The Interrelationship of Benefit Finding, Demoralization, and Stigma among Patients with Parkinson’s Disease and Their Caregivers
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Assessments
2.2.1. Benefit Finding Scale (BFS)
2.2.2. Demoralization Scale (DS)
2.2.3. Stigma Subscale of Explanatory Model Interview Catalogue (EMIC)
2.2.4. Unified Parkinson’s Disease Rating Scale (UPDRS) (Scores Range from 0 to 144)
2.2.5. Numeric Pain Rating Scale (NPRS)
2.2.6. Taiwanese Depression Questionnaire (TDQ)
2.2.7. Mini International Neuropsychiatric Interview (MINI)
2.3. Procedures
2.4. Statistical Analyses
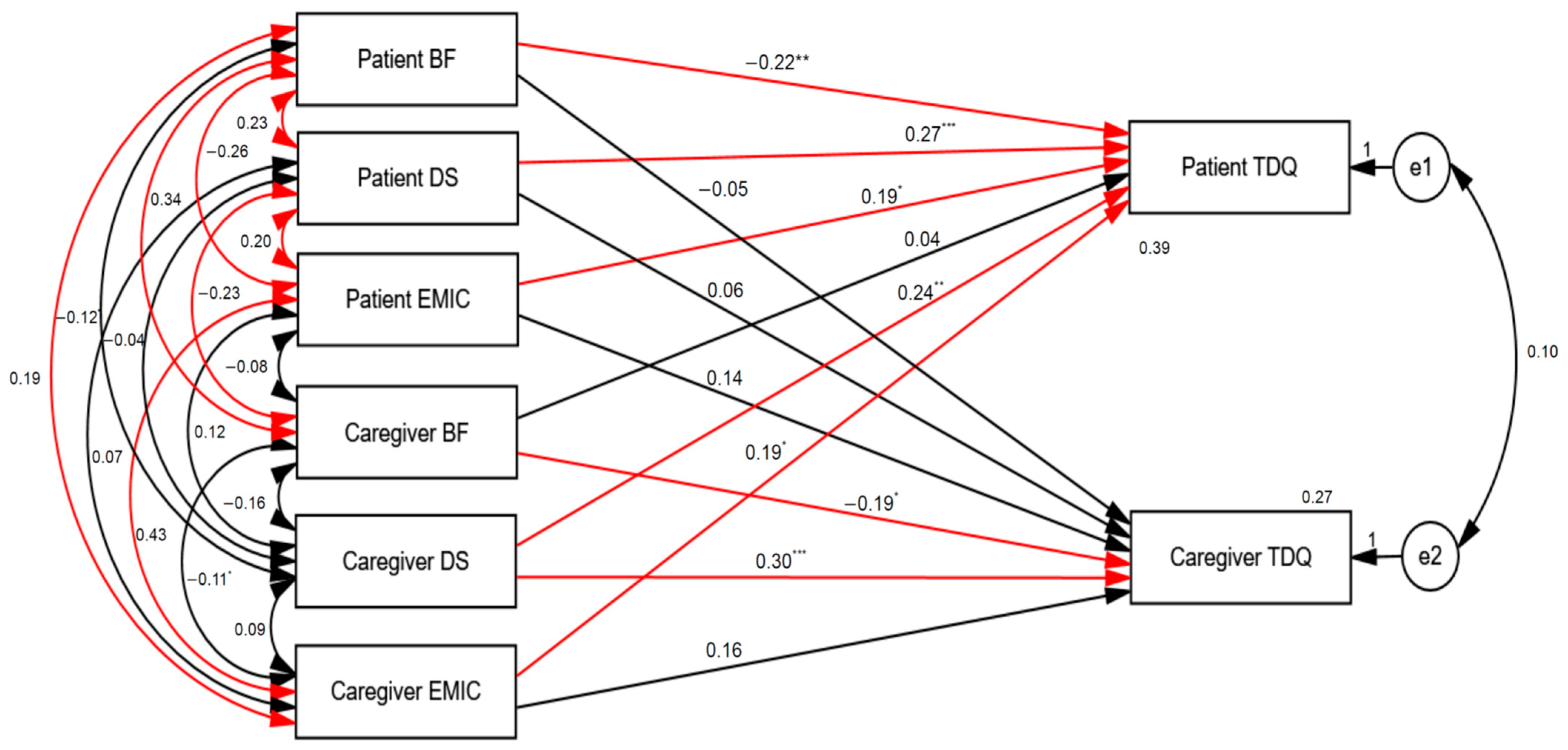
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Riccò, M.; Vezzosi, L.; Balzarini, F.; Gualerzi, G.; Ranzieri, S.; Signorelli, C.; Colucci, M.E.; Bragazzi, N.L. Prevalence of parkinson disease in italy: A systematic review and meta-analysis. Acta Bio Med. Atenei Parm. 2020, 91, e2020088. [Google Scholar] [CrossRef] [PubMed]
- Pringsheim, T.; Jette, N.; Frolkis, A.; Steeves, T.D. The prevalence of parkinson’s disease: A systematic review and meta-analysis. Mov. Disord. 2014, 29, 1583–1590. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.-C.; Li, C.-Y.; Lee, P.-C.; Sun, Y. Variations in incidence and prevalence of parkinson’s disease in taiwan: A population-based nationwide study. Park. Dis. 2016, 2016, 8756359. [Google Scholar] [CrossRef] [PubMed]
- Marinus, J.; Zhu, K.; Marras, C.; Aarsland, D.; van Hilten, J.J. Risk factors for non-motor symptoms in Parkinson’s disease. Lancet Neurol. 2018, 17, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Cong, S.; Xiang, C.; Zhang, S.; Zhang, T.; Wang, H.; Cong, S. Prevalence and clinical aspects of depression in parkinson’s disease: A systematic review and meta-analysis of 129 studies. Neurosci. Biobehav. Rev. 2022, 141, 104749. [Google Scholar] [CrossRef] [PubMed]
- Dorsey, E.R.; Elbaz, A.; Nichols, E.; Abbasi, N.; Abd-Allah, F.; Abdelalim, A.; Adsuar, J.C.; Ansha, M.G.; Brayne, C.; Choi, J.-Y.J.; et al. Global, regional, and national burden of parkinson’s disease, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2018, 17, 939–953. [Google Scholar] [CrossRef] [PubMed]
- Ransmayr, G. Belastungen in der Betreuung von Parkinson-Patientinnen und -Patienten. Fortschr. Neurol. Psychiatr. 2020, 88, 567–572. [Google Scholar] [CrossRef] [PubMed]
- D’amelio, M.; Terruso, V.; Palmeri, B.; Di Benedetto, N.; Famoso, G.; Cottone, P.; Aridon, P.; Ragonese, P.; Savettieri, G. Predictors of caregiver burden in partners of patients with parkinson’s disease. Neurol. Sci. 2009, 30, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Carod-Artal, F.J.; Mesquita, H.M.; Ziomkowski, S.; Martinez-Martin, P. Burden and health-related quality of life among caregivers of brazilian parkinson’s disease patients. Park. Relat. Disord. 2013, 19, 943–948. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Chiou, Y.-J.; Hung, C.-F.; Chang, Y.-Y.; Chen, Y.-F.; Lin, T.-K.; Wang, L.-J. Prevalence and associated factors of depressive disorder in caregivers of individuals with parkinson disease. J. Geriatr. Psychiatry Neurol. 2021, 34, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Tennen, H.; Affleck, G. Benefit-finding and benefit-reminding. In Handbook of Positive Psychology; Oxford University Press: New York, NY, USA, 2002; pp. 584–597. [Google Scholar]
- Wen, X.; Liang, Y.; Ni, J.; Han, X.; Gu, D. Impact of caregiver burden on caregiver mental health in patients with esophageal cancer: Chain mediating effects of benefit finding and rumination, a cross-sectional study. J. Gastrointest. Oncol. 2022, 13, 2132–2143. [Google Scholar] [CrossRef] [PubMed]
- Mavandadi, S.; Dobkin, R.; Mamikonyan, E.; Sayers, S.; Have, T.T.; Weintraub, D. Benefit finding and relationship quality in parkinson’s disease: A pilot dyadic analysis of husbands and wives. J. Fam. Psychol. 2014, 28, 728–734. [Google Scholar] [CrossRef] [PubMed]
- Kissane, D.W.; Clarke, D.M.; Street, A.F. Demoralization syndrome—A relevant psychiatric diagnosis for palliative care. J. Palliat. Care 2001, 17, 12–21. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, J.M.; Zhu, B.; Patel, A.; Kohn, R.; Koo, B.B.; Louis, E.D. From perceived stress to demoralization in parkinson disease: A path analysis. Front. Psychiatry 2022, 13, 876445. [Google Scholar] [CrossRef] [PubMed]
- Bovero, A.; Vitiello, L.P.; Botto, R.; Gottardo, F.; Cito, A.; Geminiani, G.C. Demoralization in End-of-life cancer patients’ family caregivers: A cross-sectional study. Am. J. Hosp. Palliat. Med. 2022, 39, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.-J.; Quan, M.-M.; Gao, L.; Li, Q.; Yan, C.-X.; Zhang, Q.; Shi, B.-X. Demoralization and depression in chinese cancer patients. Support. Care Cancer 2021, 29, 6211–6216. [Google Scholar] [CrossRef] [PubMed]
- Dudley, J.R. Confronting stigma within the services system. Soc. Work 2000, 45, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.S.; Neargarder, S.; Kinger, S.B.; Fox-Fuller, J.T.; Salazar, R.D.; Cronin-Golomb, A. Perceived stigma and quality of life in parkinson’s disease with additional health conditions. Gen. Psychiatry 2022, 35, e100653. [Google Scholar] [CrossRef] [PubMed]
- Henry, R.S.; Perrin, P.B.; Lageman, S.K.; Villaseñor, T.; Cariello, A.N.; Pugh, M.; Smith, E.R.; Arroyo, M.; Zarate, A.; Avila, J.; et al. Parkinson’s symptoms and caregiver affiliate stigma: A multinational study. Curr. Alzheimer Res. 2021, 18, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Tomich, P.L.; Helgeson, V.S. Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychol. 2004, 23, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Navarta-Sánchez, M.V.; Senosiain García, J.M.; Riverol, M.; Ursúa Sesma, M.E.; Díaz de Cerio Ayesa, S.; Anaut Bravo, S.; Caparrós Civera, N.; Portillo, M.C. Factors influencing psychosocial adjustment and quality of life in Parkinson patients and informal caregivers. Qual. Life Res. 2016, 25, 1959–1968. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Gudenkauf, L.; Zhang, L.; Wang, Z. Application and evaluation of benefit finding scale (bfs) in early-stage cancer patients from China. Eur. J. Oncol. Nurs. 2016, 23, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Kissane, D.W.; Wein, S.; Love, A.; Lee, X.Q.; Kee, P.L.; Clarke, D.M. The demoralization scale: A report of its development and preliminary validation. J. Palliat. Care 2004, 20, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Hung, H.C.; Chen, H.W.; Chang, Y.F.; Yang, Y.C.; Liu, C.L.; Hsieh, R.K.; Leu, Y.S.; Chen, Y.J.; Wang, T.-E.; Tsai, L.Y.; et al. Evaluation of the reliability and validity of the mandarin version of demoralization scale for cancer patients. J. Intern. Med. Taiwan 2010, 21, 427–435. [Google Scholar]
- Weiss, M.G.; Doongaji, D.R.; Siddhartha, S.; Wypij, D.; Pathare, S.; Bhatawdekar, M.; Bhave, A.; Sheth, A.; Fernandes, R. The explanatory model interview catalogue (emic). Br. J. Psychiatry 1992, 160, 819–830. [Google Scholar] [CrossRef] [PubMed]
- Ackumey, M.M.; Gyapong, M.; Weiss, M.G.; Pappoe, M. Help-seeking for pre-ulcer and ulcer conditions of mycobacterium ulcerans disease (buruli ulcer) in ghana. Am. J. Trop. Med. Hyg. 2011, 85, 1106–1113. [Google Scholar] [CrossRef] [PubMed]
- Van Brakel, W.H.; Cataldo, J.; Grover, S.; Kohrt, B.A.; Nyblade, L.; Stockton, M.; Wouters, E.; Yang, L.H. Out of the silos: Identifying cross-cutting features of health-related stigma to advance measurement and intervention. BMC Med. 2019, 17, 13. [Google Scholar] [CrossRef] [PubMed]
- Tseng, W.-T.; Lee, Y.; Hung, C.-F.; Lin, P.-Y.; Chien, C.-Y.; Chuang, H.-C.; Fang, F.-M.; Li, S.-H.; Huang, T.-L.; Chong, M.-Y.; et al. Validation of the chinese version of the shame and stigma scale in patients with head and neck cancer. Cancer Manag. Res. 2019, 11, 10297–10305. [Google Scholar] [CrossRef] [PubMed]
- Ramaker, C.; Marinus, J.; Stiggelbout, A.M.; van Hilten, B.J. Systematic evaluation of rating scales for impairment and disability in parkinson’s disease. Mov. Disord. 2002, 17, 867–876. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Martín, P.; Gil-Nagel, A.; Gracia, L.M.; Gómez, J.B.; Martínez-Sarriés, J.; Bermejo, F.; The Cooperative Multicentric Group. Unified parkinson’s disease rating scale characteristics and structure. Mov. Disord. 1994, 9, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P. The validity and reliability of pain measures in adults with cancer. J. Pain 2003, 4, 2–21. [Google Scholar] [CrossRef] [PubMed]
- Paice, J.A.; Cohen, F.L. Validity of a verbally administered numeric rating scale to measure cancer pain intensity. Cancer Nurs. 1997, 20, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Yang, M.J.; Lai, T.J.; Chiu, N.M.; Chau, T.T. Development of the taiwanese depression questionnaire. Chang. Gung Med. J. 2000, 23, 688–694. [Google Scholar] [PubMed]
- Lee, Y.; Wu, Y.-S.; Chien, C.-Y.; Fang, F.-M.; Hung, C.-F. Use of the hospital anxiety and depression scale and the Taiwanese Depression Questionnaire for screening depression in head and neck cancer patients in taiwan. Neuropsychiatr. Dis. Treat. 2016, 12, 2649–2657. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Balker, R.; Dunbar, G.C. The mini-international neuropsychiatric interview (m.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for dsm-iv and icd-10. J. Clin. Psychiatry 1998, 59 (Suppl. S20), 22–33; quiz 34–57. [Google Scholar]
- Sheehan, D.; Lecrubier, Y.; Sheehan, K.H.; Janavs, J.; Weiller, E.; Keskiner, A.; Schinka, J.; Knapp, E.; Sheehan, M.; Dunbar, G. The validity of the mini international neuropsychiatric interview (mini) according to the scid-p and its reliability. Eur. Psychiatry 1997, 12, 232–241. [Google Scholar] [CrossRef]
- Chung, M.L.; Moser, D.K.; Lennie, T.A.; Rayens, M.K. The effects of depressive symptoms and anxiety on quality of life in patients with heart failure and their spouses: Testing dyadic dynamics using actor–partner interdependence model. J. Psychosom. Res. 2009, 67, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Cook, W.L.; Kenny, D.A. The actor–partner interdependence model: A model of bidirectional effects in developmental studies. Int. J. Behav. Dev. 2005, 29, 101–109. [Google Scholar] [CrossRef]
- Jozwiak, N.; Postuma, R.B.; Montplaisir, J.; Latreille, V.; Panisset, M.; Chouinard, S.; Bourgouin, P.-A.; Gagnon, J.-F. REM sleep behavior disorder and cognitive impairment in parkinson’s disease. Sleep 2017, 40, zsx101. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.E.; Jeon, B.S. Clinical implication of rem sleep behavior disorder in parkinson’s disease. J. Park. Dis. 2014, 4, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xu, C.-Y.; Liu, J. Meta-analysis on the prevalence of rem sleep behavior disorder symptoms in parkinson’s disease. BMC Neurol. 2017, 17, 23. [Google Scholar] [CrossRef] [PubMed]
- Goodarzi, Z.; Mrklas, K.J.; Roberts, D.J.; Jette, N.; Pringsheim, T.; Holroyd-Leduc, J. Detecting depression in parkinson disease. Neurology 2016, 87, 426–437. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-S.; Yu, S.-H.; Lee, C.-Y.; Tseng, H.-Y.; Chiu, Y.-F.; Hsiung, C.A. Prevalence of and risk factors for minor and major depression among community-dwelling older adults in taiwan. Int. Psychogeriatr. 2017, 29, 1113–1121. [Google Scholar] [CrossRef] [PubMed]
- Chiu, E. Epidemiology of depression in the asia pacific region. Australas. Psychiatry 2004, 12, S4–S10. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Chiou, Y.-J.; Hung, C.-F.; Chang, Y.-Y.; Chen, Y.-F.; Lin, T.-K.; Wang, L.-J. A dyadic study of psychological well-being of individuals with parkinson’s disease and their caregivers. Sci. Rep. 2021, 11, 957. [Google Scholar] [CrossRef] [PubMed]
- Starr, L.T.; Bullock, K.; Washington, K.; Aryal, S.; Oliver, D.P.; Demiris, G. Anxiety, depression, quality of life, caregiver burden, and perceptions of caregiver-centered communication among black and white hospice family caregivers. J. Palliat. Med. 2022, 25, 596–605. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, T. Benefit finding through caring: The cancer caregiver experience. Psychol. Health 2013, 28, 250–266. [Google Scholar] [CrossRef] [PubMed]
- Chai, Y.C.; Mahadevan, R.; Ng, C.G.; Chan, L.F.; Dai, F.M. Caregiver depression: The contributing role of depression in patients, stigma, social support and religiosity. Int. J. Soc. Psychiatry 2018, 64, 578–588. [Google Scholar] [CrossRef] [PubMed]
- Livingston, J.D.; Boyd, J.E. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Soc. Sci. Med. 2010, 71, 2150–2161. [Google Scholar] [CrossRef]
- Watson, A.C.; Corrigan, P.; Larson, J.E.; Sells, M. Self-stigma in people with mental illness. Schizophr. Bull. 2007, 33, 1312–1318. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P.W.; Watson, A.C. Understanding the impact of stigma on people with mental illness. World Psychiatry 2002, 1, 16–20. [Google Scholar] [PubMed]
- Lin, Y.; Luo, X.; Li, J.; Xu, Y.; Li, Q. The dyadic relationship of benefit finding and its impact on quality of life in colorectal cancer survivor and spousal caregiver couples. Support. Care Cancer 2021, 29, 1477–1486. [Google Scholar] [CrossRef] [PubMed]
- Karlstedt, M.; Fereshtehnejad, S.-M.; Aarsland, D.; Lökk, J. Determinants of dyadic relationship and its psychosocial impact in patients with parkinson’s disease and their spouses. Park. Dis. 2017, 2017, 4697052. [Google Scholar] [CrossRef] [PubMed]
| Patients N (%), N = 120 | Caregivers N (%), N = 120 | Total N (%), N = 240 | Pair t/χ2 | p | |
|---|---|---|---|---|---|
| Gender | 8.07 | 0.005 | |||
| Male | 70 (58.3) | 48 (40.0) | 118 (49.2) | ||
| Female | 50 (41.7) | 72 (60.0) | 122 (50.8) | ||
| Age, years mean | 66.76 ± 8.48 | 60.81 ± 12.73 | 63.78 ± 11.20 | 5.35 | <0.001 |
| Age of onset | 58.29 ± 11.02 | ||||
| Duration of PD (years) | 8.43 ± 7.24 | ||||
| Duration of caring (years) | 8.40 ± 7.11 | ||||
| Years of education | 11.27 ± 4.47 | 12.32 ± 4.14 | 11.79 ± 4.33 | −2.25 | 0.026 |
| Education | 3.44 | 0.064 | |||
| Less than 12 years | 41 (34.2) | 28 (23.3) | 69 (28.7) | ||
| More than or equal to 12 years | 79 (65.8) | 92 (76.7) | 171 (71.3) | ||
| Marital Status | 0 | 1.00 | |||
| Unmarried | 14 (11.7) | 14 (11.7) | 28 (11.7) | ||
| Married | 106 (88.3) | 106 (88.3) | 212 (88.3) | ||
| Unemployed | 96 (80.0) | 75 (62.5) | 171 (71.3) | 8.97 | 0.003 |
| Comorbid with other diseases | 67 (55.8) | 60 (50.0) | 127 (52.9) | 0.82 | 0.37 |
| Suicide history | 2 (1.7) | 2 (1.7) | 4 (1.7) | 0 | 1.00 |
| Anxiolytics/Hypnotics use | 23 (19.2) | 43 (35.8) | 66 (27.5) | 8.36 | 0.004 |
| Family psychiatric history | 0.34 | 0.56 | |||
| No psychiatric history | 118 (98.3) | 119 (99.2) | 237 (98.8) | ||
| Depressive disorder | 2 (1.7) | 1 (0.8) | 3 (1.3) | ||
| Family suicide history | 0 | 2 (1.7) | 2 (0.8) | 2.02 | 0.16 |
| NPRS | 3.44 (0–10) | 2.49 (0–10) | 2.97 (0–10) | 3.02 | 0.003 |
| UPDRS total scores | 36.78 ± 16.91 | ||||
| H&Y staging | 2.23 ± 0.65 | ||||
| TDQ | 7.80 (0–35) | 4.86 (0–24) | 6.33 (0–35) | 4.63 | <0.001 |
| BFS total scores | 70.17 ± 13.87 | 73.03 ± 13.52 | 71.60 ± 13.74 | −2.00 | 0.048 |
| Acceptance | 10.72 ± 2.31 | 10.96 ± 2.54 | 10.84 ± 2.42 | −0.87 | 0.39 |
| Family Relations | 7.57 ± 1.89 | 7.40 ± 1.72 | 7.48 ± 1.81 | 0.85 | 0.40 |
| World View | 10.60 ± 3.36 | 11.60 ± 3.37 | 11.10 ± 3.40 | −2.58 | 0.011 |
| Personal Growth | 21.90 ± 5.85 | 23.83 ± 5.51 | 22.86 ± 5.75 | −2.84 | 0.005 |
| Social Relations | 8.90 ± 3.86 | 8.66 ± 3.47 | 8.78 ± 3.66 | 0.63 | 0.53 |
| Health Behavior | 10.48 ± 2.64 | 10.58 ± 3.01 | 10.53 ± 2.82 | −0.29 | 0.78 |
| DS total scores | 26.83 ± 9.74 | 25.44 ± 10.52 | 26.13 ± 10.14 | 1.04 | 0.30 |
| Loss of meaning | 4.93 ± 1.98 | 4.68 ± 2.51 | 4.80 ± 2.26 | 0.78 | 0.44 |
| Dysphoria | 5.69 ± 2.56 | 5.49 ± 2.78 | 5.59 ± 2.67 | 0.62 | 0.54 |
| Disheartenment | 5.35 ± 2.49 | 5.48 ± 2.95 | 5.41 ± 2.72 | −0.35 | 0.73 |
| Helplessness | 4.62 ± 2.58 | 4.06 ± 2.04 | 4.34 ± 2.34 | 1.92 | 0.06 |
| Sense of failure | 4.98 ± 1.79 | 4.60 ± 2.16 | 4.79 ± 1.99 | 1.54 | 0.13 |
| EMIC total scores | 3.60 (0–27) | 2.49 (0–17) | 3.05 (0–27) | 2.11 | 0.037 |
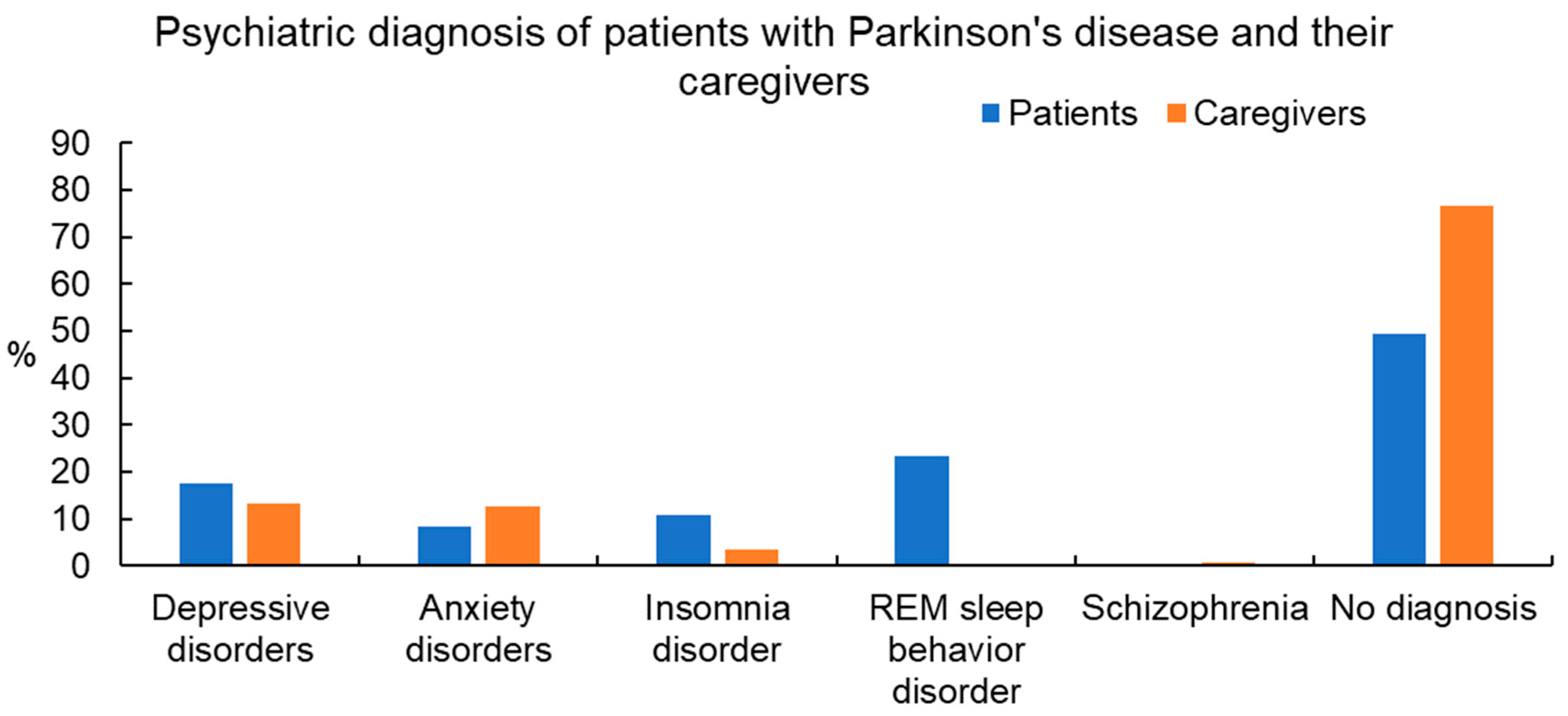
| MINI Diagnosis | Patients, N = 120 | Caregivers, N = 120 |
|---|---|---|
| Depressive disorders | 21 (17.5) | 16 (13.3) |
| Major depressive disorder | 5 (4.2) | 3 (2.5) |
| Other specified depressive disorder | 14 (11.7) | 13 (10.8) |
| Persistent depressive disorder | 2 (1.7) | 0 |
| Anxiety disorders | 10 (8.3) | 15 (12.5) |
| Other specified anxiety disorder | 6 (5.0) | 11 (9.2) |
| Generalized anxiety disorder | 3 (2.5) | 3 (2.5) |
| Panic disorder | 1 (0.8) | 1 (0.8) |
| Insomnia disorder | 13 (10.8) | 4 (3.3) |
| REM sleep behavior disorder | 28 (23.3) | 0 |
| Schizophrenia | 0 | 1 (0.8) |
| No diagnosis | 59 (49.2) | 92 (76.7) |
| Item | β | S.E. | Wald | Odds Ratio | 95% C.I. | p |
|---|---|---|---|---|---|---|
| Anxiolytics/Hypnotics use | 1.19 | 0.54 | 4.81 | 3.28 | 1.13–9.48 | 0.028 |
| EMIC | 0.13 | 0.04 | 11.77 | 1.14 | 1.06–1.23 | 0.001 |
| Item | β | S.E. | Wald | Odds Ratio | 95% C.I. | p |
|---|---|---|---|---|---|---|
| EMIC | 0.15 | 0.05 | 7.67 | 1.16 | 1.05–1.29 | 0.006 |
| BFS | −0.05 | 0.02 | 4.25 | 0.96 | 0.92–1.00 | 0.039 |
| DS | 0.06 | 0.03 | 5.29 | 1.07 | 1.01–1.13 | 0.021 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chou, P.-C.; Lee, Y.; Chang, Y.-Y.; Hung, C.-F.; Chen, Y.-F.; Lin, T.-K.; Shih, F.-Y.; Chen, W.-F.; Lin, P.-Y.; Chong, M.-Y.; et al. The Interrelationship of Benefit Finding, Demoralization, and Stigma among Patients with Parkinson’s Disease and Their Caregivers. Healthcare 2024, 12, 878. https://doi.org/10.3390/healthcare12090878
Chou P-C, Lee Y, Chang Y-Y, Hung C-F, Chen Y-F, Lin T-K, Shih F-Y, Chen W-F, Lin P-Y, Chong M-Y, et al. The Interrelationship of Benefit Finding, Demoralization, and Stigma among Patients with Parkinson’s Disease and Their Caregivers. Healthcare. 2024; 12(9):878. https://doi.org/10.3390/healthcare12090878
Chicago/Turabian StyleChou, Pei-Chien, Yu Lee, Yung-Yee Chang, Chi-Fa Hung, Ying-Fa Chen, Tsu-Kung Lin, Fu-Yuan Shih, Wu-Fu Chen, Pao-Yen Lin, Mian-Yoon Chong, and et al. 2024. "The Interrelationship of Benefit Finding, Demoralization, and Stigma among Patients with Parkinson’s Disease and Their Caregivers" Healthcare 12, no. 9: 878. https://doi.org/10.3390/healthcare12090878
APA StyleChou, P.-C., Lee, Y., Chang, Y.-Y., Hung, C.-F., Chen, Y.-F., Lin, T.-K., Shih, F.-Y., Chen, W.-F., Lin, P.-Y., Chong, M.-Y., & Wang, L.-J. (2024). The Interrelationship of Benefit Finding, Demoralization, and Stigma among Patients with Parkinson’s Disease and Their Caregivers. Healthcare, 12(9), 878. https://doi.org/10.3390/healthcare12090878


_MD__MPH_PhD.png)




