Obesity and Morbidity Risk in the U.S. Veteran
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Independent Variables
2.3. Dependent Variables for RQs 1 through 10
2.4. Model and Methods
3. Results
3.1. Descriptive Statistics
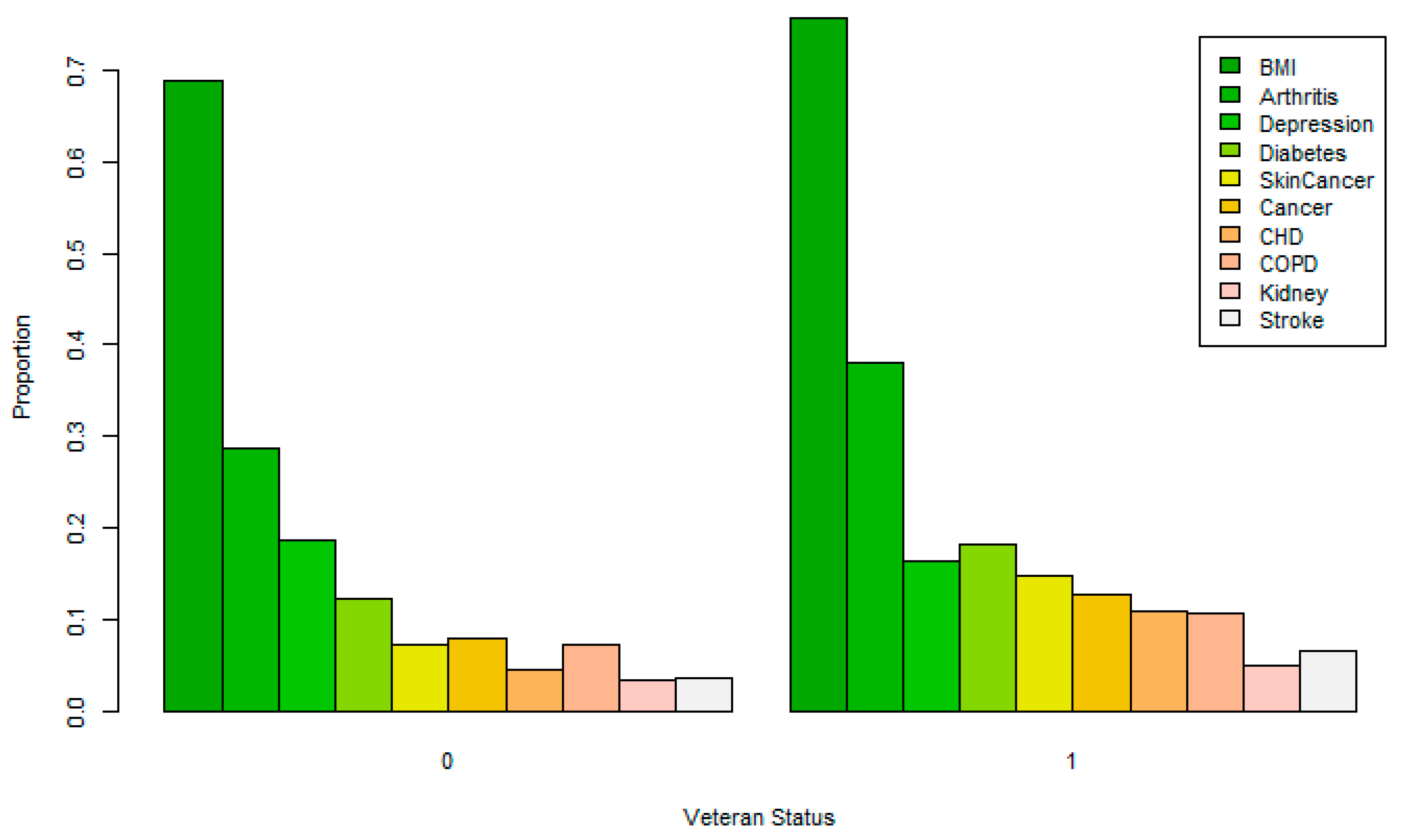
3.1.1. Dichotomous Variables
3.1.2. Other Non-Geographical Factor Variables
3.2. Inferential Statistics
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Censin, J.C.; Peters, S.A.E.; Bovijn, J.; Ferreira, T.; Pulit, S.L.; Magi, R.; Mahajan, A.; Holmes, M.V.; Lindgren, C.M. Causal relationships between obesity and the leading causes of death in women and men. PLoS Genet. 2019, 15, e1008405. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.; Mathur, K.; Barraza, G.; Sin, S.; Yang, C.J.; Arens, R.; Sutton, N.; Mahgerefteh, J. The relationship of hypertension with obesity and obstructive sleep apnea in adolescents. Pediatr. Pulmonol. 2020, 55, 1020–1027. [Google Scholar] [CrossRef] [PubMed]
- Koh, K.; Grady, S.C.; Darden, J.T.; Vojnovic, I. Adult obesity prevalence at the county level in the united states, 2000–2010: Downscaling public health survey data using a spatial microsimulation approach. Spat. Spatio-Temporal Epidemiol. 2018, 26, 153–164. [Google Scholar] [CrossRef]
- Grossbard, J.R.; Lehavot, K.; Hoerster, K.D.; Jakupcak, M.; Seal, K.H.; Simpson, T.L. Relationships among veteran status, gender, and key health indicators in a national young adult sample. Psychiatr. Serv. (Washington, DC) 2013, 64, 547–553. [Google Scholar] [CrossRef]
- Chatterjee, A.; Gerdes, M.W.; Martinez, S.G. Identification of risk factors associated with obesity and overweight—A machine learning overview. Sensors 2020, 20, 2734. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D. Improving weight management among veterans. J. Gen. Int. Med. 2017, 32, 1–3. [Google Scholar] [CrossRef]
- El-Atat, F.; Aneja, A.; Mcfarlane, S.; Sowers, J. Obesity and hypertension. Endocrinol. Metab. Clin. North Am. 2003, 32, 823–854. [Google Scholar] [CrossRef]
- Kleine, C.; Moradi, H.; Streja, E.; Kalantar-Zadeh, K. Racial and ethnic disparities in the obesity paradox. Am. J. Kidney Dis. 2018, 72, S26–S32. [Google Scholar] [CrossRef]
- Scherrer, J.F.; Salas, J.; Lustman, P.J.; van den Berk-Clark, C.; Schnurr, P.P.; Tuerk, P.; Cohen, B.E.; Friedman, M.J.; Norman, S.B.; Schneider, F.D. The role of obesity in the association between posttraumatic stress disorder and incident diabetes. JAMA Psychiatry 2018, 75, 1189–1198. [Google Scholar] [CrossRef]
- Biener, A.; Cawley, J.; Meyerhoefer, C. The high and rising costs of obesity to the US health care system. J. Gen. Int. Med. 2017, 32, 6–8. [Google Scholar] [CrossRef]
- Breland, J.; Phibbs, C.; Hoggatt, K.; Washington, D.L.; Lee, J.; Haskell, S.; Uchendu, U.S.; Saechao, F.S.; Zephyrin, L.C.; Frayne, S.M. The obesity epidemic in the veterans health administration: Prevalence among key populations of women and men veterans. J. Gen. Int. Med. 2017, 32, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Rush, T.; LeardMann, C.A.; Crum-Cianflone, N. Obesity and associated adverse health outcomes among U.S. military members and veterans: Findings from the millennium cohort study. Obesity (Silver Spring, Md.) 2016, 24, 1582–1589. [Google Scholar] [CrossRef] [PubMed]
- Clinical medicine. Available online: https://natlib-primo.hosted.exlibrisgroup.com/primo-explore/search?query=any,contains,9913371113502836&tab=catalogue&search_scope=NLNZ&vid=NLNZ&offset=0 (accessed on 25 June 2020).
- Breland, J.Y.; Wong, M.S.; Frayne, S.M.; Hoggatt, K.J.; Steers, W.N.; Saechao, F.; Washington, D.L. Obesity and health care experiences among women and men veterans. Women’s Health Issues Off. Publ. Jacobs Inst. Women’s Health 2019, 29, S32–S38. [Google Scholar] [CrossRef] [PubMed]
- McKinnon, C.R.; Garvin, J.T. Weight reduction goal achievement among veterans with mental health diagnoses. J. Am. Psychiatr. Nurs. Assoc. 2019, 25, 257–265. [Google Scholar] [CrossRef]
- Vimalananda, V.G.; Foster-Schubert, K. Geographic variation in obesity, behavioral treatment, and bariatric surgery for veterans. Obesity (Silver Spring, Md.) 2019, 27, 12. [Google Scholar] [CrossRef]
- Mokdad, A.H.; Ford, E.S.; Bowman, B.A.; Dietz, W.H.; Vinicor, F.; Bales, V.S.; Marks, J.S. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA J. Am. Med. Assoc. 2003, 289, 76–79. [Google Scholar] [CrossRef]
- Selim, A.J.; Berlowitz, D.R.; Fincke, G.; Cong, Z.; Rogers, W.; Haffer, S.C.; Ren, X.S.; Lee, A.; Qian, S.X.; Miller, D.R. The health status of elderly veteran enrollees in the veterans health administration. J. Am. Geriatr. Soc. 2004, 52, 1271–1276. [Google Scholar] [CrossRef]
- Department of Veterans Affairs. Available online: https://www.govinfo.gov/content/pkg/CFR-2011-title38-vol1/pdf/CFR-2011-title38-vol1-sec3-12a.pdf (accessed on 29 June 2020).
- Profile of Veterans: 2017. Available online: https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2017.pdf (accessed on 29 June 2020).
- Stefanovics, E.A.; Potenza, M.N.; Pietrzak, R.H. The physical and mental health burden of obesity in U.S. veterans: Results from the national health and resilience in veterans study. J. Psychiatr Res. 2018, 103, 112–119. [Google Scholar] [CrossRef]
- Milaneschi, Y.; Simmons, W.K.; van Rossum, E.F.C.; Penninx, B.W. Depression and obesity: Evidence of shared biological mechanisms. Mol. Psychiatry 2019, 24, 18–33. [Google Scholar] [CrossRef]
- Agustini, B.; Lotfaliany, M.; Woods, R.L.; McNeil, J.J.; Nelson, M.R.; Shah, R.C.; Murray, A.M.; Ernst, M.E.; Reid, C.M.; Tonkin, A. Patterns of association between depressive symptoms and chronic medical morbidities in older adults. JAGS 2020. [Google Scholar] [CrossRef]
- Ziade, N.; El Khoury, B.; Zoghbi, M.; Merheb, G.; Karam, G.A.; Mroue, K.; Messaykeh, J. Prevalence and pattern of comorbidities in chronic rheumatic and musculoskeletal diseases: The COMORD study. Sci. Rep. 2020, 10, 7683. [Google Scholar] [CrossRef] [PubMed]
- Dorflinger, L.M.; Masheb, R.M. PTSD is associated with emotional eating among veterans seeking treatment for overweight/obesity. Eating Behav. 2018, 31, 8–11. [Google Scholar] [CrossRef]
- Santhiveeran, J. The influence of obesity and sociodemographic factors on the health hardships among women veterans. Soc. Work Health Care 2019, 58, 459–470. [Google Scholar] [CrossRef] [PubMed]
- Wischik, D.L.; Magny-Normilus, C.; Whittemore, R. Risk factors of obesity in veterans of recent conflicts: Need for diabetes prevention. Curr. Diabetes Rep. 2019, 19. [Google Scholar] [CrossRef] [PubMed]
- Williams, E.P.; Mesidor, M.; Winters, K.; Dubbert, P.M.; Wyatt, S.B. Overweight and obesity: Prevalence, consequences, and causes of a growing public health problem. Curr. Obes. Rep. 2015, 4, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Wyatt, J.C. Correction to: How can clinicians, specialty societies and others evaluate and improve the quality of apps for patient use? BMC Med. 2019, 17. [Google Scholar] [CrossRef]
- U.S. Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System (BRFSS). Available online: https://www.cdc.gov/brfss/index.html (accessed on 2 February 2020).
- Fitting Regression Models to Data from Complex Surveys. An Appendix to an R Companion to Applied Regression. Available online: https://socialsciences.mcmaster.ca/jfox/Books/Companion/appendices/Appendix-Surveys.pdf (accessed on 6 February 2020).
- Analysis of Complex Survey Samples. R Package Version 3.33-2. 2019. Available online: https://www.jstatsoft.org/article/view/v009i08 (accessed on 25 June 2020).
- A Language and Environment for Statistical Computing. Foundation for Statistical Computing. Available online: https://www.R-project.org/ (accessed on 25 June 2020).
- Williams, L.M.; Pines, A.; Goldstein-Piekarski, A.; Gosas, L.G.; Kullar, M.; Sacchet, M.D.; Gevaert, O.; Bailenson, J.; Lavori, P.W.; Dagum, P.; et al. The ENGAGE study: Integrating neuroimaging, virtual reality and smartphone sensing to understand self-regulation for managing depression and obesity in a precision medicine model. Behav. Res. Ther. 2018, 101, 58–70. [Google Scholar] [CrossRef]
- Rodriguez, V.J.; Chahine, A.; Parrish, M.S.; Alcaide, M.L.; Lee, T.K.; Hurwitz, B.; Sawhney, M.; Weiss, S.M.; Jones, D.L.; Kumar, M. The contribution of syndemic conditions to cardiovascular disease risk. AIDS Care 2020, 13, 1–9. [Google Scholar] [CrossRef]
- Schneiderman, A.I.; Dougherty, D.D.; Wolters, C.L.; Fonseca, V.P.; Bossarte, R.M.; Arjomandi, M. Diagnosing chronic obstructive pulmonary disease among afghanistan and iraq veterans: Veterans affair’s concordance with clinical guidelines for spirometry administration. Milit. Med. 2017, 182, e1993–e2000. [Google Scholar] [CrossRef][Green Version]
- Liu, J.; Lezama, N.; Gasper, J.; Kawata, J.; Morley, S.; Helmer, D.; Ciminera, P. Burn pit emissions exposure and respiratory and cardiovascular conditions among airborne hazards and open burn pit registry participants. J. Occup. Environ. Med. 2016, 58, e249–e255. [Google Scholar] [CrossRef]
- Abraham, J.H.; Clark, L.L.; Sharkey, J.M.; Baird, C.P. Trends in rates of chronic obstructive respiratory conditions among US military personnel, 2001–2013. U.S. Army Med. Dep. J. 2014, 33–43. [Google Scholar]
- Spelta, F.; Fratta Pasini, A.M.; Cazzoletti, L.; Ferrari, M. Body weight and mortality in COPD: Focus on the obesity paradox. Eat Weight Disord. 2018, 23, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Hidayat, K.; Zhou, H.; Shi, B. Influence of physical activity at a young age and lifetime physical activity on the risks of 3 obesity-related cancers: Systematic review and meta-analysis of observational studies. Nutr. Rev. 2020, 78, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Gu, S.; Li, R.; Leader, J.K.; Zheng, B.; Bon, J.; Gur, D.; Sciurba, F.; Jin, C.; Pu, J. Obesity and extent of emphysema depicted at CT. Clin. Radiol. 2015, 70, e14–e19. [Google Scholar] [CrossRef] [PubMed]
- Guerra, S.; Sherrill, D.L.; Bobadilla, A.; Martinez, F.D.; Barbee, R.A. The relation of body mass index to asthma, chronic bronchitis, and emphysema. Chest 2002, 122, 1256–1263. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.; Wong, C.A.; Boyko, E.J.; Phillips, C.J.; Gackstetter, G.D.; Ryan, M.A.K.; Smith, T.C. The effects of exposure to documented open-air burn pits on respiratory health among deployers of the millennium cohort study. J. Occup. Environ. Med. 2012, 54, 708–716. [Google Scholar] [CrossRef] [PubMed]
- Zell-Baran, L.; Meehan, R.; Wolff, J.; Strand, M.; Krefft, S.; Gottschall, E.B.; Macedonia, T.; Gross, J.; Sanders, O.; Pepper, G.; et al. Military occupational specialty codes: Utility in predicting inhalation exposures in post-9/11 deployers. J. Occup. Environ. Med. 2019, 61, 1036–1040. [Google Scholar] [CrossRef]
- Samanic, C.; Gridley, G.; Chow, W.; Lubin, J.; Hoover, R.N.; Fraumeni, J.F. Obesity and cancer risk among white and black united states veterans. Cancer Causes Control 2004, 15, 35–44. [Google Scholar] [CrossRef]
- Pavuk, M.; Michalek, J.E.; Ketchum, N.S. Prostate cancer in US air force veterans of the vietnam war. J. Expo. Sci. Environ. Epidemiol. 2006, 16, 184–190. [Google Scholar] [CrossRef]
- Chadid, S.; Kreger, B.E.; Singer, M.R.; Loring Bradlee, M.; Moore, L.L. Anthropometric measures of body fat and obesity-related cancer risk: Sex-specific differences in framingham offspring study adults. Int. J. Obes. (2005) 2020, 44, 601–608. [Google Scholar] [CrossRef]
- Campisciano, G.; de Manzini, N.; Delbue, S.; Cason, C.; Cosola, D.; Basile, G.; Ferrante, P.; Comar, M.; Palmisano, S. The obesity-related gut bacterial and viral dysbiosis can impact the risk of colon cancer development. Microorganisms 2020, 8, 431. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; McGlynn, K.A.; Nations, J.A.; Shriver, C.D.; Zhu, K. Comorbidity and stage at diagnosis among lung cancer patients in the US military health system. Cancer Causes Control Int. J. Stud. Cancer Hum. Popul. 2020, 31, 255. [Google Scholar] [CrossRef] [PubMed]
- Dominick, K.L.; Golightly, Y.M.; Jackson, G.L. Arthritis prevalence and symptoms among US non-veterans, veterans, and veterans receiving department of veterans affairs healthcare. J. Rheumatol. 2006, 33, 348. [Google Scholar] [PubMed]
- Rivera, J.C.; Amuan, M.E.; Morris, R.M.; Johnson, A.E.; Pugh, M.J. Arthritis, comorbidities, and care utilization in veterans of operations enduring and iraqi freedom. J. Orthop. Res. 2017, 35, 682–687. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Oliveira, M.C.; Vullings, J.; van de Loo, F.A.J. Osteoporosis and osteoarthritis are two sides of the same coin paid for obesity. Nutrition 2020, 70, 110486. [Google Scholar] [CrossRef] [PubMed]
- Porter, C.K.; Riddle, M.S.; Laird, R.M.; Loza, M.; Cole, S.; Gariepy, C.; Alcala, A.; Gutierrez, R.; Baribaud, F.; Rao, N.L.; et al. Cohort profile of a US military population for evaluating pre-disease and disease serological biomarkers in rheumatoid and reactive arthritis: Rationale, organization, design, and baseline characteristics. Contemp. Clin. Trials Commun. 2020, 17. [Google Scholar] [CrossRef]
- Schonfeld, L.; Braue, L.A.; Stire, S.; Gum, A.M.; Cross, B.L.; Brown, L.M. Behavioral health and adjustment to college life for student service members/veterans. J. Am. Coll. Health Stud. Serv. Members/Veterans Participating Higher Educ. 2015, 63, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Forkus, S.R.; Breines, J.G.; Weiss, N.H. PTSD and alcohol misuse: Examining the mediating role of fear of self-compassion among military veterans. Psychol. Trauma-Theory Res. Pract. Policy 2020, 12, 364–372. [Google Scholar] [CrossRef]
- Curry, J.F.; Shepherd-Banigan, M.; Van Voorhees, E.; Wagner, H.R.; Kelley, M.L.; Strauss, J.; Naylor, J. Veterans Affairs Mid-Atlantic MIRECC Women Veterans Work Group; Veterans Affairs Mid-Atlantic MIRECC Work Group. Sex differences in predictors of recurrent major depression among current-era military veterans. Psychol. Serv. 2019. [Google Scholar] [CrossRef]
- Brown, M.C.; Sims, K.J.; Gifford, E.J.; Goldstein, K.M.; Johnson, M.R.; Williams, C.D.; Provenzale, D. Gender-based differences among 1990–1991 gulf war era veterans: Demographics, lifestyle behaviors, and health conditions. Women Health Issues 2019, 29, S47–S55. [Google Scholar] [CrossRef]
- Barbieri, D.; Goicoechea, M.; Sánchez-Niño, M.D.; Ortiz, A.; Verde, E.; Verdalles, U.; de Jose, A.P.; Delgado, A.; Hurtado, E.; Sanchez-Camara, L.; et al. Obesity and chronic kidney disease progression-the role of a new adipocytokine: C1q/tumour necrosis factor-related protein-1. Clin. Kidney J. 2019, 12, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Kurniawan, A.L.; Hsu, C.; Rau, H.; Lin, L.; Chao, J.C. Association of kidney function-related dietary pattern, weight status, and cardiovascular risk factors with severity of impaired kidney function in middle-aged and older adults with chronic kidney disease: A cross-sectional population study. Nutr. J. 2019, 18, 27. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Sy, J.; Tantisattamo, E. The enlarging effect of obesity on estimating kidney function: Blaming serum creatinine versus indexation and methodology. Obesity (Silver Spring) 2019, 27, 1930–1931. [Google Scholar] [CrossRef] [PubMed]
- Cole, J.B.; Florez, J.C. Genetics of diabetes mellitus and diabetes complications. Nat. Rev. Nephrol. 2020. [Google Scholar] [CrossRef]
- Yi, S.; Hong, J.; Ohrr, H.; Yi, J. Agent orange exposure and disease prevalence in korean vietnam veterans: The korean veterans health study. Environ. Res. 2014, 133, 56–65. [Google Scholar] [CrossRef]
- Akhtar, F.Z.; Garabrant, D.H.; Ketchum, N.S.; Michalek, J.E. Cancer in US air force veterans of the vietnam war. J. Occup. Environ. Med. 2004, 46. [Google Scholar] [CrossRef]
- Veterans and Agent Orange: Herbicide/Dioxin Exposure and Type 2 Diabetes. Available online: http://libproxy.txstate.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=cat00022a&AN=txi.b3119483&site=eds-live&scope=site (accessed on 25 June 2020).
| BRFSS Variable Name | Question | Code |
|---|---|---|
| AGE_G | Six-level imputed age category | 1—18 to 24 2—25 to 34 3—35 to 44 4—45 to 54 5–55 to 64 6—65+ |
| IMPRACE | Imputed race/ethnicity value | 1—White 2—Black 3—Asian 4—American Indian/Alaskan 5—Hispanic 6—Other non-Hispanic |
| SEX1 | What is your sex? or What was your sex at birth? Was it… | 0—Female 1—Male |
| MARITAL | Are you (marital status)? | 1—Married 2—Divorced 3—Widowed 4—Separated 5—Never married 6—A member of an unmarried coupled |
| BRFSS Variable Name | Question | Code |
|---|---|---|
| INCOME2 | Is your annual household income from all sources? | 1—<$10K 2—$10K ≤ Income < $15K 3—$15K ≤ Income < $20K 4—$20K ≤ Income < $25K 5—$25K ≤ Income < $35K 6—$35K ≤ Income < $50K 7—$50K ≤ Income < $75K 8—$75K or more 9—Don’t Know/Not Sure /Refused/BLANK |
| EDUCA | What is the highest grade or year of school you completed? | 1—None or Only Kindergarten 2—Grades 1 through 8 3—Grades 9 through 11 4—Grades 12 or GED 5—College 1 to 3 years 6—College 4+ years (Graduate) |
| EMPLOY1 | Are you currently…? | 1—Employed for Wages 2—Self-Employed 3—Out of Work ≥1 Year 4—Out of Work <1 Year 5—Homemaker 6—Student 7—Retired 8—Unable to Work |
| BRFSS Variable Name | Question | Coded Levels |
|---|---|---|
| VETERAN3 | Have you ever served on active duty in the United States Armed Forces, either in the regular military or in a National Guard or military reserve unit? | 0—No 1—Yes |
| Variable | Question from Codebook | Recoded Response |
|---|---|---|
| BMI5CAT | Four categories of body mass index (BMI) | 0—No 1—Yes |
| CVDCRHD4 (RQ2) | (Ever told) you had angina or coronary heart disease? | 0—No 1—Yes |
| CVDSTRK3 (RQ3) | (Ever told) you had a stroke. | 0—No 1—Yes |
| CHCSCNCR (RQ4) | (Ever told) you had skin cancer? | 0—No 1—Yes |
| CHCOCNCR (RQ5) | (Ever told) you had any other types of cancer? | 0—No 1—Yes |
| CHCCOPD1 (RQ6) | (Ever told) you have chronic obstructive pulmonary disease, emphysema or chronic bronchitis? | 0—No 1—Yes |
| HAVARTH3 (RQ7) | (Ever told) you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia? (arthritis diagnoses include: rheumatism, polymyalgia rheumatica; osteoarthritis (not osteoporosis (sic)); tendonitis, bursitis, bunion, tennis elbow; carpal tunnel syndrome, tarsal tunnel syndrome; joint infection, etc.) | 0—No 1—Yes |
| ADDEPEV2 (RQ8) | (Ever told) you have a depressive disorder (including depression, major depression, dysthymia, or minor depression)? | 0—No 1—Yes |
| CHCKDNY1 (RQ9) | (Ever told) you have kidney disease? (Do NOT include kidney stones, bladder infection or incontinence.) | 0—No 1—Yes |
| DIABETE3 (RQ10) | (Ever told) you have diabetes (If ´Yes´ and respondent is female, ask ´Was this only when you were pregnant? (Pregnancy-Related coded as 0) | 0—No 1—Yes |
| 87.9%* | 12.1%* | |||
|---|---|---|---|---|
| Variable | Not Veteran | Veteran | Relative Risk | Odds Ratio |
| BMI | 0.688 | 0.758 | 1.102 | 1.420 |
| Arthritis | 0.287 | 0.380 | 1.324 | 1.523 |
| Depression | 0.187 | 0.163 | 0.872 | 0.847 |
| Diabetes | 0.122 | 0.183 | 1.500 | 1.612 |
| Skin Cancer | 0.073 | 0.147 | 2.014 | 2.188 |
| Cancer | 0.078 | 0.128 | 1.641 | 1.735 |
| Coronary Heart Disease (CHD) | 0.044 | 0.108 | 2.455 | 2.631 |
| Chronic Obstructive Pulmonary Disease (COPD) | 0.073 | 0.107 | 1.466 | 1.522 |
| Kidney | 0.034 | 0.049 | 1.441 | 1.464 |
| Stroke | 0.036 | 0.065 | 1.806 | 1.862 |
| Variable | Estimate | SE | t Value | Pr (>|t|) | Odds Ratio |
|---|---|---|---|---|---|
| (Intercept) | −0.090 | 0.192 | −0.47 | 0.640 | |
| 25 to 34 | 0.613 | 0.030 | 20.34 | <0.001 | 1.846 |
| 35 to 44 | 0.971 | 0.032 | 30.43 | <0.001 | 2.641 |
| 45 to 54 | 1.115 | 0.032 | 34.53 | <0.001 | 3.051 |
| 55 to 64 | 1.066 | 0.032 | 33.11 | <0.001 | 2.903 |
| 65+ | 0.954 | 0.035 | 27.54 | <0.001 | 2.595 |
| Black | 0.495 | 0.024 | 20.39 | <0.001 | 1.641 |
| Asian | −0.425 | 0.039 | −11.04 | <0.001 | 0.654 |
| American Indian/Alaskan | 0.265 | 0.055 | 4.78 | <0.001 | 1.303 |
| Hispanic | 0.544 | 0.026 | 21.05 | <0.001 | 1.724 |
| Other Non-Hispanic | 0.100 | 0.035 | 2.84 | 0.005 | 1.105 |
| Male | 0.408 | 0.014 | 29.61 | <0.001 | 1.503 |
| Divorced | −0.144 | 0.020 | −7.28 | <0.001 | 0.866 |
| Widowed | −0.241 | 0.023 | −10.41 | <0.001 | 0.786 |
| Separated | −0.129 | 0.044 | −2.94 | 0.003 | 0.879 |
| Never married | −0.256 | 0.020 | −12.91 | <0.001 | 0.774 |
| A member of an unmarried coupled | −0.104 | 0.034 | −3.08 | 0.002 | 0.901 |
| $10K ≤ Income < $15K | 0.143 | 0.043 | 3.3 | <0.001 | 1.154 |
| $15K ≤ Income < $20K | 0.132 | 0.040 | 3.26 | 0.001 | 1.141 |
| $20K ≤ Income < $25K | 0.157 | 0.040 | 3.95 | <0.001 | 1.170 |
| $25K ≤ Income < $35K | 0.122 | 0.039 | 3.12 | 0.002 | 1.129 |
| $35K ≤ Income < $50K | 0.172 | 0.038 | 4.49 | <0.001 | 1.188 |
| $50K ≤ Income < $75K | 0.160 | 0.038 | 4.17 | <0.001 | 1.173 |
| 8-$75K or more | −0.015 | 0.037 | −0.41 | 0.685 | 0.985 |
| 9-Don’t Know/Not Sure/Refused/BLANK | 0.214 | 0.036 | 5.91 | <0.001 | 1.238 |
| Grades 1 through 8 | 0.277 | 0.187 | 1.48 | 0.138 | 1.319 |
| Grades 9 through 11 | 0.005 | 0.184 | 0.03 | 0.979 | 1.005 |
| Grades 12 or GED * | 0.047 | 0.183 | 0.26 | 0.796 | 1.049 |
| College 1 to 3 years | 0.073 | 0.183 | 0.4 | 0.692 | 1.075 |
| College 4+ years (Graduate) | −0.228 | 0.183 | −1.24 | 0.215 | 0.796 |
| Self-Employed | −0.250 | 0.023 | −11.09 | <0.001 | 0.778 |
| Out of Work ≥1 Year | −0.055 | 0.046 | −1.21 | 0.227 | 0.946 |
| Out of Work <1 Year | −0.059 | 0.043 | −1.37 | 0.170 | 0.943 |
| Homemaker | −0.269 | 0.030 | −9.09 | <0.001 | 0.764 |
| Student | −0.330 | 0.037 | −8.92 | <0.001 | 0.719 |
| Retired | −0.170 | 0.021 | −7.95 | <0.001 | 0.844 |
| Unable to Work | −0.001 | 0.028 | −0.02 | 0.982 | 0.999 |
| Alaska | −0.204 | 0.064 | −3.19 | 0.001 | 0.815 |
| Arizona | −0.217 | 0.047 | −4.62 | <0.001 | 0.805 |
| Arkansas | 0.036 | 0.051 | 0.71 | 0.480 | 1.037 |
| California | −0.263 | 0.040 | −6.52 | <0.001 | 0.769 |
| Colorado | −0.410 | 0.041 | −10.01 | <0.001 | 0.664 |
| Connecticut | −0.164 | 0.041 | −4.03 | <0.001 | 0.849 |
| Delaware | 0.005 | 0.049 | 0.11 | 0.913 | 1.005 |
| District of Columbia | −0.483 | 0.048 | −9.96 | <0.001 | 0.617 |
| Florida | −0.151 | 0.045 | −3.36 | 0.001 | 0.860 |
| Georgia | −0.063 | 0.041 | −1.53 | 0.126 | 0.939 |
| Guam | −0.125 | 0.076 | −1.64 | 0.100 | 0.882 |
| Hawaii | −0.266 | 0.046 | −5.78 | <0.001 | 0.766 |
| Idaho | −0.147 | 0.055 | −2.69 | 0.007 | 0.863 |
| Illinois | −0.075 | 0.046 | −1.62 | 0.104 | 0.928 |
| Indiana | −0.075 | 0.044 | −1.7 | 0.089 | 0.928 |
| Iowa | 0.089 | 0.041 | 2.14 | 0.032 | 1.093 |
| Kansas | 0.074 | 0.041 | 1.82 | 0.069 | 1.077 |
| Kentucky | 0.042 | 0.049 | 0.87 | 0.387 | 1.043 |
| Louisiana | 0.023 | 0.049 | 0.46 | 0.647 | 1.023 |
| Maine | −0.108 | 0.044 | −2.45 | 0.014 | 0.897 |
| Maryland | −0.072 | 0.039 | −1.85 | 0.065 | 0.931 |
| Massachusetts | −0.196 | 0.044 | −4.47 | <0.001 | 0.822 |
| Michigan | −0.026 | 0.041 | −0.63 | 0.530 | 0.975 |
| Minnesota | −0.042 | 0.038 | −1.11 | 0.266 | 0.959 |
| Mississippi | 0.151 | 0.049 | 3.08 | 0.002 | 1.162 |
| Missouri | −0.081 | 0.049 | −1.67 | 0.095 | 0.922 |
| Montana | −0.188 | 0.050 | −3.76 | 0.000 | 0.828 |
| Nebraska | 0.068 | 0.042 | 1.64 | 0.102 | 1.071 |
| Nevada | −0.128 | 0.060 | −2.12 | 0.034 | 0.880 |
| New Hampshire | −0.128 | 0.047 | −2.72 | 0.007 | 0.880 |
| New Jersey | −0.145 | 0.064 | −2.25 | 0.024 | 0.865 |
| New Mexico | −0.273 | 0.047 | −5.81 | <0.001 | 0.761 |
| New York | −0.187 | 0.038 | −4.95 | <0.001 | 0.830 |
| North Carolina | −0.067 | 0.049 | −1.36 | 0.173 | 0.935 |
| North Dakota | 0.200 | 0.049 | 4.07 | <0.001 | 1.222 |
| Ohio | 0.030 | 0.042 | 0.71 | 0.480 | 1.030 |
| Oklahoma | 0.032 | 0.048 | 0.66 | 0.512 | 1.032 |
| Oregon | −0.171 | 0.046 | −3.76 | 0.000 | 0.843 |
| Pennsylvania | −0.050 | 0.046 | −1.08 | 0.280 | 0.952 |
| Puerto Rico | −0.408 | 0.053 | −7.73 | <0.001 | 0.665 |
| Rhode Island | −0.121 | 0.048 | −2.54 | 0.011 | 0.886 |
| South Carolina | 0.005 | 0.042 | 0.11 | 0.910 | 1.005 |
| South Dakota | 0.079 | 0.056 | 1.4 | 0.162 | 1.082 |
| Tennessee | −0.030 | 0.051 | −0.59 | 0.558 | 0.970 |
| Texas | −0.053 | 0.050 | −1.06 | 0.291 | 0.949 |
| Utah | −0.178 | 0.040 | −4.39 | <0.001 | 0.837 |
| Vermont | −0.295 | 0.046 | −6.43 | <0.001 | 0.744 |
| Virginia | −0.086 | 0.042 | −2.04 | 0.041 | 0.918 |
| Washington | −0.114 | 0.039 | −2.88 | 0.004 | 0.893 |
| West Virginia | 0.155 | 0.049 | 3.16 | 0.002 | 1.168 |
| Wisconsin | 0.018 | 0.051 | 0.36 | 0.722 | 1.018 |
| Wyoming | −0.195 | 0.050 | −3.88 | <0.001 | 0.823 |
| Veteran? | 0.112 | 0.021 | 5.24 | <0.001 | 1.119 |
| Research Question | Comorbidity | Lower CI | Odds Ratio | Upper CI |
|---|---|---|---|---|
| RQ1 | BMI | 1.07 | 1.12 | 1.17 |
| RQ2 | Arthritis | 1.21 | 1.26 | 1.31 |
| RQ3 | Depression | 1.24 | 1.29 | 1.35 |
| RQ4 | Diabetes | 1.05 | 1.10 | 1.16 |
| RQ5 | Skin Cancer | 1.12 | 1.18 | 1.25 |
| RQ6 | Cancer | 1.30 | 1.38 | 1.47 |
| RQ7 | CHD | 1.24 | 1.32 | 1.41 |
| RQ8 | COPD | 1.37 | 1.46 | 1.56 |
| RQ9 | Kidney Disease | 0.99 | 1.08 | 1.19 |
| RQ10 | Stroke | 1.17 | 1.28 | 1.39 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Betancourt, J.A.; Stigler Granados, P.; Pacheco, G.J.; Shanmugam, R.; Kruse, C.S.; Fulton, L.V. Obesity and Morbidity Risk in the U.S. Veteran. Healthcare 2020, 8, 191. https://doi.org/10.3390/healthcare8030191
Betancourt JA, Stigler Granados P, Pacheco GJ, Shanmugam R, Kruse CS, Fulton LV. Obesity and Morbidity Risk in the U.S. Veteran. Healthcare. 2020; 8(3):191. https://doi.org/10.3390/healthcare8030191
Chicago/Turabian StyleBetancourt, Jose A., Paula Stigler Granados, Gerardo J. Pacheco, Ramalingam Shanmugam, C. Scott Kruse, and Lawrence V. Fulton. 2020. "Obesity and Morbidity Risk in the U.S. Veteran" Healthcare 8, no. 3: 191. https://doi.org/10.3390/healthcare8030191
APA StyleBetancourt, J. A., Stigler Granados, P., Pacheco, G. J., Shanmugam, R., Kruse, C. S., & Fulton, L. V. (2020). Obesity and Morbidity Risk in the U.S. Veteran. Healthcare, 8(3), 191. https://doi.org/10.3390/healthcare8030191








