The Impact of Nurse Practitioners on Hospitalizations and Discharges from Long-term Nursing Facilities: A Systematic Review
Abstract
:1. Introduction
1.1. Background
1.2. Significance
2. Materials and Methods
2.1. Design
2.2. Inclusion Criteria
2.3. Exclusion Criteria
3. Results
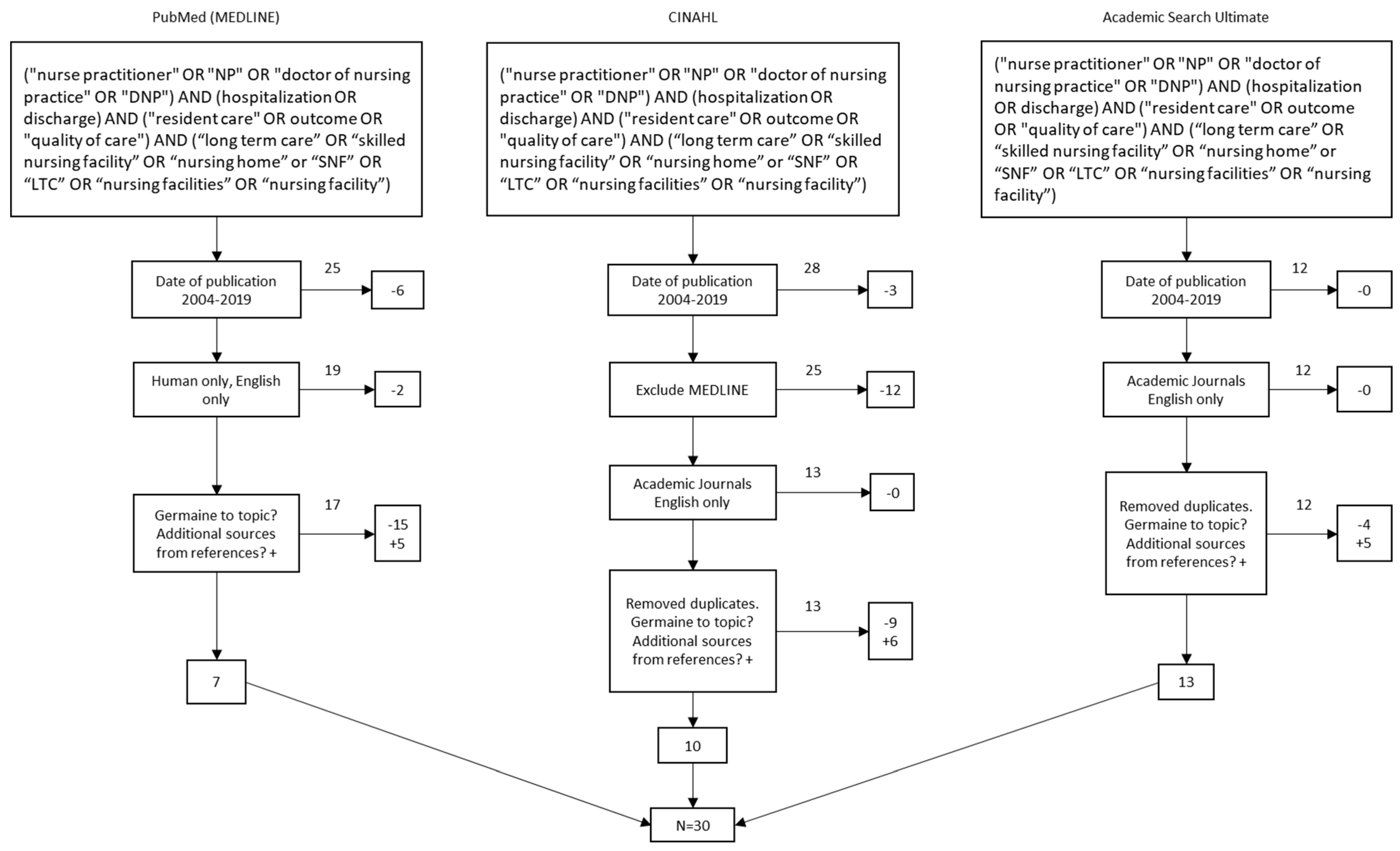
3.1. Study Selection
3.2. Assessment Tools
4. Results
4.1. Facilitators
4.2. Barriers
5. Discussion
6. Limitations
Future Research
Author Contributions
Funding
Conflicts of Interest
References
- Bakerjian, D. Care of Nursing Home Residents by Advance Practice Nurses. Res. Gerontol. Nurs. 2008, 1, 177–185. [Google Scholar] [PubMed]
- Ness, J.; Ahmed, A.; Aronow, W. Demographics and Payment Characteristics of Nursing Home Residents in the United States: A 23-Year Trend Introduction article. J. Gerontol. Med Sci. 2009, 59, 1213–1217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, L.; Laditka, S. Care Transitions by Older Adults from Nursing Homes to Hospitals: Implications for Long-Term Care Practice, Geriatrics Education, and Research. J. Am. Med Dir. Assoc. 2010, 11, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Mor, V.; Intrator, A.; Feng, Z.; Grabowski, D. The Revolving Door of Rehospitalization from Skilled Nursing Facilities. Health Aff. 2010, 29, 57–64. [Google Scholar] [CrossRef] [Green Version]
- Naylor, M.; Kurtzman, E.; Pauly, M. Transitions of Elders between Long-Term Care and Hospitals. Policy Politics Nurs. Pract. 2009, 10, 187–194. [Google Scholar] [CrossRef]
- Kruse, C.S. Writing a Systematic Review for Publication in a Health-Related Degree Program. JMIR Res. Protoc. 2019, 8, e15490. [Google Scholar] [CrossRef]
- Bethea, A.; Samanta, D.; White, T.; Payne, N.; Hardway, J. Nurse Practitioners Role in Improving Service for Elderly Trauma Patients. J. Trauma Nurs. 2019, 26, 174–179. [Google Scholar] [CrossRef]
- Anderson, R.; Ferguson, R. A nurse practitioner-led medication reconciliation process to reduce hospital readmissions from a skilled nursing facility. J. Am. Assoc. Nurse Pract. 2019, 32, 160–167. [Google Scholar] [CrossRef]
- Rantz, M.J.; Popejoy, L.; Vogelsmeier, A.; Galambos, C.; Alexander, G.; Flesner, M.; Murray, C.; Crecelius, C. Ge, B. Impact of Advanced Practice Registered Nurses on Quality Measures: The Missouri Quality Initiative Experience. J. Am. Med Dir. Assoc. 2018, 19, 541–550. [Google Scholar] [CrossRef]
- Ersek, M.; Hickman, S.; Thomas, A.; Bernard, B.; Unroe, K. Stakeholder Perspectives on the OPTIMISTIC Project. Gerontologist 2018, 58, 1177–1187. [Google Scholar] [CrossRef] [Green Version]
- Cole, M.S. Case study Realizing the Value of Nurse Practitioners in Long Term Care. Nurs. Leadersh. 2017, 3, 39–44. [Google Scholar] [CrossRef]
- Ingber, M.J.; Zhanlian, F.; Khatutsky, G.; Wang, J.M.; Bercaw, L.E. Initiative to Reduce Avoidable Hospitalizations Among Nursing Facility Residents Shows Promising Results. Health Aff. 2017, 36, 441–450. [Google Scholar] [CrossRef] [Green Version]
- Rantz, M.; Popejoy, L.; Vogelsmeir, A.; Galambos, C.; Alexander, G.; Flesner, M.; Crecelius, C.; Ge, B.; Petroski, G. Successfully Reducing Hospitalizations of Nursing Home Residents: Results of the Missouri Quality Initiative. JAMDA 2017, 18, 960–966. [Google Scholar]
- Birtley, N.; Flenser, M.; Crecelius, C.; Murray, C. Call to action APRNs in US nursing homes to improve care and reduce costs. Nurs. Outlook 2017, 65, 689–696. [Google Scholar]
- Hullick, C.; Conway, J.; Higgins, I.; Hewitt, J.; Dilworth, S.; Holliday, E.; Attia, J. Emergency department transfers and hospital admissions from residential aged care facilities a controlled pre-post design study. Bmc Geriatr. 2016, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Miller, S.C.; Lima, J.C.; Intrator, O.; Martin, E.; Bull, J.; Hanson, L.C. Palliative Care Consultations in Nursing Homes and Reductions in Acute Care Use and Potentially Burdensome End-of-Life Transitions. JAGS 2016, 64, 2280–2287. [Google Scholar] [CrossRef]
- Ouslander, J.; Naharci, I.; Engstrom, G.; Shutes, J.; Wolf, D.; Alpert, G.; Rojido, C.; Tappen, R.; Newman, D. Root cause analysis of Transfers of SNF patients to Acute Hospitals. JAMBDA 2016, 17, 256–262. [Google Scholar]
- Ouslander, J.; Naharci, I.; Engstrom, G.; Shutes, J.; Wolf, D.; Alpert, G.; Rojido, C.; Tappen, R.; Newman, D. Hospital Transfers of Skilled Nursing Facility (SNF) Patients Within 48 Hours and 30 Days After SNF Admission. JAMBDA 2016, 17, 839–845. [Google Scholar] [CrossRef] [Green Version]
- Meunier, M.; Brant, J.; Audet, S.; Dickerson, D.; Gransbery, K.; Clemins, E. Life after PACE (Program of All-Inclusive Care for the Elderly): A retrospective/prospective, qualitative analysis of the impact of closing a nurse practitioner centered PACE site. J. Am. Assoc. Nurse Pract. 2016, 28, 596–603. [Google Scholar] [CrossRef]
- Mullaney, S.; Devereaux Melillo, K.; Lee, A.J.; MacArthur, R. The association of nurse practitioners’ mortality risk assessments and advance care planning discussions on nursing home. J. Am. Assoc. Nurse Pract. 2016, 28, 304–310. [Google Scholar]
- Ordonez, M.; Hain, D. Healthy Transitions from Hospital to Skilled Nursing Facility Post-CABG. J. Nurs. Pract. Appl. Rev. Res. 2014, 4, 123–134. [Google Scholar]
- Segal, M.; Rollins, E.; Hodges, K.; Roozeboom, M. Medicare Medicaid Eligible Beneficiaries and Potentially Avoidable Hospitalizations. MMRR 2014, 4, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Ploeg, J.; Kassalainen, S.; McAiney, C.; Martin-Misener, R.; Donald, F.; Wickson-Griffiths, A.; Carter, N.; Sangster-Gormley, E.; Schindel Martin, L.; Brazil, K.; et al. Resident and family perceptions of the nurse practitioner role in long term care settings: A qualitative descriptive study. BMC Nurs. 2013, 12, 24. [Google Scholar] [CrossRef] [Green Version]
- Krichbaum, K. GAPN Postacute Care Coordination Improves Hip Fracture Outcomes. West. J. Nurs. Res. 2007, 29, 523–544. [Google Scholar] [CrossRef]
- Reidt, S.; Holtan, H.; Larson, T.; Thompson, B.; Kerzner, L.; Salvatore, T.; Adam, T. Interprofessional Collaboration to Improve Discharge from ED Visits. JAGS 2016, 64, 1895–1899. [Google Scholar] [CrossRef] [Green Version]
- Rosenfeld, P.; Kobayashi, M.; Barber, P.; Mezey, M. Utilization of Nurse Practitioners in Long-Term Care: Findings and Implications of a National Survey. JAMDA 2004, 5, 9–15. [Google Scholar] [CrossRef]
- Kane, R.L.; Flood, S.; Bershadsky, B.; Keckhafer, G. Effect of an Innovative Medicare Managed Care Program on the Quality of Care for Nursing Home Residents. Gerontologist 2004, 44, 95–103. [Google Scholar] [CrossRef] [Green Version]
- Rykina, K.L.; Yuan, Y.; Teng, S.; Burke, R. Assessing First Visits by Physicians to Medicare Patients Discharged to Skilled Nursing Facilities. Health Aff. 2019, 4, 528–536. [Google Scholar] [CrossRef]
- Arendts, G.; Deans, P.; O’Brien, K.; Etherton-Beer, C.; Howard, K.; Lewin, G.; Sim, M. A Clinical Trial of NP Care in Residential Aged Facilities. Arch. Gerontol. Geriatr. 2018, 77, 129–132. [Google Scholar] [CrossRef]
- Kuo, Y.-F.; Loresto, F.; Rounds, L.; Goodwin, J. States with the Least Restrictive Regulations Experienced the Largest Increase in Patients Seen by Nurse Practitioners. Health Aff. 2013, 32, 1236–1243. [Google Scholar] [CrossRef] [Green Version]
- Oliver, G.; Pennington, L.; Revelle, S.; Rantz, M. Impact of NPs on health outcomes of Medicare and Medicaid patients. Nurse Outlook 2014, 62, 440–447. [Google Scholar] [CrossRef]
- Dwyer, T.; Crasswell, A.; Rossi, D.; Holzberger, D. Evaluation of an aged care NP service quality of care within a resident aged care facility. Bmc Health Serv. Res. 2017, 17, 1–11. [Google Scholar] [CrossRef]
- Kaasalainen, S.; Papaioannou, A.; Burgess, J.; Van Der Horst, M.L. Exploring the NP Role in Managing Fractures in Long Term Care. Clin. Nurs. Res. 2016, 24, 567–588. [Google Scholar] [CrossRef] [Green Version]
- Yang, M.; Chang, C.-H.; Carmichael, D.; Oh, E.; Bynum, J. Who Is Providing the Predominant Care for Older Adults with Dementia? JAMDA 2016, 17, 802–806. [Google Scholar] [CrossRef] [Green Version]
- Popejoy, L.; Vogelsmeir, A.; Alexander, G.; Gallambos, C.; Crecelius, C.; Ge, B.; Flesner, M.; Canada, K.; Rantz, M. Analyzing Hospital Transfers Using INTERACT Acute Care Transfer Tools: Lessons from MOQI. JAGS 2019, 67, 1953–1959. [Google Scholar] [CrossRef]
- Poghosyan, L.; Shang, J.; Liu, J.; Poghosyan, H.; Liu, N.; Berkowitz, B. Nurse practitioners as primary care providers: Creating favorable practice environments in New York State and Massachusetts. Health Care Manag. Rev. 2015, 40, 46–55. [Google Scholar] [CrossRef] [Green Version]
| Author Last Name | Aim | Sample/Settings | Method | Assessment Tool | Key Findings |
|---|---|---|---|---|---|
| Popejoy | Exploring the differences in potentially avoidable/unavoidable hospital transfers in a retrospective analysis of INTERACT (Interventions to Reduce Acute Care Transfers, ACTs (Acute Transfer Tools) completed by advanced practice registered nurses (APRNs) working in the Missouri Quality Improvement Initiative (MOQI) | 16 nursing homes, ranging from 120 to 321 beds | Cross-sectional descriptive study | INTERACT and ACT | Over one-half of the transfers (54%) were identified as avoidable transfers. Clinical factors related to avoidable transfers included falls, fever, urinary symptoms/incontinence. The transfers had a condition which could have been managed in a nursing home (58%), transfers could have been avoided with better communication (39%), new signs/symptoms detected earlier (31%), and advance directives in place earlier (11%) |
| Ouslander, Naharci | To determine the types of SNF to hospital transfers that occur within 48 h and 30 days of SNF admission based on root cause analyses (RCAs) and to identify potential areas for improving transitional care between hospitals and SNFs | 88 skilled nursing facilities | Trained staff from SNFs enrolled in a randomized, controlled clinical trial of the INTERACT (Interventions to Reduce Acute Care Transfers) quality improvement program performed retrospective RCAs on hospital transfers during a 12-month implementation period | INTERACT (Interventions to Reduce Acute Care Transfers) Quality Improvement (QI) tool, retrospective RCA (root cause analyses) on hospital transfers | First, more intensive monitoring of these patients during the first 48 h to 7 days after SNF admission may help identify changes in condition early enough to intervene before hospital transfer is necessary. Teams of physicians and nurse practitioners have been shown to be effective in reducing hospitalizations and potentially avoidable hospitalizations in particular |
| Bethea | To compare the outcomes in elderly patients whose care was coordinated by trauma nurse practitioner (TNP) versus non trauma NP (NTNP) | 1363 patients were analyzed for this study in a Level 1 trauma center between December 2014 and June 2017 | Retrospective cohort study | Patient demographics, comorbidities, admission injuries, Injury Severity Score (ISS), hospital length of stay and unplanned ICU admission. Study outcomes also based on discharge location including home, skilled nursing, in-hospital mortality, 30-day readmission and hospital charges | Shorter length of stay for patients under care of TNPs which resulted in decreased hospital charges of $13,000 per admission. Patient under care of TNPs demonstrated higher percentage of home discharges as compared to discharge to skilled nursing facilities |
| Rantz, Popejoy | To determine if the Missouri Quality Initiative (MOQI) for long-stay nursing home residents reduced the frequency of preventable hospitalizations, improved resident health outcomes, improved the process of transition of care between hospitals and nursing facilities and reduced healthcare costs | 16 nursing homes in metro, urban and rural communities | Prospective, single group intervention design | Interventions to Reduce Acute Care Transfers (INTERACT), INTERACT RCA (Root Cause Analysis), Early illness identification (stop and watch), SBAR (Situation, background, assessment, recommendation) | The MOQI (Missouri Quality Initiative) achieved 30% reduction in all-cause hospitalizations with full-time APRNs working in each facility and supported by the MOQI team to assist with quality improvement activities, consistent use of INTERACT, increased end-of-life decision making, and improved use of HIT (health information technology) for secure communication. There was a decline in the nonavoidable transfers from 64% to 47% and an increase in the percentage of avoidable from 47% to 54% |
| Rantz, Birtley | To study the implementation of an inter-professional model in nursing facilities with advanced practice registered nurses (APRNs) with aim to reduce preventable hospitalizations among nursing home residents | 16 nursing homes. SNF, LTC | Retrospective, quasi-experimental | Physician and APRN reimbursement by CPT codes. Allowable APRN visits and orders for SNF versus NF | The model results demonstrated significant reduction in hospitalizations (40% all cause, 58% potentially avoidable), emergency room visits (54% all cause, 65% potentially avoidable), Medicare expenditures for hospitalizations (34% all cause, 45% potentially avoidable), and Medicare expenditures for emergency room visits (50% all cause, 60% potentially avoidable) |
| Ersek | To reduce the burden of costly hospitalizations of nursing home residents by using the Transforming Institutional Care Project (OPTIMISTIC) | 19 skilled nursing facilities. Participants included 23 nursing home staff and leaders, 4 primary care providers, 10 family members, and 26 OPTIMISTIC clinical staff | One time, semi structured qualitative interviews | Advance care planning (ACP), Transforming Institutional Care (OPTIMISTIC), INTERACT | This project provided NPs time to facilitate high quality ACP discussions, conduct comprehensive resident assessment, timely identification and management of acute changes, staff education, thorough discussions with residents and families regarding care plan goals and analysis of root causes for potentially preventable hospitalizations |
| Yang | To determine which clinical specialties are most significant to care of individuals with dementia in the community and long-term care (LTC) settings | Long term care setting and Community setting. Fee-for-service Medicare beneficiaries with dementia aged 65 years or older | Cross-sectional analysis | Patient characteristics were examined by specialty of the PPC (predominant provider of care) and by community versus LTC settings using t test or chi-squared tests, as appropriate. The maps were used to show geographic variation at the state level for NPs as the PPC of care | More than 90% of beneficiaries had primary care providers as their PPC in LTC compared with 77.3% of beneficiaries in the community. Among the primary care providers, NPs as PPCs had the greatest difference between community (6.9%) and LTC (19.2%). NPs play as PPCs in LTC and how their role differs across states. In LTC, 40 states had NPs serving as PPCs for 12% to 40% of dementia beneficiaries living in LTC facilities |
| Meunier | The research determines if the use of comprehensive models, such as Program of All-Inclusive Care for the Elderly (PACE), lead to improved functional outcomes for participants and cost savings through decreased utilization | Long term care in community setting. 34 former participants in PACE were monitored every 6 months for 2 years and data was collected | Retrospective, quasi-experimental | Physical Self-Maintenance Scale, Instrumental Activities of Daily Living Scale, 6-point Likert response scale, Saint Louis University Mental Status Exam (SLUMS) | Both number of ED visits and hospitalizations were found to be significantly higher after PACE closure. For every hour of home health per month, the number of ED/hospital visits decreased in a 6-month period by 5.4%. Over the 2-year study period, functional scores ADLs and IADLs significantly declined. The majority of participants (67%) reported a higher level of satisfaction with PACE services as compared to usual care provided post-PACE |
| Oliver | To examine the relationship between the level of advanced practice registered nurse (APRN) practice (full, reduced, or restricted) allowed and results of analyses of Medicare or Medicare-Medicaid beneficiaries of possibly preventable hospitalizations, readmission rates after inpatient rehabilitation, and nursing home resident hospitalizations | Hospitals, Inpatient rehab, SNF and LTC | Retrospective | Two-sampled t-tests, One-way analysis of variance, Tukey test | States with the highest level of scope of practice for NPs showed reduced hospitalizations and enhanced health outcomes. The study indicates that any type of barriers which restrict NPs to practice within their full scope is inversely related to the positive effect on hospitalizations and state health outcomes |
| Segal | To examine potentially preventable hospitalizations rates by setting, state, medical condition, and cost | Hospital, Inpatient rehab, SNF, LTC, home health and community | Retrospective | Potentially Avoidable Hospitalization Algorithm, ICD-9 diagnosis | The national rate among MMEs for potentially avoidable hospitalizations was 133 per 1000 person-years, but there was considerable variation across health care settings. For those MMEs receiving care in a skilled nursing facility, the potentially avoidable hospitalizations rate was 690 per 1000 person-years. Five conditions were responsible for nearly 80 percent of potentially avoidable hospitalizations occurring among the study population: congestive heart failure (21%), COPD/asthma (20%), urinary tract infections (15%), pneumonia (13%), and dehydration (11%) |
| Anderson and Ferguson | Reduce hospital readmissions by an NP completing a systematic medication reconciliation process for all new admissions | 90-bed skilled nursing facility | Pre- and postimplementation design | Evidence-based workflow process, chi-square analysis | 19.2% hospital readmission rate pre implementation and 13.5% postimplementation, a 29.7% decrease in hospitalizations within a 30-day period |
| Ingber | Improve the overall health and health care of participating long-stay residents of nursing facilities, reducing potentially avoidable hospitalizations, improving quality of care, and decreasing health care spending | Long-stay residents—total of 143 nursing facilities | Mixed methods, quantitative and qualitative analysis, multivariate regression | Analysis of claims and assessments, site visits, interviews, and surveys | Multipronged NP interventions reduce potentially avoidable hospitalizations and related Medicare expenditures |
| Kane | Assess the quality of care using Evercare approach which employs NPs to provide additional primary care over and above that provided by physicians | Nursing home residents | Experimental | Data from MDS, Medicare, and United Healthcare, survival analysis, risk adjustment methods applied to the quality indicators | Hazard rates significantly lower for Evercare residents, residents had fewer preventable hospitalizations |
| Krichbum | Test effectiveness of nursing intervention model to improve health function, and return-home outcomes using a gerontological advanced practice nurse (GAPN) to provide interventions 6 months post-acute care, making biweekly visits and/or phone calls | 33 elders 65 years and older with a hip fracture | Randomized clinical trial | Mini Mental Status Exam (MMSE), Global (GH) self-ratings, Geriatric Depression Scale (GDS), Functional Status Index (FSI) and listing of living situation | Improved function in mobility, home chores, and personal care activities |
| Miller | Evaluate how receipt and timing of nursing home palliative care consultations by nurse practitioners with palliative care expertise are associated with end-of-life care transitions and acute care use | Nursing home residents who died from 2006 to 2010 living in 46 nursing homes in two states | Propensity score-matched retrospective cohort study | Multivariate logistic regression analysis | Lower rates of hospitalizations, improved end-of-life nursing home care |
| Ploeg | Report the perceptions of residents and family members about the role of the nurse practitioner in long term care settings | 35 residents and family members from four long-term care settings that employed a nurse practitioner | Qualitative descriptive approach, individual and focus groups interviews | Conventional content analysis was used to identify themes and subthemes | Perceptions of residents and family members of the nurse practitioner role in long-term care setting consistent with person-centered and relationship-centered care, enhanced quality of care, positive care experience |
| Poghosyan | Determine the impact of state and organizations on nurse practitioner practice environment | 291 nurse practitioners in MA and 278 nurse practitioners in NY | Cross-sectional survey design; online surveys | Nurse Practitioner Primary Care Organizational Climate Questionnaire | NPs have positive perceptions of their relationship with physicians, NP’s perceptions of the relationships they have with administration is deficient, state and organizational policies should be taken into consideration to ensure least restrictive practice |
| Rantz | Review impact of advance practice registered nurses (APRNs) on the quality measure scores of 16 nursing homes participating the Missouri Quality Initiative (MOQI) intervention | 16 nursing homes | Two-group comparisons | Data was collected for 36 months and analysis of results conducted to create a composite quality measure score for each facility, Interventions to Reduce Acute Care Transfers (INTERACT) using the Stop and Watch and Situation, Background, Assessment, Recommendation (SBAR) | APRNs working full-time in nursing homes positively influenced quality of care, reduced unnecessary hospitalizations and emergency room transfers, improved the process of transitioning between inpatient hospitals and nursing facilities, and reduced overall healthcare spending without restricting access to care |
| Rosenfeld | Determine the national practice patterns of nurse practitioners providing care in long-term care facilities | All physicians who are members of the American Medical Directors Association (AMDA) | Mailed survey | The survey mailed out included six domains: (1) the number of LTC facilities that have NPs involved in providing care; (2) the number of NPs engaged in care at these facilities; (3) the types of employment/financial arrangements between NPs and LTC facilities; (4) the types of services provided by the NPs; (5) the effectiveness of the NPs as perceived by the medical director; and (6) the perceived future demand for NPs in LTC | NPs involved in LTC are more likely to be involved in facilities with 100+ beds, performed a wide range of services, are effective at maintaining physician, resident, and family satisfaction, were highly effective with regard to emergency room transfers, increasing the quality of care, survey preparedness, and hospital admissions. Respondents to the survey were overwhelmingly positive about working with NPs |
| Ryskina | Describe current practice behaviors to identify areas where interventions could improve post-acute care outcomes | Fee-for-service Medicare beneficiaries, 65+ years old, discharged from an acute care hospital to a SNF in the period of January 2012–October 2014 | Retrospective | Aggregate data from Medicare claims January 2012–October 2014, supplemental information from MDS and Provider of Services | Timely access to physicians or NPs after hospital discharges to a SNF depends on local practice patterns, not clinical needs |
| Kaasalainen | To evaluate the level of involvement of nurse practitioners (NPs) in activities related to preventing and managing fractures in long-term care (LTC) | Long term care (LTC) | A cross-sectional survey, qualitative interviews | The first section focused on demographic information, the second section gathered information on practice patterns of NPs related to fracture-risk assessment, post-fracture management and use of evidence-based guidelines, the third section surveyed on the processes NPs would follow to respond to related care decisions, and last section focused on identification of the barriers and facilitators faced by NPs to prevent and manage fractures | The finding suggest that the NP were involved in caring for residents’ post fractures and in risk factors assessments. The role of NP in managing fractures can be optimized by addressing barriers such as inadequate staffing at the facility and lack of timely access to diagnostic services |
| Ouslander, Naharci | To determine if conducting root cause analyses (RCA) on transition of residents from skilled nursing facility to hospitals can help prevent preventable emergency department (ED) visits and hospitalizations | Sixty-four of 88 SNFs | Retrospective, quasi-experimental | INTERACT (Interventions to Reduce Acute Care Transfers), Quality Improvement (QI) tool | The studies indicate that using RCAs provides important insights to factors contributing to the transfers, propose several areas of attention for process improvements and related education which may help reduce preventable hospitalizations |
| Kuo | The use of nurse practitioners (NPs) is one way to address the shortage of physician primary care providers | Medicare beneficiaries aged 65 or older with Parts A and B coverage and not in a health maintenance organization (HMO) for the entire twelve months of each year during 1998–2010 | We identified individual providers by their Unique Provider Identification Number for 1998–2007 and National Provider Identifier for 2007–10 | Hierarchical generalized linear mixed models | The overall number of NPs reimbursed for evaluation and management services in the 5 percent Medicare claims data rose from 3114 in 1998 to 37,638 in 2010 |
| Mullaney | To understand the impact of mortality risk assessments (MRAs) and advance care planning (ACP) discussions completed by nurse practitioners (NP) on clinical outcomes for newly registered Medicare Advantage nursing home residents | The final sample of 87 patients was 72% female with a mean age of 81 years, LTC | Prospective, nonexperimental approach | Mortality Risk Assessment (MRA) & Advance Care Planning (ACP) | The study demonstrated positive clinical outcomes post ACP discussions. The outcomes include increase in number of patients with a comfort goal of care, decline in full-code status patients, reduced hospitalizations and improved quality in end-of-life care |
| Cole | NPs collaborative practice with physician and nursing colleagues to reduce hospitalization | 190-bed residential care facility in New Brunswick, LTC | Retrospective | Daily clinical monitoring | As shown in this case, the presence of an NP clearly impacted a reduction in emergency room visits and hospitalizations, events that often accelerate further physical, mental, and functional decline particularly among the frail elderly |
| Hullick | To examines the impact of the aged care emergency services (ACE) on residential aged care facilities (RACF) residents’ transfers to hospitals | Four RACFs, LTC | Prospective, retrospective | Generalized estimating equations | This study has demonstrated that a complex multi-strategy intervention led by nursing staff can successfully reduce hospital admissions for older people living in Residential Aged Care Facilities |
| Ordonez | To examine the outcome of a gerontological nurse practitioner (GNP) care coordination model on healthy transition and 30-day rehospitalizations among older adults. In this study, the patients are discharged from a hospital to a SNF for rehabilitation post coronary artery bypass graft (CABG) surgery | 10 older adults with age > 65 years status post CABG. Skilled nursing facility | Retrospective, quasi-experimental | Scale 1-4 including control of signs and symptoms, functional status, depression, sense of integrity | Findings indicate five to eight percent more effectiveness in outcomes with GNP care coordination model than the standard of care. The project demonstrates the effectiveness of the GNP care coordination model in decreasing the risk of 30-day rehospitalization and facilitating the development of realistic and achievable goals |
| Dwyer | Reducing avoidable hospitalizations of aged care facility (ACF) residents can improve the resident experience and their health outcomes | Aged care facility (ACF), LTC | Retrospective | Donabedian model | The studies indicate that the NPs with their advanced clinical skills and prescribing rights, were able to deliver a range of timely health services within the ACF in the absence of a PCP. This resulted in reduced hospitalization and managing of care of residents at the facility |
| Reidt | To study an interprofessional collaborative practice model aimed to improve discharge management from the transitional care unit of the skilled nursing facility (SNF) to home. The model includes a geriatrician, nurse practitioner and a pharmacist | SNF, LTC | Prospective, Retrospective | Comparison of intervention and control groups | This study suggests that collaboration among a geriatrician, nurse practitioner, and pharmacist may be an effective means of decreasing hospitalizations and ED visits within 30 days after SNF discharge |
| Arendts | To enhance quality of life and reducing hospitalizations for people living in residential aged care facilities (RACF) | Six facilities (352 beds each) were included, RACF, LTC | Prospective, Retrospective, quasi-experimental. A cluster controlled clinical trial of nurse practitioner care in RACF. Six facilities were included: three randomly allocated to intervention where nurse practitioners working with general practitioners and using a best practice guide were responsible for care, and three control | Modified Barthel Index (MBI), Psychogeriatric Assessment Scale (PAS) assessments | Nurse practitioner care coordination resulted in no statistically significant change in rates of ED transfer or health care utilization, but better maintained resident quality of life |
| Facilitators | Occurrences | Sum | % |
|---|---|---|---|
| Decreased hospitalizations | 7,8,9,10,11*,12*,13,14*,15*,16,17*,18,19,20*,21,22,23*,24,25,26,27* | 37 | 27.21% |
| Improved health outcomes | 7,9*,12,14,20*,21*,23*,24*,26,28*,29*,30,31 | 27 | 19.85% |
| Improved quality of care | 8*,13,14*,18,19,20*,23*,24,26,27,28*,31,33 | 26 | 19.12% |
| Increased access to healthcare | 18,20,23,24*,25,30,31*,33,34* | 14 | 10.29% |
| Unrestrictive or least restrictive scope of practice for NPs | 10,14,16,17,31,32,33,34,35,36* | 10 | 7.35% |
| Reduced healthcare costs | 7,8,9*,12,14,23,30 | 9 | 6.62% |
| Multidisciplinary approach | 21*,25,29,32 | 5 | 3.68% |
| Improved end of life care | 16* | 3 | 2.21% |
| Patient and family education | 13,20* | 3 | 2.21% |
| Improved patient and family satisfaction | 19,32 | 2 | 1.47% |
| 136 | |||
| Barriers | Occurrences | Sum | % |
| Restrictive scope of practice for NPs | 9,14,16,20,23,24,31*,32*,34,35,36 | 13 | 28.89% |
| Poor quality of care | 13*,19,20,22,27,28* | 11 | 24.44% |
| Lack of access to healthcare | 17,20,22*,27,29 | 7 | 15.56% |
| Inadequate staffing | 8,10,17,23,28,33 | 6 | 13.33% |
| Decreased patient satisfaction | 17,23,29 | 3 | 6.67% |
| Poor decision making | 18* | 2 | 4.44% |
| Increased hospitalizations | 19 | 1 | 2.22% |
| Increased healthcare costs | 19 | 1 | 2.22% |
| Poor communication | 36 | 1 | 2.22% |
| 45 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mileski, M.; Pannu, U.; Payne, B.; Sterling, E.; McClay, R. The Impact of Nurse Practitioners on Hospitalizations and Discharges from Long-term Nursing Facilities: A Systematic Review. Healthcare 2020, 8, 114. https://doi.org/10.3390/healthcare8020114
Mileski M, Pannu U, Payne B, Sterling E, McClay R. The Impact of Nurse Practitioners on Hospitalizations and Discharges from Long-term Nursing Facilities: A Systematic Review. Healthcare. 2020; 8(2):114. https://doi.org/10.3390/healthcare8020114
Chicago/Turabian StyleMileski, Michael, Upwinder Pannu, Bobbi Payne, Erica Sterling, and Rebecca McClay. 2020. "The Impact of Nurse Practitioners on Hospitalizations and Discharges from Long-term Nursing Facilities: A Systematic Review" Healthcare 8, no. 2: 114. https://doi.org/10.3390/healthcare8020114
APA StyleMileski, M., Pannu, U., Payne, B., Sterling, E., & McClay, R. (2020). The Impact of Nurse Practitioners on Hospitalizations and Discharges from Long-term Nursing Facilities: A Systematic Review. Healthcare, 8(2), 114. https://doi.org/10.3390/healthcare8020114





