The Impact of Joining a Team on the Initial Trust in Online Physicians
Abstract
1. Introduction
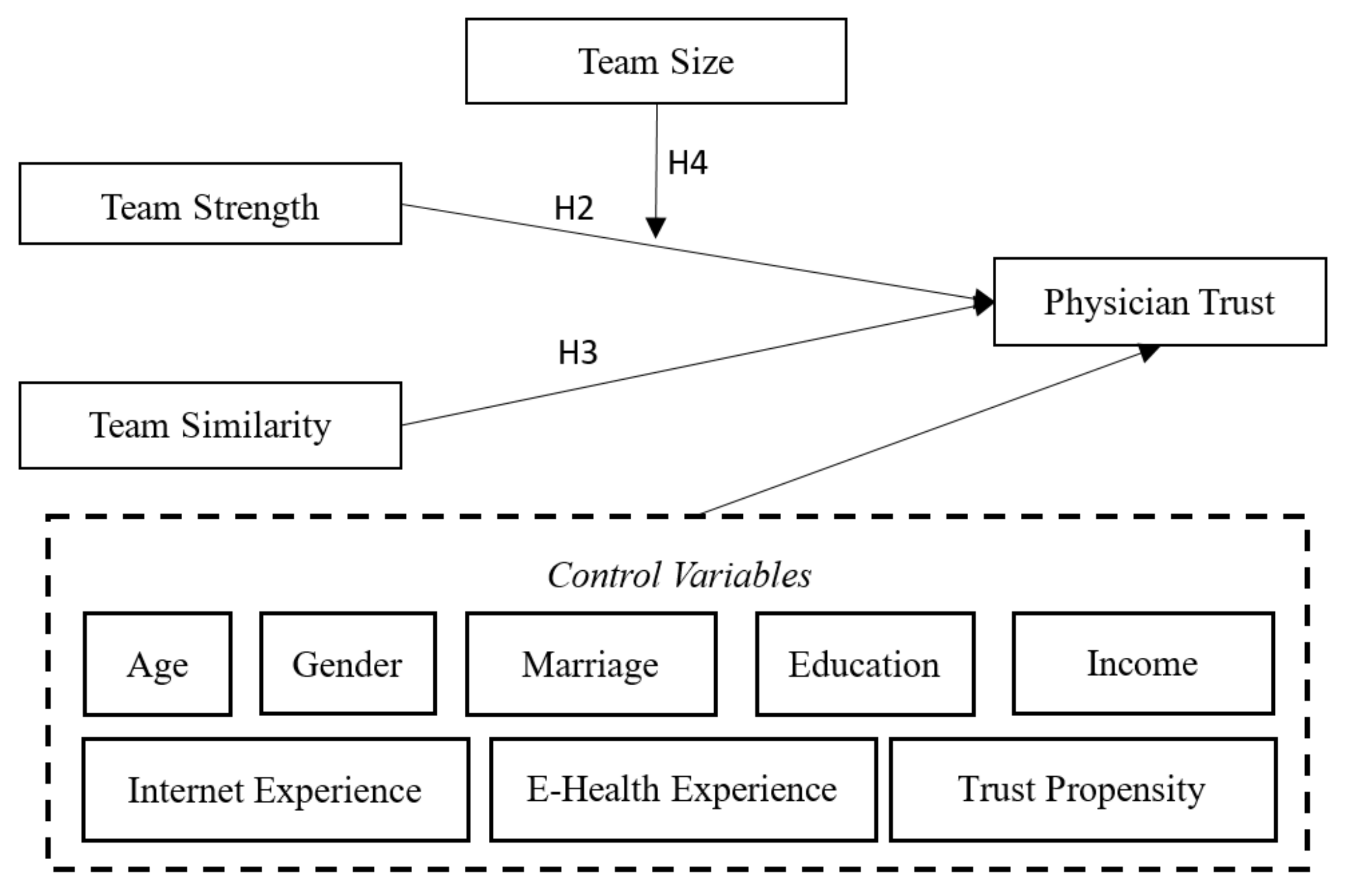
2. The Research Model and Hypothesis Development
3. Research Methodology
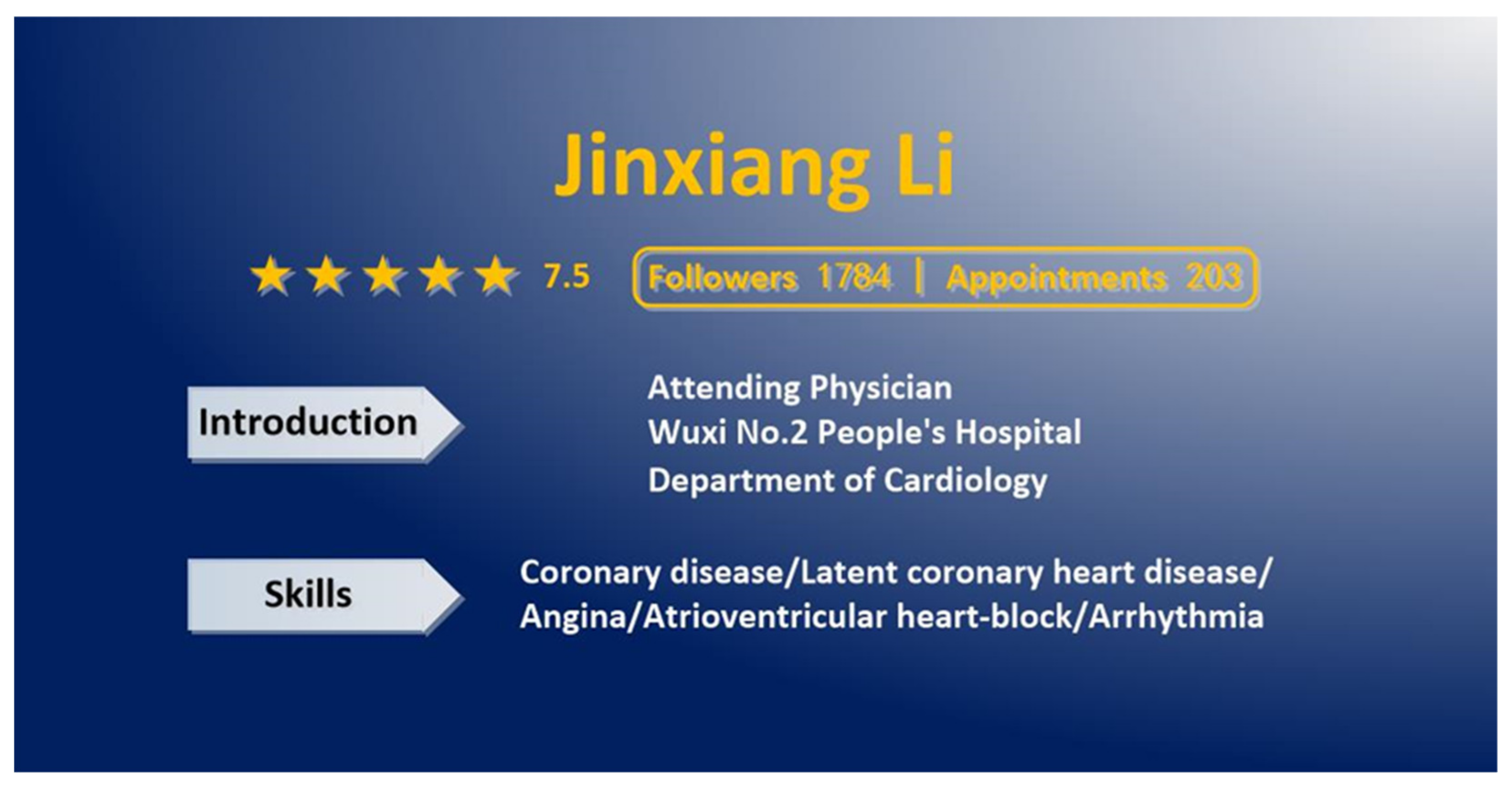
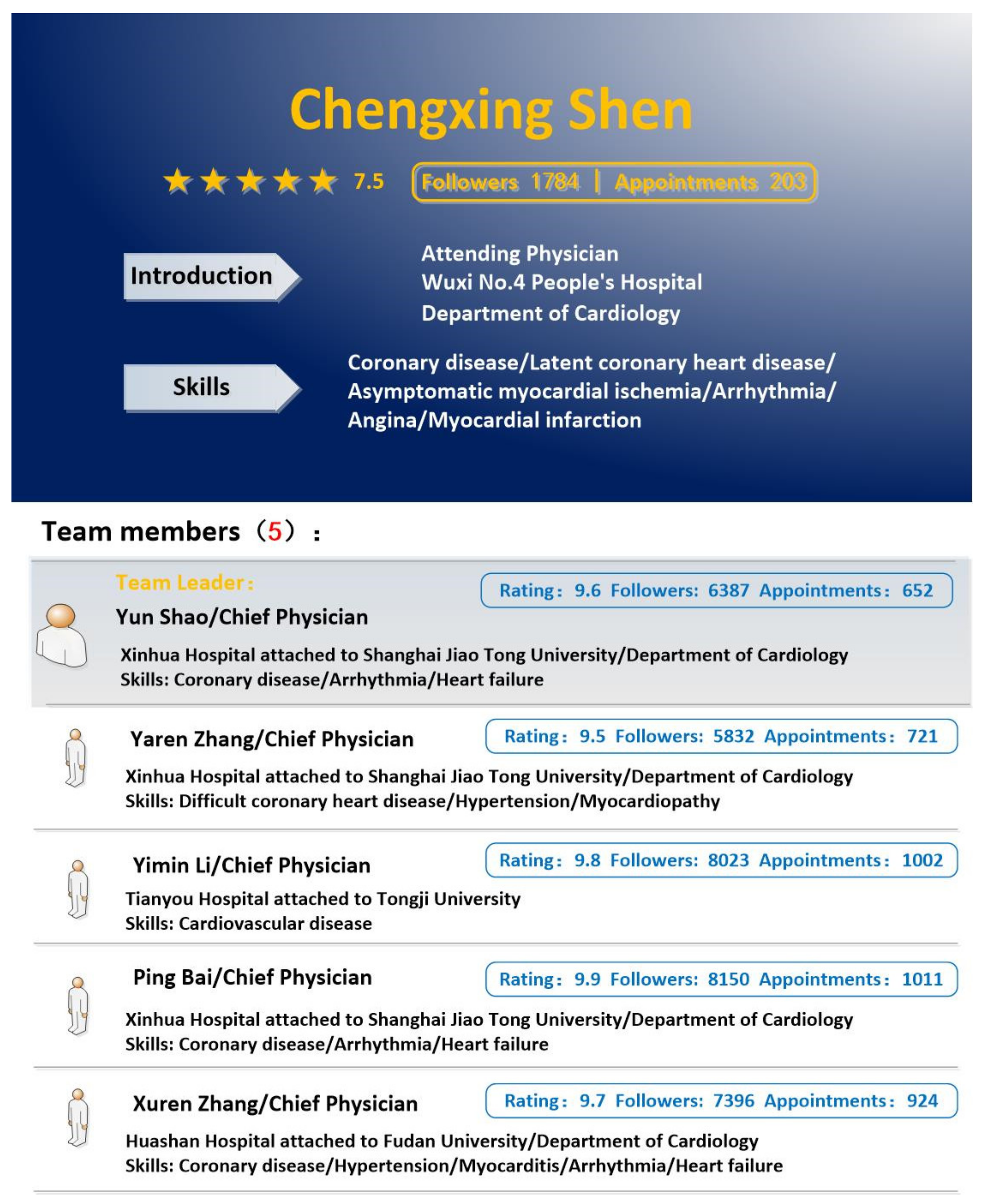
3.1. Experimental Design
3.2. Measures
4. Data Analysis and Results
4.1. The Measurement Model
4.2. The Impact of Working in a Team on Physician Trust
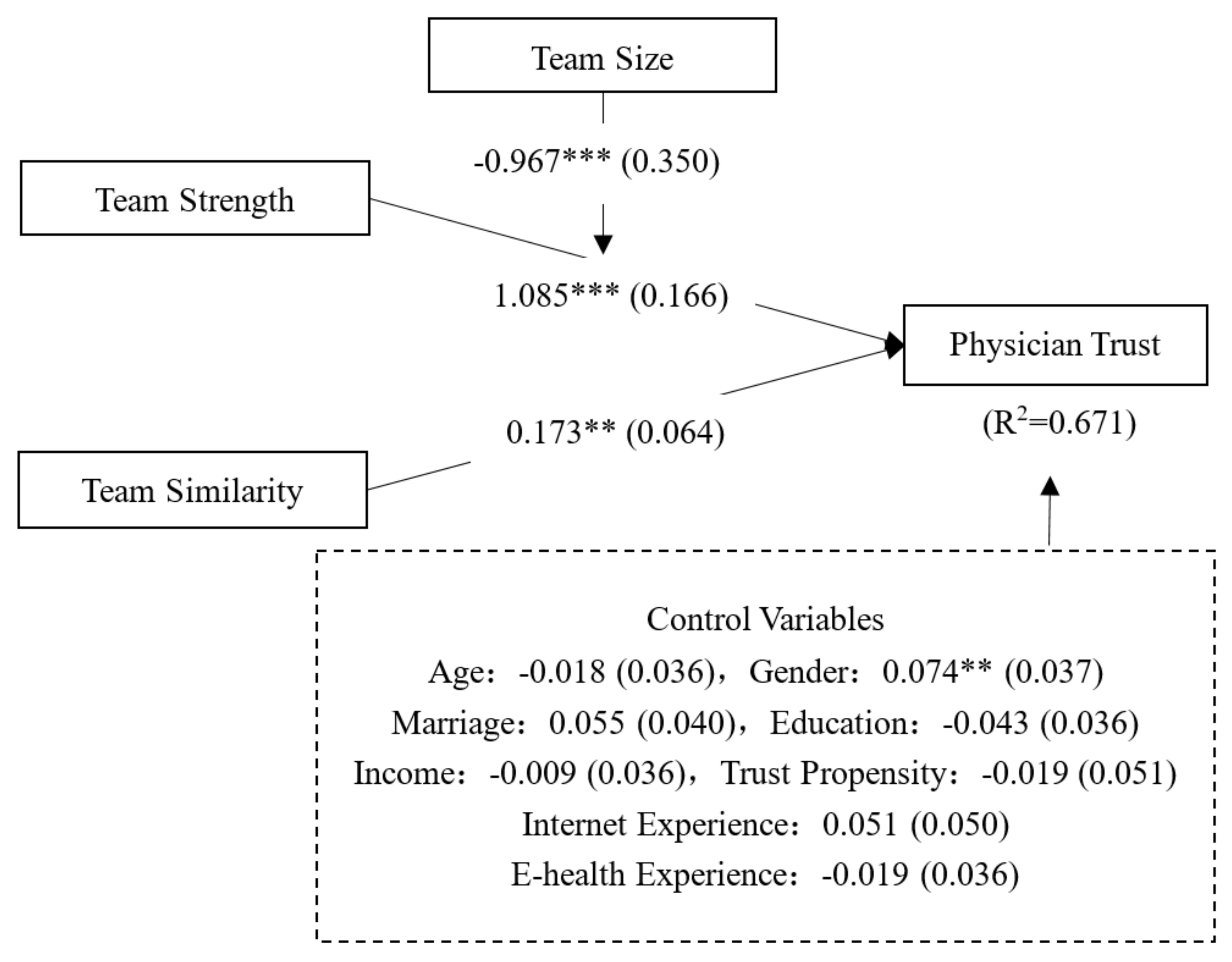
4.3. The Structural Model
5. Research Analysis and Discussion
5.1. Key Findings
5.2. Theoretical Contribution
5.3. Implications
6. Limitations and Future Research
Author Contributions
Funding
Conflicts of Interest
References
- Gefen, D.; Karahanna, E.; Straub, D.W. Trust and TAM in online shopping: An integrated model. MIS Q. 2003, 27, 51–90. [Google Scholar] [CrossRef]
- Pavlou, P.A.; Gefen, D. Building effective online marketplaces with institution-based trust. Inf. Syst. Res. 2004, 15, 37–59. [Google Scholar] [CrossRef]
- Brown, J.; Morgan, J. Reputation in online auctions: The market for trust. Calif. Manag. Rev. 2006, 49, 61–81. [Google Scholar] [CrossRef]
- Li, J.; Zhang, Y.; Ma, L.; Liu, X. The impact of the Internet on health consultation market concentration: An econometric analysis of secondary data. J. Med. Syst. 2016, 18, e276. [Google Scholar] [CrossRef] [PubMed]
- Dávalos, M.E.; French, M.T.; Burdick, A.E.; Simmons, S.C. Economic evaluation of telemedicine: Review of the literature and research guidelines for benefit–cost analysis. Telemed. J. E-health 2009, 15, 933–948. [Google Scholar] [CrossRef]
- Bloom, G.; Standing, H.; Lloyd, R. Markets, information asymmetry and health care: Towards new social contracts. Soc. Sci. Med. 2008, 66, 2076–2087. [Google Scholar] [CrossRef]
- Wun, Y.T.; Lam, T.P.; Lam, K.F.; Goldberg, D.; Li, D.K.; Yip, K.C. How do patients choose their doctors for primary care in a free market? J. Eval. Clin. Pract. 2010, 16, 1215–1220. [Google Scholar] [CrossRef]
- Li, J.; Tang, J.; Jiang, L.; Yen, D.C.; Liu, X. Economic success of physicians in the online consultation market: A signaling theory perspective. Int. J. Electron. Commer. 2019, 23, 244–271. [Google Scholar] [CrossRef]
- Liu, X.; Chen, M.; Li, J.; Ma, L. How to manage diversity and enhance team performance: Evidence from online doctor teams in China. Inter. J. Env. Res. Pub. Heal. 2020, 17, 48. [Google Scholar] [CrossRef]
- Keijser, W.; Smits, J.; Penterman, L.; Wilderom, C. Physician leadership in e-health? A systematic literature review. Leadersh. Health Serv. 2016, 29, 331–347. [Google Scholar] [CrossRef]
- Weller, J.; Boyd, M.; Cumin, D. Teams, tribes and patient safety: Overcoming barriers to effective teamwork in healthcare. Postgra. Med. J. 2014, 90, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Baggs, J.G.; Schmitt, M.H.; Mushlin, A.I.; Mitchell, P.H.; Eldredge, D.H.; Oakes, D.; Hutson, A.D. Association between nurse-physician collaboration and patient outcomes in three intensive care units. Crit. Care Med. 1999, 27, 1991–1998. [Google Scholar] [CrossRef] [PubMed]
- Rafferty, A.-M.; Ball, J.; Aiken, L.H. Are teamwork and professional autonomy compatible, and do they result in improved hospital care? Qual. Health Care 2001, 10, ii32–ii37. [Google Scholar] [CrossRef] [PubMed]
- Farland, M.Z.; Byrd, D.C.; McFarland, M.S.; Thomas, J.; Franks, A.S.; George, C.M.; Gross, B.N.; Guirguis, A.B.; Suda, K.J. Pharmacist-physician collaboration for diabetes care: The diabetes initiative program. Ann. Pharmacother. 2013, 47, 781–789. [Google Scholar] [CrossRef] [PubMed]
- Hillen, M.A.; de Haes, H.C.; Smets, E. Cancer patients’ trust in their physician—A review. Psychooncology 2011, 20, 227–241. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-Y.; Lin, J.L. The effects of trust in physician on self-efficacy, adherence and diabetes outcomes. Soc. Sci. Med. 2009, 68, 1060–1068. [Google Scholar] [CrossRef]
- Hinnen, C.; Pool, G.; Holwerda, N.; Sprangers, M.; Sanderman, R.; Hagedoorn, M. Lower levels of trust in one’s physician is associated with more distress over time in more anxiously attached individuals with cancer. Gen. Hosp. Psychiatry 2014, 36, 382–387. [Google Scholar] [CrossRef]
- Fiscella, K.; Meldrum, S.; Franks, P.; Shields, C.G.; Duberstein, P.; McDaniel, S.H.; Epstein, R.M. Patient trust: Is it related to patient-centered behavior of primary care physicians? Med. Care 2004, 42, 1049–1055. [Google Scholar] [CrossRef]
- Weng, H.-C. Does the physician’s emotional intelligence matter? Impacts of the physician’s emotional intelligence on the trust, patient-physician relationship, and satisfaction. Health Care Manag. Rev. 2008, 33, 280–288. [Google Scholar] [CrossRef]
- Holwerda, N.; Sanderman, R.; Pool, G.; Hinnen, C.; Langendijk, J.A.; Bemelman, W.A.; Hagedoorn, M.; Sprangers, M.A. Do patients trust their physician? The role of attachment style in the patient-physician relationship within one year after a cancer diagnosis. Acta. Oncologica. 2013, 52, 110–117. [Google Scholar] [CrossRef]
- Gordon, H.S.; Street Jr, R.L.; Sharf, B.F.; Kelly, P.A.; Souchek, J. Racial differences in trust and lung cancer patients’ perceptions of physician communication. J. Clin. Oncol. 2006, 24, 904–909. [Google Scholar] [CrossRef] [PubMed]
- Kao, A.C.; Green, D.C.; Zaslavsky, A.M.; Koplan, J.P.; Cleary, P.D. The relationship between method of physician payment and patient trust. JAMA 1998, 280, 1708–1714. [Google Scholar] [CrossRef]
- Scandura, T.A.; Williams, E.A. Research methodology in management: Current practices, trends, and implications for future research. Acad. Manag. J. 2000, 43, 1248–1264. [Google Scholar]
- Döhler, M. Comparing national patterns of medical specialization: A contribution to the theory of professions. Soc. Sci. Inf. 1993, 32, 185–231. [Google Scholar] [CrossRef]
- Völckner, F.; Sattler, H. Drivers of brand extension success. J. Mark. Res. 2006, 70, 18–34. [Google Scholar]
- Raaijmakers, J.G.; Shiffrin, R.M. Search of associative memory. Psychol. Rev. 1981, 88, 93. [Google Scholar] [CrossRef]
- Le, W.; Chang, P.-Y.; Chang, Y.-W.; Chen, J. Why do patients move from online health platforms to hospitals? The perspectives of fairness theory and brand extension theory. Inter. J. Env. Res. Pub. Heal. 2019, 16, 3755. [Google Scholar] [CrossRef]
- Smith, D.C.; Park, C.W. The effects of brand extensions on market share and advertising efficiency. J. Mark. Res. 1992, 29, 296–313. [Google Scholar] [CrossRef]
- Aaker, D. Brand extensions: The good, the bad, and the ugly. MIT Sloan Manag. Rev. 1990, 31, 47–56. [Google Scholar]
- Aubé, C.; Rousseau, V.; Tremblay, S. Team size and quality of group experience: The more the merrier? Group Dyn. 2011, 15, 357–375. [Google Scholar] [CrossRef]
- Brewer, M.B.; Kramer, R.M. Choice behavior in social dilemmas: Effects of social identity, group size, and decision framing. J. Pers. Soc. Psychol. 1986, 50, 543. [Google Scholar] [CrossRef]
- Brewer, M.B.; Gaertner, S.L. Toward reduction of prejudice: Intergroup contact and social categorization. In Blackwell Handbook of Social Psychology: Intergroup Processes; Brown, R., Gaertner, S.L., Eds.; Blackwell Publishers Ltd.: Hoboken, NJ, USA, 2003; pp. 451–472. [Google Scholar]
- Podsakoff, P.M.; Organ, D.W. Self-reports in organizational research: Problems and prospects. J. Manag. 1986, 12, 531–544. [Google Scholar] [CrossRef]
- Koufaris, M.; Hampton-Sosa, W. The development of initial trust in an online company by new customers. Inf. Manag. 2004, 41, 377–397. [Google Scholar] [CrossRef]
- Thom, D.H.; Ribisl, K.M.; Stewart, A.L.; Luke, D.A. Further validation and reliability testing of the trust in physician scale. Med. Care 1999, 37, 510–517. [Google Scholar] [CrossRef]
- Campbell, D.T.; Fiske, D.W. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychol. Bull. 1959, 56, 81. [Google Scholar] [CrossRef]
- Wetzels, M.; Odekerken-Schröder, G.; Van Oppen, C. Using PLS path modeling for assessing hierarchical construct models: Guidelines and empirical illustration. MIS Q. 2009, 33, 177–195. [Google Scholar] [CrossRef]
- Chin, W.W. Issues and opinion on structural equation modeling. MIS Q. 1998, 22, 1–14. [Google Scholar]
- Fornell, C.; Larcker, D.F. Structural equation models with unobservable variables and measurement error: Algebra and statistics. J. Mark. Res. 1981, 18, 382–388. [Google Scholar] [CrossRef]
- McKnight, D.H.; Choudhury, V.; Kacmar, C. Developing and validating trust measures for e-commerce: An integrative typology. Inf. Syst. Res. 2002, 13, 334–359. [Google Scholar] [CrossRef]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Komiak, S.Y.; Benbasat, I. The effects of personalization and familiarity on trust and adoption of recommendation agents. MIS Q. 2006, 30, 941–960. [Google Scholar] [CrossRef]
| Variables | Values | Frequency | Percentage |
|---|---|---|---|
| Gender | Male | 112 | 43.41% |
| Female | 146 | 56.59% | |
| Age (years) | 20–30 | 102 | 39.53% |
| 30–40 | 137 | 53.10% | |
| Others | 19 | 7.36% | |
| Education | Senior high school or less | 8 | 3.10% |
| Junior college | 26 | 10.08% | |
| Undergraduate | 211 | 81.78% | |
| Postgraduate | 13 | 5.04% | |
| Income(Chinese Yuan) | <1000 | 2 | 0.78% |
| 1000–3000 | 17 | 6.59% | |
| 3001–5000 | 54 | 20.93% | |
| 5001–8000 | 110 | 42.64% | |
| 8001–15000 | 61 | 23.64% | |
| >15000 | 14 | 5.43% |
| Constructs | Items | Literature | |
|---|---|---|---|
| Team Strength | TS1 | The team members are high in medical competence. | Self-developed |
| TS2 | The team members are high in reputation. | ||
| TS3 | The team leader is well-known and prestigious. | ||
| TS4 | In general, the medical team is high in strength. | ||
| Team Similarity | TSM1 | The focal physician is similar to the team members in terms of medical skills. | Self-developed |
| TSM2 | The focal physician is geographically near the team members. | ||
| TSM3 | The focal physician is similar to the team members in terms of title or position. | ||
| TSM4 | In general, the focal physician is similar to the team members. | ||
| Trust Propensity | TP1 | It is easy for me to trust a person/thing. | Adapted from [34] |
| TP2 | My tendency to trust a person/thing is high. | ||
| TP3 | I tend to trust a person/thing, even though I have little knowledge of it. | ||
| TP4 | Trusting someone or something is not difficult. | ||
| Physician Trust | PT1 | This physician is trustworthy. | Adapted from [34,35] |
| PT2 | This physician is qualified to me. | ||
| PT3 | I believe in the information that this physician provides me. | ||
| PT4 | I will follow the physician’s advice. | ||
| Team Size | TSI1 | The team size is large. | Self-developed |
| Internet Experience | IE1 | I have rich experience in using the Internet. | Self-developed |
| E-health Experience | EE1 | I have rich experience in using online health services. | Self-developed |
| Construct | CR | AVE | Cronbach’s Alpha | Item | Loading | T-Statistics |
|---|---|---|---|---|---|---|
| Team Strength | 0.883 | 0.654 | 0.823 | TS1 | 0.866 | 50.794 |
| TS2 | 0.803 | 28.984 | ||||
| TS3 | 0.739 | 16.655 | ||||
| TS4 | 0.823 | 30.429 | ||||
| Team Similarity | 0.867 | 0.621 | 0.803 | TSM1 | 0.722 | 13.258 |
| TSM2 | 0.758 | 18.247 | ||||
| TSM3 | 0.835 | 32.928 | ||||
| TSM4 | 0.832 | 28.691 | ||||
| Trust Propensity | 0.919 | 0.740 | 0.884 | TP1 | 0.883 | 40.376 |
| TP2 | 0.880 | 34.316 | ||||
| TP3 | 0.779 | 17.312 | ||||
| TP4 | 0.894 | 50.028 | ||||
| Physician Trust | 0.928 | 0.764 | 0.897 | PT1 | 0.838 | 32.209 |
| PT1 | 0.880 | 45.477 | ||||
| PT3 | 0.876 | 42.035 | ||||
| PT4 | 0.901 | 51.329 |
| Construct | Team Strength | Team Similarity | Trust Propensity | Physician Trust |
|---|---|---|---|---|
| Team Strength | 0.809 | |||
| Team Similarity | 0.364 | 0.788 | ||
| Trust Propensity | 0.271 | 0.192 | 0.860 | |
| Physician Trust | 0.782 | 0.451 | 0.272 | 0.874 |
| Condition | Mean | Std. Dev. | Sample Size |
|---|---|---|---|
| Worked a team | 5.57 | 0.982 | 258 |
| Did not work a team | 5.01 | 1.084 | 258 |
| Variables | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Age | −0.006 | −0.021 | −0.018 |
| (0.077) | (0.034) | (0.036) | |
| t = 0.078 | t = 0.615 | t = 0.496 | |
| Gender | 0.150 *** | 0.069 * | 0.074 ** |
| (0.058) | (0.037) | (0.037) | |
| t = 2.758 | t = 1.925 | t = 2.051 | |
| Marriage | 0.115 * | 0.068 * | 0.055 |
| (0.060) | (0.043) | (0.040) | |
| t = 1.859 | t = 1.737 | t = 1.335 | |
| Education | −0.023 | −0.043 | −0.043 |
| (0.061) | (0.037) | (0.036) | |
| t = 0.403 | t = 1.132 | t = 1.168 | |
| Income | −0.031 | −0.008 | −0.009 |
| (0.068) | (0.037) | (0.036) | |
| t = 0.496 | t = 0.225 | t = 0.248 | |
| Internet Experience | 0.220 *** | 0.044 | 0.051 |
| (0.086) | (0.050) | (0.050) | |
| t = 2.733 | t = 0.869 | t = 1.041 | |
| E-health Experience | −0.001 | −0.019 | −0.019 |
| (0.072) | (0.037) | (0.036) | |
| t = 0.017 | t = 0.524 | t = 0.502 | |
| Trust Propensity | 0.235*** | 0.042 | −0.019 |
| (0.068) | (0.056) | (0.051) | |
| t = 3.327 | t = 0.742 | t = 0.731 | |
| Team Strength | 0.686 *** | 1.085 *** | |
| (0.052) | (0.166) | ||
| t = 13.365 | t = 6.182 | ||
| Team Similarity | 0.178 *** | 0.173 ** | |
| (0.060) | (0.064) | ||
| t = 3.050 | 2.523 | ||
| Team Size | 0.749 ** | ||
| (0.290) | |||
| t = 2.428 | |||
| Team Size *Team Strength | −0.967 *** | ||
| (0.350) | |||
| t = 2.590 | |||
| Observations | 258 | 258 | 258 |
| 0.167 | 0.657 | 0.671 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, J.; Bao, X.; Liu, X.; Ma, L. The Impact of Joining a Team on the Initial Trust in Online Physicians. Healthcare 2020, 8, 33. https://doi.org/10.3390/healthcare8010033
Li J, Bao X, Liu X, Ma L. The Impact of Joining a Team on the Initial Trust in Online Physicians. Healthcare. 2020; 8(1):33. https://doi.org/10.3390/healthcare8010033
Chicago/Turabian StyleLi, Jia, Xinyu Bao, Xuan Liu, and Ling Ma. 2020. "The Impact of Joining a Team on the Initial Trust in Online Physicians" Healthcare 8, no. 1: 33. https://doi.org/10.3390/healthcare8010033
APA StyleLi, J., Bao, X., Liu, X., & Ma, L. (2020). The Impact of Joining a Team on the Initial Trust in Online Physicians. Healthcare, 8(1), 33. https://doi.org/10.3390/healthcare8010033





