Leveraging Kaizen with Process Mining in Healthcare Settings: A Conceptual Framework for Data-Driven Continuous Improvement
Abstract
:1. Introduction
2. Methodological Approach
2.1. Selection Criteria
- Kaizen in Healthcare: Research focusing on the implementation of Kaizen methodologies in hospital operations, process optimization, and continuous improvement initiatives;
- PM Applications: Studies examining how PM has been applied in healthcare, particularly in workflow optimization, bottleneck identification, and compliance monitoring;
- Integrated Improvement Models: Articles exploring data-driven approaches in Lean healthcare and case studies where data analytics supported process improvement;
- Recent and High-Quality Sources: Peer-reviewed journal articles, case studies, and authoritative healthcare management reports published within the last 20 years.
2.2. Databases and Search Strategy
- Google Scholar—Searched for broad academic discussions on Kaizen, Process Mining, and healthcare process improvement;
- PubMed—Focused on healthcare applications of Lean and data-driven methodologies;
- IEEE Xplore and SpringerLink—Identified relevant studies on PM algorithms and their real-world applications;
- ProQuest and ScienceDirect—Sourced peer-reviewed case studies and empirical research on healthcare process optimization.
2.3. Analysis and Model Development
- Identification of Key Concepts—The literature was analyzed to extract the fundamental principles of Kaizen and PM;
- Comparative Analysis—A theoretical evaluation was conducted to compare traditional Kaizen approaches with PM-based methods;
- Framework Development—Insights were synthesized to design a conceptual model that integrates Kaizen and PM, ensuring synergy between employee-driven problem-solving and data-driven process optimization.
3. Theoretical Background
3.1. Traditional Kaizen Methodology in Healthcare Settings
3.1.1. Conceptual Framework and Implementation Approaches
3.1.2. Critical Success Factors and Barriers
3.1.3. Adaptability and Evolutionary Patterns
3.1.4. Outcome Patterns and Evidence Synthesis
3.2. Process Mining Fundamentals in Healthcare Settings
3.2.1. Fundamentals of Process Mining
3.2.2. Healthcare-Specific Applications
Application Domains and Methodological Patterns
Outcome Patterns and Implementation Benefits
Implementation Challenges and Mitigation Strategies
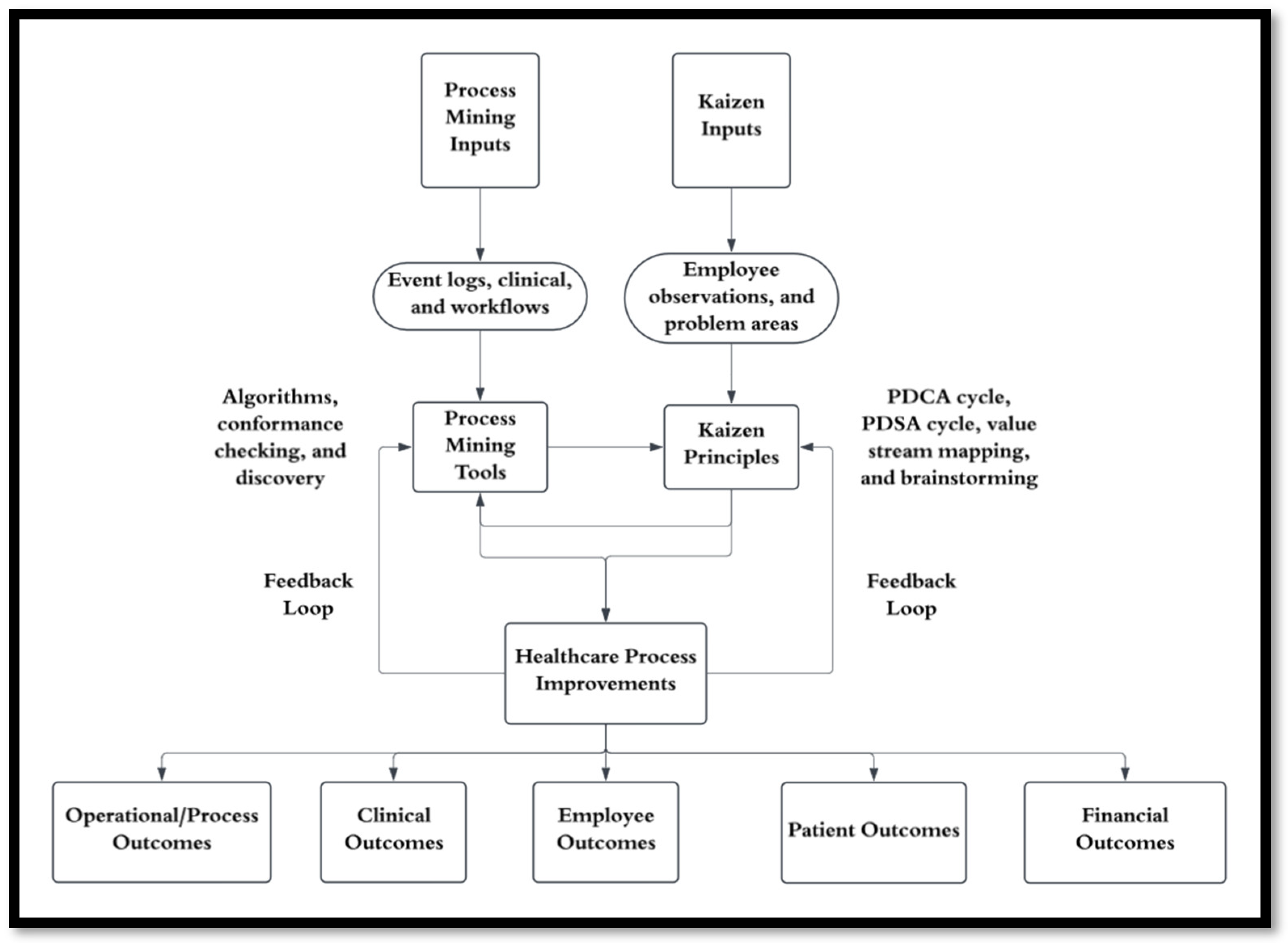
4. Proposed Integration Model
4.1. Objectives of the Integration
4.2. Key Components of the Model
4.2.1. Kaizen Principles
- Continuous Improvement: A focus on making incremental changes that collectively result in significant improvements in workflows and processes [70];
- Active Employee Involvement: Engaging healthcare staff at all levels, particularly frontline employees, in identifying and solving problems [71];
- Elimination of Inefficiencies: Addressing waste, delays, and unnecessary steps in healthcare workflows [72];
- Practical Insights: Ensuring that improvements are grounded in the day-to-day realities of healthcare operations [22];
- Tools and Methods: Table 1 represents the essential tools and methods used in Kaizen to support continuous improvement in healthcare operations.
4.2.2. Process Mining Tools
- Discovery Algorithms: These algorithms generate process models from event logs, revealing the actual flow of activities and uncovering inefficiencies, delays, and deviations [49];
- Conformance Checking: This technique compares discovered processes with predefined models to identify discrepancies and ensure compliance with clinical protocols and best practices [59];
4.2.3. Interaction Between Kaizen and Process Mining
Step 1: Data-Informed Problem Discovery
Step 2: Collaborative Root Cause Analysis
Step 3: Structured Implementation
Step 4: Data-Driven Validation
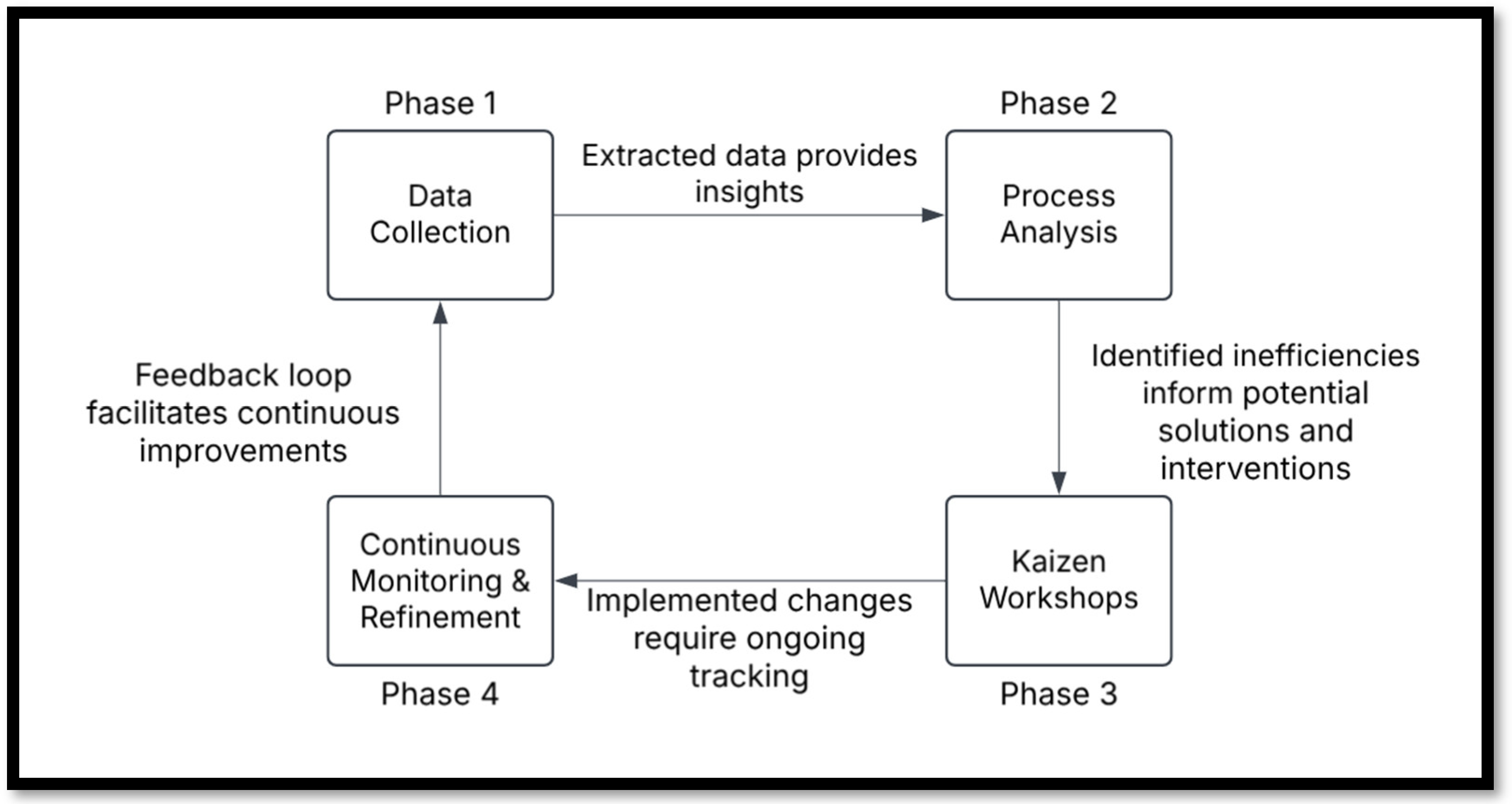
4.3. Phases of Implementation
4.3.1. Phase 1: Data Collection
4.3.2. Phase 2: Process Analysis
- Bottleneck analysis identifying critical pathway constraints (e.g., repetitive billing verification steps causing delays of up to 45 min in patient administrative processes) [90];
- Variant analysis showing deviations from standard care pathways (highlighting the most frequent alternative routes) [91];
- Performance indicators such as average case duration, processing times, and waiting times between activities;
- Social network analysis revealing handoff patterns between healthcare professionals [92].
4.3.3. Phase 3: Kaizen Events
4.3.4. Phase 4: Continuous Monitoring and Refinement
4.4. Implementation Considerations
4.5. Expected Outcomes
5. Validation and Application Scenarios
5.1. Validation Methodologies
5.2. Metrics for Assessing Effectiveness
- Error Reduction: A decrease in medication errors, scheduling conflicts, and process deviations would reflect the success of conformance checking and continuous process improvements [62];
- Resource Utilization: Comparing staff workload distribution, bed occupancy rates, and utilization before and after implementing the model can demonstrate optimization in resource allocation [122].
- Patient Outcomes: Patient feedback surveys and adherence to treatment protocols can serve as indicators of improved quality of care and patient experience [123];
- Employee Outcomes: Employee engagement and satisfaction are vital for sustaining continuous improvement efforts. Metrics such as workplace engagement levels, burnout and turnover rates, and participation in continuous improvement initiatives can provide insights into staff morale and the effectiveness of process changes [22].
- Clinical Effectiveness: Metrics such as reduced medical errors, reduced hospital readmission rates, fewer hospital-acquired conditions, and lower patient mortality and morbidity rates reflect the direct impact on patient health and safety [22].
- Cost and Utilization Metrics: Operational cost savings, reduced average length of hospital stay, increased reimbursement efficiency, and cost-effectiveness analyses help to quantify the financial value of integrated Kaizen–PM initiatives [22].
5.3. Illustrative Application Scenarios
6. Limitations and Future Research
6.1. Theoretical Constraints
6.2. Practical Challenges
6.3. Methodological Limitations
6.4. Opportunities for Future Research
- Empirical Validation: Conducting pilot studies or case studies in diverse healthcare settings is essential to evaluate the practical implementation of the framework and its impact on workflow efficiency, error reduction, and patient outcomes [149];
- AI and Advanced Analytics Integration: Exploring the incorporation of artificial intelligence and machine learning techniques to augment PM capabilities, such as predictive modeling for resource allocation or real-time decision support in healthcare processes [150];
- Cross-Sector Applications: Investigating the adaptability of this framework beyond healthcare, such as in manufacturing, education, or logistics, to assess its versatility and broader applicability. PM has been applied in various domains, and its methodologies can be tailored to different sectors to improve process efficiency and effectiveness [151]. Additionally, Kaizen has demonstrated its applicability across various sectors and industries [152];
- Data Quality Improvement: Developing standardized methods for cleaning and structuring healthcare data is crucial to ensure compatibility with PM tools and maximize the accuracy of insights. A perspective article explored how PM can extract clinical insights from mobile health data and complement data-driven techniques like machine learning, emphasizing the importance of data quality in such analyses [153];
- Human-Centric Adaptations: Examining strategies to further integrate frontline staff input and enhance their engagement in data-driven improvement processes, ensuring that the framework remains both actionable and practical [149].
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chiarini, A.; Baccarani, C.; Mascherpa, V. Lean Production, Toyota Production System and Kaizen Philosophy: A Conceptual Analysis from the Perspective of Zen Buddhism. TQM J. 2018, 30, 425–438. [Google Scholar] [CrossRef]
- Bortolotti, T.; Boscari, S.; Danese, P.; Medina Suni, H.A.; Rich, N.; Romano, P. The Social Benefits of Kaizen Initiatives in Healthcare: An Empirical Study. Int. J. Oper. Prod. Manag. 2018, 38, 554–578. [Google Scholar] [CrossRef]
- Ferreira, D.M.C.; Saurin, T.A. A Complexity Theory Perspective of Kaizen: A Study in Healthcare. Prod. Plan. Control. 2019, 30, 1337–1353. [Google Scholar] [CrossRef]
- Feldman, S.S.; Kennedy, K.C.; Nafziger, S.M.; Orewa, G.N.; Kpomblekou-Ademawou, E.; Hearld, K.R.; Hall, A.G. Critical Success Factors for Addressing Discharge Inefficiency at a Large Academic Medical Center: A Lean Six Sigma Approach. J. Nurs. Care Qual. 2022, 37, 135–141. [Google Scholar] [CrossRef]
- Johnson, J.K.; Barach, P. Tools and Strategies for Continuous Quality Improvement and Patient Safety. In Surgical Patient Care: Improving Safety, Quality and Value; Springer: Cham, Switzerland, 2017; pp. 121–132. [Google Scholar] [CrossRef]
- Dickson, E.W.; Anguelov, Z.; Vetterick, D.; Eller, A.; Singh, S. Use of Lean in the Emergency Department: A Case Series of 4 Hospitals. Ann. Emerg. Med. 2009, 54, 504–510. [Google Scholar] [CrossRef]
- Okpala, C.; Nwamekwe, C.O.; Ezeanyim, O.C.; Chikwendu, O.C.; Chiedu, O.; Onyeka, N.C. The Implementation of Kaizen Principles in Manufacturing Processes: A Pathway to Continuous Improvement. Int. J. Eng. Invent. 2024, 13, 116–124. [Google Scholar]
- Natale, J.; Uppal, R.; Wang, S. Improving Kaizen Event Success in Healthcare through Shorter Event Duration. Int. J. Collab. Enterp. 2014, 4, 3. [Google Scholar] [CrossRef]
- Franken, J.C.M.; van Dun, D.H.; Wilderom, C.P.M. Kaizen Event Process Quality: Towards a Phase-Based Understanding of High-Quality Group Problem-Solving. Int. J. Oper. Prod. Manag. 2021, 41, 962–990. [Google Scholar] [CrossRef]
- Aij, K.H.; Rapsaniotis, S. Leadership Requirements for Lean versus Servant Leadership in Health Care: A Systematic Review of the Literature. J. Healthc. Leadersh. 2017, 9, 1–14. [Google Scholar] [CrossRef]
- Danese, P.; Romano, P.; Medina Suni, H.A. Implementing Lean Management in Hospitals: A Survey on Social and Technical Outcomes of Kaizen Initiatives. Int. J. Prod. Res. 2024, 2024, 8745–8765. [Google Scholar] [CrossRef]
- Enticott, J.; Johnson, A.; Teede, H. Learning Health Systems Using Data to Drive Healthcare Improvement and Impact: A Systematic Review. BMC Health Serv. Res. 2021, 21, 200. [Google Scholar] [CrossRef]
- Fox, F.; Aggarwal, V.R.; Whelton, H.; Johnson, O. A Data Quality Framework for Process Mining of Electronic Health Record Data. In Proceedings of the 2018 IEEE International Conference on Healthcare Informatics, ICHI, New York, NY, USA, 4–7 June 2018; pp. 12–21. [Google Scholar] [CrossRef]
- Partington, A.; Wynn, M.; Suriadi, S.; Ouyang, C.; Karnon, J. Process Mining for Clinical Processes. ACM Trans. Manag. Inf. Syst. (TMIS) 2015, 5, 1–18. [Google Scholar] [CrossRef]
- Zhou, Z.; Wang, Y.; Li, L. Process Mining Based Modeling and Analysis of Workflows in Clinical Care—A Case Study in a Chicago Outpatient Clinic. In Proceedings of the 11th IEEE International Conference on Networking, Sensing and Control, ICNSC, Hangzhou, China, 18–20 October 2024; pp. 590–595. [Google Scholar] [CrossRef]
- Tlapa, D.; Tortorella, G.; Fogliatto, F.; Kumar, M.; Mac Cawley, A.; Vassolo, R.; Enberg, L.; Baez-Lopez, Y. Effects of Lean Interventions Supported by Digital Technologies on Healthcare Services: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 9018. [Google Scholar] [CrossRef]
- Yinusa, A.; Faezipour, M. Optimizing Healthcare Delivery: A Model for Staffing, Patient Assignment, and Resource Allocation. Appl. Syst. Innov. 2023, 6, 78. [Google Scholar] [CrossRef]
- Wiedermann, C.J.; Barbieri, V.; Engl, A.; Piccoliori, G. Relational Coordination at the Primary–Secondary Care Interface: Insights from a Cross-Sectional Survey in the South Tyrolean Healthcare System. Int. J. Environ. Res. Public Health 2024, 21, 425. [Google Scholar] [CrossRef]
- Albarqi, M.N. Assessing the Impact of Multidisciplinary Collaboration on Quality of Life in Older Patients Receiving Primary Care: Cross Sectional Study. Healthcare 2024, 12, 1258. [Google Scholar] [CrossRef] [PubMed]
- Walshe, N.; Ryng, S.; Drennan, J.; O’Connor, P.; O’Brien, S.; Crowley, C.; Hegarty, J. Situation Awareness and the Mitigation of Risk Associated with Patient Deterioration: A Meta-Narrative Review of Theories and Models and Their Relevance to Nursing Practice. Int. J. Nurs. Stud. 2021, 124, 104086. [Google Scholar] [CrossRef] [PubMed]
- Coelho, F.; Furtado, L.; Mendonça, N.; Soares, H.; Duarte, H.; Costeira, C.; Santos, C.; Sousa, J.P. Predisposing Factors to Medication Errors by Nurses and Prevention Strategies: A Scoping Review of Recent Literature. Nurs. Rep. 2024, 14, 1553–1569. [Google Scholar] [CrossRef]
- Haapatalo, E.; Reponen, E.; Torkki, P. Sustainability of Performance Improvements after 26 Kaizen Events in a Large Academic Hospital System: A Mixed Methods Study. BMJ Open 2023, 13, e071743. [Google Scholar] [CrossRef]
- Munoz-Gama, J.; Martin, N.; Fernandez-Llatas, C.; Johnson, O.A.; Sepúlveda, M.; Helm, E.; Galvez-Yanjari, V.; Rojas, E.; Martinez-Millana, A.; Aloini, D.; et al. Process Mining for Healthcare: Characteristics and Challenges. J. Biomed. Inf. 2022, 127, 103994. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A Typology of Reviews: An Analysis of 14 Review Types and Associated Methodologies. Health Info Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Tranfield, D.; Denyer, D.; Smart, P. Towards a Methodology for Developing Evidence-Informed Management Knowledge by Means of Systematic Review. Br. J. Manag. 2003, 14, 207–222. [Google Scholar] [CrossRef]
- Meredith, J. Theory Building through Conceptual Methods. Int. J. Oper. Prod. Manag. 1993, 13, 3–11. [Google Scholar] [CrossRef]
- Snyder, H. Literature Review as a Research Methodology: An Overview and Guidelines. J. Bus. Res. 2019, 104, 333–339. [Google Scholar] [CrossRef]
- Abuzied, Y. A Practical Guide to the Kaizen Approach as a Quality Improvement Tool. Glob. J. Qual. Saf. Healthc. 2022, 5, 79–81. [Google Scholar] [CrossRef] [PubMed]
- Schonberger, R.J. Reconstituting Lean in Healthcare: From Waste Elimination toward ‘Queue-Less’ Patient-Focused Care. Bus. Horiz. 2018, 61, 13–22. [Google Scholar] [CrossRef]
- Smith, I.M.; Smith, D.T.L. Mass Production Methods for Mass Vaccination: Improving Flow and Operational Performance in a COVID-19 Mass Vaccination Centre Using Lean. BMJ Open Qual. 2021, 10, e001525. [Google Scholar] [CrossRef]
- van Elp, B.; Roemeling, O.; Aij, K.H. Lean Leadership: Towards Continuous Improvement Capability in Healthcare. Health Serv. Manag. Res. 2022, 35, 7–15. [Google Scholar] [CrossRef]
- Shatrov, K.; Pessina, C.; Huber, K.; Thomet, B.; Gutzeit, A.; Blankart, C.R. Improving Health Care from the Bottom up: Factors for the Successful Implementation of Kaizen in Acute Care Hospitals. PLoS ONE 2021, 16, e0257412. [Google Scholar] [CrossRef]
- Abdallah, A.B.; Alkhaldi, R.Z. Lean Bundles in Health Care: A Scoping Review. J. Health Organ. Manag. 2019, 33, 488–510. [Google Scholar] [CrossRef]
- Zeferino, A.C.; Santos, G.N.; Queiroz, T.L.; Ramos, J.R.S. Evaluation of the Application of Continuous Improvement Based on the Kaizen Concept in Emergency Healthcare Units. Meta Aval. 2023, 1–22. [Google Scholar] [CrossRef]
- Courter, B.; Gardner, C.; McCrory, B. LEAN Rural Healthcare: Improving Rural Critical Access Hospital Laboratory Workflow to Optimize Processes. Proc. Int. Symp. Hum. Factors Ergon. Health Care 2024, 13, 205–210. [Google Scholar] [CrossRef]
- Flug, J.A.; Stellmaker, J.A.; Tollefson, C.D.; Comstock, E.M.; Buelna, E.; Truman, B.; Ponce, L.; Milosek, A.; McCabe, J.; Jokerst, C.E. Improving Turnaround Time in a Hospital-Based CT Division with the Kaizen Method. Radiographics 2022, 42, E125–E131. [Google Scholar] [CrossRef]
- Lian, B. Adoption of Network and Plan-Do-Check-Action in the International Classification of Disease 10 Coding. World J. Clin. Cases 2024, 12, 3734–3743. [Google Scholar] [CrossRef]
- Ishijima, H.; Miyamoto, N.; Masaule, F.; John, R. Improvements to Healthcare Waste Management at Regional Referral Hospitals in Tanzania Using the KAIZEN Approach. TQM J. 2022, 34, 939–956. [Google Scholar] [CrossRef]
- Velarde, S.; Kefalakis, K.; Hines, P. Remote Kaizen Events: A Response to COVID-19 and the New Normal. Total Qual. Manag. Bus. Excell. 2024, 35, 1378–1417. [Google Scholar] [CrossRef]
- AlZamel, O.N.; Abuawwad, L.M.; Alrabgi, K.A.; Alghamdi, M.A.; Sewaralthahab, S. Kaizen-Led Utilization Improvement at Medical Oncology Daycare Unit. JCO Oncol. Pract. 2024, 20, 293. [Google Scholar] [CrossRef]
- Denicolo, K.S.; Corboy, J.B.; Simon, N.J.E.; Balsley, K.J.; Skarzynski, D.J.; Roben, E.C.; Alpern, E.R. Multidisciplinary Kaizen Event to Improve Adherence to a Sepsis Clinical Care Guideline. Pediatr. Qual. Saf. 2021, 6, E435. [Google Scholar] [CrossRef]
- Curtin, A.G.; Anderson, V.; Brockhus, F.; Cohen, D.R. Novel Team-Based Approach to Quality Improvement Effectively Engages Staff and Reduces Adverse Events in Healthcare Settings. BMJ Open Qual. 2020, 9, e000741. [Google Scholar] [CrossRef]
- Jans, M.; Laghmouch, M. Process Mining for Detailed Process Analysis. In Advanced Digital Auditing: Theory and Practice of Auditing Complex Information Systems and Technologies; Berghout, E., Fijneman, R., Hendriks, L., de Boer, M., Butijn, B.-J., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 237–256. ISBN 978-3-031-11089-4. [Google Scholar]
- van der Aalst, W.M.P. Process Mining: A 360 Degree Overview. In Process Mining Handbook; van der Aalst, W.M.P., Carmona, J., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 3–34. ISBN 978-3-031-08848-3. [Google Scholar]
- Augusto, A.; Mendling, J.; Vidgof, M.; Wurm, B. The Connection between Process Complexity of Event Sequences and Models Discovered by Process Mining. Inf. Sci. 2022, 598, 196–215. [Google Scholar] [CrossRef]
- Rinderle-Ma, S.; Stertz, F.; Mangler, J.; Pauker, F. Process Mining—Discovery, Conformance, and Enhancement of Manufacturing Processes. In Digital Transformation: Core Technologies and Emerging Topics from a Computer Science Perspective; Vogel-Heuser, B., Wimmer, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2023; pp. 363–383. ISBN 978-3-662-65004-2. [Google Scholar]
- Maeyens, J.; Vorstermans, A.; Verbeke, M. Process Mining on Machine Event Logs for Profiling Abnormal Behaviour and Root Cause Analysis. Ann. Telecommun. 2020, 75, 563–572. [Google Scholar] [CrossRef]
- Lamghari, Z. Process Mining: A New Approach for Simplifying the Process Model Control Flow Visualization. Transdiscipl. J. Eng. Sci. 2022, 13, 205–218. [Google Scholar] [CrossRef]
- Rehse, J.-R.; Leemans, S.J.J.; Fettke, P.; van der Werf, J.M.E.M. On Process Discovery Experimentation: Addressing the Need for Research Methodology in Process Discovery. ACM Trans. Softw. Eng. Methodol. 2025, 34, 1–29. [Google Scholar] [CrossRef]
- Das, S.; BALA, P. Process Mining for Social and Economic Needs: An Introduction. In Handbook of Research on Digitalization Solutions for Social and Economic Needs; IGI Global: Hershey, PA, USA, 2023; pp. 140–154. ISBN 9781668441022. [Google Scholar]
- Julca, M.A.R.D.; Cardenas, A.R.L.; Armas-Aguirre, J.; Mayorga, S.A. Optimization Model for Healthcare Processes Using Process Mining. In Proceedings of the Iberian Conference on Information Systems and Technologies, CISTI, Aveiro, Portugal, 20–23 June 2023. [Google Scholar] [CrossRef]
- Rojas, E.; Munoz-Gama, J.; Sepúlveda, M.; Capurro, D. Process Mining in Healthcare: A Literature Review. J. Biomed. Inf. 2016, 61, 224–236. [Google Scholar] [CrossRef]
- D’Angelis, O.; Lapadula, V.; Iacuitto, M.; Ivziku, D.; Sabatini, A.; Vollero, L.; Merone, M. Application of Process Mining in the Management of Inpatient Analysis. In Proceedings of the 2023 IEEE International Symposium on Medical Measurements and Applications, MeMeA 2023—Conference Proceedings, Jeju, Republic of Korea, 14–16 June 2023. [Google Scholar] [CrossRef]
- Mohammadi, F.; Kazempourian, S.; Vanani, I.R. Process Mining Approach to Performance Analysis and Bottleneck Finding in Electronic Processes (Case Study: The Billing Process of Hospital Services). Int. J. Process Manag. Benchmarking 2023, 13, 212. [Google Scholar] [CrossRef]
- Matonya, M.M.; Pusztai, L.; Budai, I. Optimizing Healthcare Business Processes with Process Mining Software: A Comparative Analysis. Decis. Mak. Appl. Manag. Eng. 2024, 7, 380–400. [Google Scholar] [CrossRef]
- Mansur, S.S.; Kurniati, A.P.; Rojas, E. Adiwijaya Process Mining to Improve Clinical Pathways in Breast Cancer Treatment Using the Indonesia Health Insurance Dataset. In Proceedings of the 2024 12th International Conference on Information and Communication Technology, ICoICT, Bandung, Indonesia, 7–8 August 2024; pp. 173–180. [Google Scholar] [CrossRef]
- Bakhshi, A.; Hassannayebi, E.; Sadeghi, A.H. Optimizing Sepsis Care through Heuristics Methods in Process Mining: A Trajectory Analysis. Healthc. Anal. 2023, 3, 100187. [Google Scholar] [CrossRef]
- Kropp, T.; Faeghi, S.; Lennerts, K. Evaluation of Patient Transport Service in Hospitals Using Process Mining Methods: Patients’ Perspective. Int. J. Health Plan. Manag. 2023, 38, 430–456. [Google Scholar] [CrossRef] [PubMed]
- Savino, M.; Chiloiro, G.; Masciocchi, C.; Capocchiano, N.D.; Lenkowicz, J.; Gottardelli, B.; Gambacorta, M.A.; Valentini, V.; Damiani, A. A Process Mining Approach for Clinical Guidelines Compliance: Real-World Application in Rectal Cancer. Front. Oncol. 2023, 13, 1090076. [Google Scholar] [CrossRef]
- Atighehchian, A.; Alidadi, T.; Mohammadi, R.R.; Lotfi, F.; Ajami, S. Identifying the Application of Process Mining Technique to Visualise and Manage in the Healthcare Systems. In Proceedings of the Lecture Notes on Data Engineering and Communications Technologies; Springer: Cham, Switzerland, 2023; Volume 181, pp. 299–308. [Google Scholar]
- Asare, E.; Wang, L.; Fang, X. Enhancing EHR Implementation with Process Mining. J. Phys. Conf. Ser. 2022, 2356, 012025. [Google Scholar] [CrossRef]
- Heidemeyer, H.; Auhagen, L.; Majeed, R.W.; Pegoraro, M.; Bienzeisler, J.; Peeva, V.; Beyel, H.; Röhrig, R.; van der Aalst, W.M.P.; Puladi, B. A Pipeline for the Usage of the Core Data Set of the Medical Informatics Initiative for Process Mining—A Technical Case Report. Stud. Health Technol. Inf. 2024, 317, 30–39. [Google Scholar] [CrossRef]
- Schuster, D.; Benevento, E.; Aloini, D.; van der Aalst, W.M.P. Analyzing Healthcare Processes with Incremental Process Discovery: Practical Insights from a Real-World Application. J. Healthc. Inf. Res. 2024, 8, 523–554. [Google Scholar] [CrossRef] [PubMed]
- Kusuma, G.P.; Kurniati, A.P.; Hafidz, F.; Johnson, O.A. Implementing Process Mining in Indonesia Health Care: Challenges and Potentials. Int. J. Appl. Inf. Technol. 2023, 07, 62–78. [Google Scholar] [CrossRef]
- Essefi, I.; Boussi Rahmouni, H.; Solomonides, T.; Fethi Ladeb, M. HIPAA Controlled Patient Information Exchange and Traceability in Clinical Processes. In Proceedings of the 2022 IEEE 9th International Conference on Sciences of Electronics, Technologies of Information and Telecommunications, SETIT 2022; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2022; pp. 452–460. [Google Scholar]
- Zaman, R.; Cuzzocrea, A.; Hassani, M. An Innovative Online Process Mining Framework for Supporting Incremental GDPR Compliance of Business Processes. In Proceedings of the 2019 IEEE International Conference on Big Data, Big Data 2019; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2019; pp. 2982–2991. [Google Scholar]
- Ferretti, A.; Ienca, M.; Hurst, S.; Vayena, E. Big Data, Biomedical Research, and Ethics Review: New Challenges for IRBs. Ethics Hum. Res. 2020, 42, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Manias, G.; Kouremenou, E.; Alzuaz, A.A.; Kranas, P.; Melillo, F.; Kyriazis, D. An Optimized Pipeline for the Processing of Healthcare Data towards the Creation of Holistic Health Records. In Proceedings of the 2023 International Conference on Applied Mathematics and Computer Science, ICAMCS 2023; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023; pp. 50–56. [Google Scholar]
- Mavrogiorgos, K.; Kiourtis, A.; Mavrogiorgou, A.; Kleftakis, S.; Kyriazis, D. A Multi-Layer Approach for Data Cleaning in the Healthcare Domain. In Proceedings of the ACM International Conference Proceeding Series; Association for Computing Machinery: New York, NY, USA, 2022; pp. 22–28. [Google Scholar]
- Flug, J.A.; Stellmaker, J.A.; Sharpe, R.E.; Jokerst, C.E.; Tollefson, C.D.; Bowman, A.W.; Nordland, M.; Hannafin, C.L.; Froemming, A.T. Kaizen Process Improvement in Radiology: Primer for Creating a Culture of Continuous Quality Improvement. Radiographics 2022, 42, 919–928. [Google Scholar] [CrossRef]
- Gültaş, P. Improving Lean Clinics (Lean Healthcare): A Voice of Employee Approach to Reduce Waiting Times. Duzce Univ. J. Soc. Sci. 2023, 13, 198–213. [Google Scholar] [CrossRef]
- Nensi, A.; Simpson, A.; Kives, S.; Lei, R.; D’Souza, J.; Robertson, D. Utilizing Lean Methodology to Optimize Operating Room Efficiency: A Multidisciplinary Process Mapping Exercise. Am. J. Med. Qual. 2020, 35, 91. [Google Scholar] [CrossRef]
- Manandi, D.; Tu, Q.; Hafiz, N.; Raeside, R.; Redfern, J.; Hyun, K. The Evaluation of the Plan-Do-Study-Act Cycles for a Healthcare Quality Improvement Intervention in Primary Care. Aust. J. Prim. Health 2024, 30, PY23123. [Google Scholar] [CrossRef]
- van der Scheer, J.W.; Woodward, M.; Ansari, A.; Draycott, T.; Winter, C.; Martin, G.; Kuberska, K.; Richards, N.; Kern, R.; Dixon-Woods, M.; et al. How to Specify Healthcare Process Improvements Collaboratively Using Rapid, Remote Consensus-Building: A Framework and a Case Study of Its Application. BMC Med. Res. Methodol. 2021, 21, 103. [Google Scholar] [CrossRef]
- Dittmer, K.; Beckmann, M.; Pfaff, H.; Karbach, U. Contextual Factors and Mechanisms in the Implementation of Value Stream Mapping in Breast Cancer Centres—A Multiple Case Study. Z. Evid. Fortbild. Qual. Gesundhwes. 2024, 186, 52–61. [Google Scholar] [CrossRef]
- Graber, M.L.; Castro, G.M.; Danforth, M.; Tilly, J.L.; Croskerry, P.; El-Kareh, R.; Hemmalgarn, C.; Ryan, R.; Tozier, M.P.; Trowbridge, B.; et al. Root Cause Analysis of Cases Involving Diagnosis. Diagnosis 2024, 11, 353–368. [Google Scholar] [CrossRef] [PubMed]
- Burden, M.; Keniston, A.; Pell, J.; Yu, A.; Dyrbye, L.; Kannampallil, T. Unlocking Inpatient Workload Insights with Electronic Health Record Event Logs. J. Hosp. Med. 2024, 20, 79–84. [Google Scholar] [CrossRef]
- Rashed, A.H.M.; El-Attar, N.E.; Abdelminaam, D.S.; Abdelfatah, M. Analysis the Patients’ Careflows Using Process Mining. PLoS ONE 2023, 18, e0281836. [Google Scholar] [CrossRef] [PubMed]
- Shafei, I.; Karnon, J.; Crotty, M. Process Mining and Customer Journey Mapping in Healthcare: Enhancing Patient-Centred Care in Stroke Rehabilitation. Digit. Health 2024, 10, 20552076241249264. [Google Scholar] [CrossRef] [PubMed]
- Utama, N.I.; Sutrisnowati, R.A.; Kamal, I.M.; Bae, H.; Park, Y.J. Mining Shift Work Operation from Event Logs. Appl. Sci. 2020, 10, 7202. [Google Scholar] [CrossRef]
- Chittipaka, V.; Sagi, D.S. Relationship between Kaizen Events and Perceived Quality Performance in Indian Automobile Industry. SSRN Electron. J. 2012, 2. [Google Scholar] [CrossRef]
- Van Der Walt, J.J.N.; Scholl, A.T.; Joubert, I.A.; Petrovic, M.A. Implementation of a Postoperative Handoff Protocol. S. Afr. J. Anaesth. Analg. 2016, 22, 33–37. [Google Scholar] [CrossRef]
- Sharma, P.; Kumar, S.; Falor, T.; Dabral, O.; Upadhyay, A.; Gupta, R.; Andotra, V.S. Leveraging Process Mining for Enhanced Efficiency and Precision in Healthcare. In Generative Artificial Intelligence for Biomedical and Smart Health Informatics; Khamparia, A., Gupta, D., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2025; pp. 471–488. [Google Scholar] [CrossRef]
- Braithwaite, J. Formative Evaluation Feedback Loops. In Implementation Science: The Key Concepts; Taylor and Francis: Oxford, UK, 2022; pp. 85–88. ISBN 9781000583410. [Google Scholar]
- Mans, R.S.; Schonenberg, M.H.; Song, M.; Van Der Aalst, W.M.P.; Bakker, P.J.M. Application of Process Mining in Healthcare—A Case Study in a Dutch Hospital. In Proceedings of the Communications in Computer and Information Science; Springer: Berlin/Heidelberg, Germany, 2008; Volume 25, pp. 425–438. [Google Scholar]
- Cheng, K.Y.; Pazmino, S.; Schreiweis, B. ETL Processes for Integrating Healthcare Data—Tools and Architecture Patterns. Stud. Health Technol. Inf. 2022, 299, 151–156. [Google Scholar] [CrossRef]
- Khemthong, K.; Turnbull, N.; Suwanlee, S.R.; Peltzer, K. The Prevalence of Alcohol and Tobacco Use Associated Risk Factor of Noncommunicable Diseases in Si Sa Ket Province, Thailand. Stud. Health Technol. Inf. 2020, 270, 1407–1408. [Google Scholar] [CrossRef]
- Shanmuga Sundari, M.; Nayak, R.K. Deviation and Cluster Analysis Using Inductive Alpha Miner in Process Mining. In Proceedings of the Lecture Notes in Networks and Systems; Springer: Singapore, 2023; Volume 493, pp. 451–458. [Google Scholar]
- Neamsirorat, W.; Premchaiswadi, W. Analysis of Surgical Event Logs in a Hospital by Using Heuristics Miner Technique. In Proceedings of the International Conference on ICT and Knowledge Engineering; IEEE Computer Society: Washington, DC, USA, 2015; Volume 2015-December, pp. 105–109. [Google Scholar]
- I Gusti Ngurah Agung Agni Prema, N.; Naufal Avilandi, P.; Fathan; Andreswari, R.; Machado, J.M.F. Discovery of Hospital Billing Process in a Regional Hospital Using Process Mining. In Proceedings of the ICADEIS 2023—International Conference on Advancement in Data Science, E-Learning and Information Systems: Data, Intelligent Systems, and the Applications for Human Life, Proceeding; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2023. [Google Scholar]
- Kurniati, A.P.; Rojas, E.; Zucker, K.; Hall, G.; Hogg, D.; Johnson, O. Process Mining to Explore Variations in Endometrial Cancer Pathways from GP Referral to First Treatment. In Public Health and Informatics: Proceedings of MIE 2021; IOS Press: Amsterdam, The Netherlands, 2021; pp. 769–773. ISBN 9781643681856. [Google Scholar]
- Sergio Da Silva, A.; Bento, A.; Avelar, A.; Farina, M.C. The Nurse as an Integration Agent in Handoff: A Social Networks Analysis Perspective. Afr. J. Bus. Manag. 2014, 8, 922–936. [Google Scholar] [CrossRef]
- Benevento, E.; Pegoraro, M.; Antoniazzi, M.; Beyel, H.H.; Peeva, V.; Balfanz, P.; van der Aalst, W.M.P.; Martin, L.; Marx, G. Process Modeling and Conformance Checking in Healthcare: A COVID-19 Case Study: Case Study. In Proceedings of the Lecture Notes in Business Information Processing; Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2023; Volume 468 LNBIP, pp. 315–327. [Google Scholar]
- Sato, D.M.V.; De Freitas, S.C.; Dallagassa, M.R.; Scalabrin, E.E.; Portela, E.A.P.; Carvalho, D.R. Conformance Checking with Different Levels of Granularity: A Case Study on Bariatric Surgery. In Proceedings of the Proceedings—2020 13th International Congress on Image and Signal Processing, BioMedical Engineering and Informatics, CISP-BMEI 2020; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2020; pp. 820–826. [Google Scholar]
- van Kleeff, R.; van Harten, J.; Knies, E.; Boselie, P. ‘Lean Dancing’: How Involvement in Continuous Improvement and Lean Techniques Relate to Hospital Performance and Workers’ Wellbeing through Autonomy. Sustainability 2023, 15, 5546. [Google Scholar] [CrossRef]
- Cooleaf. 15 Ways to Improve Employee Engagement in Healthcare. Available online: https://www.cooleaf.com/blog/5-ways-to-improve-employee-engagement-in-healthcare?utm_source=chatgpt.com (accessed on 31 January 2025).
- Mazzocato, P.; Stenfors-Hayes, T.; Schwarz, U.V.T.; Hasson, H.; Nyström, M.E. Kaizen Practice in Healthcare: A Qualitative Analysis of Hospital Employees’ Suggestions for Improvement. BMJ Open 2016, 6, e012256. [Google Scholar] [CrossRef]
- Drejeris, R.; Drejeriene, E. Novel Approach to the Actions for Causes Elimination of Staff Resistance to Innovative Change. J. Multidiscip. Healthc. 2022, 15, 1011–1022. [Google Scholar] [CrossRef]
- Talero-Sarmiento, L.H.; Escobar-Rodríguez, L.Y.; Gomez-Avila, F.L.; Parra-Sanchez, D.T. A Literature Review on Lean Healthcare: Implementation Strategies, Challenges, and Future Research Directions. Cogent Eng. 2024, 11, 2411857. [Google Scholar] [CrossRef]
- Agarwal, S.; Tweheyo, R.; Pandya, S.; Obuya, E.; Kiyomoto, A.; Mitra, P.; Schleiff, M.; Nagpal, T.; Macis, M.; Rutebemberwa, E. Impact of a Recognition Package as an Incentive to Strengthen the Motivation, Performance, and Retention of Village Health Teams in Uganda: A Study Protocol for a Cluster Randomized Controlled Trial. Trials 2023, 24, 428. [Google Scholar] [CrossRef]
- da Silva, E.P.; Saturno-Hernández, P.J.; de Freitas, M.R.; da Silva Gama, Z.A. Motivational Drivers for Health Professionals in a Large Quality Improvement Collaborative Project in Brazil: A Qualitative Study. BMC Health Serv. Res. 2024, 24, 183. [Google Scholar] [CrossRef]
- Elkefi, S.; Asan, O.; Mnasouri, M. Change Management and Continuous Improvement for Smarter Care: A Systems Viewpoint. In Proceedings of the ISSE 2021—7th IEEE International Symposium on Systems Engineering, Proceedings; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2021. [Google Scholar]
- Murray, J.S.; Kelly, S.; Hanover, C. Promoting Psychological Safety in Healthcare Organizations. Mil. Med. 2022, 187, 808–810. [Google Scholar] [CrossRef] [PubMed]
- Dieckmann, P.; Tulloch, S.; Dalgaard, A.E.; Varming, K. Psychological Safety during the Test of New Work Processes in an Emergency Department. BMC Health Serv. Res. 2022, 22, 307. [Google Scholar] [CrossRef]
- Shah, A.; Akhtar, S.; Ayers, T.; Bevan, R.; Cannon, E.; Milarski, M.; Souza, R.; Warby, R. Increasing Joy in Work in UK Healthcare Teams: A National Quality Improvement Collaborative. Br. J. Health Care Manag. 2023, 29, 1–16. [Google Scholar] [CrossRef]
- Sheen Sheen, J.J.; Lee, B.; Clancy, E.; Considine, J.; Dwyer, A.; Tchernegovski, P.; Reupert, A.; Taylor, N.; Herrick, C.; Boyd, L. Regional Public Health Staff Workplace Psychosocial Risk Assessment and Health Promotion Initiative. Eur. J. Public Health 2023, 33, ckad160.131. [Google Scholar] [CrossRef]
- Ryan Ryan, L.L.; Cooney, F. Evaluation of a Public Health Workplace Staff Psychosocial Risk Assessment and Wellbeing Initiative. Eur. J. Public Health 2024, 34, ckae144.599. [Google Scholar] [CrossRef]
- Marin-Garcia, J.A.; Vidal-Carreras, P.I.; Garcia-Sabater, J.J. The Role of Value Stream Mapping in Healthcare Services: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 951. [Google Scholar] [CrossRef]
- Nino, V.; Claudio, D.; Valladares, L.; Harris, S. An Enhanced Kaizen Event in a Sterile Processing Department of a Rural Hospital: A Case Study. Int. J. Environ. Res. Public Health 2020, 17, 8748. [Google Scholar] [CrossRef]
- Sumer, A.M.; Ceylan, C. A Process Mining Model to Detect Adverse Patient Safety Events: Blood Products Watch. J. Patient Saf. Risk Manag. 2024, 29, 248–256. [Google Scholar] [CrossRef]
- Kawamura, H.; Arimura, S.; Murata, N.; Shigemi, A.; Niiyama, S.; Nishi, J.; Kakihana, Y. 1450. Managing a Multidrug-Resistant Acinetobacter Baumannii Outbreak in the ICU: A Successful KAIZEN Program Using Process Indicators for Antimicrobial Stewardship, Hand Hygiene, and Standardization. Open Forum Infect. Dis. 2023, 10, ofad500.1287. [Google Scholar] [CrossRef]
- Erdogan, T.G.; Tarhan, A. A Goal-Driven Evaluation Method Based On Process Mining for Healthcare Processes. Appl. Sci. 2018, 8, 894. [Google Scholar] [CrossRef]
- Silver, S.A.; McQuillan, R.; Harel, Z.; Weizman, A.V.; Thomas, A.; Nesrallah, G.; Bell, C.M.; Chan, C.T.; Chertow, G.M. How to Sustain Change and Support Continuous Quality Improvement. Clin. J. Am. Soc. Nephrol. 2016, 11, 916. [Google Scholar] [CrossRef] [PubMed]
- Clancy, G.; Graban, M. Engaging Staff as Problem Solvers Leads to Continuous Improvement at Allina Health. Glob. Bus. Organ. Excell. 2014, 33, 35–42. [Google Scholar] [CrossRef]
- Callaghan, N.I.; Quinn, J.; Liwski, R.; Chisholm, N.; Cheng, C. Process Mining Uncovers Actionable Patterns of Red Blood Cell Unit Wastage in a Health Care Network. Transfus. Med. Rev. 2024, 38, 150827. [Google Scholar] [CrossRef]
- Ker, J.-I.; Wang, Y. Kaizen Policies in Healthcare Governance: Reducing Patient-Flow Delays in Outpatient Surgery Setting through Healthcare Information Technology. SSRN Electron. J. 2015. [Google Scholar] [CrossRef]
- Mahbubani, K.; Georgiades, F.; Goh, E.L.; Chidambaram, S.; Sivakumaran, P.; Rawson, T.; Ray, S.; Hudovsky, A.; Gill, D. Clinician-Directed Improvement in the Accuracy of Hospital Clinical Coding. Future Healthc. J. 2018, 5, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Navarro, C.; Jones, B.; Pugh, G.; Moneypenny, M.; Lazarovici, M.; Grant, D.J. Improving Quality through Simulation; Developing Guidance to Design Simulation Interventions Following Key Events in Healthcare. Adv. Simul. 2024, 9, 30. [Google Scholar] [CrossRef]
- Tsebrovskaya, E.A.; Teplov, V.M.; Klyukovkin, K.S.; Prasol, D.M.; Bagnenko, S.F. Possibilities of Simulation Modeling in the Practice of the Healthcare System. Sci. Notes Pavlov. Univ. 2022, 29, 17–23. [Google Scholar] [CrossRef]
- Epistola, R.; Ho, B.; Leong, S.; Ali, S.; Germono, R.; Kummerfeldt, C.; Gutierrez, G.; Shim, J.; Lee, J.M.; Yeh, J.J. Applying Lean Kaizen to Improve Timely Computed Tomography Scan Appointments for Oncology Patients in a Safety Net Hospital. JCO Oncol. Pract. 2023, 19, e465–e469. [Google Scholar] [CrossRef] [PubMed]
- Igoe, A.; Teeling, S.P.; McFeely, O.; McGuirk, M.; Manning, S.; Kelly, V.; Coetzee, H.; Cunningham, Ú.; Connolly, K.; Lenane, P. Implementing Person-Centred Lean Six Sigma to Transform Dermatology Waiting Lists: A Case Study from a Major Teaching Hospital in Dublin, Ireland. Sci 2024, 6, 72. [Google Scholar] [CrossRef]
- Souza, D.L.; Korzenowski, A.L.; Alvarado, M.M.; Sperafico, J.H.; Ackermann, A.E.F.; Mareth, T.; Scavarda, A.J. A Systematic Review on Lean Applications’ in Emergency Departments. Healthcare 2021, 9, 763. [Google Scholar] [CrossRef]
- Khalil Alobaid, S.; Mohsen, A.; Alzahrani, M.; Alsharif, F.S.; Essa, A.; Alomar, H.; Masoud, H.; Almustanyir, S.; Sagr, A.A.; Ali, S.; et al. Enhancing Patient-Centered Care Through Process Improvement: A Systematic Review of Patient Satisfaction Outcomes. J. Ecohumanism. 2024, 3, 975–982. [Google Scholar] [CrossRef]
- Oueida, S.; Kotb, Y. Healthcare Emergency Room Optimization Using a Process Learning Algorithm. In Proceedings of the Advances in Intelligent Systems and Computing; Springer: Cham, Switzerland, 2021; Volume 1290, pp. 46–63. [Google Scholar]
- Manzanedo-Basilio, L.; Arias-Rivera, S. Streamlining of Patient Discharge and Intra-Hospital Transfer Processes Using Lean Methodology. J. Healthc. Qual. Res. 2024, 39, 23–31. [Google Scholar] [CrossRef]
- Lin, C.C.; Shen, J.H.; Chen, S.F.; Chen, H.M.; Huang, H.M. Developing a Cost-Effective Surgical Scheduling System Applying Lean Thinking and Toyota’s Methods for Surgery-Related Big Data for Improved Data Use in Hospitals: User-Centered Design Approach. JMIR Form. Res. 2024, 8, e52185. [Google Scholar] [CrossRef]
- Santos, B.; Blondon, K.S.; Van Gessel, E.; Cerutti, B.; Backes, C.; Locher, S.; Guignard, B.; Bonnabry, P.; Carpenter, D.; Schneider, M.P. Patients’ Perceptions of Conflicting Information on Chronic Medications: A Prospective Survey in Switzerland. BMJ Open 2022, 12, e060083. [Google Scholar] [CrossRef]
- Ren, W.; Liu, Z.; Wu, Y.; Zhang, Z.; Hong, S.; Liu, H.; Missing Data in Electronic health Records (MINDER) Group. Moving Beyond Medical Statistics: A Systematic Review on Missing Data Handling in Electronic Health Records. Health Data Sci. 2024, 4, 0176. [Google Scholar] [CrossRef]
- Manias, G.; Azqueta-Alzúaz, A.; Damiani, A.; Dhar, E.; Kouremenou, E.; Patino-Martínez, M.; Savino, M.; Shabbir, S.A.; Kyriazis, D. An Enhanced Standardization and Qualification Mechanism for Heterogeneous Healthcare Data. In Proceedings of the Studies in Health Technology and Informatics; IOS Press: Amsterdam, The Netherlands, 2023; Volume 302, pp. 153–154. [Google Scholar]
- Liu, J.; Xu, J.; Zhang, R.; Reiff-Marganiec, S. A Repairing Missing Activities Approach with Succession Relation for Event Logs. Knowl. Inf. Syst. 2021, 63, 477–495. [Google Scholar] [CrossRef]
- Perimal-Lewis, L.; Teubner, D.; Hakendorf, P.; Horwood, C. Application of Process Mining to Assess the Data Quality of Routinely Collected Time-Based Performance Data Sourced from Electronic Health Records by Validating Process Conformance. Health Inform. J. 2016, 22, 1017–1029. [Google Scholar] [CrossRef] [PubMed]
- Fischer, D.A.; Goel, K.; Andrews, R.; van Dun, C.G.J.; Wynn, M.T.; Röglinger, M. Enhancing Event Log Quality: Detecting and Quantifying Timestamp Imperfections. In Proceedings of the Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2020; Volume 12168 LNCS, pp. 309–326. [Google Scholar]
- Shaheen, N.A.; Manezhi, B.; Thomas, A.; Alkelya, M. Reducing Defects in the Datasets of Clinical Research Studies: Conformance with Data Quality Metrics. BMC Med. Res. Methodol. 2019, 19, 98. [Google Scholar] [CrossRef]
- Makeham, M.A.B.; Stromer, S.; Bridges-Webb, C.; Mira, M.; Saltman, D.C.; Cooper, C.; Kidd, M.R. Patient Safety Events Reported in General Practice: A Taxonomy. BMJ Qual. Saf. 2008, 17, 53–57. [Google Scholar] [CrossRef]
- Akmal, A.; Foote, J.; Podgorodnichenko, N.; Greatbanks, R.; Gauld, R. Understanding Resistance in Lean Implementation in Healthcare Environments: An Institutional Logics Perspective. Prod. Plan. Control. 2022, 33, 356–370. [Google Scholar] [CrossRef]
- Ackerhans, S.; Huynh, T.; Kaiser, C.; Schultz, C. Exploring the Role of Professional Identity in the Implementation of Clinical Decision Support Systems—A Narrative Review. Implement. Sci. 2024, 19, 11. [Google Scholar] [CrossRef]
- Heath, M.; Appan, R.; Henry, R. Value Alignment’s Role in Mitigating Resistance to IT Use: The Case of Physicians’resistance to Electronic Health Record Systems. Inf. Manag. 2022, 59, 103702. [Google Scholar] [CrossRef]
- Al-rawashdeh, M.; Keikhosrokiani, P.; Belaton, B.; Alawida, M.; Zwiri, A. IoT Adoption and Application for Smart Healthcare: A Systematic Review. Sensors 2022, 22, 5377. [Google Scholar] [CrossRef]
- Bernardi, F.A.; Alves, D.; Crepaldi, N.; Yamada, D.B.; Lima, V.C.; Rijo, R. Data Quality in Health Research: Integrative Literature Review. J. Med. Internet Res. 2023, 25, e41446. [Google Scholar] [CrossRef]
- Hohl, S.D.; Bird, J.E.; Nguyen, C.V.T.; D’angelo, H.; Minion, M.; Pauk, D.; Adsit, R.T.; Fiore, M.; Nolan, M.B.; Rolland, B. Operationalizing Leadership and Clinician Buy-In to Implement Evidence-Based Tobacco Treatment Programs in Routine Oncology Care: A Mixed-Method Study of the U.S. Cancer Center Cessation Initiative. Curr. Oncol. 2022, 29, 2406–2421. [Google Scholar] [CrossRef] [PubMed]
- Sansbury, G.M.; Pence, B.W.; Zimba, C.; Yanguela, J.; Landrum, K.; Matewere, M.; Mbota, M.D.; Malava, J.K.; Tikhiwa, H.; Morrison, A.M.; et al. Improving Integrated Depression and Non-Communicable Disease Care in Malawi through Engaged Leadership and Supportive Implementation Climate. BMC Health Serv. Res. 2023, 23, 1413. [Google Scholar] [CrossRef] [PubMed]
- Russek, M.; Quinten, C.; de Jong, V.M.T.; Cohet, C.; Kurz, X. Assessing Heterogeneity of Electronic Health-Care Databases: A Case Study of Background Incidence Rates of Venous Thromboembolism. Pharmacoepidemiol. Drug Saf. 2023, 32, 1032–1048. [Google Scholar] [CrossRef] [PubMed]
- Madigan, D.; Ryan, P.B.; Schuemie, M.; Stang, P.E.; Overhage, J.M.; Hartzema, A.G.; Suchard, M.A.; Dumouchel, W.; Berlin, J.A. Evaluating the Impact of Database Heterogeneity on Observational Study Results. Am. J. Epidemiol. 2013, 178, 645–651. [Google Scholar] [CrossRef]
- Büttner, F.; Winters, M.; Delahunt, E.; Elbers, R.; Lura, C.B.; Khan, K.M.; Weir, A.; Ardern, C.L. Identifying the ‘Incredible’! Part 1: Assessing the Risk of Bias in Outcomes Included in Systematic Reviews. Br. J. Sports Med. 2020, 54, 798–800. [Google Scholar] [CrossRef]
- McKeown, S.; Mir, Z.M. Considerations for Conducting Systematic Reviews: Evaluating the Performance of Different Methods for de-Duplicating References. Syst. Rev. 2021, 10, 38. [Google Scholar] [CrossRef]
- Rathbone, J.; Carter, M.; Hoffmann, T.; Glasziou, P. Better Duplicate Detection for Systematic Reviewers: Evaluation of Systematic Review Assistant-Deduplication Module. Syst. Rev. 2015, 4, 6. [Google Scholar] [CrossRef]
- Brunström, M. Tower of Babel Bias or Efficient Exclusion of Low-Quality Studies: How to Handle Non-English Literature in Systematic Reviews and Meta-Analyses. J. Hypertens. 2024, 42, 1681–1683. [Google Scholar] [CrossRef]
- Mao, C.; Li, M. Language Bias Among Chinese-Sponsored Randomized Clinical Trials in Systematic Reviews and Meta-Analyses—Can Anything Be Done? JAMA Netw. Open 2020, 3, e206370. [Google Scholar] [CrossRef]
- Endalamaw, A.; Khatri, R.B.; Mengistu, T.S.; Erku, D.; Wolka, E.; Zewdie, A.; Assefa, Y. A Scoping Review of Continuous Quality Improvement in Healthcare System: Conceptualization, Models and Tools, Barriers and Facilitators, and Impact. BMC Health Serv. Res. 2024, 24, 487. [Google Scholar] [CrossRef]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing Healthcare: The Role of Artificial Intelligence in Clinical Practice. BMC Med. Educ. 2023, 23, 689. [Google Scholar] [CrossRef] [PubMed]
- dos Santos Garcia, C.; Meincheim, A.; Faria Junior, E.R.; Dallagassa, M.R.; Sato, D.M.V.; Carvalho, D.R.; Santos, E.A.P.; Scalabrin, E.E. Process Mining Techniques and Applications—A Systematic Mapping Study. Expert. Syst. Appl. 2019, 133, 260–295. [Google Scholar] [CrossRef]
- Tekin, M.; Arslandere, M.; Etlioğlu, M.; Tekin, E. An Application of Kaizen in a Large-Scale Business. In Proceedings of the International Symposium for Production Research 2018; Springer: Cham, Switzerland, 2019; pp. 515–529. [Google Scholar]
- Winter, M.; Langguth, B.; Schlee, W.; Pryss, R. Process Mining in MHealth Data Analysis. NPJ Digit. Med. 2024, 7, 299. [Google Scholar] [CrossRef] [PubMed]
| Tool/Method | Description |
|---|---|
| Iterative Improvement Cycles | |
| Plan-Do-Study-Act (PDSA) Cycle Plan-Do-Check-Act (PDCA) Cycle | A structured, iterative approach to testing and implementing changes [73]. |
| Collaborative Problem-Solving Tools | |
| Brainstorming Sessions | Collaborative problem-solving methods to generate creative and actionable solutions [74]. |
| Process Visualization Tools | |
| Value Stream Mapping (VSM) | A technique for visualizing workflows to identify inefficiencies and areas for improvement [75]. |
| Root Cause Analysis (RCA) | A systematic approach to identifying and addressing the underlying causes of issues [76]. |
| Phase | Example Activities | Expected Outputs |
|---|---|---|
| Data Collection |
|
|
| Process Analysis |
|
|
| Kaizen Events |
|
|
| Continuous Monitoring |
|
|
| Outcome Category | Process Mining Contribution | Kaizen Contribution |
|---|---|---|
| Operational/Process Outcomes | ||
| Streamlined Workflows | Provides real-time visibility of operational inefficiencies and deviations from expected workflows [63]. | Uses tools like value stream mapping (VSM) and PDCA cycles to systematically remove inefficiencies and standardize best practices [108]. |
| Reduced Wait Times | Identifies bottlenecks by analyzing event logs in emergency departments, outpatient services, and surgical scheduling [14]. | Implements staff reallocation, process streamlining, and workflow redesign to optimize patient flow [109]. |
| Improved Decision-Making | Analyzes historical and real-time event logs to provide actionable insights for clinical adjustments [55]. | Engages clinicians in continuous improvement discussions, ensuring that data-driven changes are clinically relevant [110]. |
| Clinical Outcomes | ||
| Enhanced Compliance | Uses conformance checking to compare actual workflows with predefined clinical protocols, identifying deviations [46]. | Encourages staff accountability and proactive process refinement to align with evidence-based practices [32]. |
| Better Safety and Quality | Identifies patterns and risks in care processes before they affect patients [110]. | Establishes standardized protocols that reduce variation and enhance care reliability [111]. |
| Employee Outcomes | ||
| Cultivating Improvement Culture | Supplies objective, data-backed evidence to guide iterative improvements [112]. | Actively involves frontline staff in problem-solving and process optimization, fostering ownership [113]. |
| Enhanced Skills Development | Provides learning opportunities through data visualization and analysis [60]. | Builds problem-solving capabilities through structured improvement approaches [114]. |
| Patient Outcomes | ||
| Improved Experience | Ensures smoother workflows and timely interventions through automated process monitoring [14]. | Enhances service quality and patient-centered care by reducing inefficiencies [113]. |
| Financial Outcomes | ||
| Cost Reduction | Identifies resource waste and unnecessary process steps through detailed activity analysis [115]. | Implements targeted efficiency improvements that reduce operational costs while maintaining quality [116]. |
| Revenue Enhancement | Uncovers opportunities for optimizing reimbursement through analysis of billing processes and claim patterns [90]. | Develops standardized approaches to documentation and coding that maximize appropriate revenue capture [117]. |
| Validation Method | Description | Expected Benefits |
|---|---|---|
| Simulation-Based Validation | Computational simulations replicate hospital workflows to evaluate the integration of PM and Kaizen improvements [118]. | Predict potential efficiency gains before real-world implementation [119]. |
| Pilot Studies | Small-scale implementations in specific departments to test the framework in a controlled setting [35]. | Identify challenges, refine the integration, and assess feasibility [120]. |
| Case Studies | Reviewing past applications of Kaizen and PM in healthcare settings to conceptualize their combined impact [121]. | Provide empirical insights into real-world effectiveness [23,89]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samara, M.N.; Harry, K.D. Leveraging Kaizen with Process Mining in Healthcare Settings: A Conceptual Framework for Data-Driven Continuous Improvement. Healthcare 2025, 13, 941. https://doi.org/10.3390/healthcare13080941
Samara MN, Harry KD. Leveraging Kaizen with Process Mining in Healthcare Settings: A Conceptual Framework for Data-Driven Continuous Improvement. Healthcare. 2025; 13(8):941. https://doi.org/10.3390/healthcare13080941
Chicago/Turabian StyleSamara, Mohammad Najeh, and Kimberly D. Harry. 2025. "Leveraging Kaizen with Process Mining in Healthcare Settings: A Conceptual Framework for Data-Driven Continuous Improvement" Healthcare 13, no. 8: 941. https://doi.org/10.3390/healthcare13080941
APA StyleSamara, M. N., & Harry, K. D. (2025). Leveraging Kaizen with Process Mining in Healthcare Settings: A Conceptual Framework for Data-Driven Continuous Improvement. Healthcare, 13(8), 941. https://doi.org/10.3390/healthcare13080941






