Autopsy Findings in Case of Fatal Scorpion Sting: A Systematic Review of the Literature
Abstract
1. Introduction
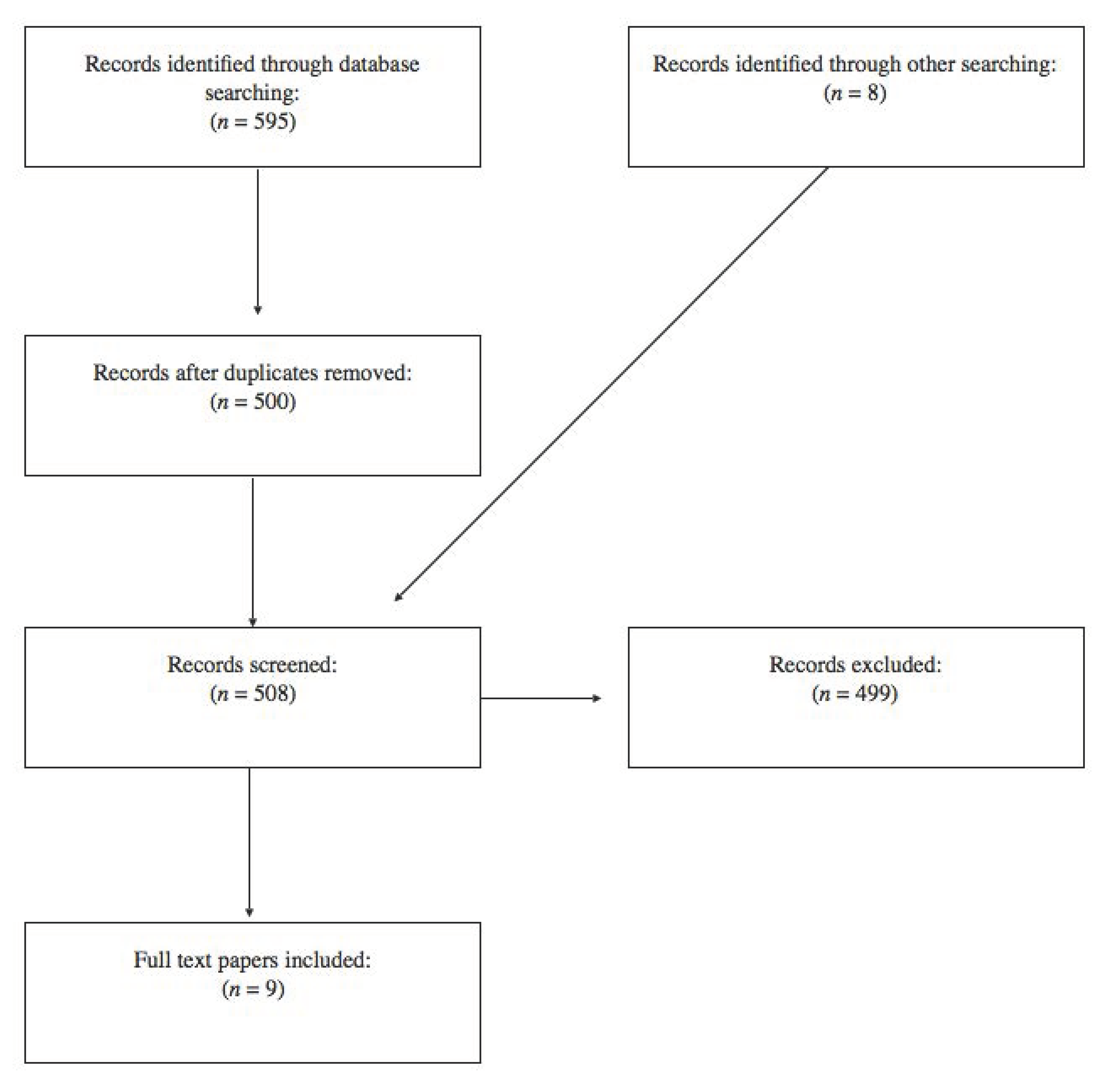
2. Materials and Method
2.1. Literature Search
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
3. Results
3.1. Characteristics of Eligible Studies
3.2. Epidemiological Findings
3.3. Autopsy Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Abd El-Aziz, F.E.A.; El Shehaby, D.M.; Elghazally, S.A.; Hetta, H.F. Toxicological and epidemiological studies of scorpion sting cases and morphological characterization of scorpions (Leiurusquin questriatus and Androctonus crassicauda) in Luxor, Egypt. Toxicol. Rep. 2019, 6, 329–335. [Google Scholar] [CrossRef]
- Silva-Domínguez, R.; Paredes-Solís, S.; Cortés-Guzmán, A.J.; Flores-Moreno, M.; Baldazo-Monsivaiz, J.G.; Anderson, N.; Cockcroft, A. Factors associated with scorpion stings in schoolchildren: Cross-sectional study from two rural communities of Guerrero, Mexico. Bol. Med. Hosp. Infant. Mex. 2019, 76, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Furtado, A.A.; Daniele-Silva, A.; Silva-Júnior, A.A.D.; Fernandes-Pedrosa, M.F. Biology, venom composition, and scorpionism induced by brazilian scorpion Tityus stigmurus (Thorell, 1876) (Scorpiones: Buthidae): A mini-review. Toxicon. 2020, 185, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Firoozfar, F.; Saghafipour, A.; Jesri, N. Scorpions and Their Human Mortality Report in Iran: A Review Article. Iran J. Public Health. 2019, 48, 2140–2153. [Google Scholar] [PubMed]
- de Araújo, K.A.M.; Tavares, A.V.; Marques, M.R.V.; Vieira, A.A.; Leite, R.S. Epidemiological study of scorpion stings in the Rio Grande do Norte State, Northeastern Brazil. Rev. Inst. Med. Trop. Sao Paulo. 2017, 59, e58. [Google Scholar] [CrossRef]
- Rafizadeh, S.; Rafinejad, J.; Rassi, Y. Epidemiology of Scorpionism in Iran during 2009. J. Arthropod Borne Dis. 2013, 7, 66–70. [Google Scholar]
- Borges, A.; Morales, M.; Loor, W.; Delgado, M. Scorpionism in Ecuador: First report of severe and fatal envenoming cases from northern Manabí by Tityus asthenes Pocock. Toxicon 2015, 105, 56–61. [Google Scholar] [CrossRef]
- Queiroz, A.M.; Sampaio, V.S.; Mendonça, I.; Fé, N.F.; Sachett, J.; Ferreira, L.C.; Feitosa, E.; Wen, F.H.; Lacerda, M.; Monteiro, W. Severity of Scorpion Stings in the Western Brazilian Amazon: A Case-Control Study. PLoS ONE 2015, 10, e0128819. [Google Scholar] [CrossRef]
- Chakroun-Walha, O.; Karray, R.; Jerbi, M.; Nasri, A.; Issaoui, F.; Amine, B.R.; Bahloul, M.; Buaziz, M.; Ksibi, H.; Rekik, N. Update on the Epidemiology of Scorpion Envenomation in the South of Tunisia. Wilderness Environ. Med. 2018, 29, 29–35. [Google Scholar] [CrossRef]
- LoVecchio, F.; McBride, C. Scorpion envenomations in young children in central Arizona. J. Toxicol. Clin. Toxicol. 2003, 41, 937–940. [Google Scholar] [CrossRef]
- Santos, M.S.V.; Silva, C.G.L.; Neto, B.S.; Grangeiro Júnior, C.R.P.; Lopes, V.H.; Teixeira Júnior, A.G.; Bezerra, D.A.; Luna, J.V.; Cordeiro, J.B.; Júnior, J.G.; et al. Clinical and epidemiological aspects of scorpionism in the world: A systematic review. Wilderness Environ. Med. 2016, 27, 504–518. [Google Scholar] [CrossRef] [PubMed]
- Chippaux, J.P.; Goyffon, M. Epidemiology of scorpionism: A global appraisal. Acta Trop. 2008, 107, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Bahloul, M.; Chabchoub, I.; Chaari, A.; Chtara, K.; Kallel, H.; Dammak, H.; Ksibi, H.; Chelly, H.; Rekik, N.; Ben Hamida, C.; et al. Scorpion envenomation among children: Clinical manifestations and outcome (analysis of 685 cases). Am. J. Trop. Med. Hyg. 2010, 83, 1084–1092. [Google Scholar] [CrossRef]
- Dudin, A.A.; Rambaud-Cousson, A.; Thalji, A.; Juabeh, I.I.; Abu-Libdeh, B. Scorpion sting in children in the Jerusalem area: A review of 54 cases. Ann. Trop. Paediatr. 1991, 11, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Vazirianzadeh, B.; Farhadpour, F.; Hosseinzadeh, M.; Zarean, M.; Moravvej, S. An epidemiological and clinical study on scorpionism in hospitalized children in khuzestan, iran. J. Arthropod. Borne Dis. 2012, 6, 62–69. [Google Scholar]
- Baseer, K.A.; Naser, M.A.A. Predictors for Mortality in Children with Scorpion Envenomation Admitted to Pediatric Intensive Care Unit, Qena Governorate, Egypt. Am. J. Trop. Med. Hyg. 2019, 101, 941–945. [Google Scholar] [CrossRef]
- LoVecchio, F. Scorpion Envenomation Causing Neuromuscular Toxicity (United States, Mexico, Central America, and Southern Africa). Available online: https://www.uptodate.com/contents/scorpion-envenomation-causing-neuromuscular-toxicity-united-states-mexico-central-america-and-southern-africa?search=scorpion&source=search_result&selectedTitle=1~18&usage_type=default&display_rank=1 (accessed on 2 September 2020).
- Ward, M.J.; Ellsworth, S.A.; Nystrom, G.S. A global accounting of medically significant scorpions: Epidemiology, major toxins, and comparative resources in harmless counterparts. Toxicon 2018, 151, 137–155. [Google Scholar] [CrossRef]
- Marks, C.J.; Muller, G.J.; Sachno, D.; Reuter, H.; Wium, C.A.; Du Plessis, C.E.; Van Hoving, D.J. The epidemiology and severity of scorpion envenoming in South Africa as managed by the Tygerberg Poisons Information Centre over a 10 year period. Afr. J. Emerg. Med. 2019, 9, 21–24. [Google Scholar] [CrossRef]
- Mullen, G.R.; Durden, L.A. Medical and Veterinary Entomology, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Shamoon, Z.; Peterfy, R.J.; Hammoud, S.; Khazaeni, B. Scorpion Toxicity; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Naseem, S.; Altamemi, S.; Ullah, I. Scorpion sting envenomstion or anaphylaxis? Report of a child with overlapping cilinical picture following scorpion sting. Arch. Dis. Child. 2016, 101, A44. [Google Scholar] [CrossRef]
- Castillo, A.; Attaluri, P. Acute respiratory failure following scorpion stings: Anaphylaxis or severe systemic envenomation? Southwest Respir. Crit. Care Chronicles. 2018, 6, 47–50. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzla, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Amaral, C.F.; de Rezende, N.A.; Freire-Maia, L. Acute pulmonary edema after Tityus serrulatus scorpion sting in children. Am. J. Cardiol. 1993, 71, 242–245. [Google Scholar] [CrossRef]
- Amaral, C.F.; Barbosa, A.J.; Leite, V.H.; Tafuri, W.L.; de Rezende, N.A. Scorpion sting-induced pulmonary oedema: Evidence of increased alveolocapillary membrane permeability. Toxicon 1994, 32, 999–1003. [Google Scholar] [CrossRef]
- Cupo, P.; Jurca, M.; Azevedo-Marques, M.M.; Oliveira, J.S.M.; Hering, S.E. Severe scorpion envenomation in Brazil: Clinical, laboratory and anatomopathological aspects. Rev. Inst. Med. trop. S. Paulo. 1994, 36, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Badhe, B.; Kumar Shaha, K.; Manickam, N.; Manigandan, G. Fatal Scorpion Envenomation: Report of Two Cases. J. Indian Acad. Forensic Med. 2013, 35, 404–407. [Google Scholar]
- Kaya, K.; Topataş, F.; Çekin, N.; Gülmen, M.K.; Akgündüz, E. A death after scorpion envenoming: ARDS. Int. Clin. Pathol. J. 2018, 6, 3–4. [Google Scholar] [CrossRef][Green Version]
- Kumar, L.; Naik, S.K.; Agarwal, S.S.; Bastia, B.K. Autopsy diagnosis of a death due to scorpion stinging-a case report. J. Forensic Leg. Med. 2012, 19, 494–496. [Google Scholar] [CrossRef] [PubMed]
- Mahamuni, N.M.; Patne, S.S.; Gadgil, P.A.; Pandit, G.A. Autopsy Case Findings in Fatal Scorpion Bite. Int. J. Eng. Sci. 2017, 6, 1145–1147. [Google Scholar]
- Melo, I.M.L.A.; Ramalho, R.D.; Bezerra, M.M.V.; de Oliveira Filho, I.E.; Medeiros, C.R.; da Costa Gadelha, M.A.; Pereira de Oliveira Pardal, P. Fatal anaphylaxis to Jaguajir rochae (borelli, 1910) (Scorpiones, Buthidae) in Brazil: A case report. J. Trop. path. 2019, 48, 1–8. [Google Scholar]
- Patil, A.; Jatti, V.; Shashikala, P.; Dileep Kumar, R.; Pravinkumar, N.K. Fatal Anaphylactic Shock Following Scorpion Sting Envenomation. J. Karnataka Med. Leg. Soc. 2017, 26, 32–34. [Google Scholar]
- Isbister, G.K.; Bawaskar, H.S. Scorpion envenomation. N. Engl. J. Med. 2014, 371, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Khattabi, A.; Soulaymani-Bencheikh, R.; Achour, S.; Salmi, L.R. Scorpion Consensus Expert Group. Classification of clinical consequences of scorpion stings: Consensus development. Trans. R. Soc. Trop. Med. Hyg. 2011, 105, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Amaral, C.F.; Rezende, N.A. Both cardiogenic and non-cardiogenic factors are involved in the pathogenesis of pulmonary oedema after scorpion envenoming. Toxicon 1997, 35, 997–998. [Google Scholar] [CrossRef]
- Agrawal, A.; Kumar, A.; Consul, S.; Yadav, A. Scorpion bite, a sting to the heart! Indian J. Crit. Care Med. 2015, 19, 233–236. [Google Scholar]
- Rahav, G.; Weiss, A.T. Scorpion sting-induced pulmonary edema. Scintigraphic evidence of cardiac dysfunction. Chest 1990, 97, 1478–1480. [Google Scholar] [CrossRef]
- Bahloul, M.; Kallel, H.; Rekik, N.; Ben Hamida, C.; Chelly, H.; Bouaziz, M. Cardiovascular dysfunction following severe scorpion envenomation. Mechanisms and physiopathology. Presse Med. 2005, 34, 115–120. [Google Scholar] [CrossRef]
- Valdivia, H.H.; Kirby, M.S.; Lederer, W.J.; Coronado, R. Scorpion toxins targeted against the sarcoplasmic reticulum Ca (2+)-release channel of skeletal and cardiac muscle. Proc. Natl. Acad. Sci. USA 1992, 89, 12185–12189. [Google Scholar] [CrossRef]
- Bawaskar, H.S.; Bawaskar, P.H. Management of scorpion sting. Heart 1999, 82, 253–254. [Google Scholar] [CrossRef]
- Clark, S.B.; Soos, M.P. Noncardiogenic Pulmonary Edema; StatPearls: Treasure Island, FL, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK542230/ (accessed on 5 September 2020).
- Dobbe, L.; Rahman, R.; Elmassry, M.; Paz, P.; Nugent, K. Cardiogenic Pulmonary Edema. Am. J. Med. Sci. 2019, 358, 389–397. [Google Scholar] [CrossRef]
- Chippaux, J.P. Emerging options for the management of scorpion stings. Drug. Des. Devel. Ther. 2012, 6, 165–173. [Google Scholar] [CrossRef]
- Maheshwari, M.; Tanwar, C.P. Scorpion bite induced myocardial damage and pulmonary edema. Heart Views. 2012, 13, 16–18. [Google Scholar] [CrossRef] [PubMed]
- Bahloul, M.; Chaari, A.; Dammak, H.; Samet, M.; Chtara, K.; Chelly, H.; Ben Hamida, C.; Kallel, H.; Bouaziz, M. Pulmonary edema following scorpion envenomation: Mechanisms, clinical manifestations, diagnosis and treatment. Int. J. Cardiol. 2013, 162, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Dokur, M.; Dogan, M.; Yagmur, E.A. Scorpion-related cardiomyopathy and acute pulmonary edema in a child who is stung by Leiurus abdullahbayrami. Turk. J. Emerg. Med. 2017, 17, 104–108. [Google Scholar] [CrossRef] [PubMed]
- LoVecchio, F. Scorpion Envenomation Causing Autonomic Dysfunction (North Africa, Middle East, Asia, South America, and the Republic of Trinidad and Tobago). Available online: https://www.uptodate.com/contents/scorpion-envenomation-causing-autonomic-dysfunction-north-africa-middle-east-asia-south-america-and-the-republic-of-trinidad-and-tobago?source=history_widget#H2423052929 (accessed on 14 August 2020).
- Muller, G.J.; Modler, H.; Wium, C.A.; Veale, D.J.H. Scorpion sting in southern Africa: Diagnosis and management. Contin. Med. Educ. 2012, 30, 356–361. [Google Scholar]
- Insects and Scorpions. Available online: https://www.cdc.gov/niosh/topics/insects/scorpions.html (accessed on 2 September 2020).
| Reference | Country | Scorpion | Age/Sex of the Victim | Time Interval Sting–Death | Site of the Sting | Autopsy Findings |
|---|---|---|---|---|---|---|
| Amaral CSF et al., 1993 [25] | Brazil | Tityus Serrulatus | 3/M | 57 h | n.a. | H: dilatated RV. Diffuse engorgement of the myocardial vessels and mild interstitial edema L: congested, edematous and stiffened, showing scattered areas of subpleural emphysema, septal thickening, diffuse alveolar edema with prominent hyaline membrane, mononuclear cell infiltration and areas of alveolar collapse |
| Amaral CSF et al., 1994 [26] | Brazil | Tityus Serrulatus | 16/M | 32 h | Left Hand | Sampled just the right lung congestion of the alveolar capillaries, widening of the interstitial spaces, focal areas of intra-alveolar edema with marked PMNs infiltration and prominent hyaline membranes lining small bronchioles and alveolar epithelium surface |
| Cupo P et al., 1994 [27] | Brazil | Tityus Serrulatus | 5/F | 17 h | Right Supraclavicular Region | B: edema, H: dilatated, pale aspect of the pectineal muscles. Interstitial edema with a moderate inflammatory infiltrate consisting of neutrophilic and some eosinophilic cells. L: ↑volume, diffuse alveolar edema and hemorrhage and polymorphonuclear infiltrate P, Li, I: unremarkable |
| Cupo P et al., 1994 [27] | Brazil | Yellow Scorpion | 4/M | 13 h | Sternal region | B: edema. H: enlarged RV L: ↑volume, ↑ consistency, proteinaceous and amorphous material and most intermingled with confluent erythrocytes in the alveoli P, Li, AG: unremarkable |
| Cupo P et al., 1994 [27] | Brazil | Tityus Serrulatus | 4/M | 15 h | Hand | B: edema and congestion H: no macroscopic changes. Focal subepicardial hemorrhage. Myocytolysis and unstructured fibrillar cytoplasmic architecture turning into an amorphous eosinophilic mass. PMNs infiltrate around the papillary muscles. L: ↑volume, intense alveolar edema and septal congestion P, Li, I: unremarkable |
| Das S et al., 2013 [28] | India | n.a. | 16/F | n.a. but >24 h | Left Foot. An area (2 × 1 cm) of the skin thickened, indurated and pigmented. Normal subcutaneous. Evidence of hyperkeratosis | Blood stained secretions in the lumen of the larynx and trachea L: heavy, congestion K: congestion Li, H: unremarkable |
| Das S et al., 2013 [28] | India | n.a. | 38/F | n.a. | Right Foot Area of thickening and pigmentation (4 × 3 cm) with hemorrhagic marks. Hemorrhagic aspect of the subcutaneous. | L: congestion with multiple petechial hemorrhages and edema H: edema between the myocytes K: congestion P: unremarkable |
| Kaya K et al., 2018 [29] | Turkey | n.a. | 5/M | n.a. but >14 h | n.a. | L: edema, atelectasis, hyaline membranes and hemosiderin-loaded macrophages (ARDS); Li, K, S, H, B, T: congestion |
| Kumar L et al., 2012 [30] | India | n.a. | 8/M | 48 h | Right Foot. Small abrasions over the foot, and no edema or redness. | H: dilatated chambers. Pale in aspect. Lymphocyte infiltrate around the papillary muscles. Myocytolysis (vacuolar degeneration), wavy fibers and focal hyalinization L: liver-like consistency and congestion. Alveoli were filled with homogeneous eosinophilic proteinaceous material P: parenchymal necrosis accompanied by interstitial hemorrhage K: congestion |
| Mahamuni NM et al., 2016 [31] | India | n.a. | 4/M | <24 h | Left Foot. Thickening and pigmentation of the skin (1 × 1cm) at the base of the left little toe. | B, L: petechial hemorrhages, edema and congestion H:LA mononuclear cell infiltration in cardiomyocytes with myocytolysis K: necrosis of tubular epithelium Congestion of all other organs |
| Melo IMLA et al., 2019 [32] | Brazil | Jaguajir Rochae | 44/M | n.a. | n.a. | glottal and lung edema |
| Patil A et al., 2017 [33] | India | n.a. | 12/F | 40 h | Left Hand. A dark-brown discoloration and swelling area (1.5 × 1 cm) with a punctured wound mark (0.2 × 0.2 cm) inside thick laminated keratin with unremarkable epidermis and upper dermal congestion | diffuse congestion St, K: congestion and hemorrhagic spots. L: edema, hemosiderin-laden macrophages with focal destruction of alveoli H: edema and pericardial infiltration of lymphocytes. Li: unremarkable |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feola, A.; Perrone, M.A.; Piscopo, A.; Casella, F.; Della Pietra, B.; Di Mizio, G. Autopsy Findings in Case of Fatal Scorpion Sting: A Systematic Review of the Literature. Healthcare 2020, 8, 325. https://doi.org/10.3390/healthcare8030325
Feola A, Perrone MA, Piscopo A, Casella F, Della Pietra B, Di Mizio G. Autopsy Findings in Case of Fatal Scorpion Sting: A Systematic Review of the Literature. Healthcare. 2020; 8(3):325. https://doi.org/10.3390/healthcare8030325
Chicago/Turabian StyleFeola, Alessandro, Marco Alfonso Perrone, Amalia Piscopo, Filomena Casella, Bruno Della Pietra, and Giulio Di Mizio. 2020. "Autopsy Findings in Case of Fatal Scorpion Sting: A Systematic Review of the Literature" Healthcare 8, no. 3: 325. https://doi.org/10.3390/healthcare8030325
APA StyleFeola, A., Perrone, M. A., Piscopo, A., Casella, F., Della Pietra, B., & Di Mizio, G. (2020). Autopsy Findings in Case of Fatal Scorpion Sting: A Systematic Review of the Literature. Healthcare, 8(3), 325. https://doi.org/10.3390/healthcare8030325









