Abstract
The objective of this study was to investigate whether ankle balance taping (ABT) applied after muscle fatigue-inducing exercise can cause immediate improvements in dynamic and static balance. A total of 31 adults (16 males and 15 females) met the inclusion criteria. The experiment was designed using a single-blinded, randomized controlled trial. Changes in static and dynamic balance were measured before and after inducing muscle fatigue in the ankles and after ABT or ankle placebo taping (APT). After ankle muscle fatigue-inducing exercise, both the ABT and APT groups showed significant increases in surface area ellipses in the static state with eyes open (p < 0.05), and significant increases in surface area ellipses in the static and dynamic states with eyes closed (both p < 0.05). After taping of the fatigued ankle, surface area ellipses decreased significantly when eyes were open and closed in the static and dynamic states, but only in the ABT group (p < 0.05). Static balance was significantly different between groups (eyes open, 36.2 ± 86; eyes closed, 22.9 ± 46.7). Dynamic balance was significantly different between groups (eyes open, 68.6 ± 152.1; eyes closed, 235.8 ± 317.6). ABT may help prevent ankle injuries in individuals who experience muscle fatigue around the ankles after sports and daily activities.
1. Introduction
Muscle fatigue is caused by repeated muscle contractions during high-intensity exercise or activities over a prolonged time, and it reduces the ability of the muscles to generate force due to temporary reduction in the ability to contract [1,2]. Muscle fatigue can impair the performance of the joints and the body during voluntary movement [3], and has a negative effect on the ability to control balance due to low reactivity to stimulation and impairment of joint proprioception and kinesthesis [4,5].
The ability to maintain balance under static or dynamic situations is a prerequisite for performing various activities of daily living [6,7]. Ankle muscles play a central role in maintaining balance in one-leg and two-leg standing positions [8,9], but when muscle fatigue occurs, the joints become unstable, causing increased postural sway and decreased ability to maintain balance [10]. Therefore, muscle fatigue near the ankle joint may increase the risk of ankle sprain injury [11].
Kinesiology taping is often used in clinical practice for treating musculoskeletal and nervous disorders, and its use in sports for preventing and treating sports-related injuries is also increasing. Previous studies have reported that kinesiology taping improves kinesthesis and proprioception [12,13,14], pain control and muscle strength [15,16], and joint range of motion (ROM) [13,17]. A recent study reported that ankle balance taping (ABT) using kinesiology tape showed immediate improvements in the dynamic balance of young soccer players with ankle instability [18] and the static balance of healthy adults [19].
There are very few studies on the immediate effects of ABT with kinesiology tape on dynamic and static balance following ankle muscle fatigue. Therefore, the objective of this study was to investigate whether ABT with kinesiology tape applied after muscle fatigue-inducing exercise affects the dynamic and static balance abilities of individuals with no ankle pain or instability.
2. Material and Methods
2.1. Participants
To calculate the sample size needed, G-Power 3.1 (University of Dusseldorf, Dusseldorf, Germany) was used with the significance level (alpha level) set at 0.05, statistical power at 0.8, and effect size at 0.7 based on the anticipated differences in static balance between pretest and post-intervention [20]. The calculation indicated that 24 participants were needed. Thirty-one adult participants who did not have any ankle pain or instability provided their consent to participate in the study. This study was approved by the Institutional Review Board of Dong-eui University (DIRB-201602-HR-E-011).
The exclusion criteria for the study were as follows: (1) orthopedic or neurosurgical injury in the past 6 months (history of surgery without experiencing sprain or fracture in the ankles or lower extremity); (2) use of any medication in the past 3 months; (3) ankle edema; (4) abnormality of the nervous system, including the vestibular organ and cerebellum; and (5) past history of contact dermatitis.
2.2. Study Design
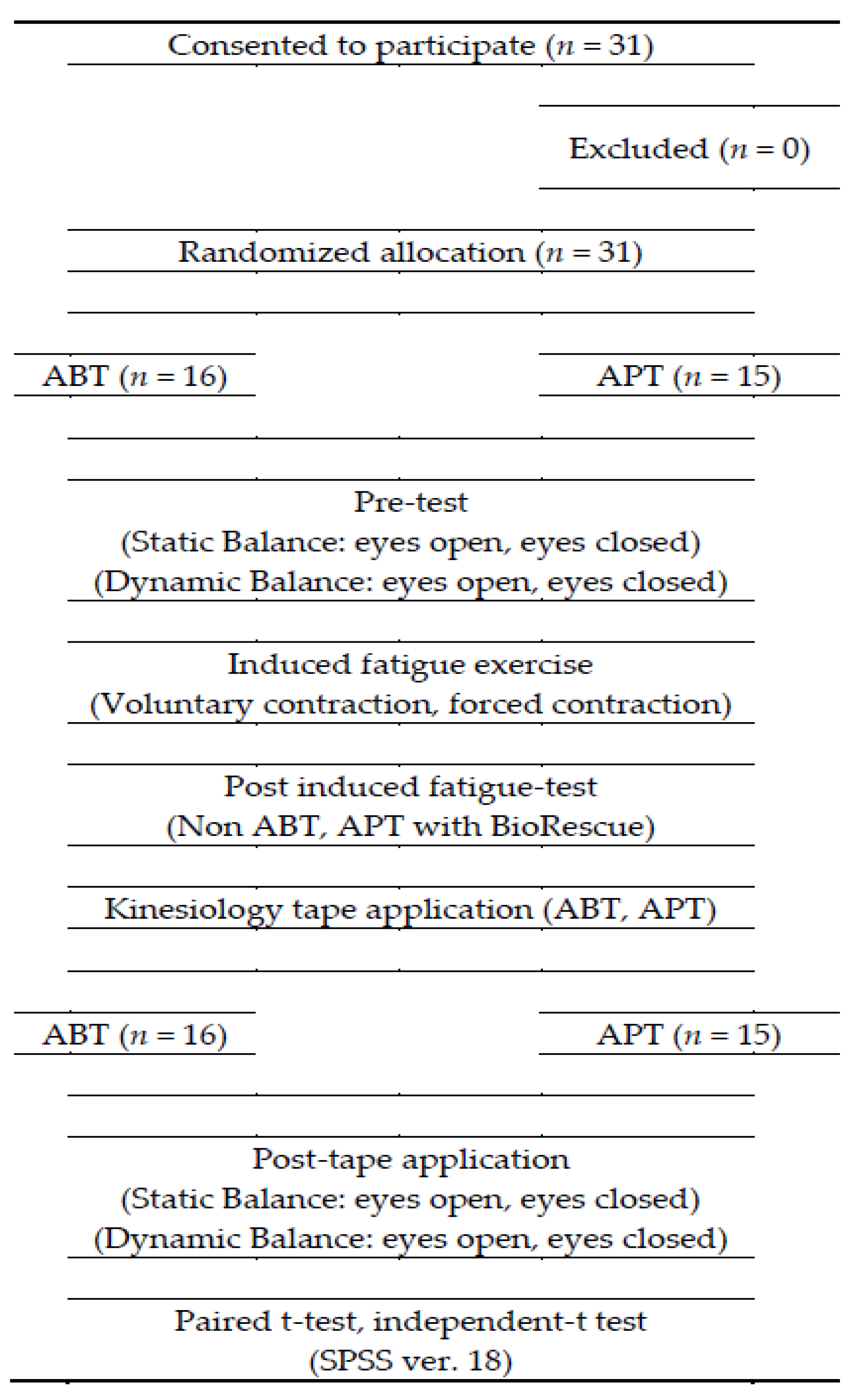
This study was designed as a single-blinded, randomized controlled trial. Participants were randomly assigned to either the control group (APT) or experimental group (ABT). All measurements were carried out by the same examiner, in a university laboratory, who was stationed behind a nontransparent screen and was blinded to group allocation. The order of measurement (eyes open, eyes closed, static, and dynamic) was randomized. The randomization process was carried out using a computer-generated table of random numbers. Taping was performed by a physical therapist with more than 10 years of experience. First, the static and dynamic balance of both groups were measured with eyes open and then with eyes closed, respectively. Immediately after the ankle muscle fatigue-inducing exercise, measurements of static and dynamic balance were measured again. ABT with kinesiology tape or APT was applied immediately and static and dynamic balance were measured for a third time. The flowchart of this study is shown in Figure 1.
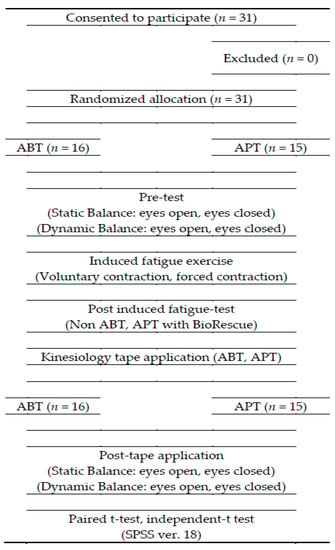
Figure 1.
Flow diagram for the study.
2.3. Measurement
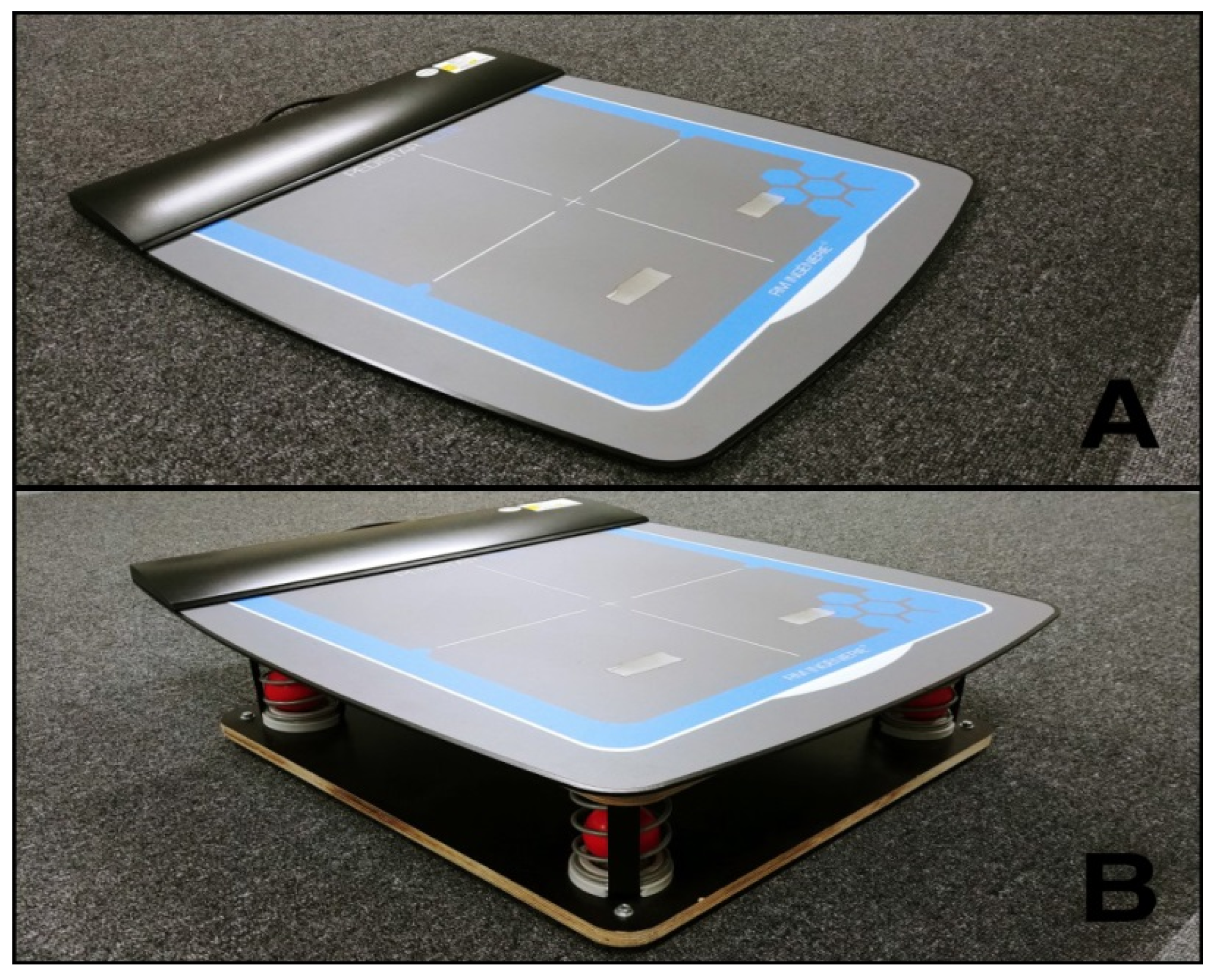
The study used BioRescue (RM Ingenierie, Rodez, France) for the measurement of changes in static and dynamic balance before and after inducing muscle fatigue in the ankles and after applying kinesiology tape. BioRescue (RM Ingenierie) is a device with 1600 sensors connected to a foot plate (610 × 580 × 10 mm) that measures the balance ability of the participant based on changes in the surface area ellipse of the center of pressure (mm2) (Figure 2) [21]. A previous study has demonstrated high test–retest reliability of this device (intraclass correlation coefficients = 0.83 − 0.95) [22].
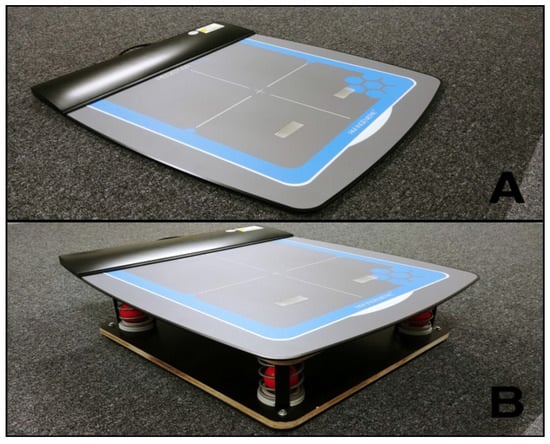
Figure 2.
BioRescue plate for static standing balance (A); BioRescue plate for dynamic standing balance (B).
2.4. Fatigue Protocol
The method suggested by Gefen et al. [11] which consists of voluntary contraction and forced contraction, was used to induce ankle muscle fatigue. For voluntary contraction, 40 repetitions of dorsiflexion and plantarflexion were performed with the participant seated in a chair without the feet touching the ground. For forced contraction, the participant performed 25 repetitions of lifting the heels as much as possible in plantarflexion and maintaining that position for 1 s before returning the heels to the ground in a standing position whilst placing their hands on the back of a chair support structure.
2.5. Intervention
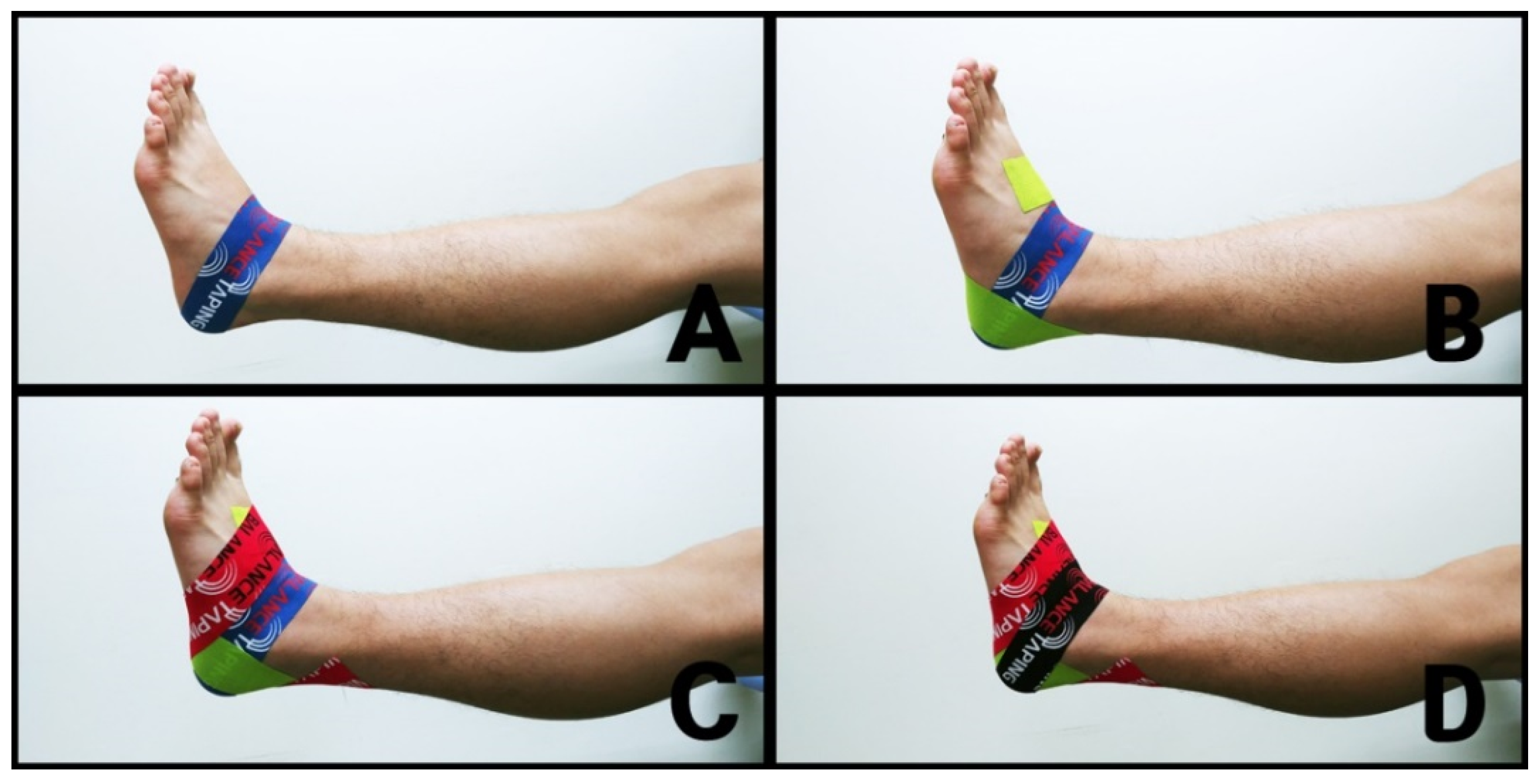
2.5.1. Ankle Balance Taping (ABT)
With the participants seated comfortably, the kinesiology tape (BB TAPE, WETAPE Inc., Paju, Korea) was stretched by approximately 30–40% and applied to both ankles, taking care not to stretch the origin and insertion (approximately 2–3 cm) in order to protect the skin [19]. The ABT application method was consisted of four steps [23]: (1) while maintaining slight ankle dorsiflexion, taping was applied to both sides, starting from the dorsal center of the talus bone to the calcaneus bone (Figure 3A); (2) while maintaining ankle inversion, taping was applied from 5 cm above the medial malleolus and passed through the lateral calcaneus below the subtalar joint, and then directed towards the lateral aspect of the dorsum (Figure 3B); (3) while maintaining ankle eversion, taping was applied from 5 cm above the lateral malleolus and passed through the medial calcaneus below the subtalar joint, and then directed towards the medial aspect of the dorsum (Figure 3C); and (4) while maintaining slight ankle dorsiflexion, taping was reapplied on top of the area taped by the initial taping to strengthen ankle support (Figure 3D) [18,19,23,24].

Figure 3.
Ankle balance taping (ABT): (A) taping was applied from the dorsal center of the talus bone to the calcaneus bone; (B) taping was applied from 5 cm above the medial malleolus and passed through the lateral calcaneus below the subtalar joint; (C) taping was applied from 5 cm above the lateral malleolus and passed through the medial calcaneus below the subtalar joint; (D) taping was reapplied on top of the area covered by the initial taping.
2.5.2. Ankle Placebo Taping (APT)
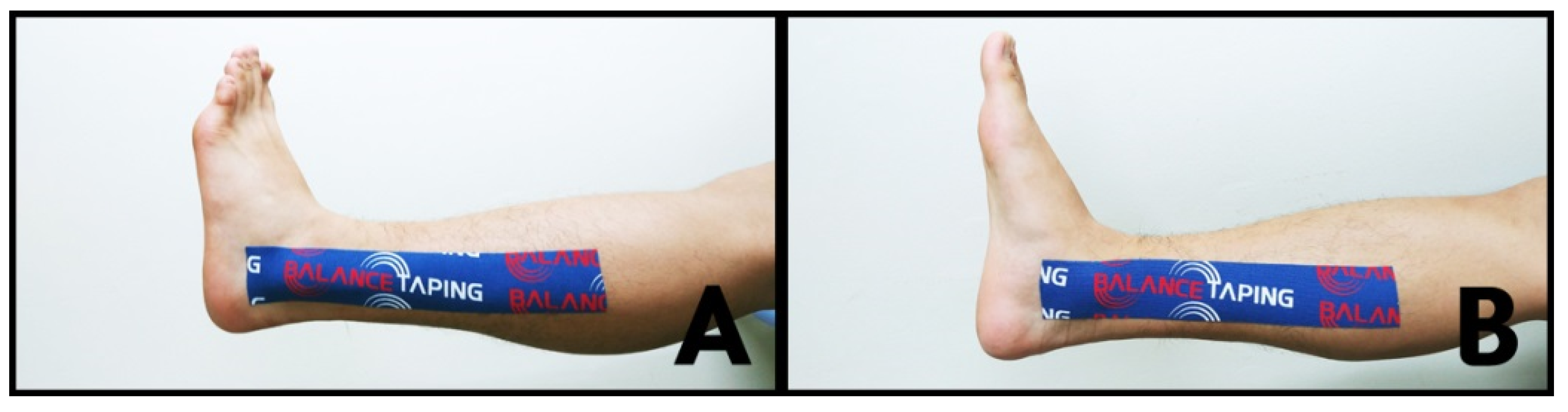
With the participant seated comfortably, the kinesiology tape was stretched by approximately 30%–40% and applied to both ankles, without stretching the origin and insertion sites (approximately 2–3 cm) in order to protect the skin [25]. APT consisted of two steps: (1) taping was applied from below the medial malleolus to half of the area below the inner knee (Figure 4A) and (2) from below the lateral malleolus to half of the area below the outer knee (Figure 4B) [18,19,24].
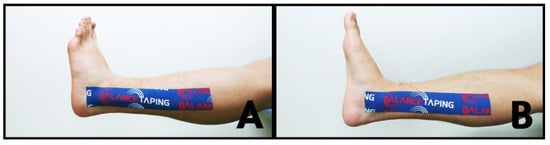
Figure 4.
Ankle placebo taping (APT): (A) taping was applied from below the medial malleolus to half of the area below the inner knee; (B) taping was applied from below the lateral malleolus to half of the area below the outer knee.
2.6. Statistical Analysis
The data were analyzed using SPSS 18.0 (IBM Corp., Armonk, NY, USA). The Shapiro–Wilk test was used to test for normality. Independent sample t-tests were used to identify significant differences in the baseline static and dynamic balance values in the ABT and APT groups, while paired samples t-tests were performed for comparisons of static and dynamic balance before and after ankle muscle fatigue-inducing exercise. Paired samples t-tests were also performed for comparisons of changes in static and dynamic balance after ABT and APT application following muscle fatigue-inducing exercise. The significance level (α) was set to 0.05.
3. Results
3.1. Participants’ General Characteristics
The general characteristics of the study participants are provided in Table 1. There were no significant differences in baseline static and dynamic balance in the ABT and APT groups (p > 0.05) (Table 2).

Table 1.
General characteristics of the study participants in each group (n = 31).

Table 2.
Comparison of initial surface area ellipse values in the two groups.
3.2. Static Balance and Dynamic Balance with Eyes Open
After ankle muscle fatigue-inducing exercises, both the ABT and APT groups showed a significant increase in surface area ellipses in the static state with eyes open (p < 0.05) (Table 3). After ankle muscle fatigue-inducing exercise, neither group showed significant changes in surface area ellipses in the dynamic state with eyes open (p > 0.05) (Table 3).

Table 3.
Comparison of variations in surface area ellipses on a static and a dynamic plate with eyes open before and after fatigue-inducing exercise.
After taping of the fatigued ankle, surface area ellipses in the static state with eyes open decreased significantly only in the ABT group (p < 0.05) (Table 4). After taping of the fatigued ankle, surface area ellipses in the dynamic state with eyes open decreased significantly only in the ABT group (p < 0.05) (Table 4).

Table 4.
Comparison of variations in surface area ellipses on a static and a dynamic plate with eyes open after fatigue-inducing exercise and after taping.
3.3. Static Balance and Dynamic Balance with Eyes Closed
After ankle muscle fatigue-inducing exercise, both the ABT and APT groups showed significant increases in surface area ellipses in the static state with eyes closed (p < 0.05) (Table 5). After ankle muscle fatigue-inducing exercise, both the ABT and APT groups showed a significant increase in surface area ellipses in the dynamic state with eyes closed (p < 0.05) (Table 5).

Table 5.
Comparison of variations in surface area ellipses on a static and a dynamic plate with eyes closed before and after fatigue-inducing exercise.
After taping of the fatigued ankle, surface area ellipses in the static state with eyes closed decreased significantly only in the ABT group (p < 0.05) (Table 6). After taping of the fatigued ankle, surface area ellipses in the dynamic state with eyes closed decreased significantly only in the ABT group (p < 0.05) (Table 6).

Table 6.
Comparison of variations in surface area ellipses on a static and a dynamic plate with eyes closed after fatigue-inducing exercise and after taping.
4. Discussion
Results demonstrate that both ABT and APT groups showed a significant increase in surface area ellipses in the static state with both eyes open and eyes closed after muscle fatigue-inducing exercise. Both groups showed a significant increase in surface area ellipses in the dynamic state with eyes closed after muscle fatigue-inducing exercise. However, in the dynamic state with eyes open, there were no significant differences in surface area ellipses after fatigue-inducing exercise.
Muscle fatigue may cause proprioceptive and kinesthetic impairment in joints [4]. Muscle fatigue may impair the maintenance of the joints and body during voluntary movement and cause low reactivity to stimuli [3]. Mello et al. [5] reported that muscle fatigue may have a negative effect on the ability to maintain standing posture and control balance due to reduced performance of the neuromuscular control mechanism. Therefore, surface area ellipses may increase significantly after muscle fatigue-inducing exercise due to impaired proprioception and kinesthetic sense and reduced neuromuscular control.
Vision has a major impact on postural stability, regardless of age [25]. It provides essential sensory information for maintaining dynamic stability during exercise in humans [26,27,28,29]. In the present study, surface area ellipses did not increase significantly after muscle fatigue-inducing exercise in the dynamic state with eyes open, and this may be due to the assistance of visual feedback on an unstable surface.
Compared to the APT group, the ABT group showed a significant decrease in surface area ellipses in both the static and dynamic states after muscle fatigue-inducing exercise. In a recent study by Lee and Lee, [18] balance ability was improved by applying ABT to a functionally unstable ankle caused by injury during a soccer match. The elasticity of kinesiology tape that returns to its original length may help return the joint to its original position [30]. The elasticity of kinesiology tape for ABT may help the ankle joint to return more quickly to an ankle’s neutral position on an unstable surface [16,19]. When kinesiology tape that has been stretched by 30–40% is applied to the ankles, the tape is instantly stretched even further by the ankle’s movement, and joint stability can be increased by the elasticity of the tape quickly returning the ankle’s neutral position [18,19].
This study had the following limitations. Firstly, since the intervention was applied to healthy adults with no pathological symptoms, the generalizability of the findings may be limited. Secondly, we did not use isokinetic equipment that induced muscle fatigue according to the muscle characteristics of each individual or provided evidence of ankle fatigue in this study. Thirdly, there may have been a learning effect for the measurement of post-fatigue activity that could have contributed to the results, since participants were younger and fatigue may not have been severe enough to induce changes. Fourthly, participants were not completely blinded to the interventions. Fifthly, we did not investigate and compare the use of tape directly applied to the muscle, such as the tibialis anterior and calf muscle, near the ankle where muscle fatigue was induced. In the future, additional studies should be conducted to improve on these limitations.
5. Conclusions
Following ankle muscle fatigue-inducing exercise, which reduced static and dynamic balance abilities, ABT improved static and dynamic balance with eyes open and closed. Therefore, we suggest that ABT helps recover immediately decreased balance resulting from muscle fatigue after daily physical activities and sports activities, thereby preventing ankle injuries.
Author Contributions
Conceptualization, J.-H.L.; methodology, H.-S.C. and J.-H.L.; software, H.-S.C.; validation, H.-S.C. and J.-H.L.; formal analysis, H.-S.C.; investigation, H.S.C. and J.-H.L.; resources, H.-S.C. and J.-H.L.; data curation, H.-S.C.; writing—Original draft preparation, H.-S.C. and J.-H.L.; writing—Review and editing, J.-H.L.; visualization, H.-S.C. and J.-H.L.; supervision, J.-H.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
This manuscript is a condensed form of the first author’s Master’s thesis from Dong-eui University.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Allen, D.G.; Westerblad, H. Role of phosphate and calcium stores in muscle fatigue. J. Physiol. 2001, 536, 657–665. [Google Scholar] [CrossRef]
- Gandevia, S.C. Spinal and supraspinal factors in human muscle fatigue. Physiol. Rev. 2001, 81, 1725–1789. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo, M.; Aguadol, X.; Gonzales, R.; Lopez, J.L.; Hakkinen, K. Maximal and explosive force production capacity and balance performance in men of different ages. Eur. J. Appl. Physiol. 1999, 79, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Rozzi, S.; Yuktanandana, P.; Pincivero, D.; Lephart, S. Role of Fatigue on Proprioception and Neuromuscular Control. In Proprioception and Neuromuscular Control in Joint Stability; Human Kinetics: Champaign, IL, USA, 2000; pp. 375–383. [Google Scholar]
- Mello, R.G.; Oliveira, L.F.; Nadal, J. Anticipation mechanism in body sway control and effect of muscle fatigue. J. Electromyogr. Kinesiol. 2007, 17, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.F.; Connolly, D.A.J.; Beynnon, B.D. Risk factors for lower extremity injury: A review of the literature. Br. J. Sports Med. 2003, 37, 13–29. [Google Scholar] [CrossRef]
- Vuillerme, N.; Forestier, N.; Nougier, V. Attentional demands and postural sway: The effect of the calf muscles fatigue. Med. Sci. Sports Exerc. 2002, 34, 1907–1912. [Google Scholar] [CrossRef]
- Billot, M.; Simoneau, E.M.; Van Hoecke, J.; Martin, A. Age–related relative increases in electromyography activity and torque according to the maximal capacity during upright standing. Eur. J. Appl. Physiol. 2010, 109, 669–680. [Google Scholar] [CrossRef]
- Riemann, B.L.; Myers, J.B.; Lephart, S.M. Comparison of the ankle, knee, hip, and trunk corrective action shown during single–leg stance on firm, foam, and multi axial surfaces. Arch. Phys. Med. Rehabil. 2003, 84, 90–95. [Google Scholar] [CrossRef]
- Yaggie, J.A.; McGregor, S.J. Effects of isokinetic ankle fatigue on the maintenance of balance and postural limits. Arch. Phys. Med. Rehabil. 2002, 83, 224–228. [Google Scholar] [CrossRef]
- Forestier, N.; Teasdale, N.; Nougier, V. Alteration of the position sense at the ankle induced by muscular fatigue in humans. Med. Sci. Sports. Exerc. 2002, 34, 117–122. [Google Scholar] [CrossRef]
- Hsu, Y.H.; Chen, W.Y.; Lin, H.C.; Wang, W.T.; Shih, Y.F. The effects of taping on scapular kinematics and muscle performance in baseball players with shoulder impingement syndrome. J. Electromyogr. Kinesiol. 2009, 19, 1092–1099. [Google Scholar] [CrossRef] [PubMed]
- Jaraczewska, E.; Long, C. Kinesio taping in stroke: Improving functional use of the upper extremity in hemiplegia. Top. Stroke Rehabil. 2006, 13, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Murray, H.; Husk, L. Effect of Kinesio taping on proprioception in the ankle. J. Orthop. Sports Phys. Ther. 2001, 31, A-37. [Google Scholar]
- Murray, H.M. Kinesio taping, muscle strength and ROM after ACL repair. J. Orthop. Sports Phys. Ther. 2000, 30, A-14. [Google Scholar]
- Vithoulka, I.; Beneka, A.; Malliou, P.; Aggelousis, N.; Karatsolis, K.; Diamantopoulos, K. The effects of Kinesio–taping on quadriceps strength during isokinetic exercise in healthy non–athlete women. Isokinet. Exerc. Sci. 2010, 18, 1–6. [Google Scholar] [CrossRef]
- González-Iglesias, J.; Fernández-de-Las-Peñas, C.; Cleland, J.A.; Huijbregts, P.; Del Rosario Gutiérrez-Vega, M. Short–term effects of cervical kinesio taping on pain and cervical range of motion in patients with acute whiplash injury: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2009, 39, 515–521. [Google Scholar] [CrossRef]
- Lee, B.G.; Lee, J.H. Immediate effects of ankle balance taping with kinesiology tape on the dynamic balance of young players with functional ankle instability. Technol. Health. Care. 2015, 23, 333–341. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, J.H. The immediate effects of ankle balance taping with kinesiology tape on ankle active range of motion and performance in the Balance Error Scoring System. Phys. Ther. Sport 2017, 25, 99–105. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Park, C.; Lee, S.; Lim, D.Y.; Yi, C.W.; Kim, J.H.; Jeon, C. Effects of the application of Low–Dye taping on the pain and stability of patients with plantar fasciitis. J. Phys. Ther. Sci. 2015, 27, 2491–2493. [Google Scholar] [CrossRef]
- Geronimi, M. Reproductibilité intra- et intersessions du test des limites de stabilité sur plateforme podobarométrique. Neurophysiol. Clin./Clin. Neurophysiol. 2014, 44, 139. [Google Scholar] [CrossRef]
- Lee, J.H.; Choi, S.W. Balance Taping: Clinical Application of Kinesiology Tape for Musculoskeletal Disorders; Wetape, Inc.: Paju, Korea, 2016. [Google Scholar]
- Kim, B.J.; Lee, J.H.; Han, J.T. The immediate effect of ankle balance taping using kinesiology tape on the weight-bearing ankle dorsiflexion range of motion and the dynamic balance in asymptomatic subjects. J. Korean Soc. Phys. Med. 2014, 9, 263–270. [Google Scholar] [CrossRef][Green Version]
- Saucedo, F.; Yang, F. Effects of visual deprivation on stability among young and older adults during treadmill walking. Gait Posture 2017, 54, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Patla, A.E. How is human gait controlled by vision. Ecol. Psychol. 1998, 10, 287–302. [Google Scholar]
- Marigold, D.S. Role of peripheral visual cues in online visual guidance of locomotion. Exerc. Sport Sci. Rev. 2008, 36, 145–151. [Google Scholar] [CrossRef]
- Redfern, M.S.; Yardley, L.; Bronstein, A.M. Visual influences on balance. J. Anxiety Disord. 2001, 15, 81–94. [Google Scholar] [CrossRef]
- Rietdyk, S.; Rhea, C.K. Control of adaptive locomotion: Effect of visual obstruction and visual cues in the environment. Exp. Brain Res. 2006, 169, 272–278. [Google Scholar] [CrossRef]
- Ristow, O.; Pautke, C.; Kehl, V.; Koerdt, S.; Schwärzler, K.; Hahnefeld, L.; Hohlweg-Majert, B. Influence of kinesiologic tape on postoperative swelling, pain and trismus after zygomatico–orbital fractures. J. Cranio-Maxillofac. Surg. 2014, 42, 469–476. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).