The Association between Health Literacy and Gait Speed in Community-Dwelling Older Adults
Abstract
:1. Introduction
2. Materials and Methods
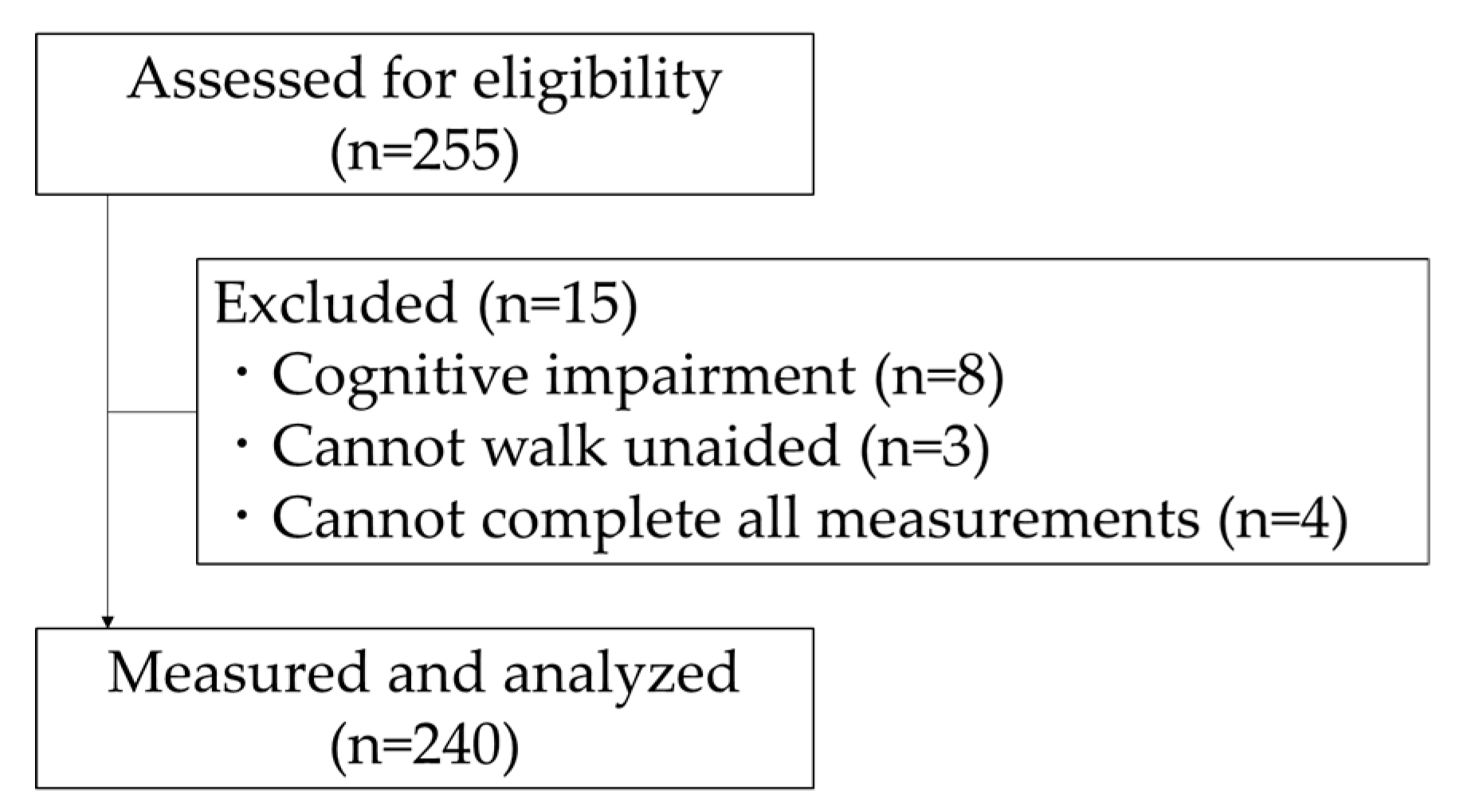
2.1. Subjects
2.2. Data Collection
2.2.1. Basic Attributes
2.2.2. Gait Speed
2.2.3. Health Literacy
2.2.4. Physical and Cognitive Function
2.3. Statistical Analysis
- -
- Model 1. Independent variable was health literacy only.
- -
- Model 2. Independent variables were model 1 plus age, gender, and height.
- -
- Model 3. Independent variables were model 2 plus CS-30 and TMT-A.
- -
- Model 4. Independent variables were model 2 plus Knee extension strength and TMT-A.
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lauretani, F.; Russo, C.R.; Bandinelli, S.; Bartali, B.; Cavazzini, C.; Di Iorio, A.; Corsi, A.M.; Rantanen, T.; Guralnik, J.M.; Ferrucci, L. Age-associated changes in skeletal muscles and their effect on mobility: An operational diagnosis of sarcopenia. J. Appl. Physiol. 2003, 95, 1851–1860. [Google Scholar] [CrossRef] [PubMed]
- Quach, L.; Galica, A.M.; Jones, R.N.; Procter-Gray, E.; Manor, B.; Hannan, M.T.; Lipsitz, L.A. The nonlinear relationship between gait speed and falls: The maintenance of balance, independent living, intellect, and zest in the elderly of boston study. J. Am. Geriatr. Soc. 2011, 59, 1069–1073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Brach, J.; Chandler, J.; Cawthon, P.; Connor, E.B.; et al. Gait speed surviv older adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. Age-related differences in walking stability. Age Ageing 2003, 32, 137–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perez-Sousa, M.A.; Venegas-Sanabria, L.C.; Chavarro-Carvajal, D.A.; Cano-Gutierrez, C.A.; Izquierdo, M.; Correa-Bautista, J.E.; Ramirez-Velez, R. Gait speed as a mediator of the effect of sarcopenia on dependency in activities of daily living. J. Cachexia Sarcopenia Muscle 2019, 10, 1009–1015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haider, S.; Luger, E.; Kapan, A.; Titze, S.; Lackinger, C.; Schindler, K.E.; Dorner, T.E. Associations between daily physical activity, handgrip strength, muscle mass, physical performance and quality of life in prefrail and frail community-dwelling older adults. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehab. 2016, 25, 3129–3138. [Google Scholar] [CrossRef] [Green Version]
- Oh, B.; Cho, B.; Choi, H.C.; Son, K.Y.; Park, S.M.; Chun, S.; Cho, S.I. The influence of lower-extremity function in elderly individuals’ quality of life (QOL): An analysis of the correlation between SPPB and EQ-5D. Arch. Gerontol. Geriatr. 2014, 58, 278–282. [Google Scholar] [CrossRef]
- Chou, C.H.; Hwang, C.L.; Wu, Y.T. Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: A meta-analysis. Arc. Phys. Med. Rehab. 2012, 93, 237–244. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Schapira, M.; Soriano, E.R.; Varela, M.; Kaplan, R.; Camera, L.A.; Mayorga, L.M. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J. Gerontol. Ser. A Biol. Sci. Med Sci. 2005, 60, 1304–1309. [Google Scholar] [CrossRef] [Green Version]
- Karpman, C.; DePew, Z.S.; LeBrasseur, N.K.; Novotny, P.J.; Benzo, R.P. Determinants of gait speed in COPD. Chest 2014, 146, 104–110. [Google Scholar] [CrossRef] [Green Version]
- Iwakura, M.; Okura, K.; Shibata, K.; Kawagoshi, A.; Sugawara, K.; Takahashi, H.; Shioya, T.; Wakasa, M. Gait characteristics and their associations with clinical outcomes in patients with chronic obstructive pulmonary disease. Gait Posture 2019, 74, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Bousquet, J.; Dinh-Xuan, A.T.; Similowski, T.; Malva, J.; Ankri, J.; Barbagallo, M.; Fabbri, L.; Humbert, M.; Mercier, J.; Robalo-Cordeiro, C.; et al. Should we use gait speed in COPD, FEV1 in frailty and dyspnoea in both? Eur. Respir. J. 2016, 48, 315–319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Figueiredo, P.; Ribeiro, P.A.; Bona, R.L.; Peyre-Tartaruga, L.A.; Ribeiro, J.P. Ventilatory determinants of self-selected walking speed in chronic heart failure. Med. Sci. Sports Exerc. 2013, 45, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.L.; Rosano, C.; Boudreau, R.M.; Simonsick, E.M.; Ferrucci, L.; Sutton-Tyrrell, K.; Hardy, S.E.; Atkinson, H.H.; Yaffe, K.; Satterfield, S.; et al. Executive function, memory, and gait speed decline in well-functioning older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2010, 65, 1093–1100. [Google Scholar] [CrossRef] [Green Version]
- Lundin-Olsson, L.; Nyberg, L.; Gustafson, Y. “Stops walking when talking” as a predictor of falls in elderly people. Lancet 1997, 349, 617. [Google Scholar] [CrossRef]
- Faulkner, K.A.; Redfern, M.S.; Cauley, J.A.; Landsittel, D.P.; Studenski, S.A.; Rosano, C.; Simonsick, E.M.; Harris, T.B.; Shorr, R.I.; Ayonayon, H.N.; et al. Multitasking: association between poorer performance and a history of recurrent falls. J. Am. Geriatr. Soc. 2007, 55, 570–576. [Google Scholar] [CrossRef]
- Federman, A.D.; Sano, M.; Wolf, M.S.; Siu, A.L.; Halm, E.A. Health literacy and cognitive performance in older adults. J. Am. Geriatr. Soc. 2009, 57, 1475–1480. [Google Scholar] [CrossRef]
- Kivela, K.; Elo, S.; Kyngas, H.; Kaariainen, M. The effects of health coaching on adult patients with chronic diseases: A systematic review. Patient Educ. Couns. 2014, 97, 147–157. [Google Scholar] [CrossRef]
- Sorensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H.; Consortium Health Literacy Project, E. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [Green Version]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Wolf, M.S.; Gazmararian, J.A.; Baker, D.W. Health literacy and health risk behaviors among older adults. Am. J. Prev. Med. 2007, 32, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Tokuda, Y.; Doba, N.; Butler, J.P.; Paasche-Orlow, M.K. Health literacy and physical and psychological wellbeing in Japanese adults. Patient Educ. Couns. 2009, 75, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, K.; Osaka, W.; Togari, T.; Ishikawa, H.; Yonekura, Y.; Sekido, A.; Matsumoto, M. Comprehensive health literacy in Japan is lower than in Europe: A validated Japanese-language assessment of health literacy. BMC Public Health 2015, 15, 505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uemura, K.; Yamada, M.; Okamoto, H. Effects of Active Learning on Health Literacy and Behavior in Older Adults: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2018, 66, 1721–1729. [Google Scholar] [CrossRef]
- Ishikawa, H.; Takeuchi, T.; Yano, E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care 2008, 31, 874–879. [Google Scholar] [CrossRef] [Green Version]
- Shirooka, H.; Nishiguchi, S.; Fukutani, N.; Adachi, D.; Tashiro, Y.; Hotta, T.; Morino, S.; Nozaki, Y.; Hirata, H.; Yamaguchi, M.; et al. Association between comprehensive health literacy and frailty level in community-dwelling older adults: A cross-sectional study in Japan. Geriatr. Gerontol. Int. 2017, 17, 804–809. [Google Scholar] [CrossRef]
- Yu, R.; Ong, S.; Cheung, O.; Leung, J.; Woo, J. Reference Values of Grip Strength, Prevalence of Low Grip Strength, and Factors Affecting Grip Strength Values in Chinese Adults. J. Am. Med. Dir. Assoc. 2017, 18, 551.e9–551.e16. [Google Scholar] [CrossRef]
- Bohannon, R.W. Test-retest reliability of hand-held dynamometry during a single session of strength assessment. Phys. Ther. 1986, 66, 206–209. [Google Scholar] [CrossRef]
- Martin, H.J.; Yule, V.; Syddall, H.E.; Dennison, E.M.; Cooper, C.; Aihie Sayer, A. Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? A comparison with the gold standard Bodex dynamometry. Gerontology 2006, 52, 154–159. [Google Scholar] [CrossRef]
- Katoh, M.; Isozaki, K.; Sakanoue, N.; Miyahara, T. Reliability of isometric knee extension muscle strength measurement using a hand-held dynamometer with a belt: A study of test-retest reliability in healthy elderly subjects. J. Phys. Ther. Sci. 2010, 22, 359–363. [Google Scholar] [CrossRef] [Green Version]
- Mickle, K.J.; Munro, B.J.; Lord, S.R.; Menz, H.B.; Steele, J.R. ISB Clinical Biomechanics Award 2009: Toe weakness and deformity increase the risk of falls in older people. Clin. Biomech. (BristolAvon) 2009, 24, 787–791. [Google Scholar] [CrossRef] [PubMed]
- Uritani, D.; Fukumoto, T.; Matsumoto, D. Intrarater and interrater reliabilitiesfor a toe grip dynamometer. J. Phys. Ther. Sci. 2012, 24, 639–643. [Google Scholar] [CrossRef] [Green Version]
- Soma, M.; Murata, S.; Kai, Y.; Nakae, H.; Satou, Y.; Murata, J.; Miyazaki, J. Examinations of factors influencing toe grip strength. J. Phys. Sci. 2016, 28, 3131–3135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abe, T.; Yaginuma, Y.; Fujita, E.; Thiebaud, R.S.; Kawanishi, M.; Akamine, T. Associations of sit-up ability with sarcopenia classification measures in Japanese older women. Interv. Med. Appl. Sci. 2016, 8, 152–157. [Google Scholar] [CrossRef]
- Jones, C.J.; Rikli, R.E.; Beam, W.C. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res. Q. Exerc. Sport 1999, 70, 113–119. [Google Scholar] [CrossRef]
- Suwa, M.; Imoto, T.; Kida, A.; Yokochi, T.; Iwase, M.; Kozawa, K. Association of body flexibility and carotid atherosclerosis in Japanese middle-aged men: A cross-sectional study. BMJ Open 2018, 8, e019370. [Google Scholar] [CrossRef] [Green Version]
- Macrae, P.G.; Lacourse, M.; Moldavon, R. Physical performance measures that predict faller status in community-dwelling older adults. J. Orthop. Sports Phys. 1992, 16, 123–128. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Cullen, B.; Fahy, S.; Cunningham, C.J.; Coen, R.F.; Bruce, I.; Greene, E.; Coakley, D.; Walsh, J.B.; Lawlor, B.A. Screening for dementia in an Irish community sample using MMSE: A comparison of norm-adjusted versus fixed cut-points. Int. J. Geriatr. Psychiatry 2005, 20, 371–376. [Google Scholar] [CrossRef]
- Tsoi, K.K.; Chan, J.Y.; Hirai, H.W.; Wong, S.Y.; Kwok, T.C. Cognitive Tests to Detect Dementia: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2015, 175, 1450–1458. [Google Scholar] [CrossRef] [Green Version]
- Heilbronner, R.L.; Henry, G.K.; Buck, P.; Adams, R.L.; Fogle, T. Lateralized brain damage and performance on trail making A and B, Digit Span Forward and Backward, and TPT Memory and Location. Arch. Clin. Neuropsychol. J. Natl. Acad. Neuropsychol. 1991, 6, 251–258. [Google Scholar] [CrossRef]
- Kaneko, M.; Morimoto, Y.; Kimura, M.; Fuchimoto, K.; Fuchimoto, T. A kinematic analysis of walking and physical fitness testing in elderly women. Can. J. Sport Sci. 1991, 16, 223–228. [Google Scholar] [PubMed]
- Grieve, D.W.; Gear, R.J. The relationships between length of stride, step frequency, time of swing and speed of walking for children and adults. Ergonomics 1966, 9, 379–399. [Google Scholar] [CrossRef] [PubMed]
- Burnfield, J.M.; Josephson, K.R.; Powers, C.M.; Rubenstein, L.Z. The influence of lower extremity joint torque on gait characteristics in elderly men. Arch. Phys. Med. Rehabil. 2000, 81, 1153–1157. [Google Scholar] [CrossRef] [PubMed]
- Buckinx, F.; Croisier, J.L.; Reginster, J.Y.; Petermans, J.; Goffart, E.; Bruyere, O. Relationship between Isometric Strength of Six Lower Limb Muscle Groups and Motor Skills among Nursing Home Residents. J. Frailty Aging 2015, 4, 184–187. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [Green Version]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Shimada, H.; Suzuki, T.; Suzukawa, M.; Makizako, H.; Doi, T.; Yoshida, D.; Tsutsumimoto, K.; Anan, Y.; Uemura, K.; Ito, T.; et al. Performance-based assessments and demand for personal care in older Japanese people: A cross-sectional study. BMJ Open 2013, 3. [Google Scholar] [CrossRef] [Green Version]
| Variable | Total | Slow Gait Speed | Fast Gait Speed | p-Value | Effect Size |
|---|---|---|---|---|---|
| (n = 240) | (n = 40) | (n = 200) | (φ, d) | ||
| Age (years) | 73.8 ± 6.0 | 73.7 ± 5.2 | 73.8 ± 6.2 | 0.859 | 0.030 |
| Gender | |||||
| male (n; %) | 52 (21.7%) | 8 (20.0%) | 44 (22.0%) | 0.779 | 0.018 |
| female (n; %) | 188 (78.3%) | 32 (80.0%) | 156 (78.0%) | ||
| Education (years) | 11.8 ± 2.3 | 11.9 ± 2.0 | 11.8 ± 2.3 | 0.849 | 0.030 |
| Height (cm) | 154.6 ± 7.7 | 151.0 ± 7.6 | 155.3 ± 7.6 | 0.001 | 0.560 |
| Weight (kg) | 53.3 ± 8.7 | 52.5 ± 8.3 | 53.4 ± 8.8 | 0.546 | 0.100 |
| BMI (kg/cm2) | 22.3 ± 3.0 | 23.0 ± 2.7 | 22.1 ± 3.1 | 0.114 | 0.270 |
| Diseases | |||||
| Hypertension, yes (n; %) | 94 (39.2%) | 18 (45.0%) | 76 (38.0%) | 0.408 | 0.053 |
| no (n; %) | 146 (61.8%) | 22 (55.0%) | 124 (62.0%) | ||
| Dyslipidemia, yes (n; %) | 30 (12.5%) | 7 (17.5%) | 23 (11.5%) | 0.295 | 0.068 |
| no (n; %) | 210 (87.5%) | 33 (82.5%) | 177 (88.5%) | ||
| Diabetes, yes (n; %) | 14 (5.8%) | 3 (7.5%) | 11 (5.5%) | 0.709 | 0.032 |
| no (n; %) | 226 (94.2%) | 37 (92.5%) | 189 (94.5%) | ||
| Cardiovascular disease, | 18 (7.5%) | 2 (5.0%) | 16 (8.0%) | 0.745 | 0.042 |
| yes (n; %) | |||||
| no (n; %) | 222 (92.5%) | 38 (95.0%) | 184 (92.0%) | ||
| Respiratory disease, | 7 (2.9%) | 1 (2.5%) | 6 (3.0%) | 1.000 | 0.011 |
| yes (n; %) | |||||
| no (n; %) | 233 (97.1%) | 39 (97.5%) | 194 (97.0%) | ||
| Osteoporosis, yes (n; %) | 17 (7.1%) | 2 (5.0%) | 15 (7.5%) | 0.745 | 0.036 |
| no (n; %) | 223 (92.9%) | 38 (95.0%) | 185 (92.5%) | ||
| Orthopedic disease, | 37 (15.4%) | 4 (10.0%) | 33 (16.5%) | 0.299 | 0.067 |
| yes (n; %) | |||||
| no (n; %) | 203 (84.6%) | 36 (90.0%) | 167 (83.5%) | ||
| CCHL (point) | 19.3 ± 2.4 | 18.3 ± 2.7 | 19.5 ± 2.3 | 0.004 | 0.510 |
| Grip strength (kg) | 25.8 ± 6.5 | 23.6 ± 7.1 | 26.2 ± 6.4 | 0.020 | 0.410 |
| Knee extension strength (%) | 43.5 ± 10.7 | 39.5 ± 11.1 | 44.3 ± 10.5 | 0.009 | 0.460 |
| Toe-grip strength (kg) | 7.0 ± 3.0 | 5.8 ± 3.5 | 7.3 ± 2.9 | 0.005 | 0.490 |
| Sit-up test (number) | 9.0 ± 6.5 | 7.6 ± 6.1 | 9.2 ± 6.6 | 0.163 | 0.250 |
| CS-30 (number) | 21.1 ± 5.3 | 17.6 ± 5.1 | 21.8 ± 5.1 | p < 0.001 | 0.820 |
| Sit-and-reach test (cm) | 34.9 ± 9.3 | 31.7 ± 10.8 | 35.6 ± 8.9 | 0.015 | 0.420 |
| One-leg stance test (sec) | 36.6 ± 36.0 | 17.0 ± 25.6 | 40.5 ± 36.5 | p < 0.001 | 0.670 |
| Gait speed (m/sec) | 1.50 ± 0.21 | 1.16 ± 0.14 | 1.57 ± 0.15 | p < 0.001 | 2.770 |
| MMSE (point) | 28.1 ± 1.8 | 27.9 ± 2.0 | 28.2 ± 1.8 | 0.397 | 0.150 |
| TMT-A (sec) | 105.5 ± 32.5 | 18.3 ± 35.3 | 101.8 ± 30.6 | p < 0.001 | 0.720 |
| Variable | OR | 95% | p-Value |
|---|---|---|---|
| Confidence Interval | |||
| Model 1 * | |||
| CCHL (point) | 1.222 | (1.062–1.405) | 0.005 |
| Model 2 † | |||
| CCHL (point) | 1.231 | (1.064–1.425) | 0.005 |
| Height (cm) | 1.091 | (1.033–1.152) | 0.002 |
| Model 3 ‡ | |||
| CCHL (point) | 1.179 | (1.013–1.371) | 0.033 |
| Height (cm) | 1.087 | (1.028–1.150) | 0.003 |
| CS-30 (number) | 1.190 | (1.090–1.300) | p < 0.001 |
| Model 4 § | |||
| CCHL (point) | 1.208 | (1.041–1.402) | 0.013 |
| Height (cm) | 1.068 | (1.012–1.128) | 0.017 |
| TMT-A (sec) | 0.985 | (0.975–0.996) | 0.006 |
| Dependent variable: gait speed (fast or slow) | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anami, K.; Murata, S.; Nakano, H.; Nonaka, K.; Iwase, H.; Shiraiwa, K.; Abiko, T.; Goda, A.; Horie, J. The Association between Health Literacy and Gait Speed in Community-Dwelling Older Adults. Healthcare 2020, 8, 369. https://doi.org/10.3390/healthcare8040369
Anami K, Murata S, Nakano H, Nonaka K, Iwase H, Shiraiwa K, Abiko T, Goda A, Horie J. The Association between Health Literacy and Gait Speed in Community-Dwelling Older Adults. Healthcare. 2020; 8(4):369. https://doi.org/10.3390/healthcare8040369
Chicago/Turabian StyleAnami, Kunihiko, Shin Murata, Hideki Nakano, Koji Nonaka, Hiroaki Iwase, Kayoko Shiraiwa, Teppei Abiko, Akio Goda, and Jun Horie. 2020. "The Association between Health Literacy and Gait Speed in Community-Dwelling Older Adults" Healthcare 8, no. 4: 369. https://doi.org/10.3390/healthcare8040369
APA StyleAnami, K., Murata, S., Nakano, H., Nonaka, K., Iwase, H., Shiraiwa, K., Abiko, T., Goda, A., & Horie, J. (2020). The Association between Health Literacy and Gait Speed in Community-Dwelling Older Adults. Healthcare, 8(4), 369. https://doi.org/10.3390/healthcare8040369





