Abstract
Background and Objectives: In-toeing and out-toeing gait are rotational deformities commonly observed in children with neuromuscular conditions. These gait abnormalities often result from internal tibial torsion, increased femoral anteversion, and metatarsus adductus. This study was conducted to create a comprehensive evaluation of the effectiveness of lower extremity orthotics as a non-operative treatment option, given their regular use in clinical settings. The aim of this literature review was to understand the efficacy of various orthotic devices in correcting rotational deformities in the transverse plane, thereby improving ambulation stability and 3D joint motion. Materials and Methods: Literature published after 1 January 1990 was reviewed, utilizing databases such as CENTRAL (Wiley), CINAHL (EBSCO), Medline (OVID), Scopus (Elsevier), and Web of Science (Clarivate). In totality, 13 studies were included, evaluating 365 participants with neuromuscular conditions using various orthotic devices. Results: Among these studies, two were randomized control trials (Level 1), nine were quasi-experimental studies (Level 2), and two were case studies (Level 4). Quality assessment determined that 69% of the included studies had a low risk of bias, while 31% demonstrated a moderate risk. Compression garments and rotational systems showcased the greatest change in proximal lower extremity rotation at 19.73° ± 1.57 and 24.13° ± 8.49, respectively. The most significant difference in foot progression angle is through the use of rotational systems, 19° ± 26.87. Conclusions: In a short-term treatment, children with neuromuscular disorders exhibiting in-toeing or out-toeing gait may benefit from different types of orthoses. Compression garments may aid joint alignment and enhance proprioception, rotational systems correct alignment with precise adjustability, AFOs that achieve effective stabilization can deliver benefits in the transverse plane, and foot orthotics may be appropriate for mild gait abnormality management.
1. Introduction
In-toeing and out-toeing are gait abnormalities commonly seen in pediatric populations [1,2]. They are characterized as rotational abnormalities resulting in an inappropriately rotated foot, with in-toeing being described as a unilateral or bilateral internal rotation of the longitudinal axis of the foot compared to the line of progression, as opposed to out-toeing consisting of external rotation [1,2]. These rotational deformities are clinical symptoms arising from an underlying anatomic or functional dysfunction consisting of range of movement, neurological, and static skeletal disorders [1,2]. Three primary deformities that lead to in-toeing include tibial torsion, metatarsus adductus, and femoral anteversion [3,4]. In comparison, the primary deformities in out-toeing gait include pelvic external rotation, hip external rotation, or external tibial torsion [1]. In these deformities, femoral anteversion refers to a deviated angle between the femoral neck and the femoral shaft caused by forward torsion of the femoral neck [5], whereas tibial torsion describes the twisting of the tibia either internally or externally [6,7]. Both femoral anteversion and tibial deformities may lead to increased internal rotation and muscle activation at the hip and knee [8,9,10,11]. If these deformities are left unaddressed, they may persist and worsen into adulthood, potentially leading to excessive subtalar joint rotation [12], hip joint arthritis [13], and patellofemoral injuries [13].
Some causes of in-toeing and out-toeing gait abnormalities are linked with conditions such as cerebral palsy and spina bifida [14,15,16]. These neuromuscular disorders can affect bone growth and orientation, muscle strength and tone, and movement coordination, creating an in-toeing or out-toeing gait [17,18]. These patients may also exhibit joint laxity, muscle imbalances, hip dislocations, knee or foot deformities, and are often prone to in-toeing gait patterns [19,20].
To effectively manage these abnormal rotations, the site of deformity must be accurately diagnosed by assessing the hip’s internal and external rotation, foot progression angle (FPA) [1,21], thigh–foot angle (TFA) [22,23], foot shape, and the transmalleolar axis (TMA) [23,24] in the knee-flexed position [25]. FPA is considered as one of commonly used standard parameters to diagnose abnormal gait. This quantitative measurement system allows clinicians to quantify motion and characterize these pathologies [26]. Unlike femoral anteversion and tibial torsion, which focus on the femur and tibia specifically, FPA is a measurement of the entire lower extremity chain presenting a summative description of rotational deformities [26]. Along with long-term consequences of arthritis and lower extremity instability [12,13], these deformities can lead to increased pain in the future, as supported by a retrospective study which identified 43 out of 50 children with increased internal hip rotation reporting pain on physical examination [21]. Depending on the level of the lower extremity affected, it can impact the adjacent musculature and result in rotational forces pulling joint alignment into an internal rotation, causing in-toeing and the need to compensate with other structures [26].
Conservative treatment options such as orthotics have proven capable of correcting misalignments and abnormal gait patterns [27,28,29]. This is accomplished through providing stability of movement and support of joints or muscles, reducing the muscle spasticity and energy for ambulation, and improving the quality of life. Currently, there are limited literature reviews that have been published on comparing multiple orthotic treatments for children with neuromuscular conditions and in-toeing or out-toeing gait. There remains a lack of comprehensive reviews that evaluate multiple orthotic types together, including TheraTogs, twister cables (TCs), twister wrap orthoses (TWOs), TheraSuits, compression garments, ankle and foot orthoses (AFOs), and foot orthoses (FOs). A recent debate has focused on the role of plantar orthotics, which have shown efficacy in reducing musculoskeletal stress and improving distal weakness in the lower extremities through redistributing plantar pressure and maintaining correct alignment, allowing for improved gait stability [30,31,32]. Given the potential for long-term complications, continued debate on orthotic efficacy, and the wide range of orthotic options available, a thorough review and comparison of the efficacy of these orthotic devices is essential for effective clinical decision making and crucial to comprehensively evaluate their impact on gait abnormalities, particularly concerning transverse plane rotation.
The goal of this study is three-fold: (1) to compare the efficacy and clinical findings of various orthotic devices in patients with in-toeing or out-toeing gait deformities; (2) to compare different orthotic influences on 3D kinematics and kinetics of the lower extremity, especially on the transverse plane movements; (3) to assess the demographic data and the quality of life for children using each orthotic.
2. Materials and Methods
2.1. Protocol and Registration
The study protocol was registered on Open Science Framework (osf.io) at https://osf.io/ecqm2/, accessed on 22 April 2024. (Registration Information: The literature review was registered to an open access platform at Open Science Framework (OSF)).
2.2. Search Strategy
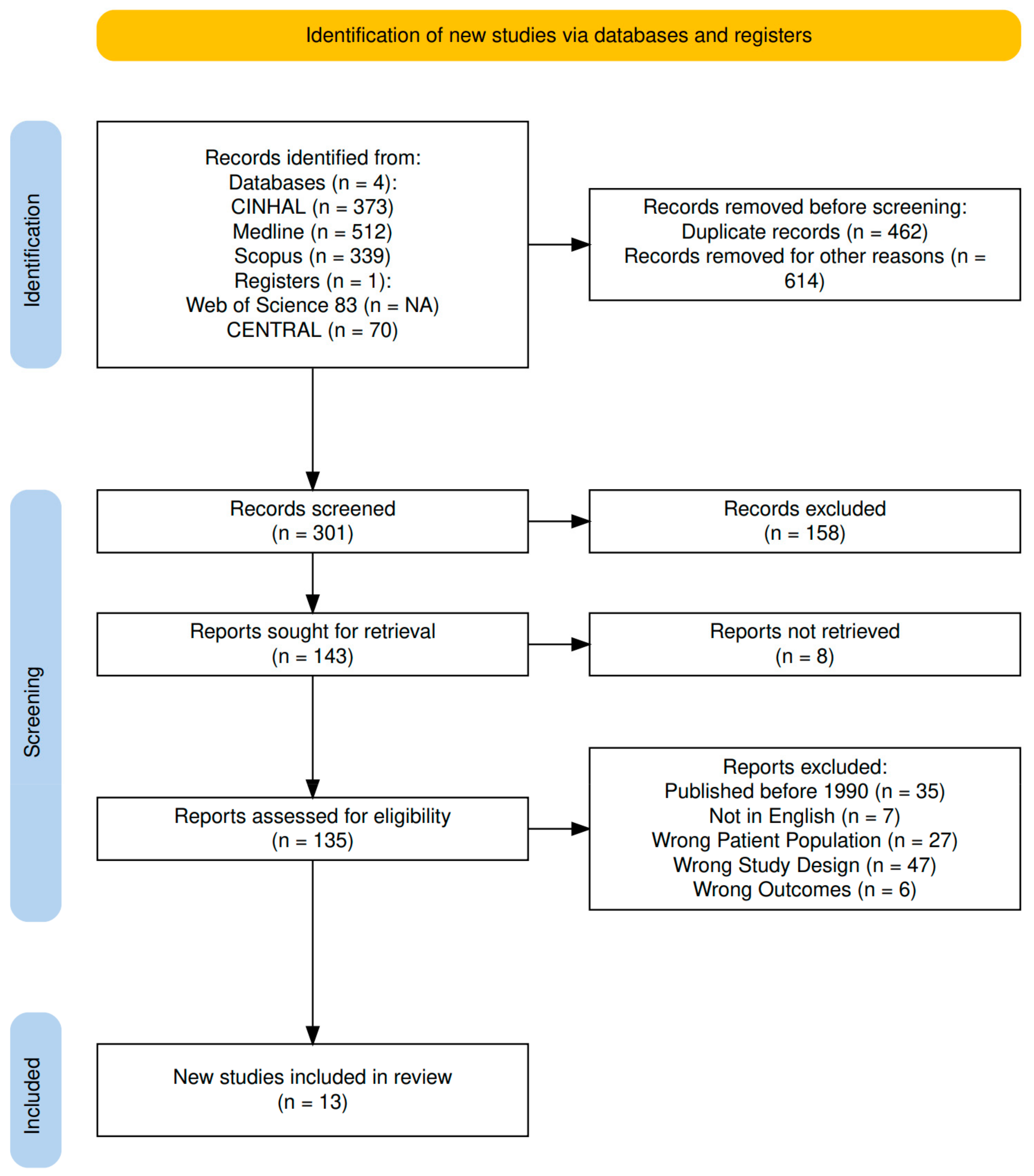
The current review was conducted on 29 May 2024 through using the following databases to find scientific articles: CENTRAL (Wiley) (Hoboken, NJ, USA), CINAHL (EBSCO) (Ipswich, MA, USA), Medline (OVID) (Norwood, MA, USA), Scopus (Elsevier) (Amsterdam, Netherlands), and Web of Science (Clarivate) (London, United Kingdom), which is outlined in Figure 1. In Ovid Medline, we used MeSH terms and free text terms related to neuromuscular diseases, neurologic gait disorders, orthotic devices, and the pediatric population. The complete search strategy is included in Table A1 in Appendix A.
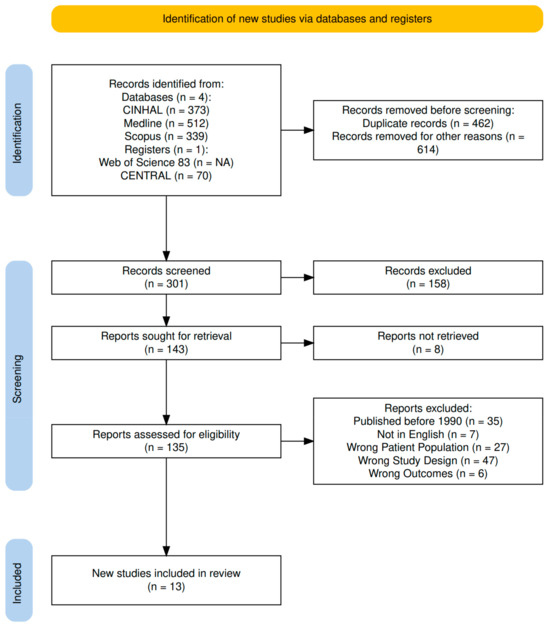
Figure 1.
PRISMA flow chart.
2.3. Eligibility Criteria
This study’s inclusion criteria focused on children with neuromuscular conditions, such as cerebral palsy and spina bifida, who present with an in-toeing or out-toeing rotational deformity. Individuals without neuromuscular conditions causing rotational deformities and aged 18 years and older were excluded. Studies that have used orthotic devices to correct lower extremity rotational deformities were chosen to be included. The inclusion criteria are based on the articles discussing one or more of the following key phrases: “in-toeing”, “out-toeing”, “neuromuscular conditions”, “transverse plane”, “rotational deformities”, “cerebral palsy”, “spina bifida”, “rehabilitation devices”, “assisted devices”, “TheraTogs”, “Twister Cables” (TC), “Tibia Counter Rotator” (TCR), “Twister Wrap Orthoses” (TWO), “compression garments”, “therasuit”, “lycra garment”, “compression leggings”, “AdeliSuit”, “Dynamic Elastomeric Fabric Orthoses” (DEFO), “Hinged Ankle Foot Orthosis” (HAFO), “Solid Ankle Foot Orthosis” (SAFO), “Supramalleolar orthosis” (SMO), “ankle foot orthosis” (AFO), and “Static Ground Reaction Ankle Foot Orthoses” (sgrAFO). Studies that have not described the listed types of orthotics, did not discuss the transverse plane or rotational deformities, or were published before January 1st, 1990, were excluded. Additionally, any unclear data relating to the variables in the inclusion criteria were not included. The comparisons of the included studies must involve different orthotic treatments or be comparisons between barefoot ambulation or baseline interventions such as physical therapy. The main outcomes of interest include changes in internal and external rotations in 3D kinematics and changes in FPA.
2.4. Study Screening
The article selection process began by removing duplicates, followed by title screening and eventually abstracts and full texts of the remaining studies, using the review software Rayyan (https://www.rayyan.ai/) (accessed on 29 May 2024) (Cambridge, MA, USA). For each synthesis, the intervention characteristics of the studies were tabulated and compared against the pre-defined inclusion criteria: (1) the type of orthotic intervention (TC, TWO, AFO, garment, etc.); (2) study population with gait disorder (e.g., children with in-toeing or out-toeing gait); (3) outcome measures (e.g., spatio-temporal data, foot progression angle, and 3D joint kinematics); (4) age from starting to walk to 18 years old. Studies that met these criteria were included in the synthesis. Articles were reviewed by two independent reviewers, who were blinded to each other’s decisions. Conflicts regarding inclusion or exclusion were resolved by a third reviewer. Exclusion criteria include: (1) age >18 years old; (2) post-surgery with soft tissue or bone osteotomy or spine; (3) no orthotics. A risk of bias assessment for the included studies was conducted.
2.5. Data Collection
One author extracted the critical data from each article to allow a comparison of the interventions. These key data included the study design, type of intervention, subject characteristics (number of participants, neuromuscular condition), spatio-temporal data, and gait analysis data such as FPA outcomes and 3D joint kinematics, focusing on the transverse plane. The changes in internal/external rotation and FPA were gathered from multiple clinical studies (Table 1, Table 2, Table 3, Table 4, Table 5, Table 6 and Table 7). The findings from each clinical study regarding changes in the transverse plane were compared and depicted for each orthotic category: compression garment [19,33,34,35,36], rotational systems [20,37], ankle and foot orthotics [38,39,40], and insole and wedges [13,41,42] (Table 6). A similar process was accomplished in comparing the average FPA between all four orthotic categories (Table 7).

Table 1.
Summary of the interventions of all included articles.

Table 2.
Summary of clinical studies on compression garments for gait correction in neuromuscular conditions.

Table 3.
Summary of clinical studies on rotation systems for gait correction in neuromuscular conditions.

Table 4.
Summary of clinical studies on ankle and foot orthotics for gait correction in neuromuscular conditions.

Table 5.
Summary of clinical studies on insoles and wedges for gait correction in neuromuscular conditions.

Table 6.
Changes in Hip and Knee Rotation in the transverse plane of different orthotic categories (mean ± SD) [20,35,37].

Table 7.
Comparing FPA improvement of different orthotic categories (mean ± SD) [13,20,33,40,41,42].
2.6. Quality Assessment
The level of evidence was assigned to each article based on the hierarchy outlined by Burns et al. in their 2011 study [43]. Two reviewers (HB, CW) evaluated all included studies independently. Inconsistencies were shown to a third reviewer (JK) for the final decision.
The Cochrane Collaboration “risk of bias” tool was used to evaluate the included randomized control trial studies [44], which included the following: sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessors; incomplete outcome data; selective outcome reporting; and other biases. Each item was rated as unclear, low risk, or high risk of bias. We did not exclude any studies for methodological quality.
For the quasi-experimental studies, the Risk of Bias In Non-randomized Studies of Interventions (ROBINS-I) tool [45] was used to assess bias across the following domains: confounding; participant selection; classification of interventions; deviations from intended interventions; missing data; measurement of outcomes; and selection of the reported result. Each domain was rated as low risk, moderate risk, serious risk, critical risk, or no information to reflect the risk of bias in non-randomized studies. We did not exclude any studies for methodological quality.
Additionally, the Joanna Briggs Institute Critical Appraisal Checklist was used to assess case series and case studies [46], examining the inclusion criteria; clear description of the participants; measurement of outcomes; appropriate statistical analysis; and clear reporting of findings. Each item was assessed for potential bias in reporting and reliability.
2.7. Outcome Measures
Among the included clinical studies, children of ages 2 to 15 years old had various neuromuscular conditions, such as diplegic and hemiplegic cerebral palsy, spina bifida, Duchenne muscular dystrophy, and Down syndrome. The types of orthotics that were investigated include rotational systems such as twister cables, compression garments such as TheraTogs and Lycra garments, various forms of ankle and foot orthotics (AFO, HAFO, SAFO), and insole and wedges. The outcomes that were analyzed include changes in the FPA [47] and 3D joint kinematics [48], specifically focusing on the transverse plane. For each outcome across different orthotic systems, the mean differences between subject age, FPA, and 3D joint kinematics were used as effect measures in the synthesis and presentation of results.
2.8. Statistical Analysis
Differences among the FPA and 3D joint kinematics from the included studies were compared among the different types of orthotics. Statistical analyses for combining means and standard deviations from the individual studies were performed using R version 4.3.2 (R Foundation for Statistical Computing). To ensure the accuracy of the analysis, the original sample sizes, means, and standard deviations for each study were carefully extracted from the corresponding published reports. These data were then aggregated using the methods suggested by Higgins et al. (2019) [49], which provide robust formulas for synthesizing summary statistics across studies. Specifically, weighted means and pooled standard deviations were calculated, considering the sample sizes and variability of each study. These comparisons are shown in Table 6 and Table 7, providing a general comparison between kinematic findings.
3. Results
3.1. Search Strategy
The initial search gathered 1299 articles, of which 462 were duplicates. Then, 301 articles were examined by reviewers. Thirteen studies were included, evaluating 365 participants with neuromuscular conditions, including diplegic and hemiplegic cerebral palsy, spina bifida, myelomeningocele, Duchenne muscular dystrophy, and Down syndrome (Figure 1). All 13 studies were based on pediatric patient populations. Institutional access through Medical College of Wisconsin libraries was used to access all articles.
3.2. Study Quality
This literature review included 13 clinical studies. Of the 13 studies analyzed, 15% were Level 1, 69% were Level 2, 15% were Level 4. Collectively, two were randomized control trials, nine were quasi-experimental studies, five were case–control studies, and two were case studies. Regarding the risk of bias, 69% of the studies had a low risk of bias, and 31% of the studies had a moderate risk of bias.
3.3. Types of Orthotics and Their Impacts
The orthotics mentioned in the tables include TheraTogs [19,20,35], SMOs [38,39], high-top shoes [33], TWOs [33], other 3D supporting garments [34,36], medial-wedge insoles [41] (MWI), DEFOs [50], a custom-made TCR [37], shoe wedges [12,13,34,38,39,41,42], TCs [20], general AFOs [51,52], and specific AFOs such as sgrAFOs [19], HAFOs [38], and SAFOs [38,53].
The orthotics were grouped into four categories: compression garments (Table 2), rotational systems (Table 3), AFOs (Table 4), and insoles and wedges (Table 5). Table 6 depicts the changes in hip and knee rotation in the transverse plane. Compression garments show a notable improvement in hip rotation with a combined mean of 19.73 degrees and a standard deviation of 1.57. However, no data were available for statistical analysis for knee rotation using compression garments. In contrast, rotational systems showed improvements in both hip rotation with a change in mean of 8.5 degrees and knee rotation with a change in mean of 24.13, although no standard deviations were able to be reported. Additionally, Table 7 illustrates changes in FPA in the transverse plane for all four orthotic groups. Rotational systems depicted the largest FPA improvement of 19 degrees, but with high variability with a standard deviation of 26.87 degrees. Compression garments showed the smallest change in FPA of 4.86. Insoles and wedges demonstrated a moderate FPA of 13.95 degrees with a high degree of variability. Ankle and foot orthotics depicted no improvement in FPA.
4. Discussion
The present literature review aimed to examine the effects of different orthotic types on changes in the transverse plane among patients with neuromuscular conditions. Of the included articles, 38% (5/13) discussed the impact of compression garments on the transverse plane [19,33,34,35,36]. These studies provide a strong evidence base suggesting that compression garments, such as TheraTogs, can improve knee alignment, allowing for enhanced muscle recruitment at the hip joint in the swing phase and rotation of the leg for improved FPA. These findings complement a study by Flanagan that underscored a 76% increase in balance after TheraTogs intervention [35] and a study by Emara assessing the quality of life and functional independence with TheraTogs use [54]. Similar to findings by Degelean [34], their results showcase how improved internal and external rotation can strengthen joint stability, increase mobility, and decrease pain and fall rates. This is supported by a study by Schelhaas et al. which observed a 4.4° decrease in out-toeing with TheraTogs intervention, indicating a marked improvement in FPA [55].
Of the studies discussing compression garments, 2/5 compared compression garments with the addition of AFOs or high-top shoes [19,33]. Abd El-Kafy also highlighted no significant differences between bilateral hip and knee rotational angles between TheraTogs and “TheraTogs + static ground reaction AFOs” conditions before and after treatment. Since AFOs are understood to increase stability of the ankle in the coronal plane, this explains how significant changes in the transverse plane, affected by TheraTogs, remain the primary contributing factor to the improvement of in-toeing or out-toeing symptoms. Davoudi et al. (2022) [33] demonstrated that in children with diplegic cerebral palsy, the use of high-top shoes combined with TWO significantly reduced center pressure sway in both anterior–posterior and medial–lateral directions, thus enhancing balance and correcting transverse plane misalignment through femoral de-rotation. This correction notably improved hip internal rotation control, thus potentially enhancing motor functionality and reducing fall risk. A randomized controlled trial by Emara et al. [56] supports these findings through showing how corrected foot pressure distribution was more significant in TheraTogs use compared to conventional physical-therapy-corrected foot pressure distribution.
Other variations, such as Lycra garments, provide dispersed pressure that improves muscle activation and proprioception by applying external force vectors to counteract internal rotation at the hip, knee, and ankle levels as depicted in Rennie et al. [36]. Correspondingly, Kim et al. [50] found an 8–9° improvement in hip rotation in the transverse plane, while Cunha et al. [57] noted enhanced proprioceptive feedback through pressure receptors, facilitating targeted muscle activation. Rennie’s study further highlighted how Lycra garments lacked sufficient foot and ankle support, which may limit overall joint stability. These findings suggest the importance of proper compression garment wrapping of the entire lower extremity to improve stabilization and mitigate internal and external forces. Overall, due to the versatility, muscle activation, and proprioceptive features of compression garments, they can be an optimal option for individuals with various neuromuscular conditions. The findings of the current review align with the previous studies regarding the rotational improvement at the hip joint and FPA improvement.
Fifteen percent of the included articles (2/13) discussed the impact of rotational systems on the transverse plane [20,37]. The results of these articles indicate that TCs and TCRs can be a valuable aid for children with neuromuscular disorders that result in severe traversal rotational deformities at multiple levels. Unlike compression garments, TCs and TCRs provide rigid, controllable rotational forces that enforce corrective alignment of the lower extremities [20], which may provide extensive benefit as the patient develops due to changes in musculoskeletal structures and joint forces. TCs consist of cables and straps that attach to a brace or shoe and provide correction at the femur and tibia. In contrast, the TCR acts as a splint, providing isolated rotational correction at the knee joint and tibia [20]. Both orthotic devices showed statistical significance in improving internal rotation. TCs have demonstrated improved hip rotation by providing external changes of 23° on the left lower extremity and 25° on the right lower extremity, along with enhanced external rotation in the FPA with 30° on the left lower extremity and 13° on the right lower extremity [20]. In comparison, the TCR was shown to be effective as an initial treatment option for internal tibial torsion [37]. Compared to TheraTogs, TCs had decreased improvements with hip external rotation but greater overall FPA improvement [20]. Our analysis reported that rotational systems have a greater impact on reducing the FPA compared to compression garments (See Table 7). TheraTogs may be more beneficial for patients with hip internal rotation, as the external forces at the hip can decrease knee stress and prevent future complications that may include knee arthritis and ligament instability [20]. Alternatively, TCs or TCRs may be better indicated for patients who require precise correction at multiple joints including the hip and knee rather than the pelvis [20]. Similarly, our analysis demonstrates how rotational systems influenced both hip and knee levels of the lower extremity, as compared to compression garments that only influenced the hip (see Table 6).
Although TCs can provide rotational changes at multiple joints due to the structure and attachment points of the orthotic, a patient satisfaction survey exhibited a preference for TheraTogs over TCs [20,36]. This partiality may be attributed to the considerable size of TCs compared to TheraTogs, which may impact the child’s willingness to wear the orthotic for long periods of time [20]. While the TCR provides a mild improvement in the transverse plane of the knee with a 5° improvement in the right leg and 0° in the left leg, unlike TCs, the TCR allows for independent movement of both legs [37]. TCRs may be a more suitable treatment for patients with tibial torsion who cannot wear TCs for long periods. However, findings in Richards et al. are similar to those in Rennie et al. as parents in the study highlighted their children’s challenges with using the restroom and chafing near joint lines [36]. Even with Rennie et al.’s study showing a moderate risk of bias, these investigations show that both garments and rotational systems can prove uncomfortable and demonstrate minimal effectiveness if the individual is unwilling to use them consistently.
Twenty-three percent of the included articles (3/13) discussed the impact of AFOs on the transverse plane [38,39,40]. The results of these articles indicate conflicting findings surrounding the utility of this class of orthotics. One study found AFOs introduced further internal rotation by 7 degrees [40]. Some findings suggests that tibial torsion shoes with either AFOs or SMOs failed to demonstrate significant correlations with gait parameters [39]. Other literature on these orthotics has demonstrated increased and varied transverse motion, such as at the knee joint [52] and increased external tibial torsion, leading to decreased knee extension mobility [53,58,59]. The sgrAFO showed no statistically significant differences in bilateral hip and knee angles between groups treated with TheraTogs versus “TheraTogs and sgrAFO” [19]. It supports the limited benefit of AFOs for pathologies affecting the transverse plane [19]. Both Carmick et al. [38] and Fatone et al. [58] observed the utility of AFOs, including SAFOs, HAFOs, and SMOs, highlighting the importance of proper alignment of the mechanical joint axis. Specifically, Carmick et al. discusses the need for a neutral subtalar joint (STJ) position for beneficial ambulation outcomes. They argue that having a neutral STJ will lead to proper biomechanical alignment of the hip, knee, and ankle, leading to reduced gait abnormalities. As compared to both compression garments and rotational systems, our study shows that AFOs have no impact on FPA (see Table 7).
Twenty-three percent of the included articles (3/13) discussed the impact of foot orthotics on the transverse plane [13,41,42]. The results of all three studies show significant improvement in FPA. For example, Munuera et al. [13] found a 5.30° improvement in the FPA in patients with in-toeing. However, there is conflicting evidence on the impact of insoles and wedges on femoral anteversion. A study by Ganjehie et al. found that gait plate insoles increased FPA between foot longitudinal axis and the center of pressure in the anterior–posterior direction in children with femoral anteversion [12]. Contrastingly, a randomized control trial by Parian et al. found that children suffering from excessive femoral anteversion experienced no statistically significant difference in FPA during the first four weeks of using the orthotic [42]. Due to confounding variables, these differences may be attributed to the time of usage for the orthotic.
Compliance and comfortability are major factors for clinicians to take into account when prescribing orthotics. The prescribed orthotic may be beneficial in correcting malalignment; however, if it consistently causes discomfort and the child becomes averse to treatment compliance, then the efficacy of the orthotic will be limited. A parental satisfaction survey in Richards et al. [20] found that parents reported higher satisfaction with TheraTogs in regard to comfortability (rated 1 for strongly agree), improved balance (rated 1 for strongly agree), and child’s willing to wear the garment all day in comparison to twister cables where parents rated a 5 for strongly disagree. Although twister cables may be more effective and accurate in correcting lower extremity malalignment, without potential risks such as overcorrection, the bulkiness and weight of the orthotic may limit in treatment success, especially in younger children, regarding the compliance of the patient [60,61]. A potential method to mitigate non-compliance may to be design custom-fit orthotics that limit discomfort observed in standard models [62].
In the current literature review, there are a few limitations that should be acknowledged. The heterogeneity among the included studies due to the differences in study design, evaluated orthotic, and outcomes places restrictions on performing a meta-analysis or statistical comparison between interventions. There are a limited number of studies discussing orthotics such as those in the rotational system category, limiting the data for a comprehensive comparison. Additionally, variations in patient demographics, ages, and number of participants in the included articles impact the conclusions that were drawn. The limited long-term follow-up in a majority of the studies places restrictions on drawing conclusions on the efficiency and sustainability of the orthotic intervention in transverse plane correction. Regarding the review process, reliance on published literature may have created a publication bias, as studies with significant findings are more often published. Thus, these studies may overrepresent the efficacy of these orthotic interventions in lower extremity malalignment, possibly limiting the generalizability of this study. To mitigate this for future studies, authors may conduct a systematic review on relevant literature, broaden their inclusion criteria with a greater number of orthotics, and include outcome measures, studies before 1990, or additional databases to overcome this limitation. Table 6 and Table 7 are representations of listed findings of rotational changes in the transverse plane and do not portray statistical significance.
5. Conclusions
Orthotic treatments vary widely but have a notable capacity to remediate gait abnormalities in the transverse plane and in pediatric patients suffering from neuromuscular conditions. While this study primarily focused on in-toeing and out-toeing gait, children with neuromuscular disorders often have complicated 3D movement abnormalities and different functional requirements at age-related milestones. Clinically, optimal orthotic selection is hardly indicated for sole management of the transversal plane. Comprehensive physical examination and gait analysis tools for assessing rotational deformities are imperative for physicians to provide effective orthotic treatment in these patients. This review included 13 clinical studies with the majority characterized by Level 2 evidence and offering primarily moderate certainty in conclusions. While 69% of studies had a low risk of bias, 31% were at moderate risk. Notably, 92% of included studies (12/13) demonstrated that orthoses, such as compression garments, rotational systems, as well as insoles and wedges, each improved internal or external rotation in the transverse plane. Compression garments provide benefit through joint alignment correction and proprioception enhancement. Rotational systems provide similar advantages, with the added capability of adjustability to specific degrees during treatment progression, although compliance among children remains a challenge. While AFOs and insoles or wedges present mixed evidence, achieving effective stabilization is crucial for AFOs to deliver measurable benefits in the transverse plan. Foot orthotics (FOs), conversely, may be more appropriate for managing mild gait abnormalities.
Author Contributions
Conceptualization, H.B. and X.-C.L.; methodology, H.B. and X.-C.L.; software, H.B.; validation, H.B., C.J.K.W. and J.D.K.; formal analysis, H.B.; investigation, H.B.; resources, H.B.; data curation, H.B.; writing—original draft preparation, H.B., C.J.K.W. and J.D.K.; writing—review and editing, H.B., C.J.K.W. and J.D.K.; visualization, H.B., C.J.K.W. and J.D.K.; supervision, X.-C.L.; project administration, X.-C.L. All authors have read and agreed to the published version of the manuscript.
Funding
There was no funding provided for this research.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article. Further data inquiry is available on request from the authors.
Acknowledgments
We would like to express gratitude and acknowledge Carly Schanock, MLIS, for her assistance with creating the literature search and organizing the selected articles in Covidence. Additionally, we would like to express gratitude to Kai Yang for sharing his expertise and aiding in the statistical analysis of the included articles.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| TCs | Twister Cables |
| TWOs | Twister Wrap Orthoses |
| TCR | Twister Counter Rotator |
| AFOs | Ankle Foot Orthotics |
| HAFO | Hinged Ankle Foot Orthosis |
| SAFO | Solid Ankle Foot Orthosis |
| SMO | Supramalleolar Orthosis |
| sgrAFOs | Static Ground Reaction Ankle Foot Orthoses |
| FOs | Foot Orthotics |
| FPA | Foot Progression Angle |
Appendix A

Table A1.
Search Strategies.
Table A1.
Search Strategies.
| Cochrane Registry of Clinical Trials (CENTRAL, Wiley) | ||
|---|---|---|
| No. | Search Details | No. of Articles |
| #1 | MeSH descriptor: [Neuromuscular Diseases] explode all trees | 15,188 |
| #2 | MeSH descriptor: [Gait Disorders, Neurologic] explode all trees | 991 |
| #3 | ((amyloid or “brachical plexus” or diabetic or “giant axonal” or “small fiber”) NEAR/3 neuropath*):ti,ab,kw | 4439 |
| #4 | ((“complex regional pain” or “Eosinophilia-Myalgia” or “Hand-Arm Vibration” or Issacs or “Locked in” or “medial tibial stress” or “nerve compression” or Postpoliomyelitis or “stiff person”) NEAR/3 syndrome?):ti,ab,kw | 1079 |
| #5 | ((muscular or neuromuscular or “motor neuron” or myotonic or “peripheral nervous system”) NEAR/3 (disorder? or disease?)):ti,ab,kw | 4692 |
| #6 | ((walk* or ambulation or gait) NEAR/3 (disorder? or abnormal*)):ti,ab,kw | 1929 |
| #7 | (intoeing or “in toeing” or in-toed or intoed or outtoeing or “out toeing” or outtoed or out-toed or Acrodynia or “Amyotrophic Lateral Sclerosis” or Botulism or Fibromyalgia or “Mitochondrial Myopathies” or Mononeuropathies or Myalgia or “Myasthenia Gravis” or Myositis or Myotoxicity or Neuralgia or Neuritis or “Neurofibromatosis 1” or “Peripheral Nerve Injuries” or (“Peripheral Nervous System” NEXT Neoplasm?) or Poliomyelitis or Polyneuropathies or Radiculopathy or “Tarlov Cysts”):ti,ab,kw | 21,008 |
| #8 | {OR #1–#7} | 34,175 |
| #9 | MeSH descriptor: [Orthotic Devices] explode all trees | 2422 |
| #10 | ((Orthotic or rehab* or assisted or kinesio*) NEAR/3 (brace? or device?)):ti,ab,kw | 1636 |
| #11 | (parapodium? or TheraTogs or Twister Cables or therasuit? or (lycra NEXT garment?) or AdeliSuit or HAFO or SAFO or DAFO or AFO):ti,ab,kw | 282 |
| #12 | (compress* NEAR/3 (cloth* or legging? or garment? or sock? or sleeve? or stocking? or wrap?)):ti,ab,kw | 1665 |
| #13 | ((“dynamic elastomeric fabric” or “ankle foot” or Supramalleloar or “twister wrap”) NEAR/3 ortho*):ti,ab,kw | 18 |
| #14 | {OR #9–#13} | 5138 |
| #15 | MeSH descriptor: [Pediatrics] explode all trees | 1044 |
| #16 | MeSH descriptor: [Adolescent] explode all trees | 136,839 |
| #17 | MeSH descriptor: [Child] explode all trees | 81,883 |
| #18 | MeSH descriptor: [Infant] explode all trees | 46,083 |
| #19 | (Infan* or newborn* or new-born* or perinat* or neonat* or baby or baby* or babies or toddler* or minors* or kid or kids or child or child* or children* or schoolchild* or schoolchild or adolescen* or juvenil* or youth* or teen* or under*age* or pubescen* or p$ediatric* or preterm*):ti,ab,kw | 374,026 |
| #20 | {OR #15–#19} | 374,156 |
| #21 | #8 AND #14 AND #20 | 70 |

Table A2.
Search Strategies.
Table A2.
Search Strategies.
| CINAHL (EBSCOhost) | ||
|---|---|---|
| No. | Search Details | No. of Articles |
| #1 | MH “Neuromuscular Diseases+” or MH “Gait Disorders, Neurologic+” | 91,434 |
| #2 | TX (amyloid or “brachical plexus” or diabetic or “giant axonal” or “small fiber”) n3 neuropath* | 11,379 |
| #3 | TX (“complex regional pain” or “Eosinophilia-Myalgia” or “Hand-Arm Vibration” or Issacs or “Locked in” or “medial tibial stress” or “nerve compression” or Postpoliomyelitis or “stiff person”) n3 syndrome? | 7068 |
| #4 | TX (muscular or neuromuscular or “motor neuron” or myotonic or “peripheral nervous system”) n3 (disorder or disorders or disease or diseases) | 24,063 |
| #5 | TX (walk* or ambulation or gait) n3 (disorder? or abnormal*) | 6644 |
| #6 | TX intoeing or “in toeing” or outtoeing or “out toeing” or Acrodynia or “Amyotrophic Lateral Sclerosis” or Botulism or Fibromyalgia or “Mitochondrial Myopathies” or Mononeuropathies or Myalgia or “Myasthenia Gravis” or Myositis or Myotoxicity or Neuralgia or Neuritis or “Neurofibromatosis 1” or “Peripheral Nerve Injuries” or “Peripheral Nervous System Neoplasm#” or Poliomyelitis or Polyneuropathies or Radiculopathy or “Tarlov Cysts” | 49,535 |
| #7 | 1 or 2 or 3 or 4 or 5 or 6 | 120,987 |
| #8 | (MH “Orthoses+”) | 11,393 |
| #9 | TX (Orthotic or rehab* or assisted or kinesio*) n3 (brace# or device#) | 4087 |
| #10 | TX parapodium# or TheraTogs or Twister Cables or therasuit# or lycra garment# or AdeliSuit or HAFO or SAFO or DAFO or AFO | 575 |
| #11 | TX (compress* n3 (cloth* or legging# or garment# or sock# or sleeve# or stocking# or wrap#) | 4932 |
| #12 | TX (“dynamic elastomeric fabric” or “ankle foot” or Supramalleloar or “twister wrap”) n3 ortho* | 1748 |
| #13 | 8 or 9 or 10 or 11 or 12 | 20,385 |
| #14 | TX Infan* or newborn* or new-born* or perinat* or neonat* or baby or baby* or babies or toddler* or minors* or kid or kids or child or child* or children* or schoolchild* or schoolchild or adolescen* or juvenil* or youth* or teen* or under*age* or pubescen* or p#ediatric* or preterm* | 1,575,348 |
| #15 | 7 and 13 and 15 | 424 |
| #16 | Limiters: Peer Reviewed | 373 |

Table A3.
Search Strategies.
Table A3.
Search Strategies.
| Ovid MEDLINE(R) ALL <1946 to 24 May 2024> | ||
|---|---|---|
| No. | Search Details | No. of Articles |
| #1 | exp Neuromuscular Diseases/ or exp Gait Disorders, Neurologic/ | 361,891 |
| #2 | ((amyloid or brachical plexus or diabetic or giant axonal or small fiber) adj3 neuropath*).ti,ab,kw. | 15,921 |
| #3 | ((complex regional pain or Eosinophilia-Myalgia or Hand-Arm Vibration or Issacs or Locked in or medial tibial stress or nerve compression or Postpoliomyelitis or stiff person) adj3 syndrome?).ti,ab,kw. | 6924 |
| #4 | ((muscular or neuromuscular or motor neuron or myotonic or peripheral nervous system) adj3 (disorder or disorders or disease or diseases)).ti,ab,kw. | 27,035 |
| #5 | ((gait or walk* or ambulation) adj3 (disorder* or abnormalit*)).ti,ab,kw. | 4655 |
| #6 | (intoeing or in toeing or outtoeing or out toeing or Acrodynia or Amyotrophic Lateral Sclerosis or Botulism or Fibromyalgia or Mitochondrial Myopathies or Mononeuropathies or Myalgia or Myasthenia Gravis or Myositis or Myotoxicity or Neuralgia or Neuritis or Neurofibromatosis 1 or Peripheral Nerve Injuries or Peripheral Nervous System Neoplasms or Poliomyelitis or Polyneuropathies or Radiculopathy or Tarlov Cysts).ab,kw,ti. | 145,731 |
| #7 | 1 or 2 or 3 or 4 or 5 or 6 | 442,779 |
| #8 | exp Orthotic Devices/ | 17,003 |
| #9 | ((Orthotic or rehab* or assisted or kinesio*) adj3 (brace? or device?)).ti,ab,kw. | 3980 |
| #10 | (parapodium? or TheraTogs or Twister Cables or therasuit? or lycra garment? or AdeliSuit or HAFO or SAFO or DAFO or AFO).ti,ab,kw. | 950 |
| #11 | (compress* adj3 (cloth* or legging? or garment? or sock? or sleeve? or stocking? or wrap?)).ti,ab,kw. | 3017 |
| #12 | ((dynamic elastomeric fabric or ankle foot or Supramalleloar or twister wrap) adj3 ortho*).ti,ab,kw. | 1509 |
| #13 | 8 or 9 or 10 or 11 or 12 | 24,286 |
| #14 | exp Pediatrics/ or exp Adolescent/ or exp Child/ or exp Infant/ | 4,071,229 |
| #15 | (Infan* or newborn* or new-born* or perinat* or neonat* or baby or baby* or babies or toddler* or minors* or kid or kids or child or child* or children* or schoolchild* or schoolchild or adolescen* or juvenil* or youth* or teen* or under*age* or pubescen* or p?ediatric* or preterm*).ti,ab,kw. | 2,975,917 |
| #16 | 14 or 15 | 4,993,168 |
| #17 | 7 and 13 and 16 | 512 |

Table A4.
Search Strategies.
Table A4.
Search Strategies.
| Scopus (Elsevier) | ||
|---|---|---|
| No. | Search Details | No. of Articles |
| #1 | TITLE-ABS-KEY ((amyloid OR “brachical plexus” OR diabetic OR “giant axonal” OR “small fiber”) W/3 neuropath*) | 43,519 |
| #2 | TITLE-ABS-KEY ((“complex regional pain” OR “Eosinophilia-Myalgia” OR “Hand-Arm Vibration” OR issacs OR “Locked in” OR “medial tibial stress” OR “nerve compression” OR postpoliomyelitis OR “stiff person”) W/3 syndrome*) | 24,899 |
| #3 | TITLE-ABS-KEY ((muscular OR neuromuscular OR “motor neuron” OR myotonic OR “peripheral nervous system”) W/3 (disorder* OR disease*)) | 99,740 |
| #4 | TITLE-ABS-KEY ((walk* OR ambulation OR gait) W/3 (disorder* OR abnormal*)) | 34,173 |
| #5 | TITLE-ABS-KEY (intoeing OR “in toeing” OR intoed OR “in toed” OR outtoeing OR “out toeing” OR outtoed OR “out toed” OR acrodynia OR “Amyotrophic Lateral Sclerosis” OR botulism OR fibromyalgia OR “Mitochondrial Myopathies” OR mononeuropathies OR myalgia OR “Myasthenia Gravis” OR myositis OR myotoxicity OR neuralgia OR neuritis OR “Neurofibromatosis 1” OR “Peripheral Nerve Injuries” OR “Peripheral Nervous System Neoplasm*” OR poliomyelitis OR polyneuropathies OR radiculopathy OR “Tarlov Cysts”) | 375,662 |
| #6 | 1 or 2 or 3 or 4 or 5 | 536,864 |
| #7 | TITLE-ABS-KEY ((orthotic OR rehab* OR assisted OR kinesio*) W/3 ( brace* OR device*)) | 16,593 |
| #8 | TITLE-ABS-KEY (parapodium* OR theratogs OR “Twister Cables” OR therasuit* OR “lycra garment*” OR adelisuit OR hafo OR safo OR dafo OR afo) | 2186 |
| #9 | TITLE-ABS-KEY (compress* W/3 ( cloth* OR legging* OR garment* OR sock* OR sleeve* OR stocking* OR wrap*)) | 8145 |
| #10 | TITLE-ABS-KEY ((“dynamic elastomeric fabric” OR “ankle foot” OR supramalleloar OR “twister wrap”) W/3 ortho*) | 2766 |
| #11 | 7 or 8 or 9 or 10 | 27,941 |
| #12 | TITLE-ABS-KEY ( infan* OR newborn* OR new-born* OR perinat* OR neonat* OR baby OR baby* OR babies OR toddler* OR minors* OR kid OR kids OR child OR child* OR children* OR schoolchild* OR schoolchild OR adolescen* OR juvenil* OR youth* OR teen* OR under*age* OR pubescen* OR p?ediatric* OR preterm*) | 6,668,988 |
| #13 | 6 and 11 and 12 | 362 |
| #14 | Limited to: Article, Review | 339 |

Table A5.
Search Strategies.
Table A5.
Search Strategies.
| Web of Science (SCI Expanded, SSCI, AHCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-Expanded, IC, Clarivate) | ||
|---|---|---|
| No. | Search Details | No. of Articles |
| #1 | TS = ((amyloid or “brachical plexus” or diabetic or “giant axonal” or “small fiber”) NEAR/3 neuropath*) | 19,297 |
| #2 | TS = ((“complex regional pain” or “Eosinophilia-Myalgia” or “Hand-Arm Vibration” or Issacs or “Locked in” or “medial tibial stress” or “nerve compression” or Postpoliomyelitis or “stiff person”) NEAR/3 syndrome$) | 7131 |
| #3 | TS = ((muscular or neuromuscular or “motor neuron” or myotonic or “peripheral nervous system”) NEAR/3 (disorder$ or disease$)) | 30,129 |
| #4 | TS = ((walk* or ambulation or gait) NEAR/3 (disorder$ or abnormal*)) | 7075 |
| #5 | TS = (intoeing or “in toeing” or outtoeing or “out toeing” or Acrodynia or “Amyotrophic Lateral Sclerosis” or Botulism or Fibromyalgia or “Mitochondrial Myopathies” or Mononeuropathies or Myalgia or “Myasthenia Gravis” or Myositis or Myotoxicity or Neuralgia or Neuritis or “Neurofibromatosis 1” or “Peripheral Nerve Injuries” or “Peripheral Nervous System Neoplasm$” or Poliomyelitis or Polyneuropathies or Radiculopathy or “Tarlov Cysts”) | 140,259 |
| #6 | 1 or 2 or 3 or 4 or 5 | 190,270 |
| #7 | TS = ((Orthotic or rehab* or assisted or kinesio*) NEAR/3 (brace$ or device$)) | 34,626 |
| #8 | TS = (parapodium$ or TheraTogs or Twister Cables or therasuit$ or lycra garment$ or AdeliSuit or HAFO or SAFO or DAFO or AFO) | 1456 |
| #9 | TS = (compress* NEAR/3 (cloth* or legging$ or garment$ or sock$ or sleeve$ or stocking$ or wrap$)) | 4575 |
| #10 | TS = ((“dynamic elastomeric fabric” or “ankle foot” or Supramalleloar or “twister wrap”) NEAR/3 ortho*) | 2012 |
| #11 | 7 or 8 or 9 or 10 | 41,721 |
| #12 | TS = (Infan* or newborn* or new-born* or perinat* or neonat* or baby or baby* or babies or toddler* or minors* or kid or kids or child or child* or children* or schoolchild* or schoolchild or adolescen* or juvenil* or youth* or teen* or under*age* or pubescen* or p$ediatric* or preterm*) | 3,150,924 |
| #13 | 6 and 11 and 12 | 83 |
Appendix B. Risk of Bias

Table A6.
Cochrane collaboration risk of bias tool.
Table A6.
Cochrane collaboration risk of bias tool.
| Study | Randomization Process | Deviations from Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of the Reported Result | Overall Bias |
|---|---|---|---|---|---|---|
| Abd El-Kafy, 2014 [19] | Low | Low | Some concerns | Low | Low | Low |
| Parian et al., 2024 [42] | Low | Low | Some concerns | Low | Low | Low |

Table A7.
ROBINS-I.
Table A7.
ROBINS-I.
| Study | Bias due to Confounding | Bias in Selection of Participants into the Study | Bias in Classification of Interventions | Bias due to Deviations from Intended Intervention | Bias Due to Missing Data | Bias in Measurement of Outcomes | Bias in Selection of the Reported Result | Overall Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Munuera et al., 2010 [13] | Moderate | Some concerns | Low | Low | Some concerns | Low | Low | Moderate |
| Rationale for judgement | No randomization which may confound individual gait patterns and baseline biomechanics. | Participants selected based on clinical presentation, potentially introducing selection bias. | Consistent and clearly defined intervention regarding treatment and non-treatment conditions. | Orthotic device protocol was followed as planned. | Some participants had limited follow-up data. | Objective outcome measures used. | Intended outcomes were addressed and reported. | |
| Davoudi et al., 2022 [33] | Some concerns | Low | Low | Low | Some concerns | Low | Low | Low |
| Rationale for judgement | Potential confounder information in study. | Participants were recruited with pre-defined inclusion criteria. | Consistent and clearly defined intervention. | Intervention was followed as planned. | Few outcome data gaps but not significant. | Validated tools used to measure outcomes. | Intended outcomes were addressed. | |
| Degelaen et al., 2016 [34] | Some concerns | Some concerns | Low | Low | Some concerns | Low | Low | Low |
| Rationale for judgement | Baseline differences in postural stability may confound results. | Convenience sampling for controls may introduce selection bias. | Clearly defined intervention regarding 3D garment. | Garment-wearing protocol was followed as planned. | Some participants had limited follow-up data. | Measurements based on objective assessments. | Intended outcomes were addressed. | |
| Flanagan et al., 2009 [35] | Some concerns | Some concerns | Low | Low | Some concerns | Low | Low | Low |
| Rationale for judgement | Potential confounders like previous interventions not adjusted for. | Small sampling with only 5 participants; limited generalizability. | Interventions (TheraTogs orthotic garment) clearly defined and used consistently across all participants. | Participants adhered to intervention protocol; no significant deviations noted. | Minimal missing data reported; however, due to small sample, any missing data could impact results. | Objective outcome measures used (e.g., Vicon motion analysis), reducing observer bias. | All intended outcomes were reported, with no selective reporting detected. | |
| Rennie et al., 2000 [36] | Moderate | Some concerns | Low | Low | Low | Low | Low | Moderate |
| Rationale for judgement | Small, heterogeneous sample with no control for age, type of neurodisability, and baseline functional level. | Convenience sampling may introduce selection bias. | Consistent and clearly defined intervention regarding orthotic treatment. | Orthotic device protocol was followed as planned. | Minimal missing data. | Objective outcome measures used. | All intended outcomes reported, including PEDI functional assessment and stability measures; no selective reporting detected. | |
| Kim et al., 2022 [37] | Moderate | Some concerns | Low | Low | Some concerns | Low | Low | Moderate |
| Rationale for judgement | Study lacked a randomized design. Factors such as baseline severity of torsion and lifestyle factors were not fully controlled. | Possible selection bias from participant selection based on parents requesting TCR treatment. | Consistent and clearly defined intervention regarding orthotic treatment. | Orthotic device protocol was followed as planned. | Some patients discontinued treatment due to discomfort. | Objective outcome measures used. | Intended outcomes were addressed and reported. | |
| Looper et al., 2012 [39] | Moderate | Some concerns | Low | Low | Some concerns | Low | Low | Moderate |
| Rationale for judgement | Small sample size and lack of control for potential confounders. | Convenience sampling may introduce selection bias. | Consistent and clearly defined intervention regarding orthotic treatment. | Orthotic device protocol was followed as planned. | Data partially missing: navicular drop measurement for one participant. | Objective outcome measures used. | Intended outcomes were addressed and reported. | |
| Selby-Silverstein et al., 2001 [40] | Some concerns | Some concerns | Low | Moderate | Low | Low | Low | Low |
| Rationale for judgement | Potential confounders include age, developmental delay, and other musculoskeletal differences. | Small sample size. | Consistent and clearly defined intervention regarding orthotic treatment. | Variability in individual participant compliance. | No missing data. | Objective outcome measures used. | All intended outcomes reported, including PEDI functional assessment and stability measures; no selective reporting detected. | |
| Mouri et al., 2019 [41] | Some concerns | Some concerns | Low | Low | Some concerns | Low | Low | Low |
| Rationale for judgement | Age and baseline gait characteristics were not fully controlled. | Convenience sampling with limited criteria may introduce selection bias. | Consistent and clearly defined intervention regarding application of medial-wedge insoles across participants. | Orthotic device protocol was followed as planned. | Few participants had limited follow-up data. | Objective outcome measures used. | Intended outcomes were addressed and reported. |

Table A8.
Joanna Briggs Institute critical appraisal tools.
Table A8.
Joanna Briggs Institute critical appraisal tools.
| Checklist Criteria | Were There Clear Criteria for Inclusion in the Case Series? | Was the Condition Measured in a Standard, Reliable Way for All Participants? | Were Valid Methods Used for Identification of the Condition for All Participants? | Did the Case Series Have Consecutive Inclusion of Participants? | Did the Case Series Have Complete Inclusion of Participants? | Was There Clear Reporting of the Demographics of the Participants in the Study? | Was There Clear Reporting of Clinical Information of the Participants? | Were the Outcomes or Follow-Up Results of Cases Clearly Reported? | Was There Clear Reporting of the Presenting Site(s)/Clinic(s) Demographic Information? | Was Statistical Analysis Appropriate? | Overall Appraisal |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Carmick et al., 2012 [27] | Yes | Yes | Unclear | No | Yes | Yes | Yes | Yes | No | No | Include |
| Hebert et al., 2005 [33] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Include |
| Richards et al., 2012 [19] | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | No | Include |
References
- Cao, L.A.; Rethlefsen, S.A.; Wren, T.A.L.; Kay, R.M. Causes of out-toeing gait in children with cerebral palsy. Gait Posture 2020, 76, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Harris, E. The intoeing child: Etiology, prognosis, and current treatment options. Clin. Podiatr. Med. Surg. 2013, 30, 531–565. [Google Scholar] [CrossRef] [PubMed]
- Panjavi, B.; Mortazavi, S.J. Rotational Deformities of the Lower Limb in Children. Iran J. Pediatr. 2007, 17, 393–397. [Google Scholar]
- Rerucha, C.M.; Dickison, C.; Baird, D.C. Lower Extremity Abnormalities in Children. Am. Fam. Physician 2017, 96, 226–233. [Google Scholar]
- Torsional Problems | Pediatric Orthopaedic Society of North America (POSNA). Available online: https://posna.org/physician-education/study-guide/torsional-problems (accessed on 10 October 2024).
- Davids, J.R.; Davis, R.B. Tibial torsion: Significance and measurement. Gait Posture 2007, 26, 169–171. [Google Scholar] [CrossRef]
- Borish, C.N.; Mueske, N.M.; Wren, T.A.L. A comparison of three methods of measuring tibial torsion in children with myelomeningocele and normally developing children. Clin. Anat. 2017, 30, 1043–1048. [Google Scholar] [CrossRef]
- Kainz, H.; Kranzl, A. In-toeing gait requires less muscular effort and reduces lower limb joint loads in people with internal torsional deformities. Gait Posture 2022, 97, S391–S392. [Google Scholar] [CrossRef]
- De Pieri, E.; Cip, J.; Brunner, R.; Weidensteiner, C.; Alexander, N. The functional role of hip muscles during gait in patients with increased femoral anteversion. Gait Posture 2023, 100, 179–187. [Google Scholar] [CrossRef]
- Arnold, A.S.; Komattu, A.V.; Delp, S.L. Internal rotation gait: A compensatory mechanism to restore abduction capacity decreased by bone deformity. Dev. Med. Child. Neurol. 1997, 39, 40–44. [Google Scholar] [CrossRef]
- Kainz, H.; Mindler, G.T.; Kranzl, A. Influence of femoral anteversion angle and neck-shaft angle on muscle forces and joint loading during walking. PLoS ONE 2023, 18, e0291458. [Google Scholar] [CrossRef]
- Ganjehie, S.; Saeedi, H.; Farahmand, B.; Curran, S. The efficiency of gait plate insole for children with in-toeing gait due to femoral antetorsion. Prosthet. Orthot. Int. 2017, 41, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Munuera, P.V.; Castillo, J.M.; Dominguez, G.; Lafuente, G. Orthotic devices with out-toeing wedge as treatment for in-toed gait in children. J. Am. Podiatr. Med. Assoc. 2010, 100, 472–478. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rethlefsen, S.A.; Healy, B.S.; Wren, T.A.L.; Skaggs, D.L.; Kay, R.M. Causes of intoeing gait in children with cerebral palsy. J. Bone Jt. Surg. Am. 2006, 88, 2175–2180. [Google Scholar] [CrossRef]
- Swaroop, V.T.; Dias, L. Orthopaedic management of spina bifida—Part II: Foot and ankle deformities. J. Child. Orthop. 2011, 5, 403–414. [Google Scholar] [CrossRef]
- Swaroop, V.T.; Dias, L. Orthopedic management of spina bifida. Part I: Hip, knee, and rotational deformities. J. Child. Orthop. 2009, 3, 441–449. [Google Scholar] [CrossRef]
- Zhou, J.; Butler, E.E.; Rose, J. Neurologic Correlates of Gait Abnormalities in Cerebral Palsy: Implications for Treatment. Front. Hum. Neurosci. 2017, 11, 103. [Google Scholar] [CrossRef]
- Tsagkaris, C.; Hamberg, M.; Villefort, C.; Dreher, T.; Krautwurst, B. Walking and Running of Children with Decreased Femoral Torsion. Children 2024, 11, 617. [Google Scholar] [CrossRef]
- Abd El-Kafy, E. The clinical impact of orthotic correction of lower limb rotational deformities in children with cerebral palsy: A randomized controlled trial. Clin. Rehabil. 2014, 28, 1004–1014. [Google Scholar] [CrossRef]
- Richards, A.; Morcos, S.; Rethlefsen, S.; Ryan, D. The use of TheraTogs versus twister cables in the treatment of in-toeing during gait in a child with spina bifida. Pediatr. Phys. Ther. 2012, 24, 321–326. [Google Scholar] [CrossRef]
- Mackay, J.; Thomason, P.; Sangeux, M.; Passmore, E.; Francis, K.; Graham, H.K. The impact of symptomatic femoral neck anteversion and tibial torsion on gait, function and participation in children and adolescents. Gait Posture 2021, 86, 144–149. [Google Scholar] [CrossRef]
- Sass, P.; Hassan, G. Lower Extremity Abnormalities in Children. Am. Fam. Physician 2003, 68, 461–468. [Google Scholar] [PubMed]
- Solaiman, R.H.; Shih, Y.; Bakker, C.; Arendt, E.A.; Tompkins, M.A. Tibial derotational osteotomy for idiopathic tibial torsion: A systematic review of surgical indications based on clinical presentation and measurement technique. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 1798–1809. [Google Scholar] [CrossRef] [PubMed]
- Aktas, S.; Aiona, M.D.; Orendurff, M. Evaluation of Rotational Gait Abnormality in the Patients Cerebral Palsy. J. Pediatr. Orthop. 2000, 20, 217. [Google Scholar] [CrossRef]
- Lincoln, T.L.; Suen, P.W. Common rotational variations in children. J. Am. Acad. Orthop. Surg. 2003, 11, 312–320. [Google Scholar] [CrossRef]
- Joseph, B. The Inverted Foot. In Paediatric Orthopaedic Diagnosis; Springer: New Delhi, India, 2015; pp. 45–58. ISBN 978-81-322-2391-7. [Google Scholar]
- Michalitsis, J.; Murphy, A.T.; Rawicki, B.; Haines, T.P.; Williams, C. Full length foot orthoses have an immediate treatment effect and modify gait of children with idiopathic toe walking. Gait Posture 2019, 68, 227–231. [Google Scholar] [CrossRef]
- Chen, W.; Liu, X.; Pu, F.; Yang, Y.; Wang, L.; Liu, H.; Fan, Y. Conservative treatment for equinus deformity in children with cerebral palsy using an adjustable splint-assisted ankle-foot orthosis. Medicine 2017, 96, e8186. [Google Scholar] [CrossRef]
- Alsancak, S.; Guner, S.; Kınık, H. Improved Gait Parameters After Orthotic Treatment in Children with Infantile Tibia Vara. Sci. Rep. 2020, 10, 3187. [Google Scholar] [CrossRef]
- Colò, G.; Leigheb, M.; Surace, M.F.; Fusini, F. The efficacy of shoes modification and orthotics in hallux valgus deformity: A comprehensive review of literature. Musculoskelet. Surg. 2024, 108, 395–402. [Google Scholar] [CrossRef]
- Cooper, S.; Hanning, J.; Hegarty, C.; Generalis, C.; Smith, A.; Hall, T.; Starbuck, C.; Kaux, J.F.; Schwartz, C.; Buckley, C. Effects of a range of 6 prefabricated orthotic insole designs on plantar pressure in a healthy population: A randomized, open-label crossover investigation. Prosthet. Orthot. Int. 2024, 48, 474. [Google Scholar] [CrossRef]
- Chiou-Tan, F.Y.; Bloodworth, D. Approach to gait disorders and orthotic management in adult onset neuromuscular diseases. Muscle Nerve 2024. early view. [Google Scholar] [CrossRef]
- Davoudi, M.; Khosravi Farsani, M.; Babaee, T.; Ranjbar, H.; Shokouhyan, S.M.; Ghaznavi, A.; Rezaei, M. The Effects of Combining High-Top Shoes with Twister Wrap Orthoses on Balance Parameters of Children with Spastic Diplegic Cerebral Palsy. J. Biomed. Phys. Eng. 2022, 12, 91–100. [Google Scholar] [CrossRef]
- Degelaen, M.; De Borre, L.; Buyl, R.; Kerckhofs, E.; De Meirleir, L.; Dan, B. Effect of supporting 3D-garment on gait postural stability in children with bilateral spastic cerebral palsy. NeuroRehabilitation 2016, 39, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, A.; Krzak, J.; Peer, M.; Johnson, P.; Urban, M. Evaluation of short-term intensive orthotic garment use in children who have cerebral palsy. Pediatr. Phys. Ther. 2009, 21, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Rennie, D.J.; Attfield, S.F.; Morton, R.E.; Polak, F.J.; Nicholson, J. An evaluation of lycra garments in the lower limb using 3-D gait analysis and functional assessment (PEDI). Gait Posture 2000, 12, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Suzuki, M.; Minowa, K.; Nittono, H.; Shimizu, T. Efficacy of a Tibia Counter Rotator System for the Treatment of Internal Tibial Torsion in Children. Children 2022, 9, 970. [Google Scholar] [CrossRef]
- Carmick, J. Importance of orthotic subtalar alignment for development and gait of children with cerebral palsy. Pediatr. Phys. Ther. 2012, 24, 302–307. [Google Scholar] [CrossRef]
- Looper, J.; Benjamin, D.; Nolan, M.; Schumm, L. What to Measure When Determining Orthotic Needs in Children With Down Syndrome: A Pilot Study. Pediatr. Phys. Ther. 2012, 24, 313–319. [Google Scholar] [CrossRef]
- Selby-Silverstein, L.; Hillstrom, H.J.; Palisano, R.J. The effect of foot orthoses on standing foot posture and gait of young children with Down syndrome. NeuroRehabilitation 2001, 16, 183–193. [Google Scholar] [CrossRef]
- Mouri, H.; Kim, W.-C.; Arai, Y.; Yoshida, T.; Oka, Y.; Ikoma, K.; Fujiwara, H.; Kubo, T. Effectiveness of medial-wedge insoles for children with intoeing gait who fall easily. Turk. J. Phys. Med. Rehabil. 2019, 65, 9–15. [Google Scholar] [CrossRef]
- Parian, S.; Farahmand, B.; Saeedi, H.; Cham, M.B. Effectiveness of gait plate insole and lateral sole wedged shoes on foot progression angle in children with in-toeing gait: A prospective randomized control trial. Gait Posture 2024, 109, 120–125. [Google Scholar] [CrossRef]
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The Levels of Evidence and their role in Evidence-Based Medicine. Plast. Reconstr. Surg. 2011, 128, 305. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef]
- Hudson, D. The rotational profile: A study of lower limb axial torsion, hip rotation, and the foot progression angle in healthy adults. Gait Posture 2016, 49, 426–430. [Google Scholar] [CrossRef]
- Scataglini, S.; Abts, E.; Van Bocxlaer, C.; Van den Bussche, M.; Meletani, S.; Truijen, S. Accuracy, Validity, and Reliability of Markerless Camera-Based 3D Motion Capture Systems versus Marker-Based 3D Motion Capture Systems in Gait Analysis: A Systematic Review and Meta-Analysis. Sensors 2024, 24, 3686. [Google Scholar] [CrossRef]
- Higgins, J. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Training. Available online: https://training.cochrane.org/handbook (accessed on 12 December 2024).
- Kim, H.S. The effects of fixed and graduated application percentage-type compression leggings in adult women with mild in-toeing gait. Text. Res. J. 2023, 00405175231208022. [Google Scholar] [CrossRef]
- Galli, M.; Cimolin, V.; Rigoldi, C.; Albertini, G. Quantitative Evaluation of the Effects of Ankle Foot Orthosis on Gait in Children with Cerebral Palsy Using the Gait Profile Score and Gait Variable Scores. J. Dev. Phys. Disabil. 2016, 28, 367–379. [Google Scholar] [CrossRef]
- Thomson, J.D.; Ounpuu, S.; Davis, R.B.; DeLuca, P.A. The effects of ankle-foot orthoses on the ankle and knee in persons with myelomeningocele: An evaluation using three-dimensional gait analysis. J. Pediatr. Orthop. 1999, 19, 27–33. [Google Scholar] [CrossRef]
- Vankoski, S.J.; Michaud, S.; Dias, L. External tibial torsion and the effectiveness of the solid ankle-foot orthoses. J. Pediatr. Orthop. 2000, 20, 349–355. [Google Scholar] [CrossRef]
- Emara, H.A.; Sobh, E.; Almohammadi, R.H.; Alamri, E.A.; Aljohani, M.M.A.; Alhammad, A.A. Quality of Life and Functional Independence of TheraTogs in Children with Spastic Diplegic Cerebral Palsy: A Randomized Controlled Clinical Trial. J. Multidiscip. Health 2024, 17, 4645–4652. [Google Scholar] [CrossRef] [PubMed]
- Schelhaas, R.; Hajibozorgi, M.; Hortobágyi, T.; Hijmans, J.M.; Greve, C. Conservative interventions to improve foot progression angle and clinical measures in orthopedic and neurological patients—A systematic review and meta-analysis. J. Biomech. 2022, 130, 110831. [Google Scholar] [CrossRef] [PubMed]
- Emara, H.A.; Al-Johany, A.H.; Khaled, O.A.; Al-Shenqiti, A.M.; Ali, A.R.H.; Aljohani, M.M.; Sobh, E. Effect of the Dynamic Orthotic Garment on Postural Control, and Endurance in Children with Spastic Diplegic Cerebral Palsy: A Randomized Controlled Trial. J. Multidiscip. Heal. 2024, 17, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Cunha, A.; Lima-Alvarez, C.; Rocha, A.; Tudella, E. Effects of elastic therapeutic taping on motor function in children with motor impairments: A systematic review. Disabil. Rehabil. 2018, 40, 1609–1617. [Google Scholar] [CrossRef]
- Fatone, S.; Johnson, W.B.; Kwak, S. Using a three-dimensional model of the Ankle-Foot Orthosis/leg to explore the effects of combinations of axis misalignments. Prosthet. Orthot. Int. 2016, 40, 247–252. [Google Scholar] [CrossRef]
- Shuman, B.R.; Totah, D.; Gates, D.H.; Gao, F.; Ries, A.J.; Russell Esposito, E. Comparison of five different methodologies for evaluating ankle–foot orthosis stiffness. J. Neuroeng. Rehabil. 2023, 20, 11. [Google Scholar] [CrossRef]
- Rambo, A.; Rhodes, L.; Lomax, J.; Cao, X.; Steele, J.; Romer, K.; Spence, D.; Sheffer, B.W.; Warner, W.C.; Sawyer, J.R.; et al. Factors that Influence Acquisition of Lower Extremity Braces in the Pediatric Orthopaedic Population. J. Pediatr. Orthop. 2022, 42, 40–46. [Google Scholar] [CrossRef]
- Marcotte, D.; Ferri, E.; Xue, X.; Katsolis, A.; Rajotte, E.; Cardiff, K.; Preuss, R. Barriers and facilitators to lower extremity orthotic compliance in the pediatric population: A scoping review of the literature. Prosthet. Orthot. Int. 2023, 47, 155–167. [Google Scholar] [CrossRef]
- Powell, M.; Seid, M.; Szer, I.S. Efficacy of custom foot orthotics in improving pain and functional status in children with juvenile idiopathic arthritis: A randomized trial. J. Rheumatol. 2005, 32, 943–950. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).