Effects of Distance, Noise, and Personal Respiratory Protective Equipment on Speech Comprehension in Simulated Critical Care Setting
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population and Sampling Strategy
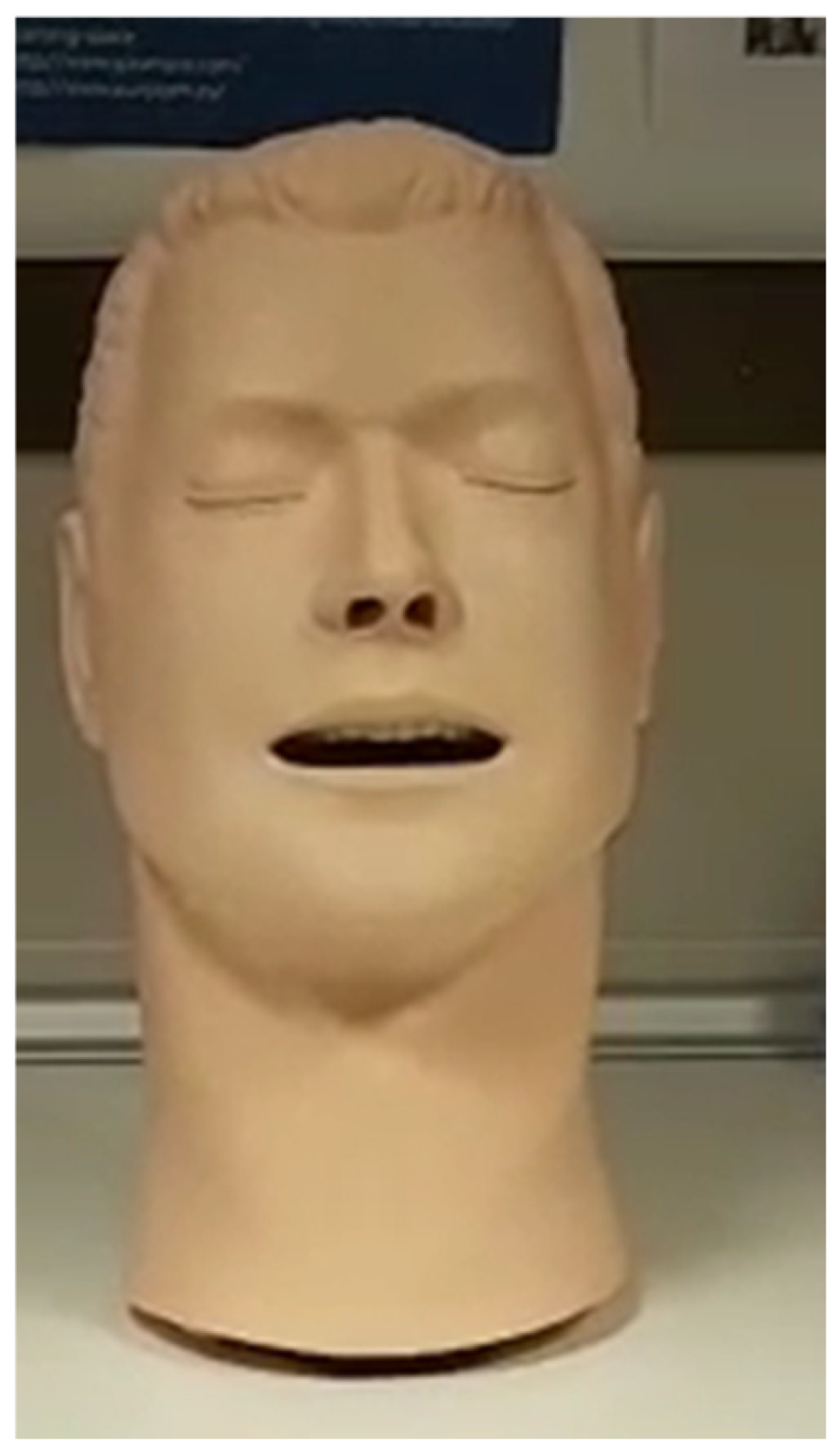
2.3. Devices and Experimental Context
2.4. Respiratory Protection Equipment: Respiratory Masks and PAPR Equipment
2.5. Experimental Design I: Conditions of the Experiment and Manipulation of Variables
2.6. Experimental Design II: Word Recognition and Sound Emission Conditions
2.7. Experimental Design III: Experiment Protocol
2.8. Data Collection Tools
2.9. Statistical Analysis
2.10. Ethical Considerations
3. Results
3.1. Participant Analysis
3.2. Descriptive Analysis of Percentage of Correct Responses
3.3. Descriptive Analysis of Experimental Data
3.3.1. Impact of Distance Between Interlocutors on Message Comprehension
3.3.2. Impact of Respiratory Protection Equipment on Message Comprehension
3.3.3. Impact of Ambient Noise Conditions on Message Comprehension
3.3.4. Relational Analysis Among Variables
Friedman Chi-Square Test
Wilcoxon Test
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, M.S.; Seong, D.; Li, H.; Chung, S.K.; Park, Y.; Lee, M.; Lee, S.W.; Yon, D.K.; Kim, J.H.; Lee, K.H.; et al. Comparative effectiveness of N95, surgical or medical, and non-medical facemasks in protection against respiratory virus infection: A systematic review and network meta-analysis. Rev. Med. Virol. 2022, 32, e2336. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Dana, T.; Jungbauer, R.; Weeks, C.; McDonagh, M.S. Masks for Prevention of Respiratory Virus Infections, Including SARS-CoV-2, in Health Care and Community Settings. Ann. Intern. Med. 2020, 173, 542–555. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.C.H.; Seet, R.C.S.; Lee, K.-H.; Wilder-Smith, E.P.V.; Chuah, B.Y.S.; Ong, B.K.C. Headaches and the N95 face-mask amongst healthcare providers. Acta Neurol. Scand. 2006, 113, 199–202. [Google Scholar] [CrossRef] [PubMed]
- I Foo, C.C.; Goon, A.T.J.; Leow, Y.; Goh, C. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome—A descriptive study in Singapore. Contact Dermat. 2006, 55, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Moon, I.-J.; Jo, M.; Kim, G.-Y.; Kim, N.; Cho, Y.-S.; Hong, S.-H.; Seol, H.-Y. How Does a Face Mask Impact Speech Perception? Healthcare 2022, 10, 1709. [Google Scholar] [CrossRef] [PubMed]
- Magee, M.; Lewis, C.; Noffs, G.; Reece, H.; Chan, J.C.S.; Zaga, C.J.; Paynter, C.; Birchall, O.; Azocar, S.R.; Ediriweera, A.; et al. Effects of face masks on acoustic analysis and speech perception: Implications for peri-pandemic protocols. J. Acoust. Soc. Am. 2020, 148, 3562–3568. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Agea, J.L.; Orcajada-Muñoz, I.; Leal-Costa, C.; Adánez-Martínez, M.G.; Oliveira, A.C.D.S.; Rojo-Rojo, A. How Did the Pandemic Affect Communication in Clinical Settings? A Qualitative Study with Critical and Emergency Care Nurses. Healthcare 2022, 10, 373. [Google Scholar] [CrossRef]
- Mheidly, N.; Fares, M.Y.; Zalzale, H.; Fares, J. Effect of Face Masks on Interpersonal Communication During the COVID-19 Pandemic. Front. Public Health 2020, 8, 582191. [Google Scholar] [CrossRef]
- Chughtai, A.A.; Stelzer-Braid, S.; Rawlinson, W.; Pontivivo, G.; Wang, Q.; Pan, Y.; Zhang, D.; Zhang, Y.; Li, L.; MacIntyre, C.R. Contamination by respiratory viruses on outer surface of medical masks used by hospital healthcare workers. BMC Infect. Dis. 2019, 19, 491. [Google Scholar] [CrossRef]
- Asadi-Pooya, A.A.; Cross, J.H. Is wearing a face mask safe for people with epilepsy? Acta Neurol. Scan. 2020, 142, 314–316. [Google Scholar] [CrossRef]
- Pörschmann, C.; Lübeck, T.; Arend, J.M. Impact of face masks on voice radiation. J. Acoust. Soc. Am. 2020, 148, 3663–3670. [Google Scholar] [CrossRef]
- Ho, G.-Y.; Kansy, I.K.; Klavacs, K.A.; Leonhard, M.; Schneider-Stickler, B. Effect of FFP2/3 Masks on Voice Range Profile Measurement and Voice Acoustics in Routine Voice Diagnostics. Folia Phoniatr. Logop. 2022, 74, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, A.; Celik, S.; Kilic, M.A. Effects of Personal Protective Equipment on Speech Acoustics. Sisli Etfal Hastan. Tip Bul. 2023, 57, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Sönnichsen, R.; Tó, G.L.; Hochmuth, S.; Hohmann, V.; Radeloff, A. How Face Masks Interfere with Speech Understanding of Normal-Hearing Individuals: Vision Makes the Difference. Otol. Neurotol. 2022, 43, 282–288. [Google Scholar] [CrossRef]
- Holm, A.; Dreyer, P. Nurses’ experiences of the phenomenon ‘isolation communication’. Nurs. Crit. Care 2023, 28, 885–892. [Google Scholar] [CrossRef] [PubMed]
- Terzi, B.; Azizoğlu, F.; Polat, Ş.; Kaya, N.; Işsever, H. The effects of noise levels on nurses in intensive care units. Nurs. Crit. Care 2019, 24, 299–305. [Google Scholar] [CrossRef]
- Darbyshire, J.L.; Young, J.D. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Crit. Care 2013, 17, R187. [Google Scholar] [CrossRef]
- Andrade, E.d.L.; Silva, D.C.d.C.e.; de Lima, E.A.; de Oliveira, R.A.; Zannin, P.H.T.; Martins, A.C.G. Environmental noise in hospitals: A systematic review. Environ. Sci. Pollut. Res. 2021, 28, 19629–19642. [Google Scholar] [CrossRef]
- Birgitta, B.; Lindvall, T.; Schwela, D.H. Occupational and Environmental Health Team. Guidelines for Community Noise; World Health Organization (WHO): Geneva, Switzerland, 1999; Available online: https://apps.who.int/iris/handle/10665/66217 (accessed on 1 May 2024).
- Corey, R.M.; Jones, U.; Singer, A.C. Acoustic effects of medical, cloth, and transparent face masks on speech signals. J. Acoust. Soc. Am. 2020, 148, 2371–2375. [Google Scholar] [CrossRef] [PubMed]
- Randazzo, M.; Koenig, L.L.; Priefer, R. The effect of face masks on the intelligibility of unpredictable sentences. In Proceedings of the 179th Meeting of the Acoustical Society of America, Philadelphia, PA, USA, 7–11 December 2020. [Google Scholar] [CrossRef]
- Chmelík, V.; Urbán, D.; Zelem, L.; Rychtáriková, M. Effect of Mouth Mask and Face Shield on Speech Spectrum in Slovak Language. Appl. Sci. 2021, 11, 4829. [Google Scholar] [CrossRef]
- Karagkouni, O. The Effects of the Use of Protective Face Mask on the Voice and Its Relation to Self-Perceived Voice Changes. J. Voice 2023, 37, 802.e1–802.e14. [Google Scholar] [CrossRef] [PubMed]
- Shekaraiah, S.; Suresh, K. Effect of Face Mask on Voice Production During COVID-19 Pandemic: A Systematic Review. J. Voice 2021, 38, 446–457. [Google Scholar] [CrossRef] [PubMed]
- Wittum, K.J.; Feth, L.L.; Hoglund, E.M. The effects of surgical masks on speech perception in noise. J. Acoust. Soc. Am. 2013, 133, 3391. [Google Scholar] [CrossRef]
- Rahne, T.; Fröhlich, L.; Plontke, S.; Wagner, L. Influence of surgical and N95 face masks on speech perception and listening effort in noise. PLoS ONE 2021, 16, e0253874. [Google Scholar] [CrossRef] [PubMed]
- Toscano, J.C.; Toscano, C.M. Effects of face masks on speech recognition in multi-talker babble noise. PLoS ONE 2021, 16, e0246842. [Google Scholar] [CrossRef] [PubMed]
- Aliabadi, M.; Aghamiri, Z.S.; Farhadian, M.; Motlagh, M.S.; Nahrani, M.H. The Influence of Face Masks on Verbal Communication in Persian in the Presence of Background Noise in Healthcare Staff. Acoust. Aust. 2022, 50, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Yi, H.; Pingsterhaus, A.; Song, W. Effects of Wearing Face Masks While Using Different Speaking Styles in Noise on Speech Intelligibility During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 682677. [Google Scholar] [CrossRef] [PubMed]
- Hilda, M.; Furmanski, M.C.; Flandín, M.I.; Howlin, M.L.; Sterin, Y.S. PIP-C: Prueba de Identificación de Palabras a Través de Consonantes; Edición del Autor: Buenos Aires, Argentina, 1997. [Google Scholar]
- San Martín-Rodrígueza, L.; Camacho-Bejarano, R. Analysis of the materials for the manufacture of masks: The challenge of facing the shortage of personal protective equipment (spanish version). Enferm. Clín. 2021, 31, s73–s77. [Google Scholar] [CrossRef]
- Saling, M.M. Disorders of Language. In Neurology and Clinical Neuroscience; Schapira, A.H.V., Byrne, E., DiMauro, S., Frackowiak, R.S.J., Johnson, R.T., Mizuno, Y., Samuels, M.A., Silberstein, S.D., Wszolek, Z.K., Eds.; Mosby: Atlanta, GA, USA, 2007; pp. 31–42. [Google Scholar] [CrossRef]
- Valero-García, J.; Vila-Rovira, J.M. Validez, precisión diagnóstica y fiabilidad del Test de Palabras Parónimas Susurradas para la detección rápida de la presbiacusia. Rev. Investig. Logop. 2022, 12, e81057. [Google Scholar] [CrossRef]
- Yeshoda, K.; Siya, S.T.; Chaithanyanayaka, M.; Pallavi, R.S.; Revathi, R. Impact of Facemasks Use on Interpersonal Communication in a Clinical Setup: A Questionnaire Based Study. Indian J. Otolaryngol. Head Neck Surg. 2023, 75, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Park, M.; Kohlrausch, A.; de Bruijn, W.; de Jager, P.; Simons, K. Analysis of the soundscape in an intensive care unit based on the annotation of an audio recording. J. Acoust. Soc. Am. 2014, 135, 1875–1886. [Google Scholar] [CrossRef]
- Pal, J.; Taywade, M.; Pal, R.; Sethi, D. Noise Pollution in Intensive Care Unit: A Hidden Enemy affecting the Physical and Mental Health of Patients and Caregivers. Noise Health 2022, 114, 130–136. [Google Scholar] [CrossRef]
- Ruettgers, N.; Naef, A.C.; Rossier, M.; Knobel, S.E.J.; Jeitziner, M.-M.; Holtforth, M.G.; Zante, B.; Schefold, J.C.; Nef, T.; Gerber, S.M. Perceived sounds and their reported level of disturbance in intensive care units: A multinational survey among healthcare professionals. PLoS ONE 2022, 17, e0279603. [Google Scholar] [CrossRef] [PubMed]
- Yi, H.; Choudhury, M.; Hicks, C. A Transparent Mask and Clear Speech Benefit Speech Intelligibility in Individuals with Hearing Loss. J. Speech Lang Hear Res. 2023, 66, 4558–4574. [Google Scholar] [CrossRef]
- Mitchell, A.; Hill, B. How to communicate effectively while wearing face masks. Pract. Nurs. 2020, 31, 508–510. [Google Scholar] [CrossRef]
- Williams, W.C.; Haque, E.; Mai, B.; Venkatraman, V. Face masks influence emotion judgments of facial expressions: A drift-diffusion model. Sci. Rep. 2023, 13, 8842. [Google Scholar] [CrossRef] [PubMed]
- Healey, E.C.; Jones, R.; Berky, R. Effects of perceived listeners on speakers’ vocal intensity. J. Voice 1997, 11, 67–73. [Google Scholar] [CrossRef]
- Zahorik, P.; Kelly, J.W. Accurate vocal compensation for sound intensity loss with increasing distance in natural environments. J. Acoust. Soc. Am. 2007, 122, EL143–EL150. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Zong, S.; Xi, X.; Xiao, H. Effect of wearing personal protective equipment on acoustic characteristics and speech perception during COVID-19. Appl. Acoust. 2022, 197, 108940. [Google Scholar] [CrossRef] [PubMed]
- Bandaru, S.V.; Augustine, A.M.; Lepcha, A.; Sebastian, S.; Gowri, M.; Philip, A.; Mammen, M.D. The effects of N95 mask and face shield on speech perception among healthcare workers in the coronavirus disease 2019 pandemic scenario. J. Laryngol. Otol. 2020, 134, 895–898. [Google Scholar] [CrossRef]
- Gao, Y.; Feng, Y.; Wu, D.; Lu, F.; He, H.; Tian, C. Effect of Wearing Different Masks on Acoustic, Aerodynamic, and Formant Parameters. J. Voice 2023. [Google Scholar] [CrossRef] [PubMed]
- Goldin, A.; Weinstein, B.E.S.N.; Shiman, N. How Do Medical Masks Degrade Speech Perception. Hear. Rev. 2020, 27, 8–9. Available online: https://hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception (accessed on 1 December 2024).
- Nguyen, D.D.; McCabe, P.; Thomas, D.; Purcell, A.; Doble, M.; Novakovic, D.; Chacon, A.; Madill, C. Acoustic voice characteristics With and Without wearing a facemask. Sci. Rep. 2021, 11, 5651–5661. [Google Scholar] [CrossRef] [PubMed]
- Altan, E.; Barmak, E.; Tatar, E.Ç.; Saylam, G.; Korkmaz, M.H. Which Mask, N95 or Surgical Mask, Causes Hoarseness in Healthcare Workers? J. Voice 2024. [Google Scholar] [CrossRef] [PubMed]
- Gama, R.; Castro, M.E.; van Lith-Bijl, J.T.; Desuter, G. Does the wearing of masks change voice and speech parameters? Eur. Arch. Oto-Rhino-Laryngology 2021, 279, 1701–1708. [Google Scholar] [CrossRef] [PubMed]
- Zollinger, S.A.; Brumm, H. The Lombard effect. Curr. Biol. 2011, 21, R614–R615. [Google Scholar] [CrossRef]
- Palmiero, A.J.; Symons, D.; Morgan, J.W.; Shaffer, R.E. Speech intelligibility assessment of protective facemasks and air-purifying respirators. J. Occup. Environ. Hyg. 2016, 13, 960–968. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Simons, J.; Yorio, P.; Rottach, D.; Zhuang, Z.; Radonovich, L. Speech intelligibility test methodology applied to powered air-purifying respirators used in healthcare. J. Occup. Environ. Hyg. 2021, 18, 28–34. [Google Scholar] [CrossRef]
- Round, M.; Isherwood, P. Speech intelligibility in respiratory protective equipment—Implications for verbal communication in critical care. Trends Anaesth. Crit. Care 2021, 36, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Atcherson, S.R.; McDowell, B.R.; Howard, M.P. Acoustic effects of non-transparent and transparent face coverings. J. Acoust. Soc. Am. 2021, 149, 2249–2254. [Google Scholar] [CrossRef]
- Tiippana, K. What is the McGurk effect? Front. Psychol. 2014, 5, 725. [Google Scholar] [CrossRef] [PubMed]
- Chládková, K.; Podlipský, V.J.; Nudga, N.; Šimáčková, Š. The McGurk effect in the time of pandemic: Age-dependent adaptation to an environmental loss of visual speech cues. Psychon. Bull. Rev. 2021, 28, 992–1002. [Google Scholar] [CrossRef] [PubMed]
- Ciociano, N.; Bagnasco, L. Look alike/sound alike drugs: A literature review on causes and solutions. Pharm. Weekbl. 2014, 36, 233–242. [Google Scholar] [CrossRef]
- Hicks, R.; Becker, S.; Cousins, D. Medmarx Data Report: A Report on the Relationship of Drug Names and Medication Errors in Response to the Institute of Medicines Call for Action; US Pharmacopedia: Rockville, MD, USA, 2008. Available online: https://psnet.ahrq.gov/issue/medmarx-data-report-report-relationship-drug-names-and-medication-errors-response-institute (accessed on 1 December 2024).
- Shaw, C.A.; Lee, K.R.; Williams, A.; Shaw, N.A.; Weeks, D.; Jackson, L.; Williams, K.N. Best practices for communication while wearing facemasks: A scoping review. J. Nurs. Scholarsh. 2024, 56, 227–238. [Google Scholar] [CrossRef]
- Schlosser, M.M.; Adao, K.B.; Derkyi, A.M.; Fitzgerald-Monroe, A.M.; Ebenezer, L.B.; Eckes, E.M. Communication Challenges in High-Containment Clinical Environments. AJN Am. J. Nurs. 2021, 121, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Knollman-Porter, K.; Burshnic, V.L. Optimizing Effective Communication While Wearing a Mask During the COVID-19 Pandemic. J. Gerontol. Nurs. 2020, 46, 7–11. [Google Scholar] [CrossRef]
- Jarvis, M.A.; Smith, L. Distanced behind the mask: The use of non-verbal communication when counselling the elderly during the COVID-19 pandemic. Health SA Gesondheid 2021, 26. [Google Scholar] [CrossRef]
- Carter, L. Face masks: Be aware of the barriers. Nurs. Stand. 2020, 35, 57–58. [Google Scholar] [CrossRef]


| Gender | Age | ||||||
|---|---|---|---|---|---|---|---|
| Mean | Median | Mode | ST | Max | Min | ||
| Women | 16 (69.6%) | 24.9 | 21.5 | 21 | 7.92 | 47 | 21 |
| Men | 7 (30.4%) | 26.1 | 24 | 22 | 6.04 | 37 | 21 |
| 1 m | 2 m | 5 m | MEAN | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WM | SM | FFP2 | PAPR | WM | SM | FFP2 | PAPR | WM | SM | FFP2 | PAPR | |
| 0.65 | 0.65 | 1.38 | 1.34 | 1.34 | 1.17 | 1.32 | 0.66 | 1.13 | 1.63 | 1.69 | 1.18 | 1.18 |
| Distance: 1M | ||||||||
|---|---|---|---|---|---|---|---|---|
| WM | SM | FFP2 | PAPR | |||||
| % Intell. | Without Noise | With Noise | Without Noise | With Noise | Without Noise | With Noise | Without Noise | With Noise |
| Excellent | 18 (79.3%) | 7 (30.4%) | 15 (65.2%) | 4 (17.3%) | 16 (69.6%) | 0 | 8 (34.8%) | 0 |
| Good | 5 (21.7%) | 12 (52.2%) | 8 (34.8%) | 15 (65.2%) | 7 (30.4%) | 11 (47.8%) | 12 (52.2%) | 4 (17.4%) |
| Regular | 0 | 4 (17.4%) | 0 | 4 (17.4%) | 0 | 8 (34.8%) | 3 (13%) | 12 (52.2%) |
| Poor | 0 | 0 | 0 | 0 | 0 | 4 (17.4%) | 0 | 7 (30.4%) |
| Bad | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Very Bad | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Distance: 2M | ||||||||
| % Intell. | Without Noise | With Noise | Without Noise | With Noise | Without Noise | With Noise | Without Noise | With Noise |
| Excellent | 14 (60.8%) | 2 (8.7%) | 11 (47.8%) | 0 | 7 (30.4%) | 0 | 0 | 0 |
| Good | 9 (39.2%) | 13 (56.5%) | 12 (52.2%) | 11 (47.8%) | 11(47.8%) | 3 (13%) | 11 (47.8%) | 4 (17.4%) |
| Regular | 0 | 4 (17.4%) | 0 | 8 (34.8%) | 5 (21.7%) | 12 (52.2%) | 6 (26.1%) | 8 (34.8%) |
| Poor | 0 | 4 (17.4%) | 0 | 4 (17.4%) | 0 | 8 (34.8%) | 6 (26.1%) | 8 (34.8%) |
| Bad | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 (13%) |
| Very Bad | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Distance: 5M | ||||||||
| % Intell. | Without Noise | With Noise | Without Noise | With Noise | Without Noise | With Noise | Without Noise | With Noise |
| Excellent | 15 (66.2%) | 4 (17.4%) | 3 (13%) | 0 | 5 (21.7%) | 0 | 0 | 0 |
| Good | 4 (17.4%) | 4 (17.4%) | 16 (69.5%) | 3 (13%) | 10 (43.5%) | 0 | 0 | 0 |
| Regular | 4 (17.4%) | 11 (47.8%) | 4 (17.4%) | 4 (17.4%) | 8 (34.8%) | 8 (34.8%) | 12 (52.2%) | 0 |
| Poor | 0 | 4 (17.4%) | 0 | 12 (52.2%) | 0 | 11 (47.8%) | 8 (34.8%) | 12 (52.2%) |
| Bad | 0 | 0 | 0 | 4 (17.4%) | 0 | 4 (17.4%) | 3 (13%) | 4 (17.4%) |
| Very Bad | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 (30.4%) |
| No Mask | ||||||
|---|---|---|---|---|---|---|
| 1M | 2M | 5M | ||||
| % Intell. | Without Noise | With Noise | Without Noise | With Noise | Without Noise | With Noise |
| Excellent | 18 (78.3%) | 7 (30.4%) | 14 (60.9%) | 2 (8.7%) | 15 (65.2%) | 4 (17.4%) |
| Good | 5 (21.7%) | 12 (52.2%) | 9 (39.1%) | 13 (56.5%) | 4 (17.4%) | 4 (17.4%) |
| Regular | 0 | 4 (17.4%) | 0 | 4 (17.4%) | 4 (17.4%) | 11 (37.8%) |
| Poor | 0 | 0 | 0 | 4 (17.4%) | 0 | 4 (17.4%) |
| Bad | 0 | 0 | 0 | 0 | 0 | 0 |
| Very Bad | 0 | 0 | 0 | 0 | 0 | 0 |
| Surgical Mask. | ||||||
| % Intell. | Without Noise | With Noise | Without Noise | With Noise | Without Noise | With Noise |
| Excellent | 15 (65.2%) | 4 (17.4%) | 11 (47.8%) | 0 | 3 (13%) | 0 |
| Good | 8 (34.8%) | 15 (65.2%) | 12 (52.2%) | 11 (47.8%) | 16 (69.5%) | 3 (13%) |
| Regular | 0 | 4 (17.4%) | 0 | 8 (34.8%) | 4 (17.4%) | 4 (17.4%) |
| Poor | 0 | 0 | 0 | 4 (17.4%) | 0 | 12 52.2%) |
| Bad | 0 | 0 | 0 | 0 | 0 | 4 (17.4%) |
| Very Bad | 0 | 0 | 0 | 0 | 0 | 0 |
| FFP2 | ||||||
| % Intell. | Without Noise | With Noise | Without Noise | With Noise | Without Noise | With Noise |
| Excellent | 16 (69.6%) | 0 | 7 (30.4%) | 0 | 5 (21.7%) | 0 |
| Good | 7 (30.4%) | 11 (48.8%) | 11 (48.8%) | 3 (13%) | 10 (43.5%) | 0 |
| Regular | 0 | 8 (34.7%) | 5 (21.7%) | 12 (52.2%) | 8 (34.7%) | 8 (34.7%) |
| Poor | 0 | 4 (17.4%) | 0 | 8 (34.7%) | 0 | 11 (48.8%) |
| Bad | 0 | 0 | 0 | 0 | 0 | 4 (17.4%) |
| Very Bad | 0 | 0 | 0 | 0 | 0 | 0 |
| PAPR. | ||||||
| % Intell. | Without Noise | With Noise | Without Noise | With Noise | Without Noise | With Noise |
| Excellent | 8 (34.8%) | 0 | 0 | 0 | 0 | 0 |
| Good | 12 (52.2%) | 4 (17.4%) | 11 (47.8%) | 4 (17.4%) | 0 | 0 |
| Regular | 3 (13%) | 12 (52.2%) | 6 (26.1%) | 8 (34.8%) | 12 (52.2%) | 0 |
| Poor | 0 | 7 (30.4%) | 6 (26.1%) | 8 (34.8%) | 8 (34.8%) | 12 (52.2%) |
| Bad | 0 | 0 | 0 | 3 (13%) | 3 (13%) | 4 (17.4%) |
| Very Bad | 0 | 0 | 0 | 0 | 0 | 7 (30.4%) |
| Without Ambient Sound Added; Noise Level <25 dB(A) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1M | 2M | 5M | ||||||||||
| % Intell. | WM | SM | FFP2 | PAPR | WM | SM | FFP2 | PAPR | WM | SM | FFP2 | PAPR |
| Excellent | 18 (78.3%) | 15 (65.2%) | 16 (69.5%) | 8 (34.8%) | 14 (60.9%) | 11 (47.8%) | 7 (30.4%) | 0 | 15 (65.2%) | 3 (13%) | 5 (21.7%) | 0 |
| Good | 5 (21.7%) | 8 (34.8%) | 7 (30.4%) | 12 (52.2%) | 9 (39.1%) | 12 (52.2%) | 11 (47.8%) | 11 (47.8%) | 4 (17.4%) | 16 (69.5%) | 10 (43.5%) | 0 |
| Regular | 0 | 0 | 0 | 3 (13%) | 0 | 0 | 5 (21.7%) | 6 (26.1%) | 4 (17.4%) | 4 (17.4%) | 8 (34.8%) | 12 (52.2%) |
| Poor | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 (26.1%) | 0 | 0 | 0 | 8 (34.8%) |
| Bad | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 (13%) |
| Very Bad | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| With ambient sound added; Noise level < 45 dB(A) | ||||||||||||
| % Intell. | WM | SM | FFP2 | PAPR | WM | SM | FFP2 | PAPR | WM | SM | FFP2 | PAPR |
| Excellent | 7 (30.4%) | 4 (17.4%) | 0 | 0 | 2 (8.7%) | 0 | 0 | 0 | 4 (17.4%) | 0 | 0 | 0 |
| Good | 12 (52.2%) | 15 (65.2%) | 11 (47.8%) | 4 (17.4%) | 13 (56.5%) | 11 (47.8%) | 3 (13%) | 4 (17.4%) | 4 (17.4%) | 3 (13%) | 0 | 0 |
| Regular | 4 (17.4%) | 4 (17.4%) | 8 (34.8%) | 12 (52.2%) | 4 (17.4%) | 8 (34.8%) | 12 (52.2%) | 8 (34.8%) | 11 (47.8%) | 4 (17.4%) | 8 (34.8%) | 0 |
| Poor | 4 (17.4%) | 7 (30.%) | 4 (17.4%) | 4 (17.4%) | 8 (34.8%) | 8 (34.8%) | 4 (17.4%) | 12 (52.2%) | 11 (47.8%) | 12 (52.2%) | ||
| Bad | 3 (13%) | 4 (17.4%) | 4 (17.4%) | 4 (17.4%) | ||||||||
| Very Bad | 7 (30.4%) | |||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rojo-Rojo, A.; Martínez-Abril, J.E.; Muñoz-Rubio, G.M.; Iniesta-Cortés, P.; Cánovas-Pallarés, J.M. Effects of Distance, Noise, and Personal Respiratory Protective Equipment on Speech Comprehension in Simulated Critical Care Setting. Healthcare 2025, 13, 398. https://doi.org/10.3390/healthcare13040398
Rojo-Rojo A, Martínez-Abril JE, Muñoz-Rubio GM, Iniesta-Cortés P, Cánovas-Pallarés JM. Effects of Distance, Noise, and Personal Respiratory Protective Equipment on Speech Comprehension in Simulated Critical Care Setting. Healthcare. 2025; 13(4):398. https://doi.org/10.3390/healthcare13040398
Chicago/Turabian StyleRojo-Rojo, Andrés, José Eugenio Martínez-Abril, Gloria María Muñoz-Rubio, Paloma Iniesta-Cortés, and Juan Manuel Cánovas-Pallarés. 2025. "Effects of Distance, Noise, and Personal Respiratory Protective Equipment on Speech Comprehension in Simulated Critical Care Setting" Healthcare 13, no. 4: 398. https://doi.org/10.3390/healthcare13040398
APA StyleRojo-Rojo, A., Martínez-Abril, J. E., Muñoz-Rubio, G. M., Iniesta-Cortés, P., & Cánovas-Pallarés, J. M. (2025). Effects of Distance, Noise, and Personal Respiratory Protective Equipment on Speech Comprehension in Simulated Critical Care Setting. Healthcare, 13(4), 398. https://doi.org/10.3390/healthcare13040398






