Deploying the Substitutive and Complementary Approaches to Enhance Predictions of Health Behaviour in Health Economics: A Quantitative Study
Abstract
:1. Introduction
2. Methods
2.1. Research Design
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Instrument Characteristics
3.3. Model Characteristics
3.3.1. Standard Approach
3.3.2. Substitutive Approach
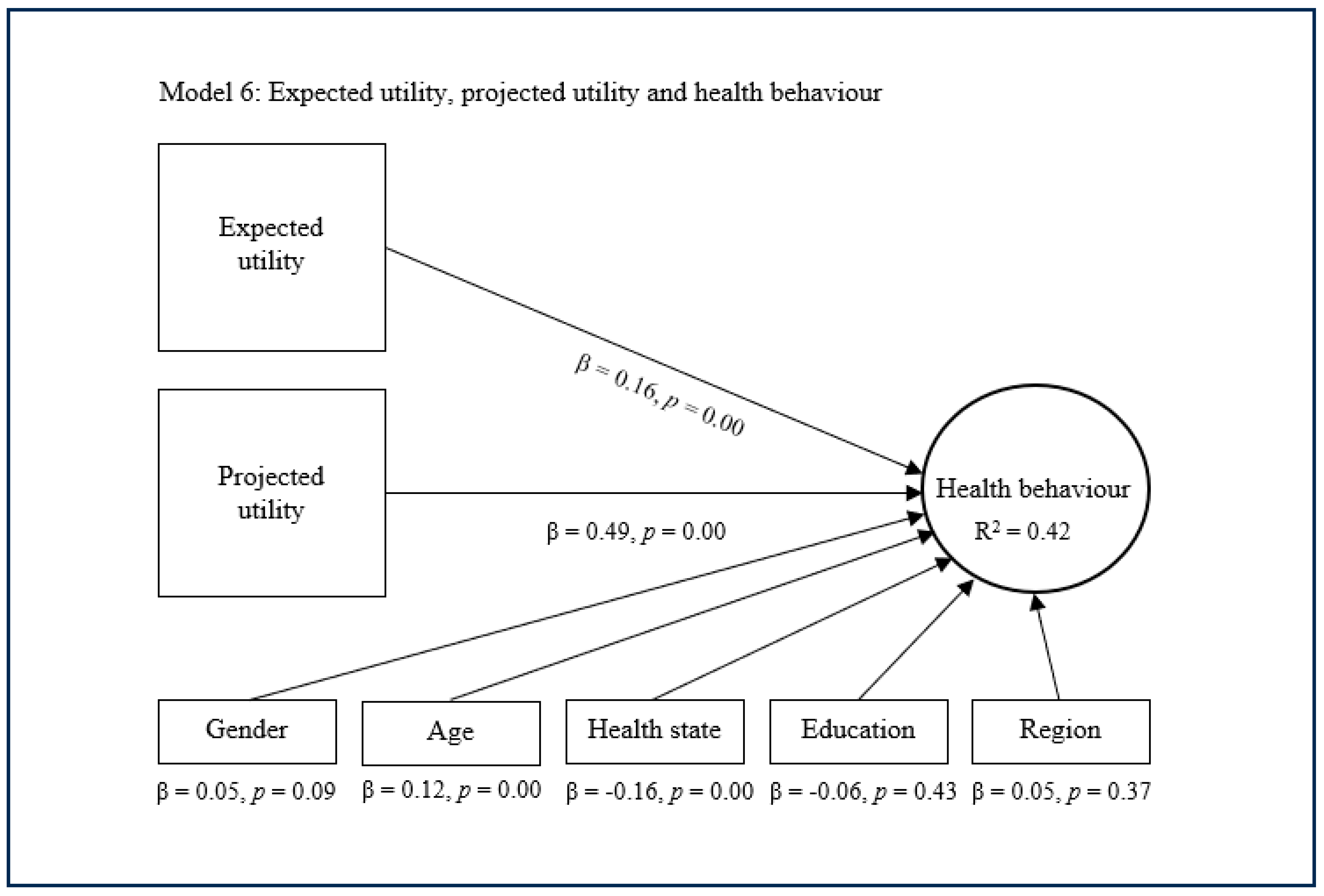
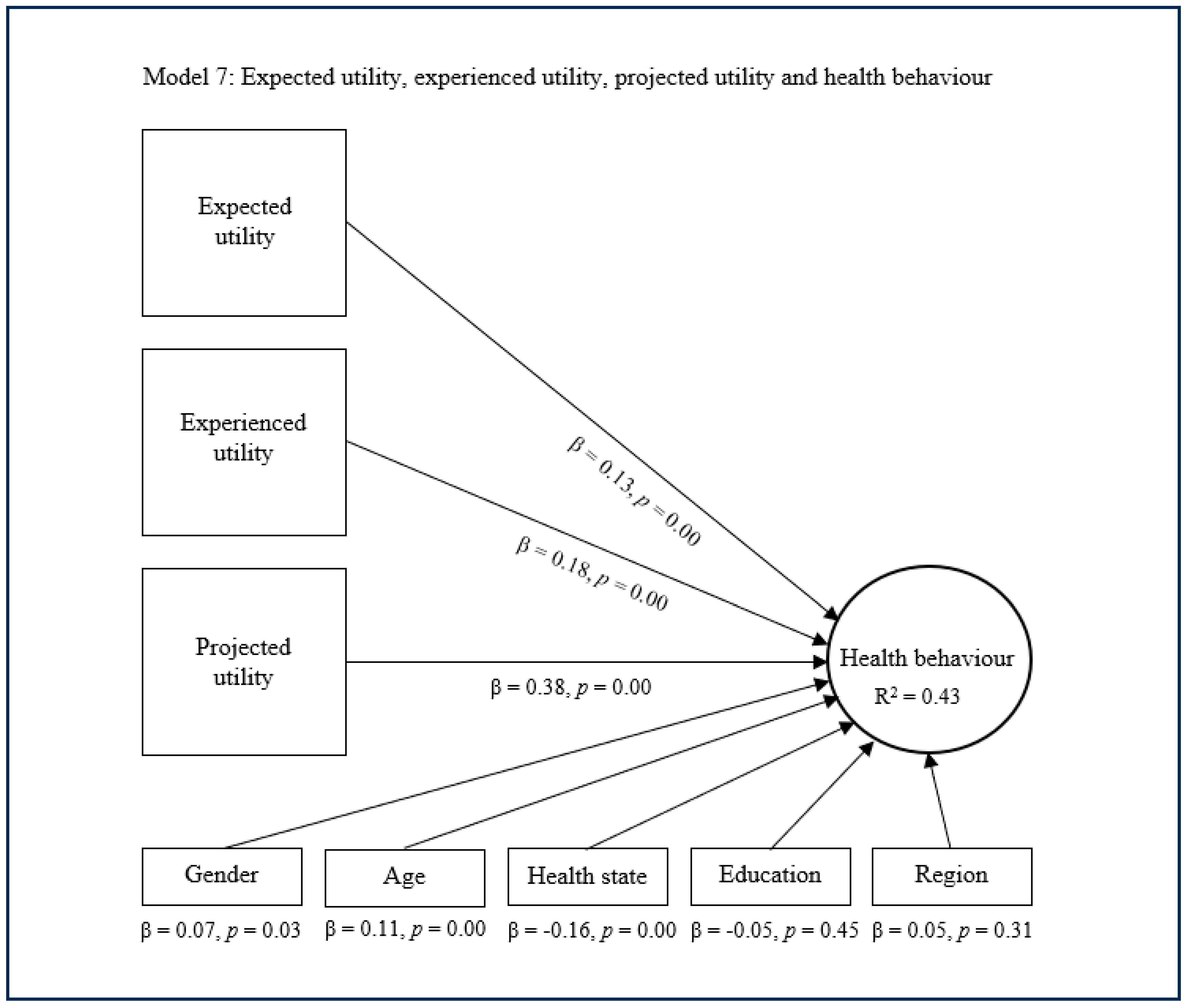
3.3.3. Complementary Approach
4. Discussion
4.1. Strengths and Limitations
4.2. Practical Implications
4.3. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vlaev, I.; King, D.; Darzi, A.; Dolan, P. Changing health behaviors using financial incentives: A Review from Behavioral Economics. BMC Public Health 2019, 19, 1059. [Google Scholar] [CrossRef] [PubMed]
- Jakovljevic, M.M.; Ogura, S. Health Economics at the Crossroads of Centuries—From the Past to the Future. Front. Public Health 2016, 4, 115. [Google Scholar] [CrossRef] [PubMed]
- Wolowacz, E.; Briggs, A.; Belozeroff, V.; Clarke, P.; Doward, L.; Goeree, R.; Lloyd, A.; Norman, R. Estimating Health-State Utility for Economic Models in Clinical Studies: An ISPOR Good Research Practices Task Force Report. Value Health 2016, 19, 704–719. [Google Scholar] [CrossRef] [PubMed]
- Broekharst, D.S.E.; Bloem, S.; Groenland, E.A.G.; van Raaij, W.F.; Jeurissen, P.P.T.; van Agthoven, M. Rethinking the eidos, genos, and diaphora of the health utility concept: A Psychological Perspective. Front. Psychol. 2023, 14, 1139931. [Google Scholar] [CrossRef]
- Conell-Price, L.; Jamison, J. Predicting health behaviors with economic preferences & locus of control. J. Behav. Exp. Econ. 2015, 54, 1–9. [Google Scholar]
- Kahneman, D.; Tversky, A. Prospect Theory: An Analysis of Decision under Risk. Econometrica 1979, 47, 263. [Google Scholar] [CrossRef]
- Berridge, K.; O’Doherty, J.P. From Experienced Utility to Decision Utility. In Neuroeconomics: Decision Making and the Brain; Glimcher, P.W., Fehr, E., Eds.; Academic Press: London, UK, 2013; pp. 325–338. [Google Scholar]
- Kahneman, D.; Thaler, R. Economic Analysis and the Psychology of Utility: Applications to Compensation Policy. Am. Econ. Rev. 1991, 81, 341–346. [Google Scholar]
- Briggs, R.A. Normative Theories of Rational Choice: Expected Utility. Stanford Encyclopedia of Philosophy. 2014. Available online: https://plato.stanford.edu/entries/rationality-normative-utility/ (accessed on 2 February 2025).
- Galaabaatar, T.; Karni, E. Subjective expected utility with incomplete preferences. Econometrica 2013, 81, 255–284. [Google Scholar]
- Fishburn, P.C. Subjective expected utility: A review of normative theories. Theory Decis. 1981, 13, 139–199. [Google Scholar] [CrossRef]
- Schipper, B.C. Awareness-dependent subjective expected utility. Int. J. Game Theory 2013, 42, 725–753. [Google Scholar] [CrossRef]
- Thompson, A.J.; Turner, A.J. A Comparison of the EQ-5D-3L and EQ-5D-5L. Pharmacoeconomics 2020, 38, 575–591. [Google Scholar] [CrossRef] [PubMed]
- Devlin, N.J.; Brooks, R. EQ-5D and the EuroQol Group: Past, Present and Future. Appl. Health Econ. Health Policy 2017, 15, 127–137. [Google Scholar] [CrossRef]
- Brazier, J.E.; Rowen, D.; Lloyd, A.; Karimi, M. Future directions in valuing benefits for estimating QALYs: Is time up for the EQ-5D? Value Health 2019, 22, 62–68. [Google Scholar] [CrossRef]
- Lugnér, A.K.; Krabbe, P.F.M. An overview of the time trade-off method: Concept, foundation, and the evaluation of distorting factors in putting a value on health. Expert Rev. Pharmacoecon. Outcomes Res. 2020, 20, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Attema, A.E.; Edelaar-Peeters, Y.; Versteegh, M.M.; Stolk, E.A. Time trade-off: One Methodology, Different Methods. Eur. J. Health Econ. 2013, 14, 53–64. [Google Scholar] [CrossRef]
- Bloem, J.G.; Stalpers, J. Subjective Experienced Health As a Driver of Health Care Behavior. Nyenrode Res. Pap. Ser. 2012, 12, 1–19. [Google Scholar] [CrossRef]
- Bloem, J.G. ‘Beleving als Medicijn’ (Experience as a Medicine: The Development of a General Subjective Health Instrument—In Dutch with English Summary); Nyenrode Business Universiteit: Breukelen, The Netherlands, 2008. [Google Scholar]
- Stalpers, J. Psychological Determinants of Subjective Health; Nyenrode Business Universiteit: Breukelen, The Netherlands, 2009. [Google Scholar]
- Bloem, S.; Stalpers, J.; Groenland, E.A.G.; van Montfort, K.; van Raaij, W.F.; de Rooij, K. Segmentation of health-care consumers: Psychological Determinants of Subjective Health and Other Person-Related Variables. BMC Health Serv. Res. 2020, 20, 726. [Google Scholar] [CrossRef]
- Peeters, M.C.W.; Ligthart, A.; Schaufeli, W.B.; Taris, A.W. BRAVO op het werk: Een onderzoek naar de relatie tussen leefstijlgedragingen en individuele werkprestatie. J. Hum. Factors 2015, 40, 5–9. [Google Scholar]
- Hair, J.F.; Risher, J.J.; Sarstedt, M.; Ringle, C.M. When to use and how to report the results of PLS-SEM. Eur. Bus. Rev. 2019, 31, 2–24. [Google Scholar] [CrossRef]
- Rönkkö, M.; McIntosh, C.N.; Antonakis, J.; Edwards, J.R. Partial least squares path modeling: Time for some serious second thoughts. J. Oper. Manag. 2016, 47, 9–27. [Google Scholar] [CrossRef]
- Bala, J. Contribution of SPSS in Social Sciences Research. Int. J. Adv. Res. Comput. Sci. Softw. Eng. 2016, 7, 250. [Google Scholar]
- Dudley, W.N.; Benuzillo, J.G.; Carrico, M.S. SPSS and SAS programming for the testing of mediation models. Nurs. Res. 2004, 53, 59–62. [Google Scholar] [CrossRef]
- CBS. Age Distribution. 2024. Available online: https://www.cbs.nl/en-gb/visualisations/dashboard-population/age/age-distribution (accessed on 2 February 2025).
- RIVM. Bevolking|Bevolkingsomvang|Leeftijd en Geslacht. 2024. Available online: https://www.vzinfo.nl/bevolking-bevolkingsomvang-leeftijd-en-geslacht#:~:text=De%20verhouding%20tussen%20mannen%20en,worden%20(51%2C3%25) (accessed on 2 February 2025).
- RIVM. Chronische Aandoeningen en Multimorbiditeit. 2024. Available online: https://www.vzinfo.nl/chronische-aandoeningen-en-multimorbiditeit/leeftijd-en-geslacht#:~:text=5%2C7%20miljoen%20mensen%20met,ten%20minste%20%C3%A9%C3%A9n%20chronische%20ziekte (accessed on 2 February 2025).
- CBS. What Is the Level of Education in the Netherlands? 2024. Available online: https://longreads.cbs.nl/the-netherlands-in-numbers-2024/what-is-the-level-of-education-in-the-netherlands/ (accessed on 2 February 2025).
- PBL. De Stad Verbeeld. 2024. Available online: https://www.pbl.nl/sites/default/files/downloads/PBL_2015_De_stad_verbeeld_1744.pdf (accessed on 2 February 2025).
- CBS. Inwoners Per Gemeente. 2024. Available online: https://www.cbs.nl/nl-nl/visualisaties/dashboard-bevolking/regionaal/inwoners (accessed on 2 February 2025).
- CBS. Income Distribution (Standardised Income). 2024. Available online: https://www.cbs.nl/en-gb/visualisations/income-distribution (accessed on 2 February 2025).
- Shrestha, N. Detecting multicollinearity in regression analysis. Am. J. Appl. Math. Stat. 2020, 8, 39–42. [Google Scholar] [CrossRef]
- Riewpaiboon, A. Measurement of costs for health economic evaluation. J. Med. Assoc. Thail. 2014, 97, 17–26. [Google Scholar]
- Krauth, C.; Hessel, F.; Hansmeier, T.; Wasem, J.; Seitz, R.; Schweikert, B. Empirical standard costs for health economic evaluation in Germany–a proposal by the working group methods in health economic evaluation. Gesundheitswesen 2005, 67, 736–746. [Google Scholar] [CrossRef]
- Rencher, A.C.; Pun, F.C. Inflation of R2 in best subset regression. Technometrics 1980, 22, 49–53. [Google Scholar] [CrossRef]
- Sober, E. The principle of parsimony. Br. J. Philos. Sci. 1981, 32, 145–156. [Google Scholar] [CrossRef]





| Variables | ||||
|---|---|---|---|---|
| Age | 49.3 years (18–89 years) | |||
| Gender | 48.6% male | 51.4% female | ||
| Health status | 37.2% healthy | 27.9% 1 disease | 34.9% comorbidities | |
| Living area | 56.8% city | 34.3% suburb | 8.9% rural | |
| Residential region | 10.1% North Netherlands | 21.1% East Netherlands | 48.1% West Netherlands | 20.7% South Netherlands |
| Education level | 31.5% low | 29.3% average | 38.9% higher | 0.4% unknown |
| Annual income | 35.2% < €36,500 | 35.8% €36,500–€73,000 | 14.6% > €73,000 | 14.4% unknown |
| Theoretical Perspective | Practical Perspective | Methodological Perspective | |
|---|---|---|---|
| Standard approach | |||
| Model 1 | X | ✓ | ✓ |
| Substitutive approach | |||
| Model 2 | ✓ | X | ✓ |
| Model 3 | ✓ | X | ✓ |
| Model 4 | ✓ | X | ✓ |
| Complementary approach | |||
| Model 5 | X | ✓ | ✓ |
| Model 6 | X | ✓ | ✓ |
| Model 7 | X | X | X |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Broekharst, D.S.E.; Bloem, S.; Groenland, E.A.G.; Jeurissen, P.P.T.; van Agthoven, M. Deploying the Substitutive and Complementary Approaches to Enhance Predictions of Health Behaviour in Health Economics: A Quantitative Study. Healthcare 2025, 13, 1007. https://doi.org/10.3390/healthcare13091007
Broekharst DSE, Bloem S, Groenland EAG, Jeurissen PPT, van Agthoven M. Deploying the Substitutive and Complementary Approaches to Enhance Predictions of Health Behaviour in Health Economics: A Quantitative Study. Healthcare. 2025; 13(9):1007. https://doi.org/10.3390/healthcare13091007
Chicago/Turabian StyleBroekharst, Damien S. E., Sjaak Bloem, Edward A. G. Groenland, Patrick P. T. Jeurissen, and Michel van Agthoven. 2025. "Deploying the Substitutive and Complementary Approaches to Enhance Predictions of Health Behaviour in Health Economics: A Quantitative Study" Healthcare 13, no. 9: 1007. https://doi.org/10.3390/healthcare13091007
APA StyleBroekharst, D. S. E., Bloem, S., Groenland, E. A. G., Jeurissen, P. P. T., & van Agthoven, M. (2025). Deploying the Substitutive and Complementary Approaches to Enhance Predictions of Health Behaviour in Health Economics: A Quantitative Study. Healthcare, 13(9), 1007. https://doi.org/10.3390/healthcare13091007






