Prognostic Factors for Responders of Home-Based Pulmonary Rehabilitation—Secondary Analysis of a Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Overview of the Randomized Controlled Trial and Main Findings
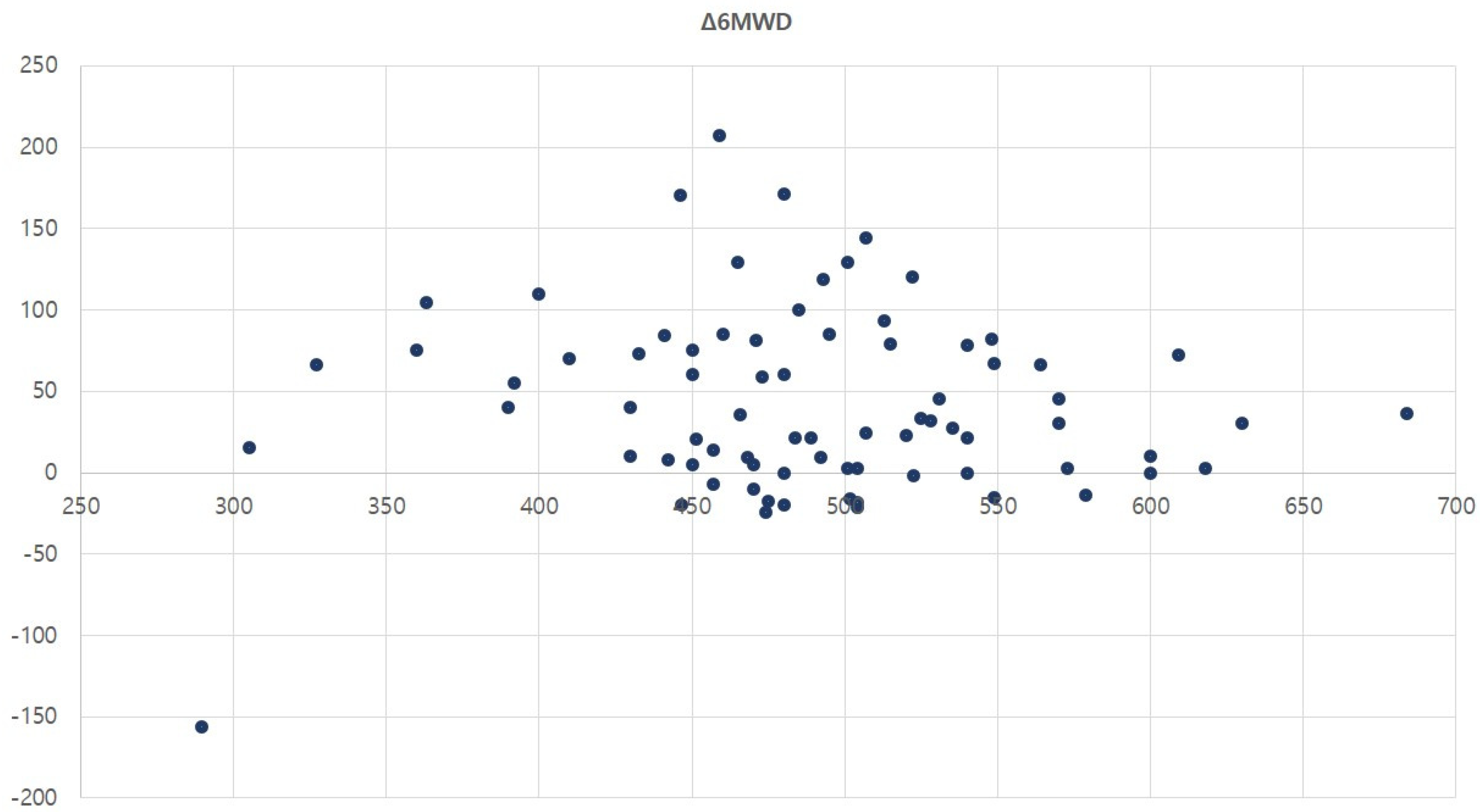
2.2. Analysis of 6 Min Walk Distance Results
2.3. Analysis of Patient-Reported Outcome Measures
3. Results
4. Discussion
4.1. Changes in Outcome Parameters Following Home-Based Pulmonary Rehabilitation
4.2. Digital Therapeutics and Pulmonary Rehabilitation
4.3. Limitations of the Present Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nici, L.; Donner, C.; Wouters, E.; Zuwallack, R.; Ambrosino, N.; Bourbeau, J.; Carone, M.; Celli, B.; Engelen, M.; Fahy, B.; et al. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2006, 173, 1390–1413. [Google Scholar] [CrossRef] [PubMed]
- Rochester, C.L.; Alison, J.A.; Carlin, B.; Jenkins, A.R.; Cox, N.S.; Bauldoff, G.; Bhatt, S.P.; Bourbeau, J.; Burtin, C.; Camp, P.G.; et al. Pulmonary Rehabilitation for Adults with Chronic Respiratory Disease: An Official American Thoracic Society Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2023, 208, e7–e26. [Google Scholar] [CrossRef]
- Uzzaman, M.N.; Agarwal, D.; Chan, S.C.; Patrick Engkasan, J.; Habib, G.M.M.; Hanafi, N.S.; Jackson, T.; Jebaraj, P.; Khoo, E.M.; Mirza, F.T.; et al. Effectiveness of home-based pulmonary rehabilitation: Systematic review and meta-analysis. Eur. Respir. Rev. 2022, 31, 220076. [Google Scholar] [CrossRef]
- Bondarenko, J.; Babic, C.; Burge, A.T.; Holland, A.E. Home-based pulmonary rehabilitation: An implementation study using the RE-AIM framework. ERJ Open Res. 2021, 7, 00469-2020. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Song, J.H.; Kim, S.H. Validation of Wearable Digital Devices for Heart Rate Measurement During Exercise Test in Patients with Coronary Artery Disease. Ann. Rehabil. Med. 2023, 47, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Han, S.H.; Choi, M.S.; Kim, Y.M.; Kim, D.M.; Park, H.E.; Hong, J.W.; Kim, S.H.; Shin, Y.B.; Lee, B.J. Is Age-Predicted Maximal Heart Rate Applicable in Patients with Heart or Lung Disease? Ann. Rehabil. Med. 2022, 46, 133–141. [Google Scholar] [CrossRef]
- Kim, C.; Song, J.; Kim, S. The Accessibility and Effect of Cardiac Rehabilitation in COVID-19 Pandemic Era. Ann. Rehabil. Med. 2024, 48, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Choi, H.E.; Rhee, C.K.; Song, J.H.; Lee, J.H. Efficacy of Digital Therapeutics for Pulmonary Rehabilitation: A Multi-Center, Randomized Controlled Trial. Life 2024, 14, 469. [Google Scholar] [CrossRef]
- Janjua, S.; Banchoff, E.; Threapleton, C.J.; Prigmore, S.; Fletcher, J.; Disler, R.T. Digital interventions for the management of chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2021, 4, CD013246. [Google Scholar] [CrossRef]
- Selzler, A.M.; Simmonds, L.; Rodgers, W.M.; Wong, E.Y.; Stickland, M.K. Pulmonary rehabilitation in chronic obstructive pulmonary disease: Predictors of program completion and success. COPD 2012, 9, 538–545. [Google Scholar] [CrossRef]
- Al Chikhanie, Y.; Bailly, S.; Veale, D.; Herengt, F.; Verges, S. Predictors of changes in 6-min walking distance following pulmonary rehabilitation in COPD patients: A retrospective cohort analysis. Eur. J. Phys. Rehabil. Med. 2022, 58, 251–257. [Google Scholar] [CrossRef]
- Garrod, R.; Marshall, J.; Barley, E.; Jones, P.W. Predictors of success and failure in pulmonary rehabilitation. Eur. Respir. J. 2006, 27, 788–794. [Google Scholar] [CrossRef] [PubMed]
- Hafner, T.; Pirc Marolt, T.; Selb, J.; Groselj, A.; Kosten, T.; Simonic, A.; Košnik, M.; Korošec, P. Predictors of Success of Inpatient Pulmonary Rehabilitation Program in COPD Patients. Int. J. Chron. Obs. Pulmon Dis. 2023, 18, 2483–2495. [Google Scholar] [CrossRef] [PubMed]
- Vagaggini, B.; Costa, F.; Antonelli, S.; De Simone, C.; De Cusatis, G.; Martino, F.; Santerini, S.; Paggiaro, P. Clinical predictors of the efficacy of a pulmonary rehabilitation programme in patients with COPD. Respir. Med. 2009, 103, 1224–1230. [Google Scholar] [CrossRef] [PubMed]
- Pradella, C.O.; Belmonte, G.M.; Maia, M.N.; Delgado, C.S.; Luise, A.P.; Nascimento, O.A.; Gazzotti, M.R.; Jardim, J.R. Home-Based Pulmonary Rehabilitation for Subjects with COPD: A Randomized Study. Respir. Care 2015, 60, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Marjanski, T.; Wnuk, D.; Bosakowski, D.; Szmuda, T.; Sawicka, W.; Rzyman, W. Patients who do not reach a distance of 500 m during the 6-min walk test have an increased risk of postoperative complications and prolonged hospital stay after lobectomy. Eur. J. Cardiothorac. Surg. 2015, 47, e213–e219. [Google Scholar] [CrossRef] [PubMed]
- Keeratichananont, W.; Thanadetsuntorn, C.; Keeratichananont, S. Value of preoperative 6-minute walk test for predicting postoperative pulmonary complications. Ther. Adv. Respir. Dis. 2016, 10, 18–25. [Google Scholar] [CrossRef]
- Kon, S.S.; Canavan, J.L.; Jones, S.E.; Nolan, C.M.; Clark, A.L.; Dickson, M.J.; Haselden, B.M.; Polkey, M.I.; Man, W.D.-C. Minimum clinically important difference for the COPD Assessment Test: A prospective analysis. Lancet Respir. Med. 2014, 2, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Kubincova, A.; Takac, P.; Demjanovic Kendrova, L.; Joppa, P. Predictors of Quality-of-Life Improvement at Different Minimum Clinically Important Difference Values in Patients with Chronic Obstructive Pulmonary Disease after Climatic Rehabilitation Treatment. Life 2023, 13, 1763. [Google Scholar] [CrossRef] [PubMed]
- Araújo Oliveira, A.L.; Andrade, L.; Marques, A. Minimal clinically important difference and predictive validity of the mMRC and mBorg in acute exacerbations of COPD. Eur. Respir. J. 2017, 50, PA4705. [Google Scholar]
- Spruit, M.A.; Singh, S.J.; Garvey, C.; ZuWallack, R.; Nici, L.; Rochester, C.; Hill, K.; Holland, A.E.; Lareau, S.C.; Man, W.D.-C.; et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2013, 188, e13–e64. [Google Scholar] [CrossRef] [PubMed]
- Morishita-Katsu, M.; Nishimura, K.; Taniguchi, H.; Kimura, T.; Kondoh, Y.; Kataoka, K.; Ogawa, T.; Watanabe, F.; Arizono, S.; Nishiyama, O.; et al. The COPD assessment test and St George’s Respiratory Questionnaire: Are they equivalent in subjects with COPD? Int. J. Chron. Obs. Pulmon Dis. 2016, 11, 1543–1551. [Google Scholar]
- Sahin, H.; Naz, I.; Varol, Y.; Aksel, N.; Tuksavul, F.; Ozsoz, A. COPD patients with severe diffusion defect in carbon monoxide diffusing capacity predict a better outcome for pulmonary rehabilitation. Rev. Port. Pneumol. 2016, 22, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, A.; Putcha, N.; MacIntyre, N.R.; Jensen, R.L.; Kinney, G.; Stringer, W.W.; Hersh, C.P.; Bowler, R.P.; Casaburi, R.; Han, M.K.; et al. Diffusing Capacity and Mortality in Chronic Obstructive Pulmonary Disease. Ann. Am. Thorac. Soc. 2023, 20, 38–46. [Google Scholar] [CrossRef]
- Ni, Y.; Yu, Y.; Dai, R.; Shi, G. Diffusing capacity in chronic obstructive pulmonary disease assessment: A meta-analysis. Chron. Respir. Dis. 2021, 18, 14799731211056340. [Google Scholar] [CrossRef]
- Devalla, L.; Ghewade, B.; Jadhav, U.; Annareddy, S. Resolving the Complexity: A Comprehensive Review on Carbon Monoxide Diffusion Capacity in Chronic Obstructive Pulmonary Disease Patients. Cureus 2024, 16, e53492. [Google Scholar] [CrossRef] [PubMed]
- Peno-Green, L.; Verrill, D.; Vitcenda, M.; Macintyre, N.; Graham, H. Patient and program outcome assessment in pulmonary rehabilitation: An AACVPR statement. J. Cardiopulm. Rehabil. Prev. 2009, 29, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.L.; Marques, A.S. Outcome Measures Used in Pulmonary Rehabilitation in Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease: A Systematic Review. Phys. Ther. 2018, 98, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Souto-Miranda, S.; Rodrigues, G.; Spruit, M.A.; Marques, A. Pulmonary rehabilitation outcomes in individuals with chronic obstructive pulmonary disease: A systematic review. Ann. Phys. Rehabil. Med. 2022, 65, 101564. [Google Scholar] [CrossRef]
- Shi, G.; Chen, C. Home-based versus outpatient pulmonary rehabilitation program for patients with chronic obstructive pulmonary disease: A protocol for systematic review and meta-analysis. Medicine 2021, 100, e26099. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.; Lee, J.W.; Lee, S.W.; Jo, M.W. Clinical Efficacy of Mobile App-Based, Self-Directed Pulmonary Rehabilitation for Patients with Chronic Obstructive Pulmonary Disease: Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth 2024, 12, e41753. [Google Scholar] [CrossRef]
- Bourne, S.; DeVos, R.; North, M.; Chauhan, A.; Green, B.; Brown, T.; Cornelius, V.; Wilkinson, T. Online versus face-to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: Randomised controlled trial. BMJ Open 2017, 7, e014580. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Lee, C.; Shin, H. Digital therapeutics from bench to bedside. npj Digit. Med. 2023, 6, 38. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-J.; Choi, H.-E.; Jang, H.-J.; Kim, H.-K.; Park, J.-H.; Lee, J.-H.; Kim, T.-H. Current status and trends of pulmonary rehabilitation in South Korea: National level data analysis using Health Insurance Review and Assessment Service (HIRA) database from 2016 to 2018. Medicine 2022, 101, e31085. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Kim, K.U.; Kim, D.K.; Kim, Y.I.; Kim, T.H.; Lee, W.Y.; Park, S.J.; Park, Y.B.; Song, J.W.; Shin, K.C.; et al. Pulmonary Rehabilitation Is Associated with Decreased Exacerbation and Mortality in Patients with COPD: A Nationwide Korean Study. Chest 2024, 165, 313–322. [Google Scholar] [CrossRef]
- Stone, P.W.; Hickman, K.; Steiner, M.C.; Roberts, C.M.; Quint, J.K.; Singh, S.J. Predictors of pulmonary rehabilitation completion in the, U.K. ERJ Open Res. 2021, 7, 00509-2020. [Google Scholar] [CrossRef]
- Augustine, A.; Bhat, A.; Vaishali, K.; Magazine, R. Barriers to pulmonary rehabilitation—A narrative review and perspectives from a few stakeholders. Lung India 2021, 38, 59–63. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Responders (n = 31) | Non-Responders (n = 46) | p-Value | |
|---|---|---|---|---|
| Group (DTx/CG ratio) | 21:10 | 18:28 | 0.01 | |
| Age (years) | 66.7 ± 7.1 | 64.8 ± 10.1 | 0.36 | |
| Sex, male/female ratio | 25:6 | 39:7 | 0.64 | |
| Height (m) | 1.64 ± 0.7 | 1.67 ± 0.6 | 0.05 | |
| Weight (kg) | 64.3 ± 14.9 | 64.8 ± 12.5 | 0.87 | |
| BMI (kg/m2) | 23.6 ± 4.6 | 32.1 ± 4.0 | 0.58 | |
| Patients with smoking history | 24 | 32 | 0.48 | |
| Smoking history (pack per day × year) | 28.1.7 ± 26.0 | 22.4 ± 17.9 | 0.27 | |
| O2 Saturation | 96.8 ± 2.0 | 96.6 ± 2.1 | 0.65 | |
| FVC (%) | 80.4 ± 13.8 | 77.3 ± 18.4 | 0.41 | |
| FEV1 (%) | 66.8 ± 11.2 | 66.3 ± 20.3 | 0.86 | |
| FEV1/FVC (%) | 61.0 ± 14.2 | 62.3 ± 16.2 | 0.72 | |
| DLCO (absolute value) | 13.7 ± 3.7 | 14.9 ± 4.2 | 0.45 | |
| Acute exacerbations | Moderate | 1 | 2 | 0.39 |
| Severe | 4 | 7 | 0.27 | |
| Baseline | 6MWD | 471.0 ± 62.8 | 501.0 ± 73.3 | 0.07 |
| mMRC | 1.2 ± 0.5 | 1.4 ± 0.7 | 0.57 | |
| CAT | 18.2 ± 7.0 | 17.5 ± 6.7 | 0.64 | |
| SGRQ | 29.6 ± 13.6 | 28.2 ± 13.3 | 0.64 | |
| HADS | 9.0 ± 5.7 | 10.0 ± 5.8 | 0.49 | |
| Characteristics | ≥500 m Group (n = 34) | <500 m Group (n = 43) | p-Value | |
|---|---|---|---|---|
| Group (DTx/CG ratio) | 17:17 | 22:21 | 0.92 | |
| Age (years) | 63.6 ± 10.4 | 67.2 ± 7.6 | 0.09 | |
| Sex, male/female ratio | 26:8 | 38:5 | 0.17 | |
| Height (m) | 1.66 ± 0.0 | 1.66 ± 0.1 | 0.74 | |
| Weight (kg) | 63.4 ± 9.4 | 65.6 ± 16.0 | 0.48 | |
| BMI (kg/m2) | 22.8 ± 2.9 | 23.7 ± 5.1 | 0.39 | |
| Patients with smoking history | 22 | 34 | 0.05 | |
| Smoking history (pack per day × year) | 21.0 ± 19.0 | 28.0 ± 23.3 | 0.17 | |
| O2 Saturation | 97.6 ± 1.9 | 95.9 ± 1.9 | 0.00 | |
| FVC (%) | 80.1 ± 15.4 | 77.4 ± 17.7 | 0.49 | |
| FEV1 (%) | 72.5 ± 12.9 | 61.7 ± 18.6 | 0.00 | |
| FEV1/FVC (%) | 68.2 ± 13.4 | 56.8 ± 15.0 | 0.00 | |
| DLCO (absolute value) | 14.2 ± 3.8 | 14.1 ± 4.3 | 0.94 | |
| Acute exacerbations | Moderate | 0 | 3 | 0.11 |
| Severe | 4 | 7 | 0.50 | |
| Baseline | 6MWD | 547.2 ± 44.0 | 442.5 ± 49.9 | 0.00 |
| mMRC | 1.1± 0.4 | 1.3 ± 0.8 | 0.25 | |
| CAT | 18.2 ± 4.9 | 17.4 ± 8.0 | 0.56 | |
| SGRQ | 24.6 ± 9.1 | 32.1 ± 15.2 | 0.01 | |
| HADS | 9.5 ± 6.2 | 9.7 ± 5.5 | 0.88 | |
| 8 week follow up | 6MWD | 582.8 ± 58.1 | 489.9 ± 87.7 | 0.00 |
| mMRC | 0.9 ± 0.4 | 1.3 ± 0.8 | 0.01 | |
| CAT | 14.4 ± 7.3 | 16.7 ± 8.5 | 0.22 | |
| SGRQ | 22.7 ± 10.0 | 33.3 ± 15.8 | 0.00 | |
| HADS | 8.5 ± 6.5 | 8.1 ± 6.0 | 0.77 | |
| Six MWD Results | DTx (n = 39) | CG (n = 38) | p-Value | ≥500 m (n = 34) | <500 m (n = 43) | p-Value |
|---|---|---|---|---|---|---|
| Exceeded MCID | 21 | 10 | 0.01 | 10 | 21 | 0.08 |
| Gradual improvement | 19 | 8 | 0.01 | 9 | 18 | 0.16 |
| Gradual improvement over MCID | 16 | 7 | 0.03 | 6 | 17 | 0.03 |
| Gradual decline | 0 | 3 | 0.08 | 0 | 3 | 0.08 |
| Deterioration from the baseline | 12 | 19 | 0.09 | 16 | 15 | 0.28 |
| Independent Variables | mMRC Improvement | ΔCAT Exceeding MCID | ΔSGRQ Exceeding MCID |
|---|---|---|---|
| Groups (DTx vs. CG) | 22.7, 1.8–287.2 (a) | 11.1, 2.7–46.6 (b) | 9.4, 2.1–43.2 (c) |
| Age | 0.9, 0.8–1.0 | 0.9, 0.8–1.0 | 1.0, 0.9–1.0 |
| Male sex | 0.6, 0.1–3.4 | 0.8, 0.2–4.2 | 1.1, 0.3–4.8 |
| DLCO (absolute value) | 0.5, 0.3–0.9 (a) | 0.9, 0.8–1.1 | 1.0, 0.9–1.2 |
| Current smoker | 0.5, 0.0–9.7 | 1.4, 0.2–7.9 | 0.3, 0.0–2.8 |
| Comorbid liver dz. | 0.0, - | 0.6, 0.0–13.6 | 3.0, 0.1–62.6 |
| Comorbid cancer | 6.7, 0.0–12,074.7 | 2.1, 0.1–31.0 | 0.0, - |
| CAT at Week 8 | ΔCAT | SGRQ at Week 8 | ΔSGRQ | ||
|---|---|---|---|---|---|
| Δ6MWD | Pearson’s Correlation Coefficient | −0.29 | −0.35 | −0.36 | −0.81 |
| p-value | 0.01 | 0.00 | 0.38 | 0.24 | |
| N | 77 | 77 | 77 | 77 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, C.; Choi, H.-E.; Rhee, C.K.; Lee, J.H.; Oh, J.H.; Song, J.H. Prognostic Factors for Responders of Home-Based Pulmonary Rehabilitation—Secondary Analysis of a Randomized Controlled Trial. Healthcare 2025, 13, 308. https://doi.org/10.3390/healthcare13030308
Kim C, Choi H-E, Rhee CK, Lee JH, Oh JH, Song JH. Prognostic Factors for Responders of Home-Based Pulmonary Rehabilitation—Secondary Analysis of a Randomized Controlled Trial. Healthcare. 2025; 13(3):308. https://doi.org/10.3390/healthcare13030308
Chicago/Turabian StyleKim, Chul, Hee-Eun Choi, Chin Kook Rhee, Jae Ha Lee, Ju Hyun Oh, and Jun Hyeong Song. 2025. "Prognostic Factors for Responders of Home-Based Pulmonary Rehabilitation—Secondary Analysis of a Randomized Controlled Trial" Healthcare 13, no. 3: 308. https://doi.org/10.3390/healthcare13030308
APA StyleKim, C., Choi, H.-E., Rhee, C. K., Lee, J. H., Oh, J. H., & Song, J. H. (2025). Prognostic Factors for Responders of Home-Based Pulmonary Rehabilitation—Secondary Analysis of a Randomized Controlled Trial. Healthcare, 13(3), 308. https://doi.org/10.3390/healthcare13030308







