Effect of Wearable Exoskeleton Robots on Muscle Activation and Gait Parameters on a Treadmill: A Randomized Controlled Trial
Abstract
1. Introduction
2. State of the Art
2.1. Maximum Voluntary Contraction with Wearable Exoskeleton
2.2. Muscle Fatigue Analysis with Wearable Exoskeleton
2.3. Changes in Gait Parameters Associated with Exoskeleton
2.4. Research Summary and Implications
3. Evaluating Exoskeletons for Industrial Use: Purpose and Impact
4. Materials and Methods
4.1. Participants
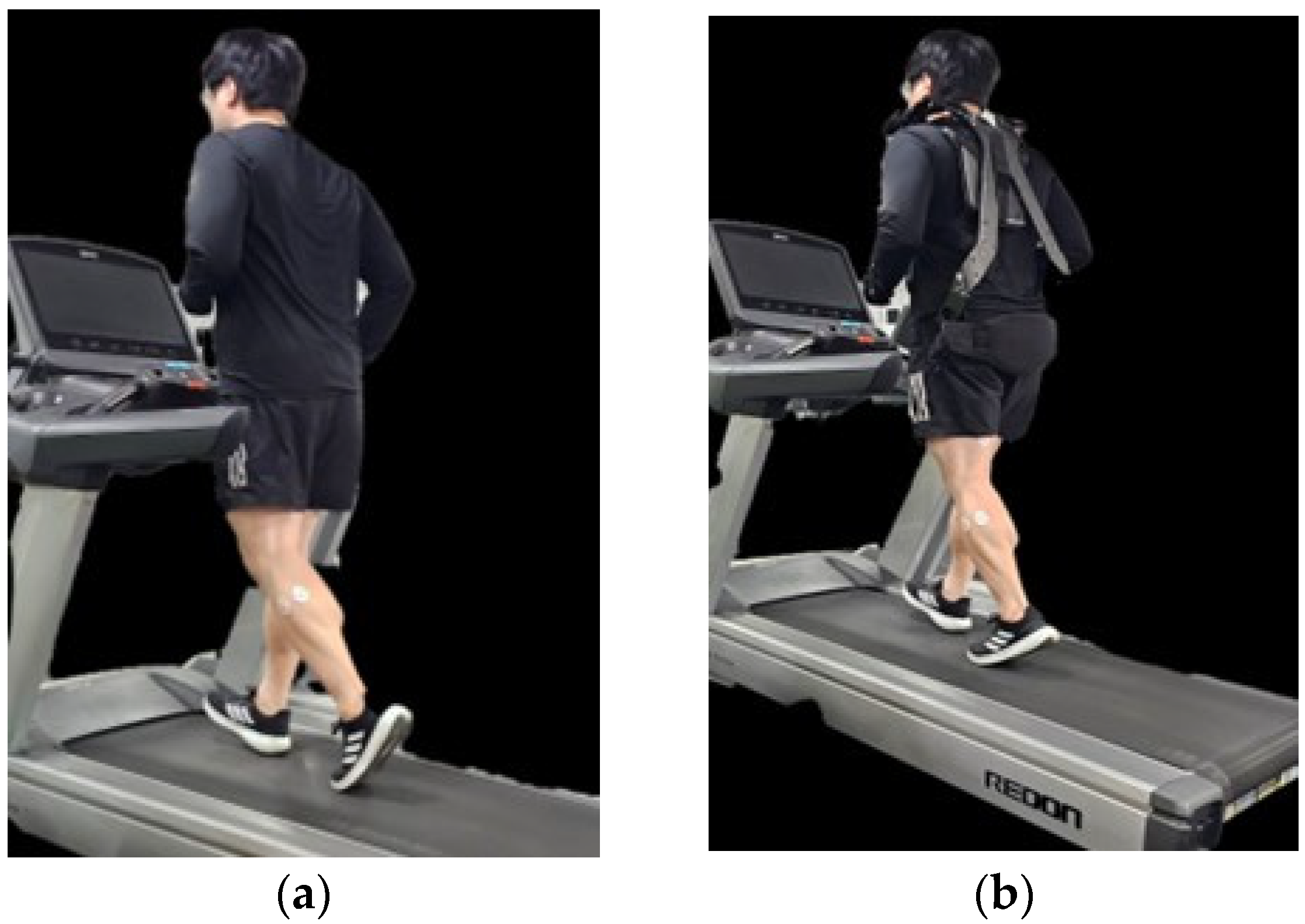
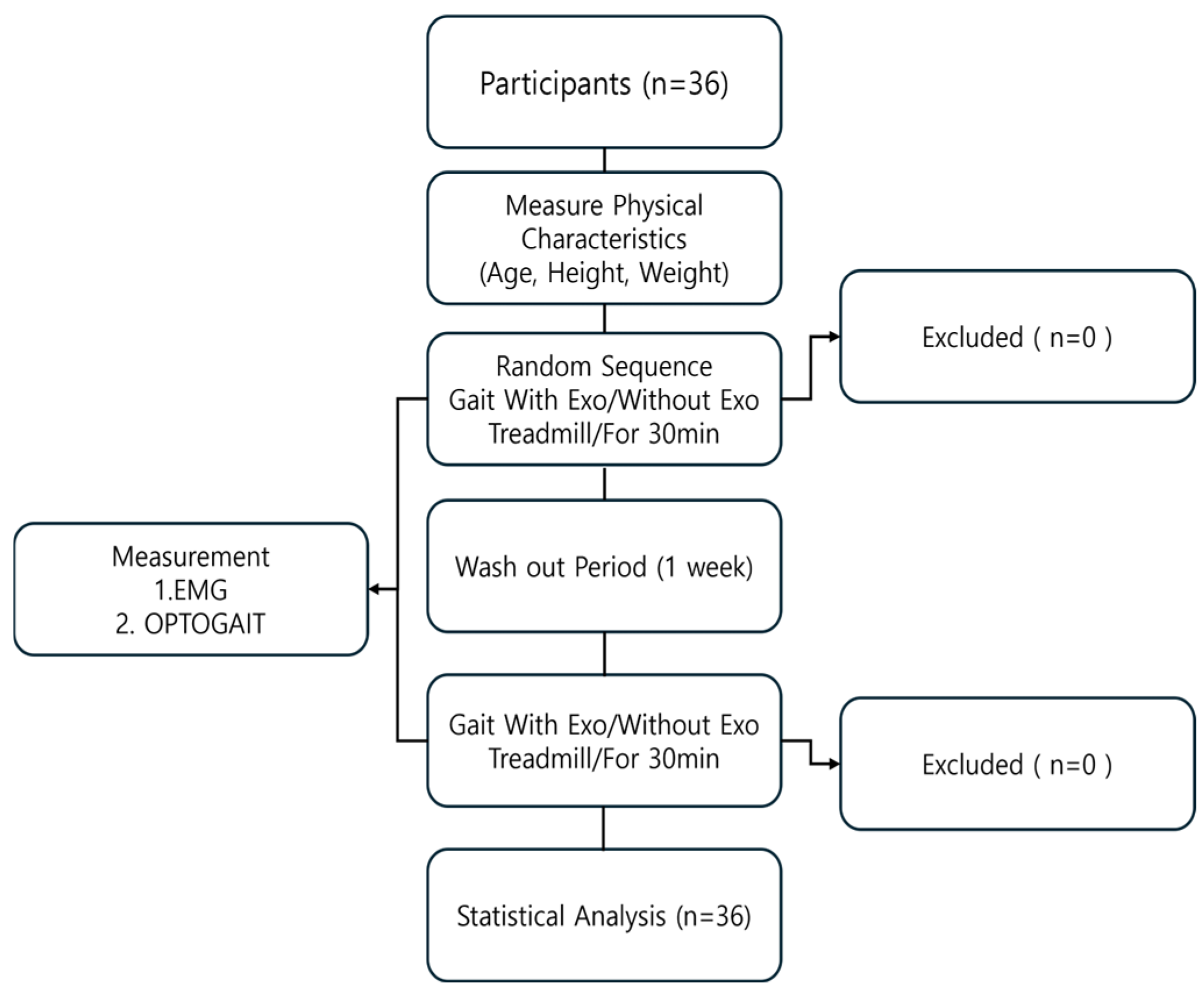
4.2. Experimental Procedure
4.3. Exoskeleton Robot
4.4. Electromyography
4.5. Optogait
4.6. Statistical Analysis
5. Results
5.1. Comparison of Maximum Voluntary Contraction Values During Gait with and Without an Exoskeleton
5.2. Comparison of Muscle Fatigue Values During Gait with and Without Exoskeleton
5.3. Comparison of Stance Phase and Swing Phase Values During Gait with and Without Exoskeleton
5.4. Comparison of Loading Response and Pre-Swing Values During Gait with and Without Exoskeleton
5.5. Comparison of Step Length and Stride Length Measurements During Gait with and Without Exoskeleton Support
6. Discussion
6.1. LEXO-V Wearable Robot
6.2. Muscle Activation, Fatigue Accumulation, and Gait Adaptation During Extended Exoskeleton Use
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vélez-Guerrero, M.A.; Callejas-Cuervo, M.; Mazzoleni, S. Artificial intelligence-based wearable robotic exoskeletons for upper limb rehabilitation. A review. Sensors 2021, 21, 2146. [Google Scholar] [CrossRef] [PubMed]
- Xia, H.; Zhang, Y.; Rajabi, N.; Taleb, F.; Yang, Q.; Kragic, D.; Li, Z. Shaping high-performance wearable robots for human motor and sensory reconstruction and enhancement. Nat. Commun. 2024, 15, 1760. [Google Scholar] [PubMed]
- Xiong, J.; Chen, J.; Lee, P.S. Functional fibers and fabrics for soft robotics, wearables, and human–robot interface. Adv. Mater. 2021, 33, 2002640. [Google Scholar] [PubMed]
- Sivan, M.; O’Connor, R.; Makower, S.; Levesley, M.; Bhakta, B. Systematic review of outcome measures used in the evaluation of robot-assisted upper limb exercise in stroke. J. Rehabil. Med. 2021, 43, 181–189. [Google Scholar]
- Molteni, F.; Gasperini, G.; Cannaviello, G.; Guanziroli, E. Exoskeleton and end-effector robots for upper and lower limbs rehabilitation: Narrative review. PM&R 2018, 10, S174–S188. [Google Scholar]
- Theurel, J.; Desbrosses, K. Occupational exoskeletons: Overview of their benefits and limitations in preventing work-related musculoskeletal disorders. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 264–280. [Google Scholar] [CrossRef]
- Meng, W.; Liu, Q.; Zhou, Z.; Ai, Q.; Sheng, B.; Xie, S.S. Recent development of mechanisms and control strategies for robot-assisted lower limb rehabilitation. Mechatronics 2015, 31, 132–145. [Google Scholar]
- Chen, B.; Ma, H.; Qin, L.Y.; Gao, F.; Chan, K.M.; Law, S.W.; Liao, W.H. Recent developments and challenges of lower extremity exoskeletons. J. Orthop. Transl. 2016, 5, 26–37. [Google Scholar] [CrossRef]
- Kitatani, R.; Ohata, K.; Takahashi, H.; Shibuta, S.; Hashiguchi, Y.; Yamakami, N. Reduction in energy expenditure during walking using an automated stride assistance device in healthy young adults. Arch. Phys. Med. Rehabil. 2014, 95, 2128–2133. [Google Scholar]
- Lu, R.; Li, Z.; Su, C.Y.; Xue, A. Development and learning control of a human limb with a rehabilitation exoskeleton. IEEE Trans. Ind. Electron. 2013, 61, 3776–3785.13. [Google Scholar] [CrossRef]
- Meng, Q.; Zeng, Q.; Xie, Q.; Fei, C.; Kong, B.; Lu, X.; Yu, H. Flexible lower limb exoskeleton systems: A review. Neurorehabilitation 2022, 50, 367–390. [Google Scholar] [CrossRef] [PubMed]
- Van Sluijs, R.; Scholtysik, T.; Brunner, A.; Kuoni, L.; Bee, D.; Kos, M.; Lambercy, O. Design and evaluation of the OmniSuit: A passive occupational exoskeleton for back and shoulder support. Appl. Ergon. 2024, 120, 104332. [Google Scholar] [CrossRef] [PubMed]
- Bär, M.; Steinhilber, B.; Rieger, M.A.; Luger, T. The influence of using exoskeletons during occupational tasks on acute physical stress and strain compared to no exoskeleton–A systematic review and meta-analysis. Appl. Ergon. 2021, 94, 103385. [Google Scholar] [CrossRef]
- Kong, Y.K.; Choi, K.H.; Cho, M.U.; Kim, S.Y.; Kim, M.J.; Shim, J.W.; Shim, H.H. Ergonomic assessment of a lower-limb exoskeleton through electromyography and Anybody modeling system. Int. J. Environ. Res. Public Health 2022, 19, 8088. [Google Scholar] [CrossRef]
- Shim, H.H.; Choi, K.H.; Keum, H.; Son, S.; Kim, J.H.; Seo, M.T.; Kong, Y.K. Evaluation of the Effects of Passive Lower-Limb Exoskeletons on Muscle Activities According to Working Heights. Appl. Sci. 2023, 13, 11754. [Google Scholar] [CrossRef]
- Pillai, M.V.; Van Engelhoven, L.; Kazerooni, H. Evaluation of a lower leg support exoskeleton on floor and below hip height panel work. Hum. Factors 2020, 62, 489–500. [Google Scholar] [CrossRef]
- Del Ferraro, S.; Falcone, T.; Ranavolo, A.; Molinaro, V. The effects of upper-body exoskeletons on human metabolic cost and thermal response during work tasks—A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 7374. [Google Scholar] [CrossRef]
- Arachchige, S.D.; Piyathilaka, L.; Sul, J.H.; Preethichandra, D.M.G. A Review of Potential Exoskeletons for the Prevention of Work-Related Musculoskeletal Disorders in Agriculture. Sensors 2024, 24, 7026. [Google Scholar] [CrossRef]
- Wang, Z.; Wu, X.; Zhang, Y.; Chen, C.; Liu, S.; Liu, Y.; Ma, Y. A semi-active exoskeleton based on EMGs reduces muscle fatigue when squatting. Front. Neurorobotics 2021, 15, 625479. [Google Scholar] [CrossRef]
- Van Sluijs, R.M.; Rodriguez-Cianca, D.; Sanz-Morère, C.B.; Massardi, S.; Bartenbach, V.; Torricelli, D. A method to quantify the reduction of back and hip muscle fatigue of lift-support exoskeletons. Wearable Technol. 2023, 4, e2. [Google Scholar] [CrossRef]
- Chang, Y.; Kang, J.; Jeong, B.; Kim, G.; Lim, B.; Choi, B.; Lee, Y. Verification of industrial worker walking efficiency with wearable hip exoskeleton. Appl. Sci. 2023, 13, 12609. [Google Scholar] [CrossRef]
- Bosch, T.; van Eck, J.; Knitel, K.; de Looze, M. The effects of passive exoskeleton on muscle activity, discomfort and endurance time in forward bending work. Appl. Ergon. 2016, 54, 212–217. [Google Scholar]
- Veneman, J.F.; Kruidhof, R.; Hekman, E.E.; Ekkelenkamp, R.; Van Asseldonk, E.H.; Van Der Kooij, H. Design and evaluation of the LOPES exoskeleton robot for interactive gait rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 379–386. [Google Scholar] [PubMed]
- Farkhatdinov, I.; Ebert, J.; Van Oort, G.; Vlutters, M.; Van Asseldonk, E.; Burdet, E. Assisting human balance in standing with a robotic exoskeleton. IEEE Robot. Autom. Lett. 2019, 4, 414–421. [Google Scholar]
- Lee, S.H.; Lee, H.J.; Chang, W.H.; Choi, B.O.; Lee, J.; Kim, J.; Kim, Y.H. Gait performance and foot pressure distribution during wearable robot-assisted gait in elderly adults. J. Neuroeng. Rehabil. 2017, 14, 123. [Google Scholar] [PubMed]
- Banala, S.K.; Kim, S.H.; Agrawal, S.K.; Scholz, J.P. Robot assisted gait training with active leg exoskeleton (ALEX). IEEE Trans. Neural Syst. Rehabil. Eng. 2008, 17, 2–8. [Google Scholar]
- Lee, G.; Cha, D. Statistical Analysis of the Effectiveness of Wearable Robot. Electronics 2021, 10, 1006. [Google Scholar] [CrossRef]
- Kim, H.R.; Park, J.S.; Lee, K.H.; Ryu, J.K. Development of muscle-strength-assistant device and military suitability for high-weight carrying. J. Korea Robot. Soc. 2022, 17, 191–197. [Google Scholar]
- DONGBANG CULTURE UNIVERSITY Institutional Review Board. Available online: https://www.dongbang.ac.kr/html/index/ (accessed on 11 December 2024).
- Kyeong, S.; Kim, W.D.; Feng, J.; Kim, J. Implementation issues of EMG-based motion intention detection for exoskeletal robots. In Proceedings of the 2018 27th IEEE International Symposium on Robot and Human Interactive Communication (RO-MAN), Nanjing, China, 27–31 August 2018; pp. 915–920. [Google Scholar]
- Rodrigues-Carvalho, C.; Fernández-García, M.; Pinto-Fernández, D.; Sanz-Morere, C.; Barroso, F.O.; Borromeo, S.; Del-Ama, A.J. Benchmarking the effects on human–exoskeleton interaction of trajectory, admittance and EMG-triggered exoskeleton movement control. Sensors 2023, 23, 791. [Google Scholar] [CrossRef]
- Avdan, G.; Onal, S.; Smith, B.K. Normalization of EMG signals: Optimal MVC positions for the lower limb muscle groups in healthy subjects. J. Med. Biol. Eng. 2023, 43, 195–202. [Google Scholar] [CrossRef]
- De Luca, C.J. Myoelectrical manifestations of localized muscular fatigue in humans. Crit. Rev. Biomed. Eng. 1984, 11, 251–279. [Google Scholar]
- Iranzo, S.; Piedrabuena, A.; García-Torres, F.; Martinez-de-Juan, J.L.; Prats-Boluda, G.; Sanchis, M.; Belda-Lois, J.M. Assessment of a passive lumbar exoskeleton in material manual handling tasks under laboratory conditions. Sensors 2022, 22, 4060. [Google Scholar] [CrossRef]
- Carbajales-Lopez, J.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Casado-Hernández, I.; Benito-De Pedro, M.; Rodríguez-Sanz, D.; San Antolín, M. The optogait motion analysis system for clinical assessment of 2D spatio-temporal gait parameters in young adults: A reliability and repeatability observational study. Appl. Sci. 2020, 10, 3726. [Google Scholar] [CrossRef]
- Lee, S.H.; Kim, J.; Lim, B.; Lee, H.J.; Kim, Y.H. Exercise with a wearable hip-assist robot improved physical function and walking efficiency in older adults. Sci. Rep. 2023, 13, 7269. [Google Scholar] [CrossRef] [PubMed]
- Kong, Y.K.; Kim, J.H.; Shim, H.H.; Shim, J.W.; Park, S.S.; Choi, K.H. Efficacy of passive upper-limb exoskeletons in reducing musculoskeletal load associated with overhead tasks. Appl. Ergon. 2023, 109, 103965. [Google Scholar] [PubMed]
- Raasch, C.C.; Zajac, F.E. Locomotor strategy for pedaling muscle groups and biomechanical functions. J. Neurophysiol. 1999, 82, 515–525. [Google Scholar]
- Cleather, D.J.; Southgate, D.F.; Bull, A.M. The role of the biarticular hamstrings and gastrocnemius muscles in closed chain lower limb extension. J. Theor. Biol. 2015, 365, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Durandau, G.; Rampeltshammer, W.F.; van der Kooij, H.; Sartori, M. Neuromechanical model-based adaptive control of bilateral ankle exoskeletons: Biological joint torque and electromyogram reduction across walking conditions. IEEE Trans. Robot. 2022, 38, 1380–1394. [Google Scholar]
- Baptista, R.; Salvaggio, F.; Cavallo, C.; Pizzocaro, S.; Galasso, S.; Schmid, M.; De Nunzio, A.M. Training-induced muscle fatigue with a powered lower-limb exoskeleton: A preliminary study on healthy subjects. Med. Sci. 2022, 10, 55. [Google Scholar] [CrossRef]
- Dai, X.; Zhou, Z.; Wang, Z.; Ruan, L.; Wang, R.; Rong, X.; Wang, Q. Reducing Knee Joint Loads During Stance Phase with a Rigid-Soft Hybrid Exoskeleton. IEEE Trans. Neural Syst. Rehabil. Eng. 2024, 32, 4164–4173. [Google Scholar]
- Hultman, E.R.I.C.; Spriet, L.L. Skeletal muscle metabolism, contraction force and glycogen utilization during prolonged electrical stimulation in humans. J. Physiol. 1986, 374, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Cheng, W.; Liu, F.; Zhang, M.; Wang, K. The effects on muscle activity and discomfort of varying load carriage with and without an augmentation exoskeleton. Appl. Sci. 2018, 8, 2638. [Google Scholar] [CrossRef]

| Variables | Total (n = 36) |
|---|---|
| Age | 23.10 ± 4.70 |
| Sex | Male, n = 21, Female, n = 15 |
| Height, cm | 168.92 ± 8.68 |
| Body weight, kg | 63.99 ± 10.43 |
| Body mass index, kg/m2 | 22.48 ± 2.51 |
| MVC (%) | 10 min | t | p | 20 min | t | p | 30 min | t | p | |
|---|---|---|---|---|---|---|---|---|---|---|
| Rectus femoris | W/O Exo | 44.93 ± 9.92 | 2.576 | 0.014 * | 46.49 ± 8.66 | 5.241 | <0.00 ** | 52.39 ± 5.70 | 10.946 | <0.00 ** |
| W/Exo | 40.60 ± 3.39 | 36.7 ± 3.32 | 32.81 ± 3.57 | |||||||
| Gastrocnemius medialis | W/O Exo | 18.25 ± 3.18 | −11.58 | <0.00 ** | 19.46 ± 3.42 | −6.936 | <0.00 ** | 24.34 ± 4.39 | 3.711 | 0.001 * |
| W/Exo | 24.73 ± 2.16 | 23.59 ± 2.11 | 21.33 ± 2.25 | |||||||
| Hamstring | W/O Exo | 17.05 ± 3.61 | 0.069 | 0.945 | 19.22 ± 3.96 | 3.595 | 0.001 * | 24.16 ± 4.13 | 10.329 | <0.00 ** |
| W/Exo | 17.00 ± 2.05 | 16.49 ± 2.06 | 14.16 ± 3.41 | |||||||
| Vastus medialis | W/O Exo | 26.70 ± 2.95 | −0.657 | 0.515 | 19.22 ± 3.96 | 3.651 | 0.001 * | 36.60 ± 6.13 | 13.36 | <0.00 ** |
| W/Exo | 27.21 ± 3.35 | 25.19 ± 2.14 | 22.21 ± 3.43 | |||||||
| Muscle Fatigue (%) | 10 min | t | p | 20 min | t | p | 30 min | t | p | |
|---|---|---|---|---|---|---|---|---|---|---|
| Rectus Femoris | W/O Exo | 29.88 ± 8.74 | −6.552 | <0.00 ** | 34.22 ± 7.36 | 2.326 | 0.026 * | 42.90 ± 7.07 | 8.284 | <0.00 ** |
| W/Exo | 39.26 ± 2.97 | 31.32 ± 4.13 | 32.08 ± 4.97 | |||||||
| gastrocnemius medialis | W/O Exo | 23.56 ± 4.71 | 2.480 | <0.00 ** | 28.18 ± 3.83 | 14.097 | <0.00 ** | 33.60 ± 4.53 | 18.702 | <0.00 ** |
| W/Exo | 21.32 ± 3.38 | 18.93 ± 1.84 | 16.13 ± 3.32 | |||||||
| Hamstring | W/O Exo | 25.14 ± 3.92 | −9.088 | <0.00 ** | 30.57 ± 2.49 | 3.491 | <0.00 ** | 37.22 ± 3.17 | 20.096 | <0.00 ** |
| W/Exo | 32.25 ± 3.40 | 27.64 ± 5.06 | 24.91 ± 2.01 | |||||||
| vastus medialis | W/O Exo | 18.31 ± 3.00 | −14.129 | <0.00 ** | 23.02 ± 2.94 | −2.158 | 0.038 * | 31.36 ± 4.06 | 19.275 | <0.00 ** |
| W/Exo | 29.88 ± 8.74 | 24.41 ± 2.09 | 20.66 ± 2.45 | |||||||
| Gait Parameter (%) | 10 min | t | p | 20 min | t | p | 30 min | t | p | |
|---|---|---|---|---|---|---|---|---|---|---|
| Stance Phase | Right W/O Exo | 72.69 ± 0.48 | 2.737 | 0.01 * | 71.47 ± 0.48 | −2.66 | 0.012 * | 71.11 ± 0.44 | −12.109 | <0.00 ** |
| Right W/Exo | 72.09 ± 1.35 | 72.28 ± 1.81 | 74.50 ± 1.60 | |||||||
| Left W/O Exo | 71.62 ± 0.49 | 7.531 | <0.00 ** | 70.78 ± 0.55 | −13.885 | <0.00 ** | 70.73 ± 0.52 | −14.680 | <0.00 ** | |
| Left W/Exo | 70.65 ± 0.12 | 74.18 ± 1.49 | 74.86 ± 1.71 | |||||||
| Swing Phase | Right W/O Exo | 28.58 ± 0.48 | 3.777 | 0.001 * | 28.04 ± 0.51 | 1.376 | 0.178 | 29.55 ± 0.34 | 10.799 | <0.00 ** |
| Right W/Exo | 27.46 ± 1.78 | 27.55 ± 1.98 | 27.26 ± 1.24 | |||||||
| Left W/O Exo | 29.40 ± 0.44 | 4.356 | <0.00 ** | 30.43 ± 0.52 | 3.795 | 0.001 * | 30.13 ± 1.77 | 5.079 | <0.00 ** | |
| Left W/Exo | 28.29 ± 1.48 | 28.72 ± 2.50 | 23.94 ± 6.82 | |||||||
| Gait Parameter (%) | 10 min | t | p | 20 min | t | p | 30 min | t | p | |
|---|---|---|---|---|---|---|---|---|---|---|
| Loading Response | Right W/O Exo | 20.27 ± 2.21 | −6.175 | <0.00 ** | 21.79 ± 1.87 | 11.457 | <0.00 ** | 23.02 ± 0.99 | 28.305 | <0.00 ** |
| Right W/Exo | 22.96 ± 1.08 | 18.51 ± 0.95 | 17.73 ± 0.52 | |||||||
| Left W/O Exo | 21.81 ± 1.87 | −3.472 | 0.001 * | 22.85 ± 1.80 | 10.727 | <0.00 ** | 23.30 ± 1.15 | 17.772 | <0.00 ** | |
| Left W/Exo | 23.29 ± 1.16 | 19.91 ± 0.92 | 18.57 ± 1.17 | |||||||
| Pre-Swing | Right W/O Exo | 21.76 ± 1.94 | 2.042 | 0.049 * | 21.27 ± 2.58 | 1.376 | <0.00 ** | 22.55 ± 1.41 | 10.799 | <0.00 ** |
| Right W/Exo | 20.54 ± 2.85 | 21.82 ± 1.86 | 17.31 ± 0.74 | |||||||
| Left W/O Exo | 20.50 ± 1.58 | 4.356 | 0.148 | 18.56 ± 0.91 | 3.795 | 0.041 * | 20.91 ± 1.14 | 5.079 | <0.00 ** | |
| Left W/Exo | 21.27 ± 2.85 | 20.02 ± 0.85 | 18.29 ± 0.76 | |||||||
| Gait Parameter (cm) | 10 min | t | p | 20 min | t | p | 30 min | t | p | |
|---|---|---|---|---|---|---|---|---|---|---|
| Step Length | Right W/O Exo | 72.96 ± 1.41 | 4.181 | <0.00 ** | 72.11 ± 1.24 | −0.279 | 0.782 | 71.53 ± 1.72 | −7.191 | <0.00 ** |
| Right W/Exo | 71.57 ± 1.80 | 72.22 ± 1.49 | 75.11 ± 2.65 | |||||||
| Left W/O Exo | 75.06 ± 1.24 | 12.568 | <0.00 ** | 71.63 ± 1.45 | −0.148 | 0.883 | 72.08 ± 1.27 | −11.046 | <0.00 ** | |
| Left W/Exo | 72.12 ± 1.32 | 71.69 ± 1.55 | 75.92 ± 1.55 | |||||||
| Stride Length | W/O Exo | 148.03 ± 2.62 | 8.366 | <0.00 ** | 143.74 ± 1.88 | −0.287 | 0.776 | 143.61 ± 2.67 | −9.573 | <0.00 ** |
| W/Exo | 143.70 ± 2.82 | 143.91 ± 2.35 | 151.04 ± 3.92 | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.-J.; Nam, Y.-G.; Yu, J.-H.; Kim, J.-S. Effect of Wearable Exoskeleton Robots on Muscle Activation and Gait Parameters on a Treadmill: A Randomized Controlled Trial. Healthcare 2025, 13, 700. https://doi.org/10.3390/healthcare13070700
Lee K-J, Nam Y-G, Yu J-H, Kim J-S. Effect of Wearable Exoskeleton Robots on Muscle Activation and Gait Parameters on a Treadmill: A Randomized Controlled Trial. Healthcare. 2025; 13(7):700. https://doi.org/10.3390/healthcare13070700
Chicago/Turabian StyleLee, Kyung-Jin, Yeon-Gyo Nam, Jae-Ho Yu, and Jin-Seop Kim. 2025. "Effect of Wearable Exoskeleton Robots on Muscle Activation and Gait Parameters on a Treadmill: A Randomized Controlled Trial" Healthcare 13, no. 7: 700. https://doi.org/10.3390/healthcare13070700
APA StyleLee, K.-J., Nam, Y.-G., Yu, J.-H., & Kim, J.-S. (2025). Effect of Wearable Exoskeleton Robots on Muscle Activation and Gait Parameters on a Treadmill: A Randomized Controlled Trial. Healthcare, 13(7), 700. https://doi.org/10.3390/healthcare13070700






