Measuring Transformational Leadership in Establishing Nursing Care Excellence
Abstract
:1. Introduction
1.1. Transformational Leadership
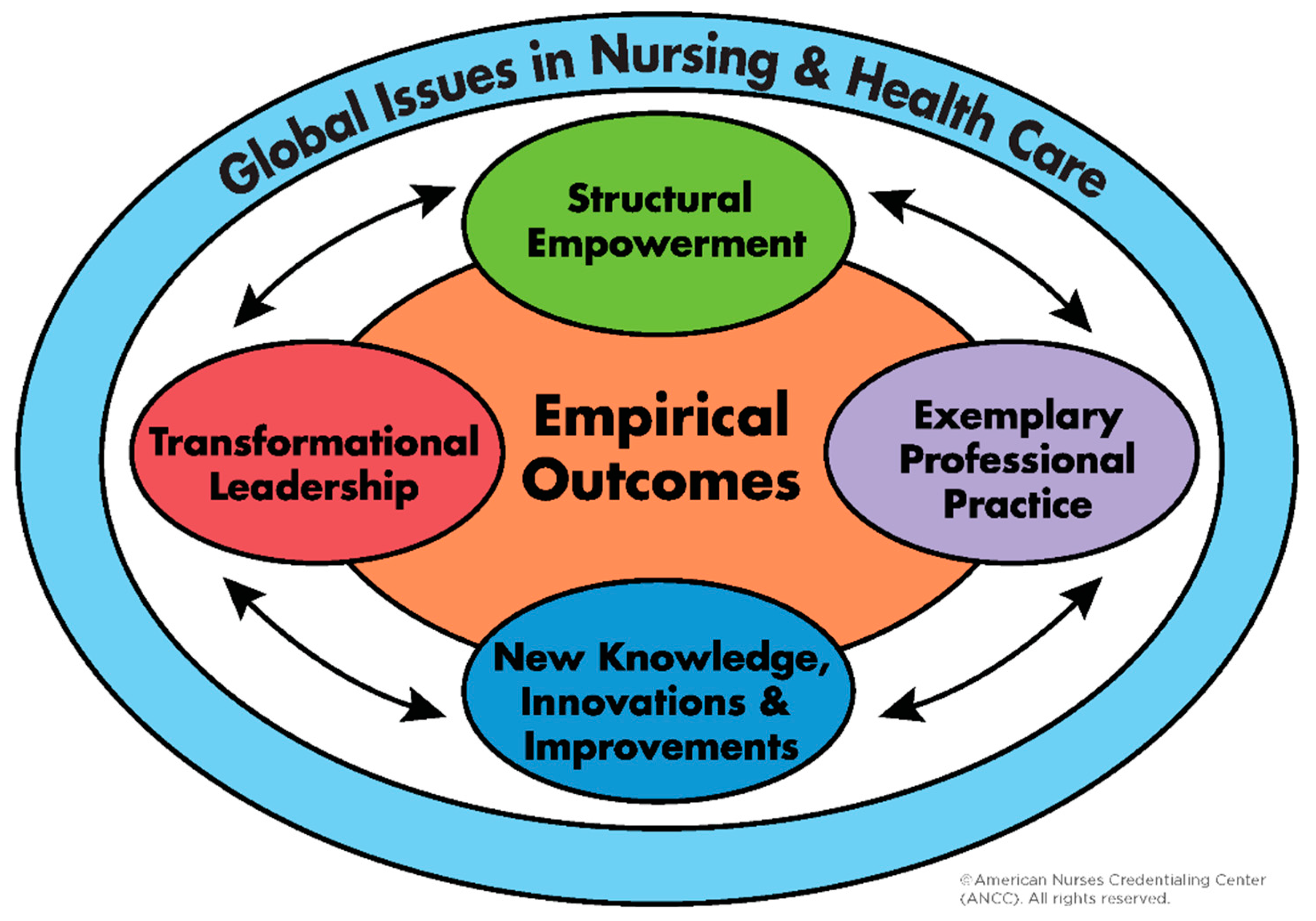
1.2. Transformational Leadership in Magnet®
1.3. Magnet® in Regional Australia
1.4. Study Purpose
2. Materials and Methods
3. Results
4. Discussion
4.1. Intellectual Stimulation
4.2. Individualized Consideration
4.3. Management-By-Exception
4.4. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bish, M. Chapter 2 Leadership and management frameworks and theories. In Leading and Managing in Health Services: An Australasian Aerspective, 1st ed.; Day, G.E., Leggat, S.G., Eds.; Cambridge University Press: Port Melbourne, Austrilia, 2015; pp. 16–28. [Google Scholar]
- West, M.; Armit, K.; Loewenthal, L.; Eckert, R.; West, T.; Lee, A. Leadership and Leadership Development in Health Care. The Faculty of Medical Leadership and Management: Lancaster University Management School, London, UK, 2015. Available online: https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/leadership-leadership-development-health-care-feb-2015.pdf (accessed on 1 November 2019).
- Bass, B. Leadership and Performance beyond Expectations; Free Press: New York, NY, USA, 1985. [Google Scholar]
- Bass, B.; Avolio, B. Multifactor Leadership Questionnaire—Manual, 3rd ed.; Mind Garden: Menlo Park, CA, USA, 2011. [Google Scholar]
- Barnes, H.; Rearden, J.; McHugh, M. Magnet® hospital recognition linked to lower central line-associated bloodstream infection rates. Res. Nurs. Health 2016, 39, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Bekelis, K.; Missios, S.; MacKenzie, T.A. Association of Magnet status with hospitalization outcomes for ischemic stroke patients. J. Am. Heart Assoc. 2017, 6. [Google Scholar] [CrossRef] [PubMed]
- Bormann, L.; Abrahamson, K. Do staff nurse perceptions of nurse leadership behaviors influence staff nurse job satisfaction? The case of a hospital applying for Magnet® designation. J. Nurs. Admin. 2014, 44, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Carter, S.S. The Relationship between Transformational Leadership and Organisational Learning Culture in Magnet and Non-Magnet Hospitals. Ph.D. Thesis, Northeastern University, Boston, MA, USA, 1 March 2016. [Google Scholar]
- Friese, C.; Xia, R.; Ghaferi, A.; Birkmeyer, J.; Banerjee, M. Hospitals In ‘Magnet’ Program Show Better Patient Outcomes On Mortality Measures Compared To Non-‘Magnet’ Hospitals. Health Affair. 2015, 34, 986–992. [Google Scholar] [CrossRef] [PubMed]
- Kutney-Lee, A.; Stimpfel, A.W.; Sloane, D.M.; Cimiotti, J.P.; Quinn, L.W.; Aiken, L.H. Changes in Patient and Nurse Outcomes Associated with Magnet Hospital Recognition. Med. Care. 2015, 53, 550–557. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.D.; Kelly, L.A.; Smith, H.L.; Wu, E.S.; Vanak, J.M.; Aiken, L.H. Lower Mortality in Magnet Hospitals. Med. Care. 2013, 51, 382–388. [Google Scholar] [CrossRef] [Green Version]
- West, S.L. The Influence of Magnet Designation on the Recruitment and Retention of Registered Nurses in a Hospital. Master’s Thesis, D’Youville College, Buffalo, NY, USA, 4 June 2014. [Google Scholar]
- ANCC. Magnet Model. Available online: https://www.nursingworld.org/organizational-programs/magnet/magnet-model/ (accessed on 3 October 2019).
- ANCC. Benefits. Available online: https://www.nursingworld.org/organizational-programs/magnet/why-become-magnet/benefits/ (accessed on 3 October 2019).
- Tai, T.W.C.; Bame, S.I. Organisational and community factors associated with Magnet status of U.S. hospitals. J. Healthc. Manag. 2017, 62, 62–76. [Google Scholar] [CrossRef]
- Moss, S.; Mitchell, M.; Casey, V. Creating a culture of success: Using the Magnet Recognition Program(R) as a framework to engage nurses in an Australian healthcare facility. J. Nurs. Adm. 2017, 47, 116–122. [Google Scholar] [CrossRef]
- Walker, K.; Fitzgerald, K.; Duff, J. Supporting a healthy culture: Results of the Practice Environment Scale, Australia in a Magnet® designated hospital. J. Nurs. Adm. 2014, 44, 653–658. [Google Scholar] [CrossRef]
- Walker, K.; Middleton, S.; Rolley, J.; Duff, J. Nurses report a healthy culture: Results of the Practice Environment Scale (Australia) in an Australian hospital seeking Magnet recognition. Int. J. Nurs. Pract. 2010, 16, 616–623. [Google Scholar] [CrossRef]
- Burns, J.M. Leadership; Harper & Row: New York, NY, USA, 1978. [Google Scholar]
- Bass, B.; Avolio, B. Improving Organisational Effectiveness Through Transformational Leadership; Sage Publications: Thousand Oaks, CA, USA, 1994. [Google Scholar]
- Cummings, G.G.; MacGregor, T.; Davey, M.; Lee, H.; Wong, C.A.; Lo, E.; Muise, M.; Stafford, E. Leadership styles and outcome patterns for the nursing workforce and work environment: A systematic review. Int. J. Nurs. Stud. 2010, 47, 363–385. [Google Scholar] [CrossRef] [PubMed]
- Bottomley, P.; Mostafa, A.M.S.; Gould-Williams, J.S.; León-Cázares, F. The impact of transformational leadership on organizational citizenship behaviours: The contingent role of public service motivation. Br. J. Manag. 2016, 27, 390–405. [Google Scholar] [CrossRef]
- Hayati, D.; Charkhabi, M.; Naami, A.Z. The relationship between transformational leadership and work engagement in governmental hospitals nurses: A survey study. SpringerPlus 2014, 3. [Google Scholar] [CrossRef] [PubMed]
- Andrews, D.R.; Richard, D.C.S.; Robinson, P.; Celano, P.; Hallaron, J. The influence of staff nurse perception of leadership style on satisfaction with leadership: A cross-sectional survey of pediatric nurses. Int. J. Nurs. Stud. 2012, 49, 1103–1111. [Google Scholar] [CrossRef] [PubMed]
- Gardner, B.D. Improve RN retention through transformational leadership styles. Nurs. Manag. 2010, 41. [Google Scholar] [CrossRef]
- Weberg, D. Transformational leadership and staff retention. Nurs. Adm. Q. 2010, 34, 246–258. [Google Scholar] [CrossRef]
- ANCC. Magnet Recognition Program® Overview: Teaching Tips; ANCC: Silver Spring, MD, USA, 2011. [Google Scholar]
- Hayden, M.A.; Wolf, G.A.; Zedreck-Gonzalez, J.F. Beyond Magnet® designation: Perspectives from nurse managers on factors of sustainability and high-performance programming. J. Nurs. Admin. 2016, 46, 530–534. [Google Scholar] [CrossRef]
- Australian Department of Health. Nursing and Midwifery Retention. Available online: http://www.health.gov.au/internet/publications/publishing.nsf/Content/work-review-australian-government-health-workforce-programs-toc~chapter-7-nursing-midwifery-workforce%E2%80%93education-retention-sustainability~chapter-7-nursing-midwifery-retention (accessed on 3 October 2019).
- Dawson, A.J.; Stasa, H.; Roche, M.A.; Homer, C.S.; Duffield, C. Nursing churn and turnover in Australian hospitals: Nurses perceptions and suggestions for supportive strategies. BMC Nurs. 2014, 13. [Google Scholar] [CrossRef]
- Duffield, C.M.; Roche, M.A.; Blay, N.; Stasa, H. Nursing unit managers, staff retention and the work environment. J. Clin. Nurs. 2011, 20, 23–33. [Google Scholar] [CrossRef]
- Thomas, L.; Chaperon, Y. Submission to the Health Workforce Australia Consultation Paper on Nursing Workforce Retention and Productivity; Australian Nursing and Midiwifery Federation: Melbourne, Austrilia, 2013. [Google Scholar]
- Australian College of Nursing. Nurses are Essential in Health and Aged Care Reform. Available online: https://www.acn.edu.au/wp-content/uploads/white-paper-nurses-essential-health-aged-care-reform.pdf (accessed on 3 October 2019).
- Australian Bureau of Statistics Remoteness Structure. Available online: http://www.abs.gov.au/websitedbs/d3310114.nsf/home/remoteness+structure (accessed on 3 October 2019).
- Tasmanian Department of Treasury and Finances. Population; Cat. No. 3101.0; ABS, Tasmanian Department of Treasury and Finances: Hobart, Austrilia, 2018.
- Tasmanian Department of Health. The State of Public Health: Tasmania 2018; Tasmanian Government: Hobart, Austrilia, 2018.
- Tasmanian Department of Health. Tasmanian Strategic Health Workforce Framework: Delivering Future Care (Discussion Paper). Available online: https://anmftas.org.au/wp-content/uploads/2013/12/Tasmanian-Strategic-Workforce-Discussion-Paper1.pdf (accessed on 3 October 2019).
- Bass, B.; Avolio, B. Multifactor Leadership Questionnaire—Short Form 6S; Center for Leadership Studies: Binghamton, NY, USA, 1992. [Google Scholar]
- Antonakis, J. Charisma and the “new leadership”. In The Nature of Leadership; Antonakis, J., Day, D., Eds.; SAGE: Thousand Oaks, CA, USA, 2018; pp. 54–81. [Google Scholar]
- Elenkov, D.S.; Judge, W.; Wright, P. Strategic leadership and executive innovation influence: An international multi-cluster comparative study. Strateg. Manag. J. 2005, 26, 665–682. [Google Scholar] [CrossRef]
- Hand, L.E. Role Factors, Leadership Styles and Stress Among Catholic Primary School Executives. Master’s Thesis, Bond University, Gold Coast, Austrilia, 9 October 2010. [Google Scholar]
- Tejeda, M.J.; Scandura, T.; Pillai, R. The MLQ revisited: Psychometric properties and recommendations. Leadership Quart. 2001, 12, 31–52. [Google Scholar] [CrossRef]
- LimeSurvey. Available online: https://www.limesurvey.org/ (accessed on 3 October 2019).
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Van Dam, P.J.; Ford, K.M. Nursing leadership learning in practice: A four stage learning process. Int. Arch. Nurs. Health Care 2019, 5, 3. [Google Scholar] [CrossRef]
- Elliott, N.; Begley, C.; Sheaf, G.; Higgins, A. Barriers and enablers to advanced practitioners’ ability to enact their leadership role: A scoping review. Int. J. Nurs. Stud. 2016, 24–45. [Google Scholar] [CrossRef] [PubMed]
- Doucette, J.N. Aligning systems with the Magnet® Model to create a culture of safety. Nurs. Manag. 2012, 7, 52–55. [Google Scholar] [CrossRef]
- Arthurs, K.; Bell-Gordon, C.; Chalupa, B.; Rose, A.L.; Martinez, D.; Watson, J.A.; Bernard, D.P. A culture of nursing excellence: A community hospital’s journey from Pathway to Excellence® to Magnet® recognition. J. Nurs. Edu. Prac. 2018, 8, 5. [Google Scholar] [CrossRef]
- Clavelle, J.T.; Drenkard, K.; Tullai-McGuinness, S.; Fitzpatrick, J.J. Transformational leadership practices of chief nursing officers in Magnet® organizations. J. Nurs. Admin. 2012, 42, 195–201. [Google Scholar] [CrossRef]
- ANCC. International Information for the Magnet Program. Available online: https://www.nursingworld.org/organizational-programs/magnet/international/ (accessed on 3 October 2019).
- Bines, J.E.; Jamieson, P. Designing new collaborative learning space in clinical environments: Experiences from a children’s hospital in Australia. J. Interprof. Care 2013, 27. [Google Scholar] [CrossRef]
- Productivity Commission. Chapter 12 Public Hospitals. Available online: https://www.pc.gov.au/research/ongoing/report-on-government-services/2017/health/public-hospitals/rogs-2017-volumee-chapter12.pdf (accessed on 3 October 2019).
- Manning, J. The influence of nurse manager leadership style on staff nurse work engagement. J. Nurs. Admin. 2017, 46, 438–443. [Google Scholar] [CrossRef]
- Herman, S.; Gish, M.; Rosenblum, R.; Herman, M. Effects of RN age and experience on transformational leadership practices. J. Nurs. Admin. 2017, 47, 327–337. [Google Scholar] [CrossRef]
- Aarons, G.; Sommerfeld, D. Leadership, innovation climate, and attitudes toward evidence-based practice during a statewide implementation. J. Am. Acad. Child Psy. 2012, 51, 423–431. [Google Scholar] [CrossRef]
- Wallis, M.; Chaboyer, W. Building the clinical bridge: An Australian success. Nurs. Res. Pract. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Witmer, H.; Mellinger, M.S. Organisational resilience: Nonprofit organizations’ response to change. Work 2016, 54, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Eagly, A.H.; Johannesen-Schmidt, M.C.; van Engen, M.L. Transformational, transactional, and laissez-faire leadership styles: A meta-analysis comparing women and men. Psychol. Bull. 2003, 129, 569–591. [Google Scholar] [CrossRef] [PubMed]
- Stempel, C.R.; Rigotti, T.; Mohr, G. Think transformational leadership: Think female? Leadership 2015, 11, 259–280. [Google Scholar] [CrossRef]
| Full Range Leadership | Element |
|---|---|
| Transformational leadership | Idealized Influence |
| Inspirational Motivation | |
| Intellectual Stimulation | |
| Individualized Consideration | |
| Transactional leadership | Contingent Rewards |
| Active Management-By-Exception | |
| Passive/avoidant leadership | Passive Management-By-Exception |
| Laissez-Faire |
| Category | Description | No. of Responses (%) |
|---|---|---|
| Total | 78 (100) | |
| Gender | Female | 67 (86) |
| Male | 11 (14) | |
| Other | 0 | |
| Age | 31–35 years | 4 (5) |
| 36–40 years | 7 (9) | |
| 41–45 years | 6 (7) | |
| 46–50 years | 15 (19) | |
| 51–55 years | 17 (22) | |
| 56–60 years | 21 (27) | |
| 61 or older | 8 (10) | |
| Region | North | 27 (35) |
| North West | 19 (24) | |
| South | 32 (41) | |
| Role | Nurse Manager with no clinical responsibilities | 10 (13) |
| Nurse (Unit) Manager | 47 (60) | |
| Assistant Director of Nursing | 12 (15) | |
| (Co-) Director or Executive Director of Nursing | 9 (12) | |
| Highest education | Hospital/training Certificate | 6 (8) |
| Bachelor’s Degree | 11 (14) | |
| Post-graduate Certificate | 12 (15) | |
| Post-graduate Diploma | 22 (28) | |
| Master’s Degree | 27 (35) | |
| Doctoral Degree | 0 (0) | |
| Work length at current hospital | Less than 1 year | 1 (1) |
| 1–5 years | 7 (9) | |
| 6–10 years | 12 (15) | |
| 11–15 years | 8 (10) | |
| 16–20 years | 8 (10) | |
| 21 years plus | 42 (54) | |
| Work setting | Community/Primary care | 4 (5) |
| Hospital/Acute care | 66 (85) | |
| Non-hospital inpatient facility (sub-acute care) | 3 (4) | |
| Other | 5 (6) | |
| MLQ Factors (MLQ-6S) | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Factor 6 | Factor 7 | |
|---|---|---|---|---|---|---|---|---|
| Leadership styles | Transformational | Transactional | Passive/Avoidant | |||||
| MLQ-6S score average | 9.2 | 8.6 | 8.7 | 9.5 | 7.2 | 8.4 | 4.1 | |
| Average score for leadership style | 9.0 | 7.2 | 6.3 | |||||
| Demographic variance | Idealized Influence (mean (SD 1)) | Inspirational Motivation (mean (SD)) | Intellectual Stimulation (mean (SD)) | Individualized Consideration (mean (SD)) | Contingent Reward (mean (SD)) | Management-By-Exception (mean (SD)) | Laissez Faire (mean (SD)) | |
| Gender | Female | 9.2 (1.4) | 8.6 (1.5) | 8.6 (1.7) | 9.5 (1.5) | 7.2 (2.3) | 8.6 (1.5) | 4.3 (2.1) |
| Male | 9.1 (1.6) | 8.8 (1.1) | 8.7 (1.4) | 9.1 (1.3) | 7.0 (2.0) | 7.5 (2.1) | 3.2 (1.8) | |
| p-value 2 | 0.79 | 0.66 | 0.88 | 0.37 | 0.74 | 0.04 | 0.07 | |
| Age | 31–35 | 9.5 (0.6) | 8.8 (1.3) | 9.3 (2.5) | 8.5 (1.3) | 5.8 (1.3) | 9.3 (1.7) | 4.5 (2.1) |
| 36–40 | 9.0 (1.5) | 9.4 (1.0) | 8.9 (1.6) | 8.6 (1.5) | 7.7 (2.0) | 7.1 (0.9) | 3.6 (2.2) | |
| 41–45 | 10.0 (1.4) | 7.8 (1.6) | 7.5 (0.8) | 8.8 (1.5) | 6.7 (2.1) | 7.7 (1.0) | 2.8 (2.4) | |
| 46–50 | 9.2 (1.5) | 8.9 (1.4) | 8.8 (1.7) | 8.9 (1.2) | 7.1 (2.6) | 8.3 (1.2) | 4.1 (1.8) | |
| 51–55 | 9.5 (1.5) | 9.1 (1.4) | 9.2 (1.4) | 10.2 (1.7) | 7.9 (2.3) | 8.4 (2.2) | 4.2 (2.3) | |
| 56–60 | 8.8 (1.3) | 8.2 (1.5) | 8.4 (1.7) | 9.8 (1.2) | 7.1 (1.9) | 9.1 (1.5) | 4.8 (2.0) | |
| ≥ 61 | 9.0 (1.2) | 8.0 (1.1) | 8.1 (2.2) | 9.8 (1.2) | 7.0 (2.8) | 7.9 (1.6) | 3.6 (1.6) | |
| p-value | 0.48 | 0.13 | 0.34 | 0.03 | 0.66 | 0.06 | 0.46 | |
| Highest completed Education | Hospital training | 8.8 (1.2) | 7.2 (1.3) | 8.0 (1.4) | 9.2 (1.2) | 7.2 (1.8) | 9.3 (1.6) | 4.7 (0.8) |
| Bachelor’s | 9.1 (1.0) | 8.9 (0.9) | 8.6 (1.2) | 9.0 (1.5) | 7.3 (2.3) | 8.2 (1.0) | 4.6 (1.5) | |
| Post-grad Certificate | 9.0 (1.3) | 8.4 (1.2) | 7.4 (1.4) | 9.5 (1.3) | 6.6 (2.4) | 8.3 (1.5) | 4.3 (1.6) | |
| Post-grad Diploma | 9.6 (1.4) | 8.5 (1.6) | 8.7 (1.6) | 9.7 (1.6) | 7.4 (2.4) | 8.6 (1.7) | 4.3 (2.4) | |
| Master’s | 9.1 (1.6) | 8.9 (1.5) | 9.3 (1.7) | 9.5 (1.5) | 7.3 (2.2) | 8.2 (1.9) | 3.6 (2.3) | |
| Doctoral | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| p-value | 0.70 | 0.08 | 0.02 | 0.73 | 0.89 | 0.51 | 0.62 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moon, S.E.; Van Dam, P.J.; Kitsos, A. Measuring Transformational Leadership in Establishing Nursing Care Excellence. Healthcare 2019, 7, 132. https://doi.org/10.3390/healthcare7040132
Moon SE, Van Dam PJ, Kitsos A. Measuring Transformational Leadership in Establishing Nursing Care Excellence. Healthcare. 2019; 7(4):132. https://doi.org/10.3390/healthcare7040132
Chicago/Turabian StyleMoon, Sarah E., Pieter J. Van Dam, and Alex Kitsos. 2019. "Measuring Transformational Leadership in Establishing Nursing Care Excellence" Healthcare 7, no. 4: 132. https://doi.org/10.3390/healthcare7040132
APA StyleMoon, S. E., Van Dam, P. J., & Kitsos, A. (2019). Measuring Transformational Leadership in Establishing Nursing Care Excellence. Healthcare, 7(4), 132. https://doi.org/10.3390/healthcare7040132





