Emerging Evidence on Balneotherapy and Thermal Interventions in Post-COVID-19 Syndrome: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Data Extraction and Synthesis
2.5. Risk of Bias Assessment
3. Results
3.1. Effects on Primary Outcomes
3.2. Treatment Response Patterns
3.3. Treatment Adherence and Patient Satisfaction
3.4. Safety and Tolerability
3.5. Results of Risk of Bias Assessment
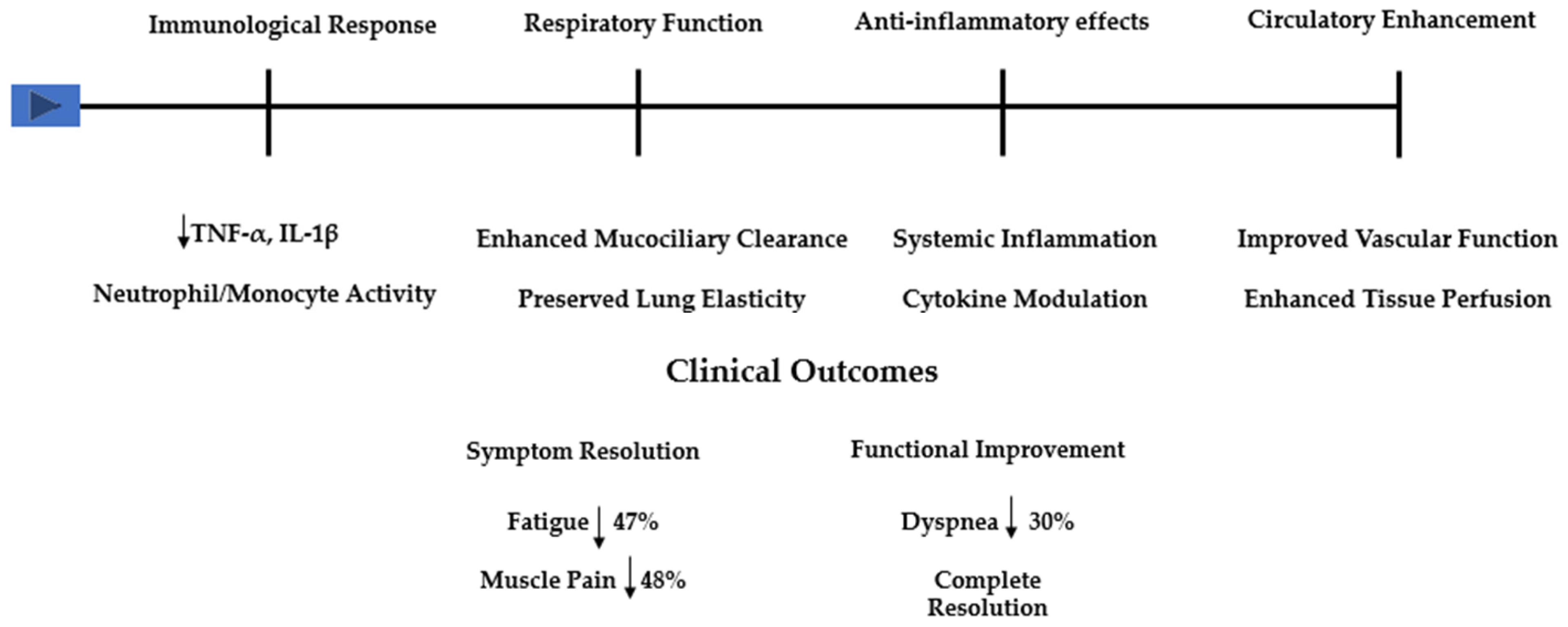
4. Discussion
5. Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mallah, S.I.; Ghorab, O.K.; Al-Salmi, S.; Abdellatif, O.S.; Tharmaratnam, T.; Iskandar, M.A.; Sefen, J.A.N.; Sidhu, P.; Atallah, B.; El-Lababidi, R.; et al. COVID-19: Breaking down a global health crisis. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 35. [Google Scholar] [CrossRef]
- Corrao, S.; Gervasi, F.; Di Bernardo, F.; Natoli, G.; Raspanti, M.; Catalano, N.; Argano, C. Immunological Characteristics of Non-Intensive Care Hospitalized COVID-19 Patients: A Preliminary Report. J. Clin. Med. 2021, 10, 849. [Google Scholar] [CrossRef]
- Mateos González, M.; Sierra Gonzalo, E.; Casado Lopez, I.; Arnalich Fernández, F.; Beato Pérez, J.L.; Monge Monge, D.; Núñez, J.A.V.; Fenoll, R.G.; Fernández, C.S.; Castro, S.J.F.; et al. The Prognostic Value of Eosinophil Recovery in COVID-19: A Multicentre, Retrospective Cohort Study on Patients Hospitalised in Spanish Hospitals. J. Clin. Med. 2021, 10, 305. [Google Scholar] [CrossRef] [PubMed]
- Farré, N.; Mojón, D.; Llagostera, M.; Belarte-Tornero, L.C.; Calvo-Fernández, A.; Vallés, E.; Negrete, A.; García-Guimaraes, M.; Bartolomé, Y.; Fernández, C.; et al. Prolonged QT Interval in SARS-CoV-2 Infection: Prevalence and Prognosis. J. Clin. Med. 2020, 9, 2712. [Google Scholar] [CrossRef] [PubMed]
- Su, S.; Zhao, Y.; Zeng, N.; Liu, X.; Zheng, Y.; Sun, J.; Zhong, Y.; Wu, S.; Ni, S.; Gong, Y.; et al. Epidemiology, clinical presentation, pathophysiology, and management of long COVID: An update. Mol. Psychiatry 2023, 28, 4056–4069. [Google Scholar] [CrossRef] [PubMed]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V.; WHO Clinical Case Definition Working Group on Post-COVID-19 Condition. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, A.; Shetty, A.; Delanerolle, G.; Zeng, Y.; Zhang, Y.; Raymont, V.; Rathod, S.; Halabi, S.; Elliot, K.; Shi, J.Q.; et al. A systematic review and meta-analysis of long COVID symptoms. Syst. Rev. 2023, 27, 88. [Google Scholar] [CrossRef]
- Lippi, G.; Sanchis-Gomar, F.; Henry, B.M. COVID-19 and its long-term sequelae: What do we know in 2023? Pol. Arch. Intern. Med. 2023, 133, 16402. [Google Scholar] [CrossRef]
- Astin, R.; Banerjee, A.; Baker, M.R.; Dani, M.; Ford, E.; Hull, J.H.; Lim, P.B.; McNarry, M.; Morten, K.; O’Sullivan, O.; et al. Long COVID: Mechanisms, risk factors and recovery. Exp. Physiol. 2023, 108, 12–27. [Google Scholar] [CrossRef]
- Koc, H.C.; Xiao, J.; Liu, W.; Li, Y.; Chen, G. Long COVID and its Management. Int. J. Biol. Sci. 2022, 18, 4768–4780. [Google Scholar] [CrossRef] [PubMed]
- Crook, H.; Raza, S.; Nowell, J.; Young, M.; Edison, P. Long covid-mechanisms, risk factors, and management. BMJ 2021, 374, n1648. [Google Scholar] [CrossRef] [PubMed]
- Karagülle, M.; Kardeş, S.; Dişçi, R.; Karagülle, M.Z. Spa therapy adjunct to pharmacotherapy is beneficial in rheumatoid arthritis: A crossover randomized controlled trial. Int. J. Biometeorol. 2018, 62, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Özkuk, K.; Ateş, Z. Balneotherapy in the Treatment of Chronic Shoulder Pain: A Randomized Controlled Clinical Trial. Altern. Ther. Health Med. 2020, 26, 18–24. [Google Scholar] [PubMed]
- Pérez-Fernández, M.R.; Calvo-Ayuso, N.; Martínez-Reglero, C.; Salgado-Barreira, Á.; Muiño López-Álvarez, J.L. Efficacy of baths with mineral-medicinal water in patients with fibromyalgia: A randomized clinical trial. Int. J. Biometeorol. 2019, 63, 1161–1170. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Fioravanti, A.; Cantarini, L.; Guidelli, G.M.; Galeazzi, M. Mechanisms of action of spa therapies in rheumatic diseases: What scientific evidence is there? Rheumatol. Int. 2011, 31, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hernandez Torres, A.; San Martín Bacaicoa, J.; Perea Horno, M.; Martínez Galán, I.; Meijide Failde, R.; Ceballos Hernansanz, Á.; Ramon-Gimenez, J.R.; Casado Moragón, Á.; Saz Peiró, P.; y Viseras Iborra, C. Técnicas y Tecnologías en Hidrología Médica e Hidroterapia. 2006. N° 50. Available online: https://repisalud.isciii.es/rest/api/core/bitstreams/bea82fb0-0df0-4f5e-b4d7-164433615f60/content (accessed on 4 January 2025).
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef] [PubMed]
- Costantino, M.; Giudice, V.; Farroni, M.; Marongiu, F.; De Caro, F.; Filippelli, A. Impact of Spa Therapy on Symptoms and Quality of Life in Post-COVID-19 Patients with Chronic Conditions. J. Clin. Med. 2024, 13, 5091. [Google Scholar] [CrossRef] [PubMed]
- Crucianelli, S.; Mariano, A.; Valeriani, F.; Cocomello, N.; Gianfranceschi, G.; Baseggio Conrado, A.; Moretti, F.; D’Abusco, A.S.; Mennuni, G.; Fraioli, A.; et al. Effects of Sulfur Thermal Water inhalations in long-COVID syndrome: Spa-centred, double-blinded, randomised case-control pilot study. Clin. Med. 2024, 24, 100251. [Google Scholar] [CrossRef] [PubMed]
- Onik, G.; Knapik, K.; Sieroń, K. Long COVID Cardiopulmonary Symptoms and Health Resort Treatment: A Retrospective Study. J. Clin. Med. 2024, 13, 5563. [Google Scholar] [CrossRef]
- Ponikowska, I.; Adamczyk, P.; Wojciechowski, R.; Jarosz, K. Balneological treatment of patients with long COVID-19 syndrome in health-resort conditions. Acta Balneol. 2023, 173, 75–81. [Google Scholar] [CrossRef]
- Shchikota, A.M.; Pogonchenkova, I.V.; Rassulova, M.A.; Filippov, M.S.; Golubev, M.V.; Cherepanov, I.A. Use of hydrobalneotherapy in ambulatory rehabilitation of patients with post-COVID syndrome. Russ. J. Physiother. Balneol. Rehabil. 2023, 22, 141–150. [Google Scholar] [CrossRef]
- Grishechkina, I.A.; Lobanov, A.A.; Andronov, S.V.; Rachin, A.P.; Fesyun, A.D.; Ivanova, E.P.; Masiero, S.; Maccarone, M.C. Long-term outcomes of different rehabilitation programs in patients with long COVID syndrome: A cohort prospective study. Eur. J. Transl. Myol. 2023, 33, 11063. [Google Scholar] [CrossRef]
- Gálvez, I.; Torres-Piles, S.; Ortega-Rincón, E. Balneotherapy, Immune System, and Stress Response: A Hormetic Strategy? Int. J. Mol. Sci. 2018, 6, 1687. [Google Scholar] [CrossRef] [PubMed]
- Mooventhan, A.; Nivethitha, L. Scientific evidence-based effects of hydrotherapy on various systems of the body. N. Am. J. Med Sci. 2014, 6, 199–209. [Google Scholar] [CrossRef]
- Silva, J.; Martins, J.; Nicomédio, C.; Gonçalves, C.; Palito, C.; Gonçalves, R.; Fernandes, P.O.; Nunes, A.; Alves, M.J. A Novel Approach to Assess Balneotherapy Effects on Musculoskeletal Diseases-An Open Interventional Trial Combining Physiological Indicators, Biomarkers, and Patients’ Health Perception. Geriatrics 2023, 8, 55. [Google Scholar] [CrossRef] [PubMed]
- Ortega, E.; Gálvez, I.; Hinchado, M.D.; Guerrero, J.; Martín-Cordero, L.; Torres-Piles, S. Anti-inflammatory effect as a mechanism of effectiveness underlying the clinical benefits of pelotherapy in osteoarthritis patients: Regulation of the altered inflammatory and stress feedback response. Int. J. Biometeorol. 2017, 61, 1777–1785. [Google Scholar] [CrossRef]
- Antonelli, M.; Donelli, D. Effects of balneotherapy and spa therapy on levels of cortisol as a stress biomarker: A systematic review. Int. J. Biometeorol. 2018, 62, 913–924. [Google Scholar] [CrossRef]
- Masiero, S.; Maccarone, M.C.; Magro, G. Balneotherapy and human immune function in the era of COVID-19. Int. J. Biometeorol. 2020, 64, 1433–1434. [Google Scholar] [CrossRef] [PubMed]
- Tamás, B.; Gabriella, K.; Kristóf, Á.; Anett, I.; János Pál, K.; Bálint, T.; Péter, L.; Márton, P.; Katalin, N. The Effects of Lakitelek Thermal Water and Tap Water on Skin Microbiome, a Randomized Control Pilot Study. Life 2023, 13, 746. [Google Scholar] [CrossRef]
- Rapolienė, L.; Razbadauskas, A.; Mockevičienė, D.; Varžaitytė, L.; Skarbalienė, A. Balneotherapy for musculoskeletal pain: Does the mineral content matter? Int. J. Biometeorol. 2020, 64, 965–979. [Google Scholar] [CrossRef]
- Castelli, L.; Galasso, L.; Mulè, A.; Ciorciari, A.; Fornasini, F.; Montaruli, A.; Roveda, E.; Esposito, F. Sleep and spa therapies: What is the role of balneotherapy associated with exercise? A systematic review. Front. Physiol. 2022, 13, 964232. [Google Scholar] [CrossRef] [PubMed]
- Varzaityte, L.; Kubilius, R.; Rapoliene, L.; Bartuseviciute, R.; Balcius, A.; Ramanauskas, K.; Nedzelskiene, I. The effect of balneotherapy and peloid therapy on changes in the functional state of patients with knee joint osteoarthritis: A randomized, controlled, single-blind pilot study. Int. J. Biometeorol. 2020, 64, 955–964. [Google Scholar] [CrossRef]
- Raza, H.M.A.; Krutulyte, G.; Rimdeikiene, I.; Savickas, R. Efficacy of balneotherapy and mud therapy in patients with knee osteoarthritis: A systematic literature review. Aktuelle Rheumatol. 2021, 46, 187–197. [Google Scholar] [CrossRef]
- Munteanu, C.; Munteanu, D.; Hoteteu, M.; Dogaru, G.; Stanescu, I.; Rotariu, M. Therapeutic gases used in balneotherapy and rehabilitation medicine-scientific relevance in the last ten years (2011–2020)-Synthetic literature review. Balneo PRM Res. J. 2021, 12, 111–122. [Google Scholar] [CrossRef]
- Gebretsadik, A.; Taddesse, F.; Melaku, N.; Haji, Y. Balneotherapy for Musculoskeletal Pain Management of Hot Spring Water in Southern Ethiopia: Perceived Improvements. Inquiry 2021, 58, 469580211049063. [Google Scholar] [CrossRef] [PubMed]
- Gusev, E.; Sarapultsev, A. Exploring the Pathophysiology of Long COVID: The Central Role of Low-Grade Inflammation and Multisystem Involvement. Int. J. Mol. Sci. 2024, 25, 6389. [Google Scholar] [CrossRef] [PubMed]
- Pozzi, G.; Masselli, E.; Gobbi, G.; Mirandola, P.; Taborda-Barata, L.; Ampollini, L.; Carbognani, P.; Micheloni, C.; Corazza, F.; Galli, D.; et al. Hydrogen Sulfide Inhibits TMPRSS2 in Human Airway Epithelial Cells: Implications for SARS-CoV-2 Infection. Biomedicines 2021, 9, 1273. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Zhao, Z.; Lv, M.; Wang, H.; Li, L.; Gang, S.; Zuo, L.; Zhang, P.; Wang, Y.; Li, C.; et al. Discovery of Environmental Nanoparticles in a Mineral Water Spring from Yiyuan County, Shandong Province, Eastern China: A New Form of Elements in Mineral Water. Water 2023, 15, 3497. [Google Scholar] [CrossRef]
- Viegas, J.; Esteves, A.F.; Cardoso, E.M.; Arosa, F.A.; Vitale, M.; Taborda-Barata, L. Biological Effects of Thermal Water-Associated Hydrogen Sulfide on Human Airways and Associated Immune Cells: Implications for Respiratory Diseases. Front. Public Health 2019, 7, 128. [Google Scholar] [CrossRef]
- Ortega-Collazos, E.; Hinchado, M.D.; Otero, E.; López-Jurado, C.F.; Gálvez, I.; Legido, J.L.; Muñoz-Torrero, J.F.S.; Ortega, E.; Torres-Piles, S. Balneotherapy (Mud-Bath Therapy) with a Peloid Enriched with Rosmarinic Acid Enhances Clinical Outcomes and Innate Immune Benefits in Elderly Patients with Osteoarthritis: A Pilot Study. Appl. Sci. 2024, 14, 12017. [Google Scholar] [CrossRef]
- Puerto Valencia, L.M.; He, Y.; Wippert, P.M. The changes of blood-based inflammatory biomarkers after non-pharmacologic interventions for chronic low back pain: A systematic review. BMC Musculoskelet. Disord. 2024, 25, 209. [Google Scholar] [CrossRef]
- Tékus, V.; Borbély, É.; Kiss, T.; Perkecz, A.; Kemény, Á.; Horváth, J.; Kvarda, A.; Pintér, E. Investigation of Lake Hévíz Mineral Water Balneotherapy and Hévíz Mud Treatment in Murine Osteoarthritis and Rheumatoid Arthritis Models. Evid.-Based Complement. Altern. Med. 2018, 2018, 4816905. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Wang, J.; Chen, Y.; Ruan, Y.; Dai, S. Efficacy of aquatic exercise in chronic musculoskeletal disorders: A systematic review and meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2023, 18, 942. [Google Scholar] [CrossRef] [PubMed]
- Aquino-Martinez, R.; Hernández-Vigueras, S. Severe COVID-19 Lung Infection in Older People and Periodontitis. J. Clin. Med. 2021, 10, 279. [Google Scholar] [CrossRef] [PubMed]
- Firouzi, M.; Ehteshamzadeh, M.; Saba, F.; Khayati, G.R. Effect of mineral nanoparticles obtained from thermal spring water on COVID-19. Environ. Health Eng. Manag. 2023, 10, 33–39. [Google Scholar] [CrossRef]
- Parotto, E.; Lamberti-Castronuovo, A.; Censi, V.; Valente, M.; Atzori, A.; Ragazzoni, L. Exploring Italian healthcare facilities response to COVID-19 pandemic: Lessons learned from the Italian Response to COVID-19 initiative. Front. Public Health 2023, 10, 1016649. [Google Scholar] [CrossRef]

| Criterion | Description |
|---|---|
| Population | Adults (≥18 years) with confirmed post-acute COVID-19 syndrome. The 12-week minimum interval from initial SARS-CoV-2 infection was adopted following WHO criteria for post-COVID-19 condition definition [6] |
| Intervention | Balneotherapy, thermal therapy, or thermal spa treatments. The minimum treatment duration of 5 days was established based on previous systematic reviews demonstrating this as the minimum period necessary to achieve therapeutic effects in balneotherapy protocols [16]. All interventions required supervision by healthcare professionals and clear documentation of water composition and treatment protocols |
| Outcomes | Primary: Changes in symptom severity (validated scales) Quality of life measures Functional capacity assessments Secondary: Physiological parameters Adverse events Treatment adherence Patient satisfaction |
| Study design | Randomized controlled trials, non-randomized controlled trials, prospective and retrospective cohort studies, and case-control studies |
| Author (Year) | Study Design and Sample | Intervention Details | Duration and Assessment | Primary Outcomes | Key Findings |
|---|---|---|---|---|---|
| Costantino et al. (2024) [19] | Prospective observational; n = 159 (87 symptomatic) | Comprehensive spa therapy program, including balneotherapy and/or inhalation therapy | 2-week therapeutic spa cycle; Follow-up assessments at completion |
|
|
| Crucianelli et al. (2024) [20] | Double-blind, randomized pilot trial; n = 30 (15 per group) | Active: Sulfur thermal water inhalations Control: Sterile distilled water inhalations Daily treatments | 12 consecutive days; Assessments at baseline, 14 days, 3 months |
|
|
| Onik et al. (2024) [21] | Retrospective study; n = 122 (71 F, 51 M) | Comprehensive health resort treatment:
| Mean 24.59 ± 6.38 days |
|
|
| Ponikowska et al. (2023) [22] | Prospective intervention; n = 33 (19 F, 14 M) | Multimodal program:
| 14–28 days; 5 procedures daily |
|
|
| Shchikota et al. (2023) [23] | Prospective cohort with parallel groups; n = 160 (74 M, 86 F) | Four treatment arms: 1. Chloride-sodium baths 2. Whirlpool baths 3. “Biolong” baths 4. Control group All with exercise therapy | 10-day hydrotherapy course |
|
|
| Grishechkina et al. (2023) [24] | Prospective cohort; n = 113 (120 initial, 7 dropouts) | Four rehabilitation approaches:
| 7–15 sessions; 6-month follow-up |
|
|
| Study | Design | Tool | Domain 1 | Domain 2 | Domain 3 | Domain 4 | Domain 5 | Domain 6 | Domain 7 | Overall Risk |
|---|---|---|---|---|---|---|---|---|---|---|
| Costantino et al. [19] | Prospective observational | ROBINS-I | Confounding: Moderate | Selection of participants: Low | Classification of interventions: Low | Deviations from intended interventions: Low | Missing data: Low | Measurement of outcomes: Moderate | Selection of the reported result: Low | Moderate |
| Crucianelli et al. [20] | RCT | RoB 2 | Randomization process: Low | Deviations from intended interventions: Low | Missing outcome data: Low | Measurement of the outcome: Low | Selection of the reported result: Some concerns | N/A | N/A | Low |
| Onik et al. [21] | Retrospective | ROBINS-I | Confounding: Moderate | Selection of participants: Low | Classification of interventions: Low | Deviations from intended interventions: Low | Missing data: No information | Measurement of outcomes: Low | Selection of the reported result: Low | Moderate |
| Ponikowska et al. [22] | Prospective intervention | ROBINS-I | Confounding: Moderate | Selection of participants: Low | Classification of interventions: Low | Deviations from intended interventions: Low | Missing data: Low | Measurement of outcomes: Low | Selection of the reported result: Moderate | Moderate |
| Shchikota et al. [23] | Prospective cohort | ROBINS-I | Confounding: Moderate | Selection of participants: Low | Classification of interventions: Low | Deviations from intended interventions: Low | Missing data: No information | Measurement of outcomes: Low | Selection of the reported result: Moderate | Low |
| Grishechkina et al. [24] | Prospective cohort | ROBINS-I | Confounding: Moderate | Selection of participants: Low | Classification of interventions: Low | Deviations from intended interventions: Low | Missing data: Low | Measurement of outcomes: Low | Selection of the reported result: Moderate | Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrara, E.; Scaramuzzino, M.; Murmura, G.; D’Addazio, G.; Sinjari, B. Emerging Evidence on Balneotherapy and Thermal Interventions in Post-COVID-19 Syndrome: A Systematic Review. Healthcare 2025, 13, 96. https://doi.org/10.3390/healthcare13020096
Ferrara E, Scaramuzzino M, Murmura G, D’Addazio G, Sinjari B. Emerging Evidence on Balneotherapy and Thermal Interventions in Post-COVID-19 Syndrome: A Systematic Review. Healthcare. 2025; 13(2):96. https://doi.org/10.3390/healthcare13020096
Chicago/Turabian StyleFerrara, Elisabetta, Manela Scaramuzzino, Giovanna Murmura, Gianmaria D’Addazio, and Bruna Sinjari. 2025. "Emerging Evidence on Balneotherapy and Thermal Interventions in Post-COVID-19 Syndrome: A Systematic Review" Healthcare 13, no. 2: 96. https://doi.org/10.3390/healthcare13020096
APA StyleFerrara, E., Scaramuzzino, M., Murmura, G., D’Addazio, G., & Sinjari, B. (2025). Emerging Evidence on Balneotherapy and Thermal Interventions in Post-COVID-19 Syndrome: A Systematic Review. Healthcare, 13(2), 96. https://doi.org/10.3390/healthcare13020096









