Does Government Trust Matter? The Effectiveness of Policy Responses in the Health-Disaster Era
Abstract
:1. Introduction
2. Literature Review
2.1. Types of Policy Responses in COVID-19 Pandemic
2.2. The Effectiveness of Government Responses
2.3. Government Trust and Pandemic Performance
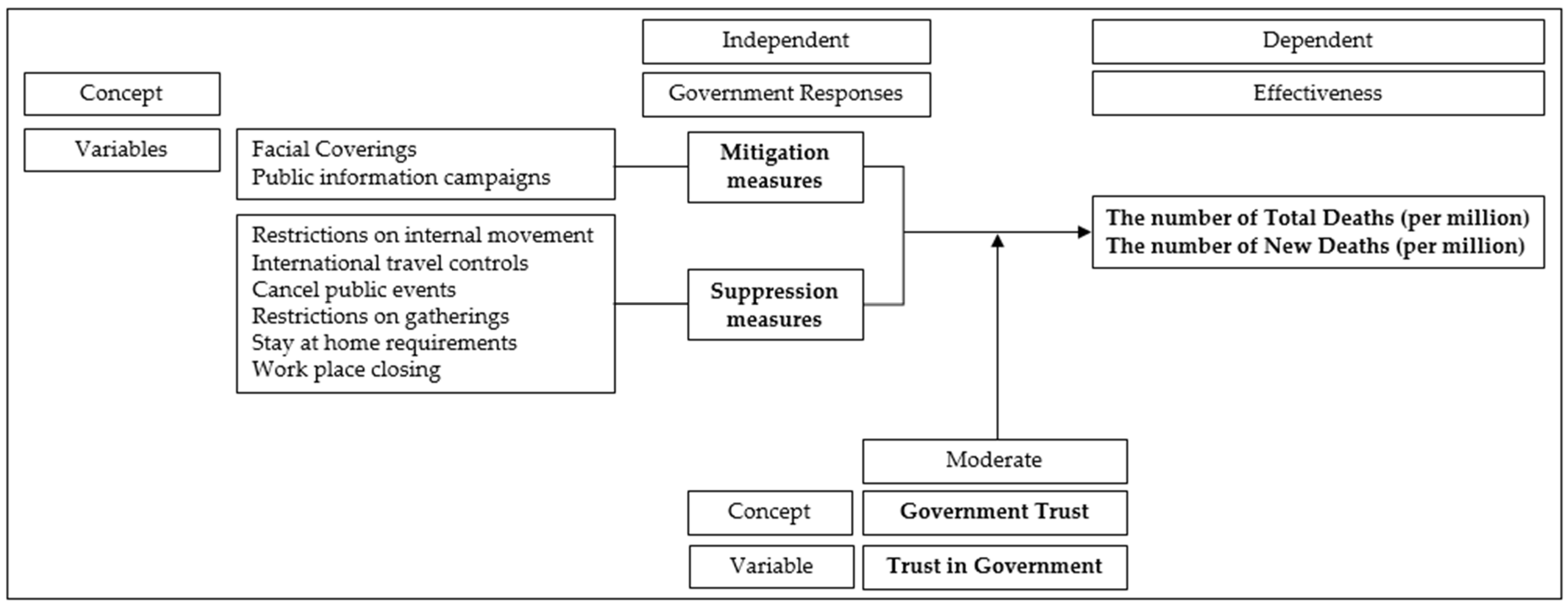
3. Materials and Methods
3.1. Measurement
3.2. Data and Methods
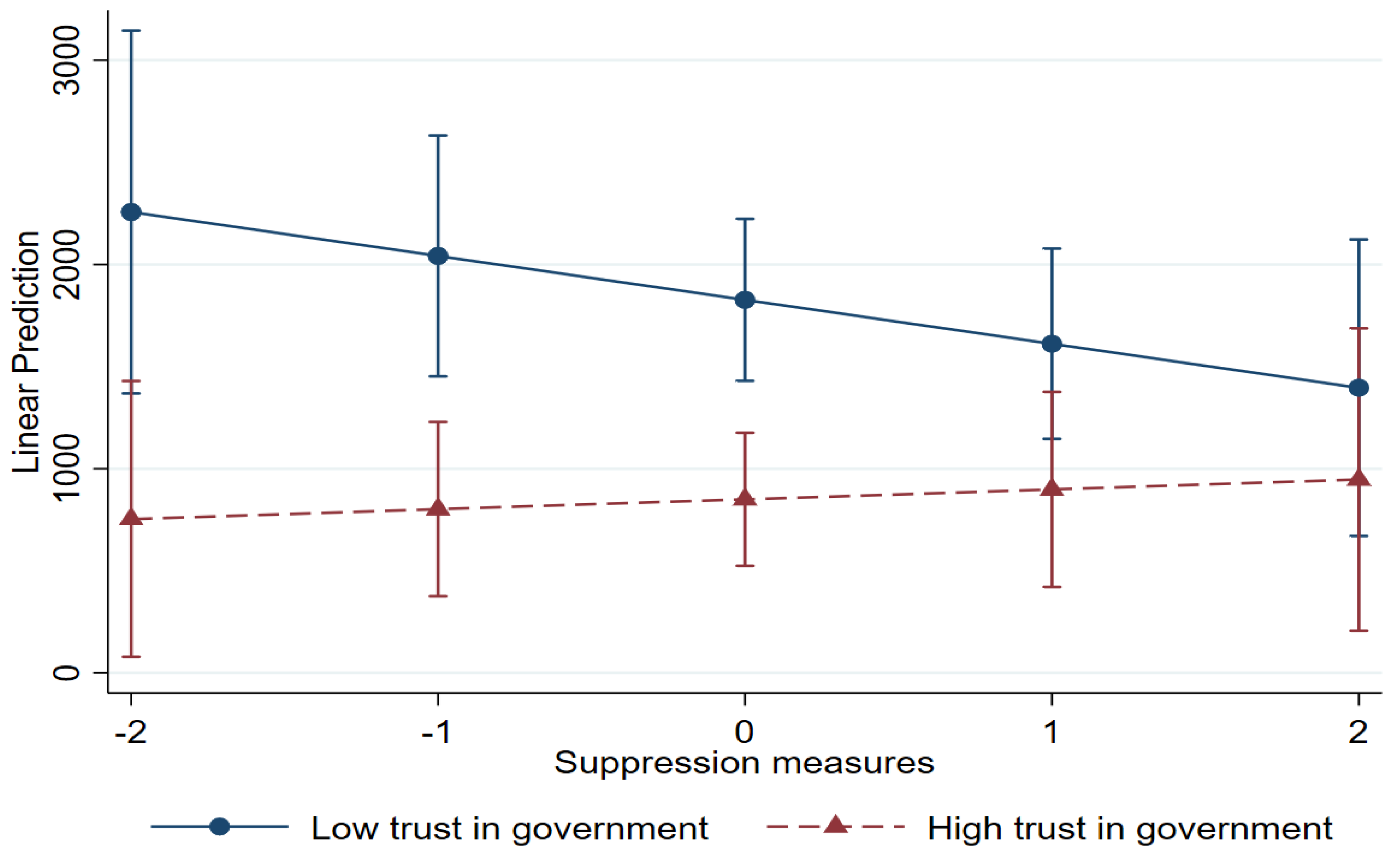
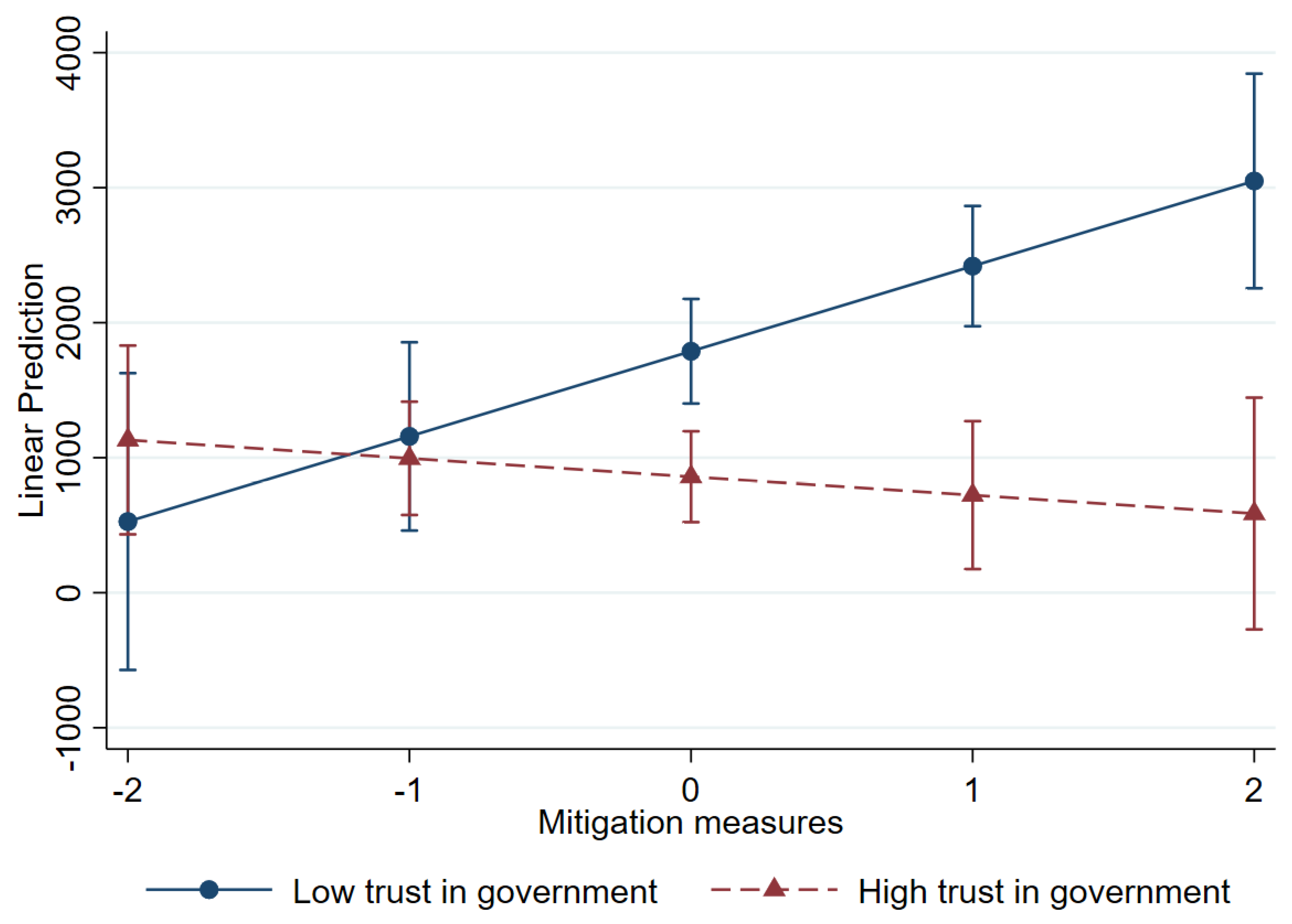
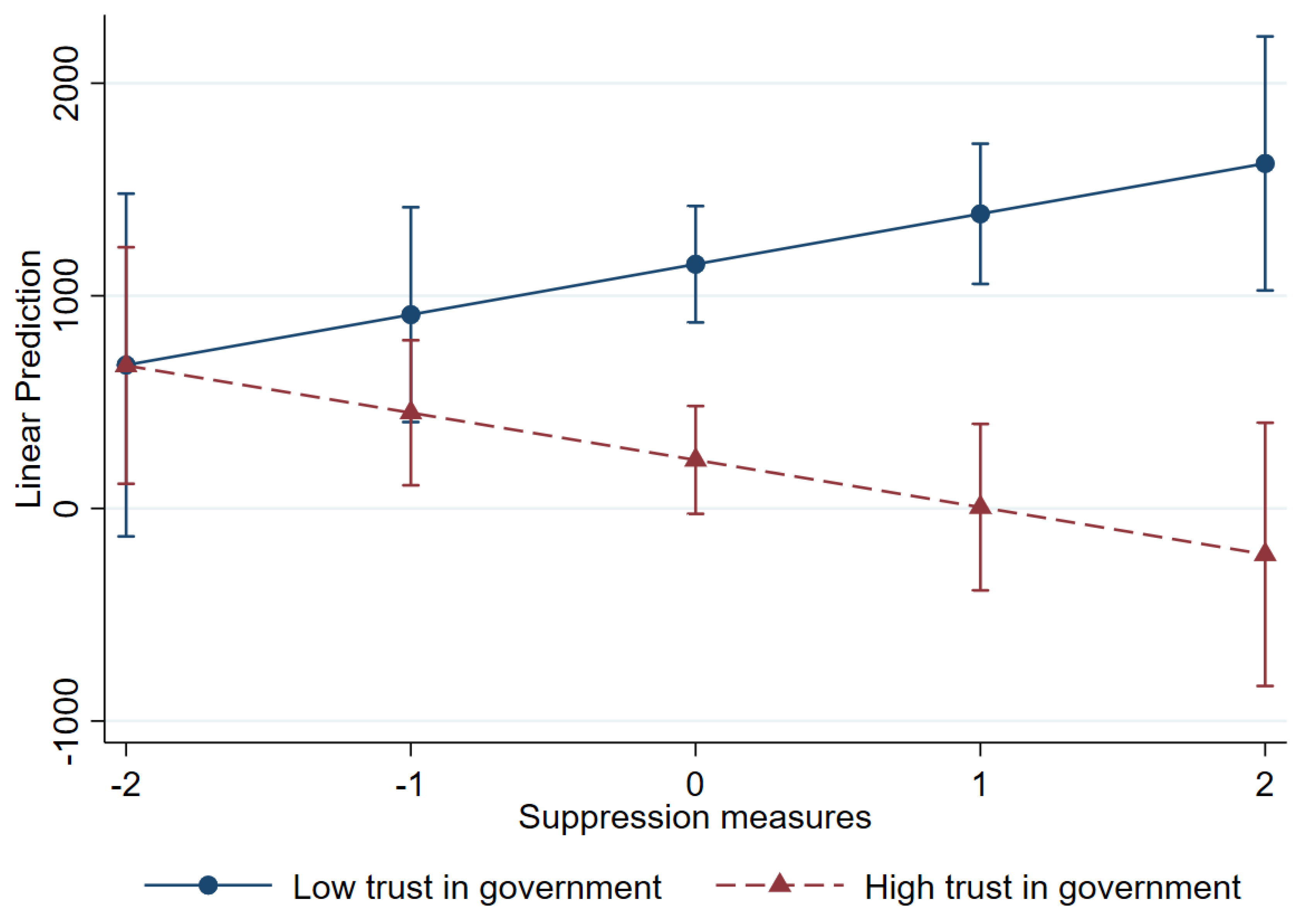
4. Results
4.1. Descriptive Analysis
4.2. Regression Analysis
5. Discussion
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Component | Suppression | Mitigation |
|---|---|---|
| Facial coverings | 0.409 | 0.748 |
| Restrictions on internal movement | 0.787 | −0.002 |
| International travel controls | 0.807 | −0.056 |
| Public information campaigns | −0.239 | 0.858 |
| Cancellation of public events | 0.945 | 0.026 |
| Restrictions on gatherings | 0.876 | 0.068 |
| Stay-at-home requirements | 0.873 | 0.055 |
| Workplace closures | 0.933 | 0.139 |
References
- Dergiades, T.; Milas, C.; Mossialos, E.; Panagiotidis, T. Effectiveness of government policies in response to the first COVID-19 outbreak. PLoS Glob. Public Health 2022, 2, e0000242. [Google Scholar] [CrossRef] [PubMed]
- Cowling, B.J.; Ali, S.T.; Ng, T.W.Y.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.W.; Lee, S.L.; Chiu, S.S.; et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020, 5, e279–e288. [Google Scholar] [CrossRef] [PubMed]
- Hartl, T.; Wälde, K.; Weber, E. Measuring the impact of the German public shutdown on the spread of COVID-19. COVID Econ. 2020, 1, 25–32. [Google Scholar]
- Hsiang, S.; Allen, D.; Annan-Phan, S.; Bell, K.; Bolliger, I.; Chong, T.; Druckenmiller, H.; Huang, L.Y.; Hultgren, A.; Krasovich, E.; et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020, 584, 262–267. [Google Scholar] [CrossRef]
- Mitze, T.; Kosfeld, R.; Rode, J.; Wälde, K. Face masks considerably reduce COVID-19 cases in Germany. Proc. Natl. Acad. Sci. USA 2020, 117, 32293–32301. [Google Scholar] [CrossRef]
- Agyapon-Ntra, K.; McSharry, P.E. A global analysis of the effectiveness of policy responses to COVID-19. Sci. Rep. 2023, 13, 5629. [Google Scholar] [CrossRef]
- Wang, J.; Kwak, D.; Park, C.M. Pandemic and Role of Government. In COVID-19 Pandemic in Korea: Public Views, 1st ed.; Park, C.M., Yoon, G.S., Eds.; Park Young-sa: Seoul, Republic of Korea, 2024; pp. 323–354. [Google Scholar]
- Fukuyama, F. Governance: What Do We Know, and How Do We Know It? Annu. Rev. Political Sci. 2016, 19, 89–105. [Google Scholar] [CrossRef]
- Ji, C.; Jiang, J.; Zhang, Y. Political trust and government performance in the time of COVID-19. World Dev. 2024, 176, 106499. [Google Scholar] [CrossRef]
- Thoradeniya, T.; Jayasinghe, S. COVID-19 and future pandemics: A global systems approach and relevance to SDGs. Glob. Health 2021, 17, 59. [Google Scholar] [CrossRef]
- Behl, A.; Nair, A.; Mohagaonkar, S.; Yadav, P.; Gambhir, K.; Tyagi, N.; Sharma, R.K.; Butola, B.S.; Sharma, N. Threat, challenges, and preparedness for future pandemics: A descriptive review of phylogenetic analysis based predictions. Infect. Genet. Evol. 2022, 98, 105217. [Google Scholar] [CrossRef]
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Hale, T.; Angrist, N.; Kira, B.; Goldszmidt, R.; Petherick, A.; Phillips, T. Pandemic Governance Requires Understanding Socioeconomic Variation in Government and Citizen Responses to COVID-19. SSRN 2020, June. Available online: https://ssrn.com/abstract=3641927 (accessed on 24 April 2024).
- World Health Organization(WHO). WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 27 April 2024).
- OECD. First lessons from government evaluations of COVID-19 responses: A synthesis. In OECD Policy Responses to Coronavirus (COVID-19); OECD Publishing: Paris, France, 2022. [Google Scholar] [CrossRef]
- Rahmouni, M. Efficacy of Government Responses to COVID-19 in Mediterranean Countries. Risk Manag. Healthc. Policy 2021, 14, 3091–3115. [Google Scholar] [CrossRef] [PubMed]
- Toshkov, D.; Carroll, B.; Yesilkagit, K. Government capacity, societal trust or party preferences: What accounts for the variety of national policy responses to the COVID-19 pandemic in Europe. J. Eur. Public Policy 2022, 29, 1009–1028. [Google Scholar] [CrossRef]
- Stanica, C.; Crosby, A.; Larson, S. Trust in Government and COVID-19 Response Policy: A Comparative Approach. J. Compar. Policy Anal. Res. Prac. 2023, 25, 156–171. [Google Scholar] [CrossRef]
- Ha, H.; Knox, C.; Janenova, S. Authoritarian and democratic states: The COVID-19 pandemic and the dfficacy of public health outcomes. J. Public Policy 2024, 44, 767–784. [Google Scholar] [CrossRef]
- Zaki, B.L.; Nicoli, F.; Wayenberg, E.; Verschuere, B. In trust we trust: The impact of trust in government on excess mortality during the COVID-19 pandemic. Public Policy Adm. 2022, 37, 226–252. [Google Scholar] [CrossRef]
- Ferguson, N.M.; Laydon, D.; Nedjati-Gilani, G.; Imai, N.; Ainslie, K.; Baguelin, M.; Bhatia, S.; Boonyasiri, A.; Cucunubá, Z.; Cuomo-Dannenburg, G.; et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. In MRC Centre for Global Infectious Disease Analysis Report 9; Imperial College London: London, UK, 2020. [Google Scholar]
- González-Bustamante, B. Evolution and early government responses to COVID-19 in South America. World Dev. 2021, 137, 1–8. [Google Scholar] [CrossRef]
- Wang, J. The Pandemic and the light and shade of the government intervention. In COVID-19 Pandemic in Korea: Public Views, 1st ed.; Park, C.M., Yoon, G.S., Eds.; Park Young-sa: Seoul, Republic of Korea, 2024; pp. 179–225. [Google Scholar]
- Slovic, P. Perceived risk, trust, and democracy. Risk Anal. 1993, 13, 675–682. [Google Scholar] [CrossRef]
- Poortinga, W.; Pidgeon, N.F. Exploring the Dimensionality of Trust in Risk Regulation. Risk Anal. 2003, 23, 961–972. [Google Scholar] [CrossRef]
- Siegrist, M.; Zingg, A. The Role of Public Trust During Pandemics. Eur. Psychol. 2014, 19, 23–32. [Google Scholar] [CrossRef]
- Siegrist, M. Trust and Risk Perception: A Critical Review of the Literature. Risk Anal. 2019, 41, 480–490. [Google Scholar] [CrossRef] [PubMed]
- Zahariadis, N.; Petridou, E.; Exadaktylos, T.; Sparf, J. The Politics of National Responses to the COVID-19 Pandemic. In Policy Styles and Trust in the Age of Pandemics: Global Threat, National Responses, 1st ed.; Zahariadis, N., Petridou, E., Exadaktylos, T., Sparf, J., Eds.; Routledge: New York, NY, USA, 2022; pp. 3–16. [Google Scholar]
- Bulut, H.; Samuel, R. The role of trust in government and risk perception in adherence to COVID-19 prevention measures: Survey findings among young people in Luxembourg. Health Risk Soc. 2023, 25, 324–349. [Google Scholar] [CrossRef]
- Steen, T.; Brandsen, T. Coproduction during and after the COVID-19 Pandemic: Will It Last? Public Adm. Rev. 2020, 80, 851–855. [Google Scholar] [CrossRef]
- Cao, C.; Li, N.; Liu, L. Do national cultures matter in the containment of COVID-19? Int. J. Sociol. Soc. Policy 2020, 40, 939–961. [Google Scholar] [CrossRef]
- Harring, N.; Jagers, S.C. Should We Trust in Values? Explaining Public Support for Pro-Environmental Taxes. Sustainability 2013, 5, 201–227. [Google Scholar] [CrossRef]
- Widaningrum, A. Public trust and regulatory compliance. J. ISIP 2017, 21. [Google Scholar] [CrossRef]
- Bollyky, T.J.; Hulland, E.N.; Barber, R.M.; Collins, J.K.; Kiernan, S.; Moses, M.; Pigott, D.M.; Reiner Jr, R.C.; Sorensen, R.J.D.; Abbafati, C.; et al. Pandemic preparedness and COVID-19: An exploratory analysis of infection and fatality rates, and contextual factors associated with preparedness in 177 countries, form Jan 1, 2020, to Sept 20, 2021. Lancet 2022, 399, 1489–1512. [Google Scholar] [CrossRef]
- Fetzer, T.; Witte, M.; Hensel, L.; Jachimowicz, J.M.; Haushofer, J.; Ivchenko, A.; Caria, S.; Reutskaja, E.; Roth, C.; Fiorin, S.; et al. Global Behaviors and Perceptions in the COVID-19 Pandemic. CEPR Discussion Paper No. DP14631 2020. Available online: https://ssrn.com/abstract=3594262 (accessed on 4 October 2024).
- Adolph, C.; Amano, K.; Bang-Jensen, B.; Fullman, N.; Wilkerson, J. Pandemic Politics: Timing State-Level Social Distancing Responses to COVID-19. J. Health Polit. Policy Law 2021, 46, 211–233. [Google Scholar] [CrossRef]
- Haerpfer, C.; Inglehart, R.; Moreno, A.; Welzel, C.; Kizilova, K.; Diez-Medrano, J.; Lagos, M.; Norris, P.; Ponarin, E.; Puranen, B. World Values Survey: Round Seven-Country-Pooled Datafile Version 5.0; Values Survey Association: Madrid, Spain; Vienna, Austria, 2022. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Gavrilov, D.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; et al. COVID-19 Pandemic. Published Online at OurWorldinData.org. 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 3 October 2024).
- OECD. Trust in Government Indicator. Available online: https://www.oecd.org/en/data/indicators/trust-in-government.html (accessed on 24 October 2024).
- World Bank. World Development Indicators. Available online: https://databank.worldbank.org/source/world-development-indicators (accessed on 11 November 2024).
- Korea Disease Control and Prevention Agency. KDCA White Paper; KDCA: Osong, Republic of Korea, 2023.
- Dye, T.R. Understanding Public Policy, 15th ed.; Pearson: Hoboken, NJ, USA, 2016; pp. 3–13. [Google Scholar]
- Lasswell, H.D. The Policy Orientation. In The Policy Sciences: Recent Developments in Scope and Method, 1st ed.; Lerner, D., Lasswell, H.D., Eds.; Stanford University Press: Stanford, CA, USA, 1951; pp. 3–15. [Google Scholar]
- Dror, Y. Public Policy Making Reexamined, 1st ed.; Routledge: New York, NY, USA, 1983; pp. 25–32. [Google Scholar]



| Variables | Min. | Max. | Mean | S.D. |
|---|---|---|---|---|
| Total deaths (per million) | 4.82 | 4859.79 | 1487.02 | 1133.79 |
| New deaths (per million) | 4.82 | 2935.60 | 746.43 | 556.78 |
| Suppression measures | 0.18 | 15.04 | 7.23 | 4.06 |
| Mitigation measures | 1.74 | 6.00 | 3.84 | 0.87 |
| Trust in government | 17.15 | 84.63 | 48.38 | 15.75 |
| Economic development | 13,254.95 | 94,277.96 | 38,420.32 | 15,373.47 |
| Aging population rate | 6.86 | 27.05 | 16.98 | 4.35 |
| Hospital beds (per thousand) | 1.13 | 13.05 | 4.47 | 2.62 |
| Human Development Index | 0.77 | 0.96 | 0.90 | 0.05 |
| Variables | 2020 | 2021 | 2022 |
|---|---|---|---|
| Total deaths (per million) | 609.64 | 1612.35 | 2239.07 |
| New deaths (per million) | 609.64 | 1002.71 | 626.94 |
| Suppression measures | 9.47 | 10.10 | 2.13 |
| Mitigation measures | 3.33 | 4.56 | 3.63 |
| Independent Variables | Dependent Variables | ||||
|---|---|---|---|---|---|
| Total Deaths (per million) | t-Value | New Deaths (per million) | t-Value | ||
| Trust in Gov. | below avg. | 1702.00 | 3.54 *** | 983.13 | 4.64 *** |
| above avg. | 980.18 | 508.27 | |||
| Suppression | below avg. | 2056.12 | 4.08 *** | 594.17 | −2.61 ** |
| above avg. | 1155.05 | 835.25 | |||
| Mitigation | below avg. | 1015.34 | −4.12 *** | 528.22 | −4.12 *** |
| above avg. | 1842.59 | 910.93 | |||
| Total Deaths (per million) | New Deaths (per million) | |||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Suppression measures | −135.624 | −302.787 | −34.185 | 390.056 |
| (133.504) | (241.802) | (96.610) | (238.630) | |
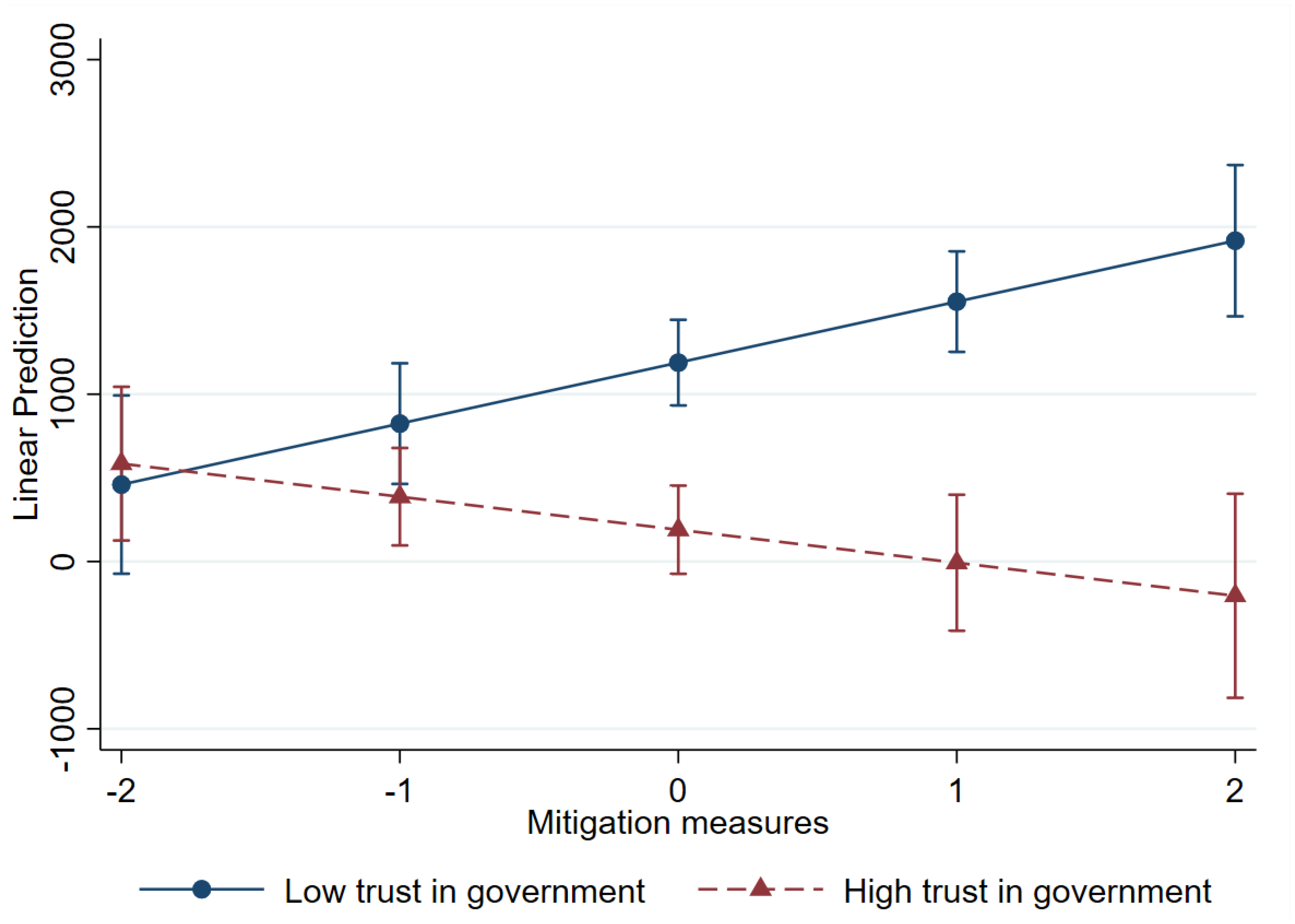
| Mitigation measures | 290.744 | 886.208 ** | 102.510 | 551.695 *** |
| (164.769) | (276.184) | (84.105) | (149.403) | |
| Trust in government | −13.378 * | −16.248 ** | −16.257 *** | −15.320 *** |
| (6.243) | (4.946) | (4.077) | (4.028) | |
| Suppression measures × Trust in government | 4.389 | −7.652 † | ||
| (3.842) | (4.022) | |||
| Mitigation measures × Trust in government | −12.781 *** | −9.364 *** | ||
| (3.564) | (2.696) | |||
| Economic development | 820.277 | 749.117 | 582.502 | 593.782 |
| (908.938) | (871.221) | (404.544) | (423.655) | |
| Aging population rate | 84.705 ** | 79.856 ** | 55.843 *** | 49.649 ** |
| (26.981) | (26.697) | (14.138) | (16.496) | |
| Hospital beds (per thousand) | −54.163 | −45.348 | −50.298 | −29.980 |
| (51.287) | (52.460) | (28.127) | (32.670) | |
| Human Development Index | −12,654.656 | −11,960.880 | −6587.950 | −6454.345 |
| (7487.267) | (7331.710) | (3683.646) | (3827.781) | |
| Year 2021 | 443.738 | 511.743 | 173.194 | 196.801 |
| (355.856) | (345.869) | (213.076) | (195.741) | |
| Year 2022 | 994.931 * | 1159.508 ** | −149.972 | −15.045 |
| (390.674) | (403.362) | (198.804) | (185.599) | |
| Constant | 3262.998 | 3454.582 | 653.227 | 276.521 |
| (3810.904) | (3512.675) | (1413.619) | (1541.312) | |
| R2 | 0.57 | 0.61 | 0.38 | 0.45 |
| Number of observations | 98 | 98 | 98 | 98 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J. Does Government Trust Matter? The Effectiveness of Policy Responses in the Health-Disaster Era. Healthcare 2025, 13, 959. https://doi.org/10.3390/healthcare13090959
Wang J. Does Government Trust Matter? The Effectiveness of Policy Responses in the Health-Disaster Era. Healthcare. 2025; 13(9):959. https://doi.org/10.3390/healthcare13090959
Chicago/Turabian StyleWang, Jaesun. 2025. "Does Government Trust Matter? The Effectiveness of Policy Responses in the Health-Disaster Era" Healthcare 13, no. 9: 959. https://doi.org/10.3390/healthcare13090959
APA StyleWang, J. (2025). Does Government Trust Matter? The Effectiveness of Policy Responses in the Health-Disaster Era. Healthcare, 13(9), 959. https://doi.org/10.3390/healthcare13090959






