.; Nentin, F.; Silverman, M.E. Using clinical decision support as a means of implementing a universal postpartum depression screening program. Arch. Women’s Ment. Health 2016, 19, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef]
- Lin, L.; Chu, H. Quantifying publication bias in meta-analysis. Biometrics 2018, 74, 785–794. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Ahn, E.; Kang, H. Introduction to systematic review and meta-analysis. Korean J. Anesthesiol. 2018, 71, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Tufanaru, C.; Munn, Z.; Stephenson, M.; Aromataris, E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. JBI Evid. Implement. 2015, 13, 196–207. [Google Scholar] [CrossRef]
- Abdollahi, F.; Lye, M.S.; Zarghami, M. Perspective of postpartum depression theories: A narrative literature review. N. Am. J. Med Sci. 2016, 8, 232. [Google Scholar] [PubMed]
- Payne, J.L.; Maguire, J. Pathophysiological mechanisms implicated in postpartum depression. Front. Neuroendocrinol. 2019, 52, 165–180. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, C.A.; Johnson, J.L.; Silva, S.; Bunevicius, R.; Meltzer-Brody, S.; Hamer, R.M.; Leserman, J. Antenatal thyroid correlates of postpartum depression. Psychoneuroendocrinology 2007, 32, 235–245. [Google Scholar] [CrossRef] [PubMed]
- Skalkidou, A.; Hellgren, C.; Comasco, E.; Sylvén, S.; Poromaa, I.S. Biological aspects of postpartum depression. Women’s Health 2012, 8, 659–672. [Google Scholar] [CrossRef]
- Harris, B.; Oretti, R.; Lazarus, J.; Parkes, A.; John, R.; Richards, C.; Newcombe, R.; Hall, R. Randomised trial of thyroxine to prevent postnatal depression in thyroid-antibody-positive women. Br. J. Psychiatry 2002, 180, 327–330. [Google Scholar] [CrossRef]
- Okun, M.L.; Hanusa, B.H.; Hall, M.; Wisner, K.L. Sleep complaints in late pregnancy and the recurrence of postpartum depression. Behav. Sleep Med. 2009, 7, 106–117. [Google Scholar] [CrossRef]
- Okun, M.L.; Luther, J.; Prather, A.A.; Perel, J.M.; Wisniewski, S.; Wisner, K.L. Changes in sleep quality, but not hormones predict time to postpartum depression recurrence. J. Affect. Disord. 2011, 130, 378–384. [Google Scholar] [CrossRef]
- Kendall-Tackett, K. A new paradigm for depression in new mothers: The central role of inflammation and how breastfeeding and anti-inflammatory treatments protect maternal mental health. Int. Breastfeed. J. 2007, 2, 6. [Google Scholar] [CrossRef]
- Kendall-Tackett, K. The new paradigm for depression in new mothers: Current findings on maternal depression, breastfeeding and resiliency across the lifespan. Breastfeed. Rev. 2015, 23, 7–10. [Google Scholar]
- Skalkidou, A.; Sylvén, S.M.; Papadopoulos, F.C.; Olovsson, M.; Larsson, A.; Sundström-Poromaa, I. Risk of postpartum depression in association with serum leptin and interleukin-6 levels at delivery: A nested case–control study within the UPPSAT cohort. Psychoneuroendocrinology 2009, 34, 1329–1337. [Google Scholar] [CrossRef]
- Field, T. Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behav. Dev. 2010, 33, 1–6. [Google Scholar] [CrossRef]
- Managing Complications in Pregnancy and Childbirth. Available online: https://www.who.int/publications/i/item/WHO-MCA-17.02 (accessed on 27 December 2022).
- Tsakiridis, I.; Bousi, V.; Dagklis, T.; Sardeli, C.; Nikolopoulou, V.; Papazisis, G. Epidemiology of antenatal depression among women with high-risk pregnancies due to obstetric complications: A scoping review. Arch. Gynecol. Obstet. 2019, 300, 849–859. [Google Scholar] [CrossRef]
- Bansal, T.; Joon, A. A comparative study to assess preoperative anxiety in obstetric patients undergoing elective or emergency cesarean section. Anaesth. Pain Intensive Care 2019, 21, 25–30. [Google Scholar]
- Orovou, E.; Dagla, M.; Iatrakis, G.; Lykeridou, A.; Tzavara, C.; Antoniou, E. Correlation between kind of cesarean section and posttraumatic stress disorder in Greek women. Int. J. Environ. Res. Public Health 2020, 17, 1592. [Google Scholar] [CrossRef] [PubMed]
- Meky, H.K.; Shaaban, M.M.; Ahmed, M.R.; Mohammed, T.Y. Prevalence of postpartum depression regarding mode of delivery: A cross-sectional study. J. Matern.-Fetal Neonatal Med. 2020, 33, 3300–3307. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Qiu, J.; Meng, L.; Lai, X.; Yao, Z.; Peng, S. Postpartum hemorrhage and postpartum depressive symptoms: A retrospective cohort study. Depress. Anxiety 2022, 39, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Parry-Smith, W.; Okoth, K.; Subramanian, A.; Gokhale, K.M.; Chandan, J.S.; Humpston, C.; Coomarasamy, A.; Nirantharakumar, K.; Šumilo, D. Postpartum haemorrhage and risk of mental ill health: A population-based longitudinal study using linked primary and secondary care databases. J. Psychiatr. Res. 2021, 137, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Asif, S.; Mulic-Lutvica, A.; Axfors, C.; Eckerdal, P.; Iliadis, S.I.; Fransson, E.; Skalkidou, A. Severe obstetric lacerations associated with postpartum depression among women with low resilience–a Swedish birth cohort study. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 1382–1390. [Google Scholar] [CrossRef] [PubMed]
- Hall, W.A.; Hauck, Y.L.; Carty, E.M.; Hutton, E.K.; Fenwick, J.; Stoll, K. Childbirth fear, anxiety, fatigue, and sleep deprivation in pregnant women. J. Obstet. Gynecol. Neonatal Nurs. 2009, 38, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Nilvér, H.; Begley, C.; Berg, M. Measuring women’s childbirth experiences: A systematic review for identification and analysis of validated instruments. BMC Pregnancy Childbirth 2017, 17, 203. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Qu, J.; Wang, A.Y. Anxiety, depression and social support in pregnant women with a history of recurrent miscarriage: A cross-sectional study. J. Reprod. Infant Psychol. 2020, 38, 497–508. [Google Scholar] [CrossRef]
- Laganà, A.S.; La Rosa, V.L.; Rapisarda, A.M.C.; Valenti, G.; Sapia, F.; Chiofalo, B.; Rossetti, D.; Ban Frangež, H.; Vrtačnik Bokal, E.; Vitale, S.G. Anxiety and depression in patients with endometriosis: Impact and management challenges. Int. J. Women’s Health 2017, 9, 323–330. [Google Scholar] [CrossRef]
- Auger, N.; Low, N.; Paradis, G.; Ayoub, A.; Fraser, W.D. Preeclampsia and the longitudinal risk of hospitalization for depression at 28 years. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Bergink, V.; Laursen, T.; Johannsen, B.; Kushner, S.; Meltzer-Brody, S.; Munk-Olsen, T. Pre-eclampsia and first-onset postpartum psychiatric episodes: A Danish population-based cohort study. Psychol. Med. 2015, 45, 3481–3489. [Google Scholar] [CrossRef]
- Byrn, M.; Penckofer, S. The relationship between gestational diabetes and antenatal depression. J. Obstet. Gynecol. Neonatal Nurs. 2015, 44, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Zhang, C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: A global perspective. Curr. Diabetes Rep. 2016, 16, 7. [Google Scholar] [CrossRef] [PubMed]
- Hompoth, E.A.; Peto, Z.; Furészné Balogh, V.; Töreki, A. Associations between depression symptoms, psychological intervention and perinatal complications. J. Clin. Psychol. Med. Settings 2020, 27, 199–205. [Google Scholar] [CrossRef]
- Koutra, K.; Vassilaki, M.; Georgiou, V.; Koutis, A.; Bitsios, P.; Kogevinas, M.; Chatzi, L. Pregnancy, perinatal and postpartum complications as determinants of postpartum depression: The Rhea mother–child cohort in Crete, Greece. Epidemiol. Psychiatr. Sci. 2018, 27, 244–255. [Google Scholar] [CrossRef]
- Meltzer-Brody, S.; Maegbaek, M.; Medland, S.; Miller, W.; Sullivan, P.; Munk-Olsen, T. Obstetrical, pregnancy and socio-economic predictors for new-onset severe postpartum psychiatric disorders in primiparous women. Psychol. Med. 2017, 47, 1427–1441. [Google Scholar] [CrossRef]
- Eckerdal, P.; Kollia, N.; Löfblad, J.; Hellgren, C.; Karlsson, L.; Högberg, U.; Wikström, A.K.; Skalkidou, A. Delineating the association between heavy postpartum haemorrhage and postpartum depression. PLoS ONE 2016, 11, e0144274. [Google Scholar] [CrossRef]
- Zaręba, K.; Banasiewicz, J.; Rozenek, H.; Wójtowicz, S.; Jakiel, G. Peripartum predictors of the risk of postpartum depressive disorder: Results of a case-control study. Int. J. Environ. Res. Public Health 2020, 17, 8726. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, L.; Guo, N.; Jiang, H. Postpartum depression and postpartum post-traumatic stress disorder: Prevalence and associated factors. BMC Psychiatry 2021, 21, 487. [Google Scholar] [CrossRef]
- Wassef, A.; Nguyen, Q.D.; St-André, M. Anaemia and depletion of iron stores as risk factors for postpartum depression: A literature review. J. Psychosom. Obstet. Gynecol. 2019, 40, 19–28. [Google Scholar] [CrossRef]
- Kukulskienė, M.; Žemaitienė, N. Postnatal depression and post-traumatic stress risk following miscarriage. Int. J. Environ. Res. Public Health 2022, 19, 6515. [Google Scholar] [CrossRef] [PubMed]
- Karbanova, J.; Rusavy, Z.; Betincova, L.; Jansova, M.; Necesalova, P.; Kalis, V. Clinical evaluation of early postpartum pain and healing outcomes after mediolateral versus lateral episiotomy. Int. J. Gynecol. Obstet. 2014, 127, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Macarthur, A.J.; Macarthur, C. Incidence, severity, and determinants of perineal pain after vaginal delivery: A prospective cohort study. Am. J. Obstet. Gynecol. 2004, 191, 1199–1204. [Google Scholar] [CrossRef] [PubMed]
- Faisal-Cury, A.; Menezes, P.R. Type of delivery is not associated with maternal depression. Arch. Women’s Ment. Health 2019, 22, 631–635. [Google Scholar] [CrossRef] [PubMed]
- Santamaria, X.; Isaacson, K.; Simón, C. Asherman’s syndrome: It may not be all our fault. Hum. Reprod. 2018, 33, 1374–1380. [Google Scholar] [CrossRef]
- Bahat, P.Y.; Turan, G.; Selçuki, N.F.T.; Çakmak, K.; Kaya, C. Comparison of Depression and Anxiety Scores in Multi/Nulliparous Women who have Undergone Dilatation and Curettage. Acta Bio Med. Atenei Parm. 2022, 93, e2022038. [Google Scholar]
- JayaSalengia, B.; Rajeswari, S.; Nalini, S. The relationship between maternal confidence, infant temperament, and postpartum depression. Iran. J. Nurs. Midwifery Res. 2019, 24, 437. [Google Scholar]
- Grippi, C. Factors That Influence Women’s Symptoms of Postpartum Depression After Discharge of Their Preterm Infants From the NICU. J. Obstet. Gynecol. Neonatal Nurs. 2021, 50, 610–620. [Google Scholar] [CrossRef] [PubMed]
- Wyatt, T.; Shreffler, K.M.; Ciciolla, L. Neonatal intensive care unit admission and maternal postpartum depression. J. Reprod. Infant Psychol. 2019, 37, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Garfield, C.F.; Lee, Y.S.; Warner-Shifflett, L.; Christie, R.; Jackson, K.L.; Miller, E. Maternal and paternal depression symptoms during NICU stay and transition home. Pediatrics 2021, 148, e2020042747. [Google Scholar] [CrossRef] [PubMed]
- Tsai, J.M.; Tsai, L.Y.; Tsay, S.L.; Chen, Y.H. The prevalence and risk factors of postpartum depression among women during the early postpartum period: A retrospective secondary data analysis. Taiwan. J. Obstet. Gynecol. 2023, 62, 406–411. [Google Scholar] [CrossRef] [PubMed]
- Ölmestig, T.K.; Siersma, V.; Birkmose, A.R.; Kragstrup, J.; Ertmann, R.K. Infant crying problems related to maternal depressive and anxiety symptoms during pregnancy: A prospective cohort study. BMC Pregnancy Childbirth 2021, 21, 777. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.J.; Broidy, L.; Baird, K.; Rahman, M.; Zobair, K.M. Early exclusive breastfeeding cessation and postpartum depression: Assessing the mediating and moderating role of maternal stress and social support. PLoS ONE 2021, 16, e0251419. [Google Scholar] [CrossRef] [PubMed]
- Katon, W.; Russo, J.; Gavin, A. Predictors of postpartum depression. J. Women’s Health 2014, 23, 753–759. [Google Scholar] [CrossRef]
- Brown, H.K.; Qazilbash, A.; Rahim, N.; Dennis, C.L.; Vigod, S.N. Chronic medical conditions and peripartum mental illness: A systematic review and meta-analysis. Am. J. Epidemiol. 2018, 187, 2060–2068. [Google Scholar] [CrossRef]
- Surita, F.G.d.C.; Parpinelli, M.Â.; Yonehara, E.; Krupa, F.; Cecatti, J.G. Systemic lupus erythematosus and pregnancy: Clinical evolution, maternal and perinatal outcomes and placental findings. Sao Paulo Med. J. 2007, 125, 91–95. [Google Scholar] [CrossRef]
- Aker, A.M.; Vigod, S.N.; Dennis, C.L.; Brown, H.K. Perinatal complications as a mediator of the association between chronic disease and postpartum mental illness. J. Women’s Health 2022, 31, 564–572. [Google Scholar] [CrossRef]
- Silverman, M.E.; Reichenberg, A.; Savitz, D.A.; Cnattingius, S.; Lichtenstein, P.; Hultman, C.M.; Larsson, H.; Sandin, S. The risk factors for postpartum depression: A population-based study. Depress. Anxiety 2017, 34, 178–187. [Google Scholar] [CrossRef]
- Onyemaechi, C.I.; Afolabi, A.B.; Mike Ifeagwazi, C. Postpartum depression: The role of self-esteem, social support and age. IFE Psychol. Int. J. 2017, 25, 105–115. [Google Scholar]
- Ghosh, A.; Goswami, S. Evaluation of post partum depression in a tertiary hospital. J. Obstet. Gynecol. India 2011, 61, 528–530. [Google Scholar] [CrossRef]
- Guintivano, J.; Manuck, T.; Meltzer-Brody, S. Predictors of postpartum depression: A comprehensive review of the last decade of evidence. Clin. Obstet. Gynecol. 2018, 61, 591–603. [Google Scholar] [CrossRef]
- Shour, A.R.; Muehlbauer, A.; Anguzu, R.; Weeks, F.; Meurer, J. Examining the association between racial bias exposure and postpartum depression among women in Wisconsin. Wis. Med. J. 2021, 120, S24–S30. [Google Scholar]
- Hahn-Holbrook, J.; Cornwell-Hinrichs, T.; Anaya, I. Economic and health predictors of national postpartum depression prevalence: A systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Front. Psychiatry 2018, 8, 248. [Google Scholar] [CrossRef] [PubMed]
- Di Florio, A.; Meltzer-Brody, S. Is postpartum depression a distinct disorder? Curr. Psychiatry Rep. 2015, 17, 76. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef]
| No. | Search String | Number of Articles |
|---|---|---|
| 1 | “postpartum period”[MeSH Terms]
OR “postpartum”[Title/Abstract] OR “puerperium”[Title/Abstract] OR “pregnancy”[MeSH Terms] OR “pregnancy”[Title/Abstract] | 1,136,113 |
| 2 |
“depression, postpartum”[MeSH Terms]
OR “depressive disorder”[MeSH Terms] OR “depression”[MeSH Terms] OR “depressive disorder”[MeSH Terms] OR “mood disorders”[MeSH Terms] OR “suicide”[MeSH Terms] OR “postpartum depression”[Title/Abstract] OR “mood disorder”[Title/Abstract] OR “baby blues”[Title/Abstract] | 361,517 |
| 3 |
((((((((((((((((((((((risk factors[MeSH Terms])
(Obstetric Labor Complications[MeSH Terms])) OR (fetal disease[MeSH Terms])) OR (pregnancy complications[MeSH Terms])) OR (complication*[Title/Abstract])) OR (intrapartum complication*[Title/Abstract])) OR (birt complication*[Title/Abstract])) OR (maternal complication*[Title/Abstract])) OR (shoulder dystocia[Title/Abstract])) OR (hemorrhage[Title/Abstract])) OR (hemorrhage[Title/Abstract])) OR (asphyxia[Title/Abstract])) OR (baby complication[Title/Abstract])) OR (vaginal birth[Title/Abstract])) OR (vaginal delivery[Title/Abstract])) OR (caesarean section[Title/Abstract])) OR (vacuum extractor[Title/Abstract])) OR (forceps delivery[Title/Abstract])) OR (vaginal tears[Title/Abstract])) OR (vaginal laceration[Title/Abstract])) OR (episiotomy[Title/Abstract])) OR (uterine curettage[Title/Abstract]) | 2,579,080 |
| 4 | “Forecasting”[MeSH Terms:noexp] OR “predict*”[Title/Abstract] OR “determinants”[Title/Abstract] | 2,264,321 |
| 5 | String #1 AND String #2 AND String #3 AND String #4 | 2156 |
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| For Literature | For Participants | |
| 1. Cross-sectional or longitudinal
design original studies. 2. English, Arabic, or Polish peer-reviewed articles. 3. Articles reporting risk factors for PPD. 4. Studies focusing on changes in postpartum mood, suicidal ideation, and suicides following the last birth. 5. Study subjects who had psychiatric consultation or referral due to symptoms of depression. | 1. Grey literature. 2. Case studies, reviews, meta-analyses, and letters to the editor case studies. 3. Research describing mental problems, neurocognitive diseases, and mood disorders that were present before birth. 4. Studies that did not report sensitivity and specificity. 5. Studies reporting the relationship between PPD and COVID-19-associated factors. | Pregnant women with the following
diseases and conditions diagnosed
before the last birth: 1. Mental and psychological disorders (F00–F99 in ICD-10). 2. Cerebrovascular diseases (I60–I69). 3. Organic pathologies of the central nervous system (e.g., brain and meninges tumours—C71, D32–33). 4. Serious abnormalities or diseases known before the last birth that are known risk factors for PPD (O35.9 in ICD10). 5. Partner or other type of violence. |
| Group | Subgroup | Variables |
|---|---|---|
| Obstetric determinants | Birth-management-related risks | Type of delivery: |
| - Spontaneous vaginal delivery | ||
| - Assisted vaginal delivery (forceps or vacuum extraction) | ||
| - Planned (elective) caesarean section | ||
| - Emergency caesarean section | ||
| Type of anaesthesia: | ||
| - Epidural | ||
| - Spinal | ||
| - Local (pudendal block) | ||
| - General | ||
| Fetal lie/presentation/position: | ||
| - Shoulder dystocia | ||
| Peripartum emergencies: | ||
| - Amniotic fluid embolism | ||
| - Intrapartum/postpartum hemorrhage | ||
| - Pulmonary embolism | ||
| - Placenta abruption | ||
| - Uterine rupture | ||
| - Fetal bradycardia | ||
| - Severe perineal tears (III and IV degree) | ||
| - Severe vaginal lacerations | ||
| - Prolonged I, II, or III stage of labour | ||
| Assistance in labour: | ||
| - Induction of labour | ||
| - Episiotomy | ||
| - Amniotomy | ||
| Drugs in delivery: | ||
| - Oxytocic hormones | ||
| - Prostaglandin E1 analogues | ||
| Maternal risks | Complications: | |
| - Postpartum anemia | ||
| - Postpartum endometritis | ||
| - Urinary incontinence | ||
| Others: | ||
| - Length of stay in hospital after delivery | ||
| - Time since giving birth | ||
| Neonate risks | APGAR score | |
| Hypoxia | ||
| Abnormalities found after delivery | ||
| Confounders | Demographic risks | Age group |
| Country of study | ||
| Race/ethnicity | ||
| Socioeconomic risks | Socioeconomic status (low, medium, high) | |
| Level of education | ||
| Income | ||
| Marital status | ||
| Employment status |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhaj Ahmad, M.; Al Awar, S.; Sayed Sallam, G.; Alkaabi, M.; Smetanina, D.; Statsenko, Y.; Zaręba, K. Biopsychosocial Predictors of Postpartum Depression: Protocol for Systematic Review and Meta-Analysis. Healthcare 2024, 12, 650. https://doi.org/10.3390/healthcare12060650
Alhaj Ahmad M, Al Awar S, Sayed Sallam G, Alkaabi M, Smetanina D, Statsenko Y, Zaręba K. Biopsychosocial Predictors of Postpartum Depression: Protocol for Systematic Review and Meta-Analysis. Healthcare. 2024; 12(6):650. https://doi.org/10.3390/healthcare12060650
Chicago/Turabian StyleAlhaj Ahmad, Marwa, Shamsa Al Awar, Gehan Sayed Sallam, Meera Alkaabi, Darya Smetanina, Yauhen Statsenko, and Kornelia Zaręba. 2024. "Biopsychosocial Predictors of Postpartum Depression: Protocol for Systematic Review and Meta-Analysis" Healthcare 12, no. 6: 650. https://doi.org/10.3390/healthcare12060650
APA StyleAlhaj Ahmad, M., Al Awar, S., Sayed Sallam, G., Alkaabi, M., Smetanina, D., Statsenko, Y., & Zaręba, K. (2024). Biopsychosocial Predictors of Postpartum Depression: Protocol for Systematic Review and Meta-Analysis. Healthcare, 12(6), 650. https://doi.org/10.3390/healthcare12060650







