Perception of Patient Safety Culture in the Framework of the Psychosocial Care Network in Western Amazon: A Cross-Sectional Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Measurements
2.3. Statistical Analysis
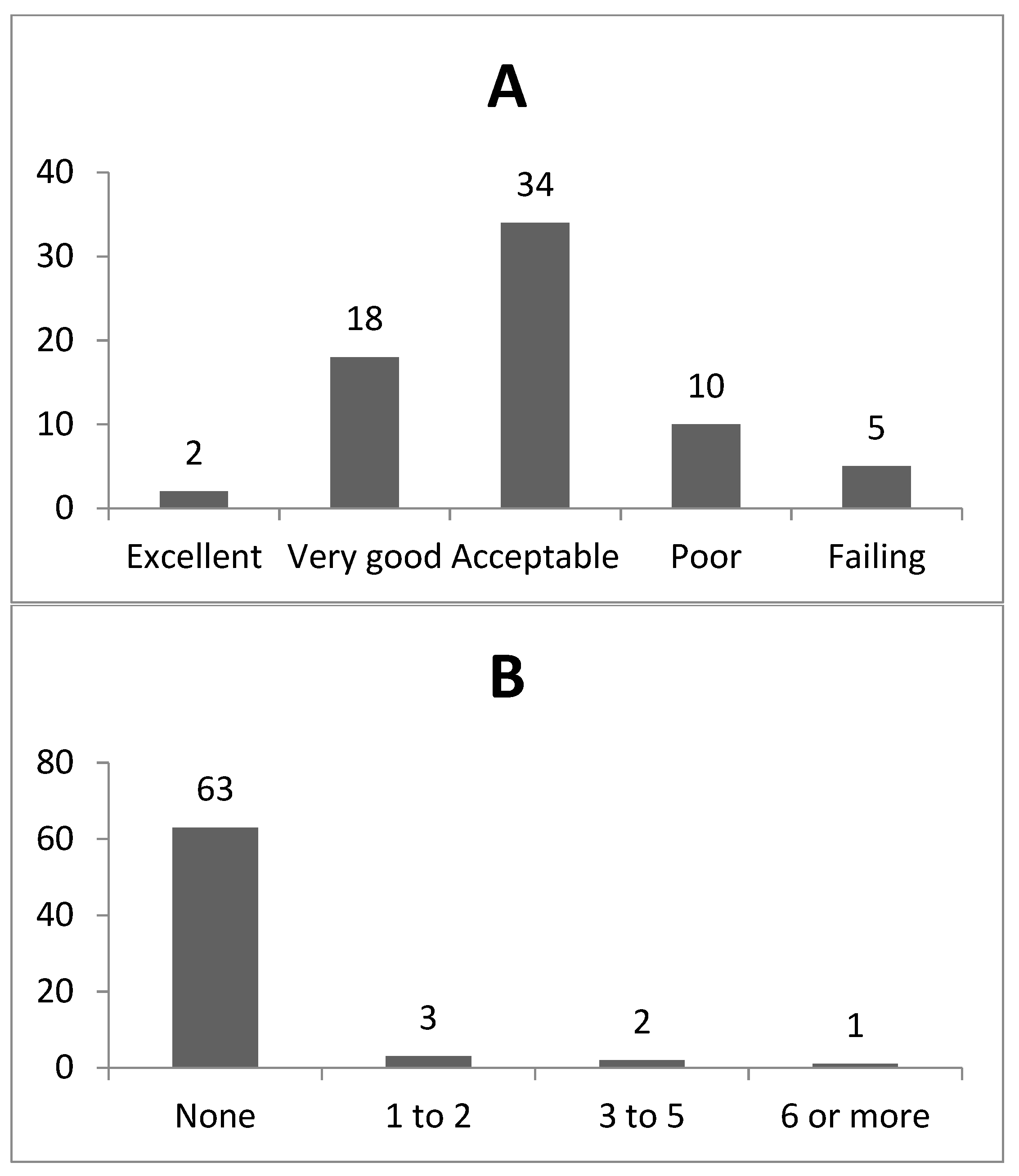
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Silva, N.D.; Barbosa, A.P.; Padilha, K.G.; Malik, A.M. Patient safety in organizational culture as perceived by leaderships of hospital institutions with different types of administration. Rev. Esc. Enfem. USP 2016, 50, 490–497. [Google Scholar] [CrossRef] [PubMed]
- Organización Mundial de la Salud. Marco Conceptual de la Clasificación Internacional para la Seguridad del Paciente; Organización Mundial de la Salud: Geneva, Switzerland, 2009; Versión 1.1. [Google Scholar]
- Anvisa (Brasil). Boletins Informativo—Segurança do Paciente e Qualidade em Serviços de Saúde; Aeroporto Internacional de Sau Paulo: Guarulhos, Brasil, 2013. [Google Scholar]
- Proqualis/Icict/Fiocruz. (s.d.). Centro Colaborador para a Qualidade do Cuidado e a Segurança do Paciente. Available online: http://proqualis.net/ (accessed on 5 May 2019).
- Abraão, S.R.; Bezerra, A.L.Q.; Branquinho, N.C.S.S.; Paranagua, T.T.B. Characterization motivation and satisfaction level of nursing technicians of a university hospital. Rev. Enferm. UERJ 2010, 18, 253–258. [Google Scholar]
- Filho, A.P.; Andrade, J.C.S.; Marinho, M.M.O. Culture e safety management: The proposal of a model. Gest. Prod. 2011, 18, 205–220. [Google Scholar]
- Reis, C.T.; Laguardia, J.; Martins, M. Adaptação transcultural da versão brasileira do Hospital Survey on Patient Safety Culture: Etapa inicial. Cad. Saúde Pública 2012, 28, 2199–2210. [Google Scholar] [CrossRef]
- Badhwar, V.; Rankin, J.S.; He, X.; Jacobs, J.P.; Gammie, J.S.; Furnary, A.P.; Fazzalari, F.L.; Han, J.; O’Brien, S.M.; Shahian, D.M. The Society of Thoracic Surgeons mitral repair/replacement composite score: A report of the Society of Thoracic Surgeons Quality Measurement Task Force. Ann. Thorac. Surg. 2016, 30, 2265–2271. [Google Scholar] [CrossRef]
- Burstin, H.; Leatherman, S.; Goldmann, D. The evolution of healthcare quality measurement in the United States. J. Int. Med. 2016, 279, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Martins, R.M. Investigação de Incidentes e Acidentes de Trabalho num Terminal Portuário. Ph.D. Thesis, Instituto Politécnico de Setúbal. Escola Superior de Ciências Empresariais, Setúbal, Portugal, 2017. [Google Scholar]
- Patterson, P.D.; Pfeiffer, A.J.; Weaver, M.D.; Krackhardt, D.; Arnold, R.M.; Yealy, D.M.; Lave, J.R. Network analysis of team communication in a busy emergency department. BMC Health Serv. Res. 2013, 13, 109. [Google Scholar] [CrossRef]
- Kiaei, M.Z.; Ziaee, A.; Mohebbifar, R.; Khoshtarkib, H.; Ghanati, E.; Ahmadzadeh, A.; Teymoori, S.; Khosravizadeh, O.; Zieaeeha, M. Patient safety culture in teaching hospitals in Iran: Assessment by the hospital survey on patient safety culture (HSOPSC). J. Health Inform. 2016, 3, 51–56. [Google Scholar]
- Rosen, A.K.; Loveland, S.; Shin, M.; Shwartz, M.; Hanchate, A.; Chen, Q.; Kaafarani, H.M.; Borzecki, A. Examining the impact of the AHRQ Patient Safety Indicators (PSIs) on the Veterans Health Administration: The case of readmissions. Med. Care 2013, 51, 37–44. [Google Scholar] [CrossRef]
- Sadeghi, B.; White, R.H.; Maynard, G.; Zrelak, P.; Strater, A.; Hensley, L.; Cerese, J.; Romano, P. Improved coding of postoperative deep vein thrombosis and pulmonary embolism in administrative data (AHRQ patient safety indicator 12) after introduction of new ICD-9-CM diagnosis codes. Med. Care 2015, 53, 37–40. [Google Scholar] [CrossRef]
- Mello, J.F. Cultura de Segurança do Paciente em Unidade de Terapia Intensiva: Perspectiva da Enfermagem. Master’s Thesis, Universidade Federal de Santa Catarina Florianópolis, Florianópolis, Brazil, 2011. [Google Scholar]
- Reis, C.T.; Laguardia, J.; Vasconcelos, A.G.G.; Martins, M. Reliability and validity of the Brazilian version of the Hospital Survey on Patient Safety Culture (HSOPSC): A pilot study. Cad. Saud Pub. 2016, 32, e00115614. [Google Scholar] [CrossRef] [PubMed]
- Sexton, J.B.; Helmreich, R.L.; Neilands, T.B.; Rowan, K.; Vella, K.; Boyden, J.; Roberts, P.R.; Thomas, E.J. The Safety Attitudes Questionnaire: Psychometric properties, benchmarking data, and emerging research. BMC Heal. Serv. Res. 2006, 6, 44. [Google Scholar] [CrossRef] [PubMed]
- Minuzzi, A.P.; Chiodelli, S.N.; Orlandi, H.L.M.; Nazareth, A.L.; Matos, E. Contribuições da equipe de saúde visando à promoção da segurança do paciente no cuidado intensivo. Esc. Anna Nery Rev. Enferm. 2016, 20, 121–129. [Google Scholar]
- Minuzz, A.P.; Salum, N.C.; Locks, M.O.H. Avaliação da cultura de segurança do paciente em terapia intensiva na perspectiva da equipe de saúde. Texto Contexto Enferm. 2016, 25, 161–169. [Google Scholar] [CrossRef][Green Version]
- Sorra, J.S.; Nieva, V. Hospital Survey on Patient Safety Culture: User’s Guide; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2014. [Google Scholar]
- Santos, K.O.B.; Carvalho, F.M.; Araújo, T.M. Internal consistency of the self-reporting questionnaire-20 in occupational groups. Rev. Saud. Pub. 2016, 50, 6. [Google Scholar] [CrossRef]
- Silva-Batalha, E.M.S.; Melleiro, M.M. Cultura de segurança do paciente em um hospital de ensino: Diferenças de percepção existentes nos diferentes cenários dessa instituição. Texto Contexto Enferm. 2015, 24, 432–441. [Google Scholar] [CrossRef]
- Tomazoni, A.; Rocha, P.K.; Kusahara, D.M.; de Souza, A.I.J.; Macedo, T.R. Avaliação da cultura de segurança do paciente em terapia intensiva neonatal. Texto Contexto Enferm. 2015, 24, 161–169. [Google Scholar] [CrossRef]
- Azimi, L.; Bahadori, M. The effect of Safety Culture Education on Improvement of Managers Attitudes towards Patients Safety. Int. J. Collab. Res. Intern. Med. Public Health 2012, 4, 217–226. [Google Scholar]
- Fermo, V.C.; Radünz, V.; Rosa, L.M.; Marinho, M.M. Cultura de segurança do paciente em unidade de Transplante de Medula Óssea. Rev. Bras. Enferm. 2015, 68, 1139–1146. [Google Scholar] [CrossRef]
- Kowalczuk, K.; Krajewska-Kułak, E.; Sobolewski, M. Factors determining work arduousness levels among nurses: Using the example of surgical, medical treatment, and emergency wards. Biomed Res. Int. 2019, 2019, 6303474. [Google Scholar] [CrossRef]
- Müller, M.A.M.; Dall’Agnol, C.M.; Beryl, M.P. Carga de trabalho da equipe de enfermagem e segurança do paciente-estudo com método misto na abordagem ecológica restaurativa. Rev. Latino Am. Enferm. 2013, 21. [Google Scholar] [CrossRef]
- Duarte, S.D.; Stipp, M.A.; da Silva, M.M.; de Oliveira, F.T. Eventos adversos e segurança na assistência de enfermagem. Rev. Bras. Enferm. 2015, 68, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Somensen, C.B.; Duran, E.C.M. Fatores higiênicos e motivacionais do trabalho do enfermeiro em enfermaria de cardiologia. Rev. Gaúcha Enferm. 2014, 35, 82–89. [Google Scholar]
- Rigobello, M.C.; Carvalho, R.E.; Cassiani, S.H.; Galon, T.; Capucho, H.C.; Deus, N.N. The climate of patient safety: Perception of nursing professionals. Acta Paul Enferm. 2012, 25, 728–735. [Google Scholar] [CrossRef]
- Silva, C.M.; Barroso, F.F. Promover uma cultura de segurança em cuidados de saúde primários. Rev. Port. Saud Pub. 2014, 31, 197–205. [Google Scholar]
- Andrade, L.E. Evolução da Cultura de Segurança em Hospitais antes e após a Implantação do Programa Nacional de Segurança do Paciente. Master’s Thesis, Universidade Federal do Rio Grande do Norte, Natal, Brazil, 2016. [Google Scholar]
- Rodrigues, M.C.; Guerreiro, M.O. Cultura de segurança: A percepção dos profissionais de enfermagem intensivistas. Enferm. Glob. 2016, 15, 208–219. [Google Scholar]
- Abdou, H.A.; Saber, K.M.M. A baseline assessment of patient safety culture among nurses at student university hospital. World J. Med. Sci. 2011, 6, 7–26. [Google Scholar]
- Barbosa, M.H.; Sousa, E.M.; Félix, M.M.S.; Oliveira, K.F.; Barichello, E. Clima de segurança do paciente em um hospital especializado em oncologia. Rev. Eletrôn. Enferm. 2016, 17, 1–9. [Google Scholar]
- Carvalho, P.A.; Göttems, L.B.D.; Pires, M.R.G.M.; Oliveira, M.L.C.D.E. Safety culture in the operating room of a public hospital in the perception of healthcare professionals. Rev. Latino Am. Enferm 2015, 23, 1041–1048. [Google Scholar] [CrossRef]
- Alves, S.R.; dos Santos, R.P.; Gimenes, R.M.; Yamaguchi, M.U. Sobrecarga de trabalho da Enfermagem em saúde mental. Rev. Rene 2016, 17, 684–690. [Google Scholar] [CrossRef]
- Claro, C.M.; Krocockz, D.V.; Toffolleto, M.C.; Padilha, K.G. Adverse events at the Intensive Care Unit: Nurses’ perception about the culture of no-punishment. Rev. Esc. Enferm USP 2011, 45, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Silva, G.M.; Lima, M.V.M.; Araripe, M.C.; Vasconcelos, S.P.; Opitz, S.P.; Laporta, G.Z. Evaluation of the Patient Safety Culture in the Western Amazon. J. Hum. Growth Dev. 2018, 28, 307–315. [Google Scholar] [CrossRef][Green Version]
- Huang, C.-H.; Wu, H.-H.; Lee, Y.-C. The perceptions of patient safety culture: A difference between physicians and nurses in Taiwan. Appl. Nurs. Res. 2017, 40, 39–44. [Google Scholar] [CrossRef] [PubMed]
| Variables | N | % |
|---|---|---|
| Area/Work Unit | ||
| Ambulatory of Mental Health | 42 | 60.9 |
| Emergency Sector | 03 | 4.3 |
| Pharmacy | 03 | 4.3 |
| Others | 20 | 29.0 |
| Total | 69 | 100.0 |
| Office or function | ||
| Nursing technicians | 26 | 37.7 |
| Nurse | 09 | 13.0 |
| Physiotherapy | 06 | 8.7 |
| Psychologist | 02 | 2.9 |
| Pharmacist/Biochemist/Biomedical | 01 | 1.4 |
| Nutritionist | 01 | 1.4 |
| Other categories | 06 | 8.7 |
| No reply | 18 | 26.1 |
| Total | 69 | 100.0 |
| Network Location | ||
| Acre Mental Health Hospital (HOSMAC) | 62 | 89.9 |
| Center for Psychosocial Care (CAPS AD III) | 07 | 10.1 |
| Total | 69 | 100.0 |
| Interaction with patients | ||
| YES, I usually have interaction or direct contact with patients. | 55 | 79.0 |
| I DO NOT have interaction or direct contact with patients. | 14 | 21.0 |
| Total | 69 | 100 |
| Time working in the hospital (Years) | ||
| Less than 1 year | 06 | 8.7 |
| 1 to 5 years | 22 | 31.9 |
| 6 to 10 years | 16 | 23.2 |
| 11 to 15 years | 05 | 7.2 |
| 16 to 20 years | 05 | 7.2 |
| 21 years and over | 15 | 21.7 |
| Total | 69 | 69 |
| Time working in the current area/unit of the hospital (Years) | ||
| Less than 1 year | 04 | 5.8 |
| 1 to 5 years | 22 | 31.9 |
| 6 to 10 years | 19 | 27.5 |
| 11 to 15 years | 05 | 7.2 |
| 16 to 20 years | 11 | 15.9 |
| 21 years and over | 08 | 11.6 |
| Total | 69 | 100.0 |
| Working Hours per Week (Hours) | ||
| Less than 20 h per week | 01 | 1.4 |
| 20 to 39 h per week | 31 | 44.9 |
| 40 to 59 h per week | 25 | 36.2 |
| 60 to 79 h per week | 09 | 13.0 |
| No reply | 03 | 4.3 |
| Total | 69 | 100.0 |
| Time working on your Current Specialty (Years) | ||
| Less than 1 year | 03 | 4.3 |
| 1 to 5 years | 14 | 20.3 |
| 6 to 10 years | 19 | 27.5 |
| 11 to 15 years | 09 | 13.0 |
| 16 to 20 years | 07 | 10.1 |
| 21 years and over | 16 | 23.2 |
| No reply | 01 | 1.4 |
| Total | 69 | 100.0 |
| Patient Safety Dimensions Rate of Positive Responses (%) | Rate of Positive Responses (%) |
|---|---|
| Expectations and actions to promote the safety of supervisors and managers | 75 |
| Hospital management support for patient safety | 64 |
| Internal Transfers and Work Placement | 56 |
| Communication opening | 52 |
| Organizational learning | 51 |
| Teamwork within the units | 49 |
| Teamwork between units | 49 |
| Frequency of Reported Events | 48 |
| Feedback and Communication About Errors | 43 |
| Staffing | 38 |
| General Perceptions of Patient Safety | 35 |
| Non-punitive responses to errors | 27 |
| Factors (Items) | Cronbach’s Alpha | Silva-Batalha and Mellerio [22] | Reis et al. [16] | Tomazoni et al. [23] |
|---|---|---|---|---|
| All items from HSOPSC | 0.86 | 0.90 | - | - |
| Frequency of related events (D1, D2, D3) | 0.89 | 0.87 | 0.91 | 0.88 |
| Expectations and actions to promote the safety of supervisors and managers (B1, B2, B3R, B4R) | 0.65 | 0.77 | 0.76 | 0.74 |
| Feedback and communication about errors (C1, C3, C5) | 0.77 | 0.67 | 0.72 | 0.72 |
| Teamwork within the units (A1, A3, A4, A11) | 0.68 | 0.68 | 0.66 | 0.61 |
| Communication opening (C2, C4, C6R) | 0.79 | 0.63 | 0.69 | 0.64 |
| Hospital management support for patient safety (F1, F8, F9R) | 0.79 | 0.72 | 0.84 | 0.60 |
| Internal transfers and tickets on duty (F3R, F5R, F7R, F11R) | 0.58 | 0.70 | 0.70 | 0.64 |
| Non-punitive responses to errors (A8R, A12R, A16R) | 0.10 | 0.40 | 0.35 | 0.47 |
| Organizational learning (A6, A9, A13) | 0.53 | 0.60 | 0.56 | 0.74 |
| Teamwork between hospital units (F2R, F4, F6R, F10) | 0.53 | 0.56 | 0.67 | 0.60 |
| General safety perceptions (A10R, A15, A17R, A18R) | - | 0.47 | 0.52 | 0.43 |
| Staffing (A2, A5R, A7R, A14R) | 0.12 | 0.66 | 0.20 | 0.46 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Araripe, M.C.; Silva, G.M.; de Lima, M.V.M.; Bezerra, Í.M.P.; de Melo, W.A.L.; Laporta, G.Z. Perception of Patient Safety Culture in the Framework of the Psychosocial Care Network in Western Amazon: A Cross-Sectional Study. Healthcare 2020, 8, 289. https://doi.org/10.3390/healthcare8030289
Araripe MC, Silva GM, de Lima MVM, Bezerra ÍMP, de Melo WAL, Laporta GZ. Perception of Patient Safety Culture in the Framework of the Psychosocial Care Network in Western Amazon: A Cross-Sectional Study. Healthcare. 2020; 8(3):289. https://doi.org/10.3390/healthcare8030289
Chicago/Turabian StyleAraripe, Marcos Cordeiro, Glauco Martins Silva, Marcos Venicius Malveira de Lima, Ítalla Maria Pinheiro Bezerra, Walédya Araújo Lopes de Melo, and Gabriel Zorello Laporta. 2020. "Perception of Patient Safety Culture in the Framework of the Psychosocial Care Network in Western Amazon: A Cross-Sectional Study" Healthcare 8, no. 3: 289. https://doi.org/10.3390/healthcare8030289
APA StyleAraripe, M. C., Silva, G. M., de Lima, M. V. M., Bezerra, Í. M. P., de Melo, W. A. L., & Laporta, G. Z. (2020). Perception of Patient Safety Culture in the Framework of the Psychosocial Care Network in Western Amazon: A Cross-Sectional Study. Healthcare, 8(3), 289. https://doi.org/10.3390/healthcare8030289






