Evaluating the Agreement and Associations with Physical Function Between Equation- and Linear Position Transducer-Estimated Sit-to-Stand Muscle Power in Aging Adults
Abstract
:1. Introduction
2. Materials and Methods
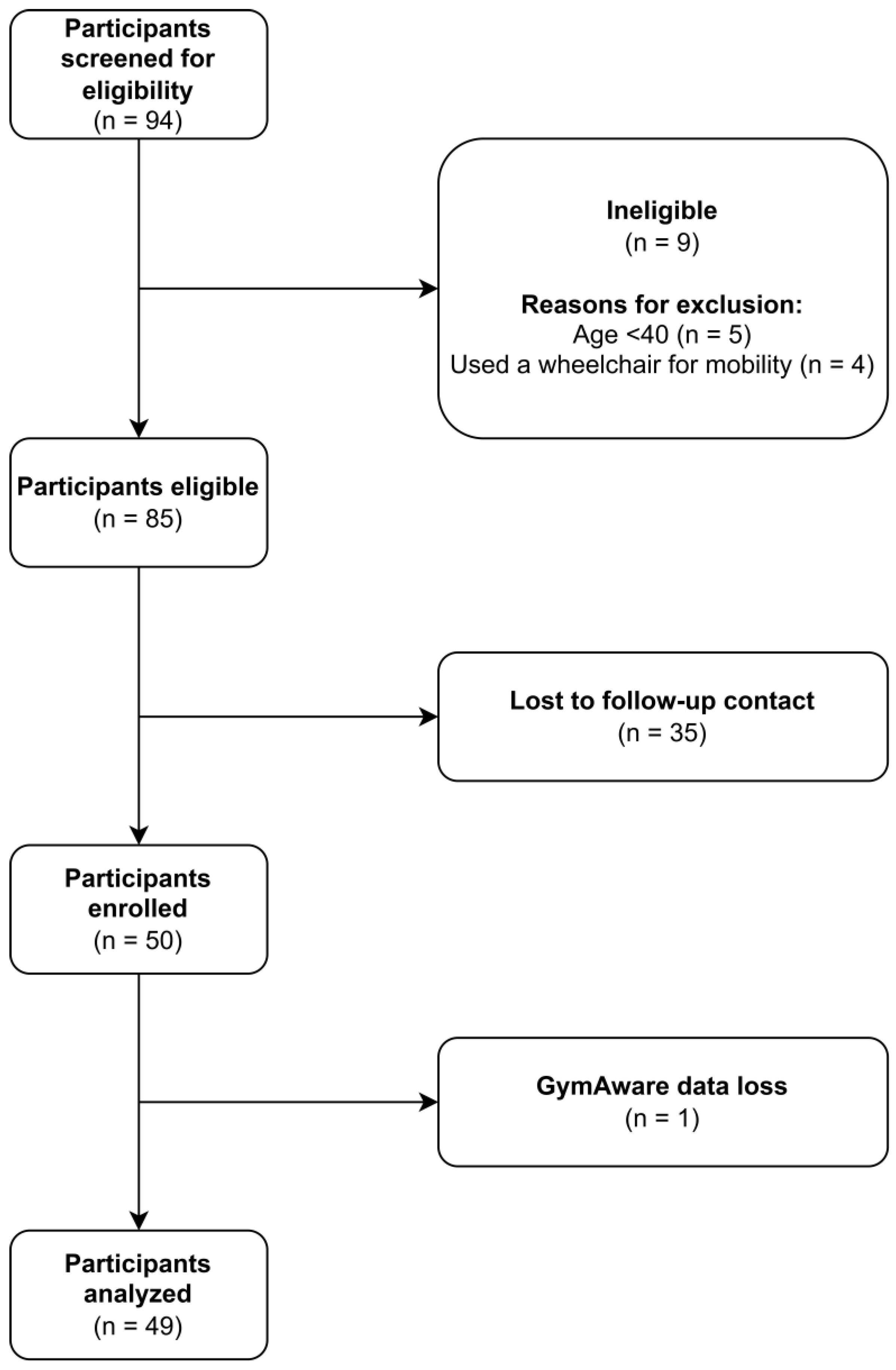
2.1. Participants
2.2. Sociodemographic Variables, Anthropometrics, and Body Composition
2.3. STS Power Assessments
2.4. Objective Physical Function Outcomes
2.5. Self-Report Physical Function
2.6. Power Calculation
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PF | physical function |
| EQ | equation |
| STS | sit-to-stand |
| UGS | usual gait speed |
| FGS | fast gait speed |
| TUG | timed up-and-go |
| LPT | linear position transducer |
| BMI | body mass index |
| HGS | handgrip strength |
| 400MWT | 400 m walk test |
| LLFDI | Late-Life Function and Disability Instrument |
| Std. β | standardized beta coefficient |
References
- Alcazar, J.; Losa-Reyna, J.; Rodriguez-Lopez, C.; Alfaro-Acha, A.; Rodriguez-Mañas, L.; Ara, I.; García-García, F.J.; Alegre, L.M. The sit-to-stand muscle power test: An easy, inexpensive and portable procedure to assess muscle power in older people. Exp. Gerontol. 2018, 112, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Reid, K.F.; Fielding, R.A. Skeletal Muscle Power: A Critical Determinant of Physical Functioning in Older Adults. Exerc. Sport Sci. Rev. 2012, 40, 4–12. [Google Scholar] [CrossRef]
- Bean, J.F.; Kiely, D.K.; Herman, S.; Leveille, S.G.; Mizer, K.; Frontera, W.R.; Fielding, R.A. The Relationship Between Leg Power and Physical Performance in Mobility-Limited Older People. J. Am. Geriatr. Soc. 2002, 50, 461–467. [Google Scholar] [PubMed]
- Bean, J.F.; Kiely, D.K.; Larose, S.; Goldstein, R.; Frontera, W.R.; Leveille, S.G. Are changes in leg power responsible for clinically meaningful improvements in mobility in older adults? J. Am. Geriatr. Soc. 2010, 58, 2363–2368. [Google Scholar] [CrossRef]
- Orange, S.T.; Metcalfe, J.W.; Liefeith, A.; Jordan, A.R. Validity of various portable devices to measure sit-to-stand velocity and power in older adults. Gait Posture 2020, 76, 409–414. [Google Scholar] [CrossRef]
- Simpkins, C.; Yang, F. Muscle power is more important than strength in preventing falls in community-dwelling older adults. J. Biomech. 2022, 134, 111018. [Google Scholar] [CrossRef]
- Steinbrink, G.M.; Martinez, J.; Swartz, A.M.; Strath, S.J. Sit-to-Stand Power Is a Stronger Predictor of Gait Speed than Knee Extension Strength. J. Funct. Morphol. Kinesiol. 2024, 9, 103. [Google Scholar] [CrossRef]
- Alcazar, J.; Navarrete-, D.; Mañas, A.; Alegre, L.M.; Villa, G.; Cabello, A.G.-; Pedrero-, R.; Gusi, N.; González-, M.; Casajús, J.A.; et al. ‘Fat but powerful ’ paradox: Association of muscle power and adiposity markers with all-cause mortality in older adults from the EXERNET multicentre study. Br. J. Sports Med. 2021, 55, 1204–1211. [Google Scholar] [CrossRef]
- Freitas, S.; Cruz-Montecinos, C.; Ratel, S.; Pinto, R. Powerpenia: Should it be considered a biomarker of healthy aging? Sports Med.-Open 2024, 10, 27. [Google Scholar] [CrossRef]
- Alcazar, J.; Guadalupe-Grau, A.; García-García, F.J.; Ara, I.; Alegre, L.M. Skeletal Muscle Power Measurement in Older People: A Systematic Review of Testing Protocols and Adverse Events. J. Gerontol.-Ser. A Biol. Sci. Med. Sci. 2018, 73, 914–924. [Google Scholar] [CrossRef]
- Baltasar-Fernandez, I.; Alcazar, J.; Losa-Reyna, J.; Soto-Paniagua, H.; Alegre, L.M.; Takai, Y.; Ruiz-Cárdenas, J.D.; Signorile, J.F.; Rodriguez-Mañas, L.; García-García, F.J.; et al. Comparison of available equations to estimate sit-to-stand muscle power and their association with gait speed and frailty in older people: Practical applications for the 5-rep sit-to-stand test. Exp. Gerontol. 2021, 156, 111619. [Google Scholar] [CrossRef] [PubMed]
- Losa-Reyna, J.; Alcazar, J.; Carnicero, J.; Alfaro-Acha, A.; Castillo-Gallego, C.; Rosado-Artalejo, C.; Rodríguez-Mañas, L.; Ara, I.; García-García, F.J. Impact of Relative Muscle Power on Hospitalization and All-Cause Mortality in Older Adults. J. Gerontol. Ser. A 2021, 77, 781–789. [Google Scholar] [CrossRef] [PubMed]
- Baltasar-Fernandez, I.; Alcazar, J.; Martín-Braojos, S.; Ara, I.; Alegre, L.M.; García-García, F.J.; Alfaro-Acha, A.; Losa-Reyna, J. Power-oriented resistance training combined with high-intensity interval training in pre-frail and frail older people: Comparison between traditional and cluster training set configurations on the force–velocity relationship, physical function and frailty. Eur. J. Appl. Physiol. 2023, 124, 623–632. [Google Scholar] [CrossRef]
- Lanzi, S.; Pousaz, A.; Calanca, L.; Mazzolai, L. Sit-to-stand muscle power is related to functional performance at baseline and after supervised exercise training in patients with lower extremity peripheral artery disease. Eur. J. Vasc. Endovasc. Surg. 2022, 65, 512–527. [Google Scholar] [CrossRef]
- Baltasar-Fernandez, I.; Alcazar, J.; Rodriguez-Lopez, C.; Losa-Reyna, J.; Alonso-Seco, M.; Ara, I.; Alegre, L.M. Sit-to-stand muscle power test: Comparison between estimated and force plate-derived mechanical power and their association with physical function in older adults. Exp. Gerontol. 2021, 145, 111213. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.Y.; Wei, S.H.; Chen, P.Y.; Tsai, M.W.; Cheng, I.C.; Liu, D.H.; Kao, C.L. Can sit-to-stand lower limb muscle power predict fall status? Gait Posture 2014, 40, 403–407. [Google Scholar] [CrossRef]
- Tateoka, K.; Tsuji, T.; Shoji, T.; Tokunaga, S.; Okura, T. Relationship between Acceleration in a Sit-To-Stand Movement and Physical Function in Older Adults. Geriatrics 2023, 8, 123. [Google Scholar] [CrossRef]
- Van Lummel, R.C.; Walgaard, S.; Maier, A.B.; Ainsworth, E.; Beek, P.J.; Van Dieën, J.H. The instrumented Sit-To-Stand test (iSTS) has greater clinical relevance than the manually recorded sit-to-stand test in older adults. PLoS ONE 2016, 11, e0157968. [Google Scholar] [CrossRef]
- Gray, M.; Paulson, S. Developing a measure of muscular power during a functional task for older adults. BMC Geriatr. 2014, 14, 145. [Google Scholar] [CrossRef]
- Sherwood, J.J.; Inouye, C.; Webb, S.L.; Jenny, O. Reliability and validity of the sit-to-stand as a muscular power measure in older adults. J. Aging Phys. Act. 2020, 28, 455–466. [Google Scholar] [CrossRef]
- Balachandran, A.T.; Vigotsky, A.D.; Quiles, N.; Mokkink, L.B.; Belio, M.A.; Glenn, J.M.K. Validity, reliability, and measurement error of a sit-to-stand power test in older adults: A pre-registered study. Exp. Gerontol. 2021, 145, 111202. [Google Scholar] [CrossRef] [PubMed]
- Glenn, J.M.; Gray, M.; Binns, A. Relationship of Sit-to-Stand Lower-Body Power With Functional Fitness Measures Among Older Adults With and Without Sarcopenia. J. Geriatr. Phys. Ther. 2017, 40, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Alcazar, J.; Alegre, L.M.; Van Roie, E.; Magalhães, J.P.; Nielsen, B.R.; González-Gross, M.; Júdice, P.B.; Casajús, J.A.; Delecluse, C.; Sardinha, L.B.; et al. Relative sit-to-stand power: Aging trajectories, functionally relevant cut-off points, and normative data in a large European cohort. J. Cachexia Sarcopenia Muscle 2021, 12, 921–932. [Google Scholar] [CrossRef]
- Hetherington-Rauth, M.; Magalhães, J.P.; Alcazar, J.; Rosa, G.B.; Correia, I.R.; Ara, I.; Sardinha, L.B. Relative Sit-to-Stand Muscle Power Predicts an Older Adult’s Physical Independence at Age of 90 Yrs Beyond That of Relative Handgrip Strength, Physical Activity, and Sedentary Time: A Cross-sectional Analysis. Am. J. Phys. Med. Rehabil. 2022, 101, 995–1000. [Google Scholar] [CrossRef]
- Ramírez-Vélez, R.; Izquierdo, M.; García-Hermoso, A.; Ordoñez-Mora, L.T.; Cano-Gutierrez, C.; Campo-Lucumí, F.; Pérez-Sousa, M.Á. Sit to stand muscle power reference values and their association with adverse events in Colombian older adults. Sci. Rep. 2022, 12, 11820. [Google Scholar] [CrossRef]
- Losa-Reyna, J.; Alcazar, J.; Rodríguez-Gómez, I.; Alfaro-Acha, A.; Alegre, L.M.; Rodríguez-Mañas, L.; Ara, I.; García-García, F.J. Low relative mechanical power in older adults: An operational definition and algorithm for its application in the clinical setting. Exp. Gerontol. 2020, 142, 111141. [Google Scholar] [CrossRef] [PubMed]
- Campitelli, A.; Paulson, S.; Vincenzo, J.; Glenn, J.M.; Gills, J.L.; Jones, M.D.; Powers, M.; Gray, M. Sit-to-Stand Power Across the Lifespan: A Cross-Sectional Analysis. J. Aging Phys. Act. 2021, 30, 678–688. [Google Scholar] [CrossRef]
- Orange, S.T.; Marshall, P.; Madden, L.A.; Vince, R.V. Can sit-to-stand muscle power explain the ability to perform functional tasks in adults with severe obesity? J. Sports Sci. 2019, 37, 1227–1234. [Google Scholar] [CrossRef]
- Balachandran, A.T.; Orange, S.T.; Wang, Y.; Lustin, R.; Vega, A.; Quiles, N. Comparison of two popular transducers to measure sit-to-stand power in older adults. PLoS ONE 2024, 19, e0308808. [Google Scholar] [CrossRef]
- Vaishya, R.; Misra, A.; Vaish, A.; Ursino, N.; D’Ambrosi, R. Hand grip strength as a proposed new vital sign of health: A narrative review of evidences. J. Health Popul. Nutr. 2024, 43, 7. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed Up and Go: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Peters, D.M.; Fritz, S.L.; Krotish, D.E. Assessing the Reliability and Validity of a Shorter Walk Test Compared With the 10-Meter Walk Test for Measurements of Gait Speed in Healthy, Older Adults. J. Geriatr. Phys. Ther. 2013, 36, 24–30. [Google Scholar] [CrossRef]
- Abellan Van Kan, G.; Rolland, Y.; Andrieu, S.; Bauer, J.; Beauchet, O.; Bonnefoy, M.; Cesari, M.; Donini, L.M.; Gillette-Guyonnet, S.; Inzitari, M.; et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J. Nutr. Health Aging 2009, 13, 881–889. [Google Scholar] [CrossRef] [PubMed]
- McGrath, B.M.; Johnson, P.J.; Mcgrath, R.; Cawthon, P.M.; Klawitter, L.; Choi, B. A Matched Cohort Analysis for Examining the Association Between Slow Gait Speed and Shortened Longevity in Older Americans. J. Appl. Gerontol. 2022, 41, 1905–1913. [Google Scholar] [CrossRef] [PubMed]
- Middleton, A.; Fritz, S.L.; Lusardi, M. Walking speed: The functional vital sign. J. Aging Phys. Act. 2015, 23, 314–322. [Google Scholar] [CrossRef]
- Raisi, A.; Zerbini, V.; Myers, J.; Masotti, S.; Piva, T.; Lordi, R.; Chiaranda, G.; Grazzi, G.; Mazzoni, G.; Mandini, S. Moderate walking speed and survival association across 23-years follow-up in female patients with cardiovascular disease. Int. J. Cardiol. 2022, 371, 371–376. [Google Scholar] [CrossRef]
- Gray, M.; Paulson, S.; Powers, M. Maximal, Not Habitual, Walking Velocity is More Highly Correlated to Functional Fitness of Community-Dwelling Older Adults. J. Aging Phys. Act. 2016, 24, 305–310. [Google Scholar] [CrossRef]
- Simonsick, E.M.; Fan, E.; Fleg, J.L. Estimating Cardiorespiratory Fitness in Well-Functioning Older Adults: Treadmill Validation of the Long Distance Corridor Walk: Estimating Fitness in Older Adults. J. Am. Geriatr. Soc. 2006, 54, 127–132. [Google Scholar] [CrossRef]
- Vestergaard, S.; Patel, K.V.; Bandinelli, S.; Ferrucci, L.; Guralnik, J.M. Characteristics of 400-meter walk test performance and subsequent mortality in older adults. Rejuvenation Res. 2009, 12, 177–184. [Google Scholar] [CrossRef]
- Newman, A.B.; Simonsick, E.M.; Naydeck, B.L.; Boudreau, R.M.; Kritchevsky, S.B.; Nevitt, M.C.; Pahor, M.; Satterfield, S.; Brach, J.S.; Studenski, S.A.; et al. Association of Long-Distance Corridor Walk Performance With Mortality, Cardiovascular Disease, Mobility Limitation, and Disability. JAMA 2006, 295, 2018. [Google Scholar] [CrossRef]
- Sayers, S.P.; Jette, A.M.; Haley, S.M.; Heeren, T.C.; Guralnik, J.M.; Fielding, R.A. Validation of the Late-Life Function and Disability Instrument: Validation of LLFDI. J. Am. Geriatr. Soc. 2004, 52, 1554–1559. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Int. J. Nurs. Stud. 2010, 47, 931–936. [Google Scholar] [CrossRef]
- Ranganathan, P.; Pramesh, C.; Aggarwal, R. Common pitfalls in statistical analysis: Measures of agreement. Perspect. Clin. Res. 2017, 8, 187. [Google Scholar] [CrossRef]
- Garcia-Aguirre, M.; Baltasar-Fernandez, I.; Alcazar, J.; Losa-Reyna, J.; Alfaro-Acha, A.; Ara, I.; Rodriguez-Mañas, L.; Alegre, L.M.; Garcia-Garcia, F.J. Cut-Off Points for Low Relative 30-s Sit-to-Stand Power and Their Associations With Adverse Health Conditions. J. Cachexia Sarcopenia Muscle 2025, 16, e13676. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, L.; Bochicchio, G.; Bottari, A.; Lucertini, F.; Scarton, A.; Pogliaghi, S. Estimating Muscle Power of the Lower Limbs through the 5-Sit-to-Stand Test: A Comparison of Field vs. Laboratory Method. Appl. Sci. 2022, 12, 11577. [Google Scholar] [CrossRef]
- Moreno-Villanueva, A.; Pino-Ortega, J.; Rico-González, M. Validity and reliability of linear position transducers and linear velocity transducers: A systematic review. Sports Biomech. 2021, 23, 1340–1369. [Google Scholar] [CrossRef]
- Gurses, H.N.; Zeren, M.; Denizoglu Kulli, H.; Durgut, E. The relationship of sit-to-stand tests with 6-minute walk test in healthy young adults. Medicine 2018, 97, e9489. [Google Scholar] [CrossRef]
- Gephine, S.; Frykholm, E.; Nyberg, A.; Mucci, P.; Van Hees, H.W.H.; Lemson, A.; Klijn, P.; Maltais, F.; Saey, D. Specific Contribution of Quadriceps Muscle Strength, Endurance, and Power to Functional Exercise Capacity in People With Chronic Obstructive Pulmonary Disease: A Multicenter Study. Phys. Ther. 2021, 101, pzab052. [Google Scholar] [CrossRef]
- Stavrinou, P.S.; Aphamis, G.; Pantzaris, M.; Sakkas, G.K.; Giannaki, C.D. Exploring the Associations between Functional Capacity, Cognitive Function and Well-Being in Older Adults. Life 2022, 12, 1042. [Google Scholar] [CrossRef]
- Hafer, J.F.; Boyer, K.A. Comparisons of knee extensor functional demand during gait by age, physical activity level, and the impact of acute exercise and walking speed. J. Appl. Biomech. 2020, 36, 163–170. [Google Scholar] [CrossRef]
- Zanker, J.; Scott, D.; Alajlouni, D.; Kirk, B.; Bird, S.; DeBruin, D.; Vogrin, S.; Bliuc, D.; Tran, T.; Cawthon, P.; et al. Mortality, falls and slow walking speed are predicted by different muscle strength and physical performance measures in women and men. Arch. Gerontol. Geriatr. 2023, 114, 105084. [Google Scholar] [CrossRef] [PubMed]
- Villareal, D.T.; Aguirre, L.; Gurney, A.B.; Waters, D.L.; Sinacore, D.R.; Colombo, E.; Armamento-Villareal, R.; Qualls, C. Aerobic or Resistance Exercise, or Both, in Dieting Obese Older Adults. N. Engl. J. Med. 2017, 376, 1943–1955. [Google Scholar] [CrossRef] [PubMed]
- Alcazar, J.; Kamper, R.S.; Aagaard, P.; Haddock, B.; Prescott, E.; Ara, I.; Suetta, C. Relation between leg extension power and 30-s sit-to-stand muscle power in older adults: Validation and translation to functional performance. Sci. Rep. 2020, 10, 16337. [Google Scholar] [CrossRef] [PubMed]
- Pulignano, G.; Del Sindaco, D.; Di Lenarda, A.; Alunni, G.; Senni, M.; Tarantini, L.; Cioffi, G.; Tinti, M.D.; Barbati, G.; Minardi, G.; et al. Incremental Value of Gait Speed in Predicting Prognosis of Older Adults With Heart Failure. JACC Heart Fail. 2016, 4, 289–298. [Google Scholar] [CrossRef]
- Mercieca-Bebber, R.; King, M.T.; Calvert, M.J.; Stockler, M.R.; Friedlander, M. The importance of patient-reported outcomes in clinical trials and strategies for future optimization. Patient Relat. Outcome Meas. 2018, 9, 353–367. [Google Scholar] [CrossRef]

| Characteristic | N = 49 1 |
|---|---|
| Age, years | 61 (11) |
| Sex | |
| Male | 16 (33%) |
| Female | 33 (67%) |
| Race and ethnicity | |
| Hispanic | 1 (2.0%) |
| NH Asian | 1 (2.0%) |
| NH Black | 1 (2.0%) |
| NH White | 44 (90%) |
| NH More than one race | 2 (4.1%) |
| BMI, kg/m2 | 26.4 (5.2) |
| EQ STS power, W/kg | 2.95 (0.98) |
| LPT STS power, W/kg | 5.69 (1.64) |
| Handgrip strength, kg/kg | 0.47 (0.13) |
| Timed up-and-go, s | 8.98 (1.81) |
| Usual gait speed, m/s | 1.37 (0.20) |
| Fast gait speed, m/s | 2.01 (0.34) |
| 400 m walk, s | 248 (44) |
| LLFDI total physical function | 81 (12) |
| LLFDI basic lower-body physical function | 92 (11) |
| LLFDI advanced lower-body physical function | 79 (15) |
| Variable | Handgrip Strength | Timed Up-and-Go | Usual Gait Speed | Fast Gait Speed | 400 m Walk Test | LLFDI Total Function | LLFDI Basic Lower-Body Function | LLFDI Advanced Lower-Body Function |
|---|---|---|---|---|---|---|---|---|
| EQ STS power | 0.37 | −0.52 | 0.49 | 0.61 | −0.70 | 0.54 | 0.51 | 0.51 |
| LPT STS power | 0.53 | −0.38 | 0.42 | 0.55 | −0.67 | 0.52 | 0.48 | 0.51 |
| Handgrip Strength | Timed Up-and-Go | Usual Gait Speed | Fast Gait Speed | 400 m Walk Test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Std. β | 95% CI | Std. β | 95% CI | Std. β | 95% CI | Std. β | 95% CI | Std. β | 95% CI | |
| EQ STS power | 0.19 | −0.10, 0.48 | −0.45 | −0.74, −0.17 | 0.37 | 0.08, 0.66 | 0.48 | 0.23, 0.74 | −0.55 | −0.77, −0.33 |
| LPT STS power | 0.44 | 0.18, 0.70 | −0.26 | −0.56, 0.04 | 0.28 | −0.01, 0.57 | 0.40 | 0.14, 0.66 | −0.51 | −0.73, −0.29 |
| LLFDI Total Function | LLFDI Basic Lower-Body Function | LLFDI Advanced Lower-Body Function | ||||
|---|---|---|---|---|---|---|
| Std. β | 95% CI | Std. β | 95% CI | Std. β | 95% CI | |
| EQ STS power | 0.30 | 0.05, 0.55 | 0.30 | 0.04, 0.57 | 0.30 | 0.03, 0.57 |
| LPT STS power | 0.31 | 0.07, 0.55 | 0.29 | 0.03, 0.55 | 0.32 | 0.06, 0.58 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steinbrink, G.; Danielson, T.; Martinez, J.; Patnode, J.; Swartz, A.; Strath, S. Evaluating the Agreement and Associations with Physical Function Between Equation- and Linear Position Transducer-Estimated Sit-to-Stand Muscle Power in Aging Adults. Healthcare 2025, 13, 905. https://doi.org/10.3390/healthcare13080905
Steinbrink G, Danielson T, Martinez J, Patnode J, Swartz A, Strath S. Evaluating the Agreement and Associations with Physical Function Between Equation- and Linear Position Transducer-Estimated Sit-to-Stand Muscle Power in Aging Adults. Healthcare. 2025; 13(8):905. https://doi.org/10.3390/healthcare13080905
Chicago/Turabian StyleSteinbrink, Garrett, Taylor Danielson, Julian Martinez, Joseph Patnode, Ann Swartz, and Scott Strath. 2025. "Evaluating the Agreement and Associations with Physical Function Between Equation- and Linear Position Transducer-Estimated Sit-to-Stand Muscle Power in Aging Adults" Healthcare 13, no. 8: 905. https://doi.org/10.3390/healthcare13080905
APA StyleSteinbrink, G., Danielson, T., Martinez, J., Patnode, J., Swartz, A., & Strath, S. (2025). Evaluating the Agreement and Associations with Physical Function Between Equation- and Linear Position Transducer-Estimated Sit-to-Stand Muscle Power in Aging Adults. Healthcare, 13(8), 905. https://doi.org/10.3390/healthcare13080905






