The Lonely, Isolating, and Alienating Implications of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Abstract
1. The Lonely, Isolating, and Alienating Implications of ME/CFS
2. Method
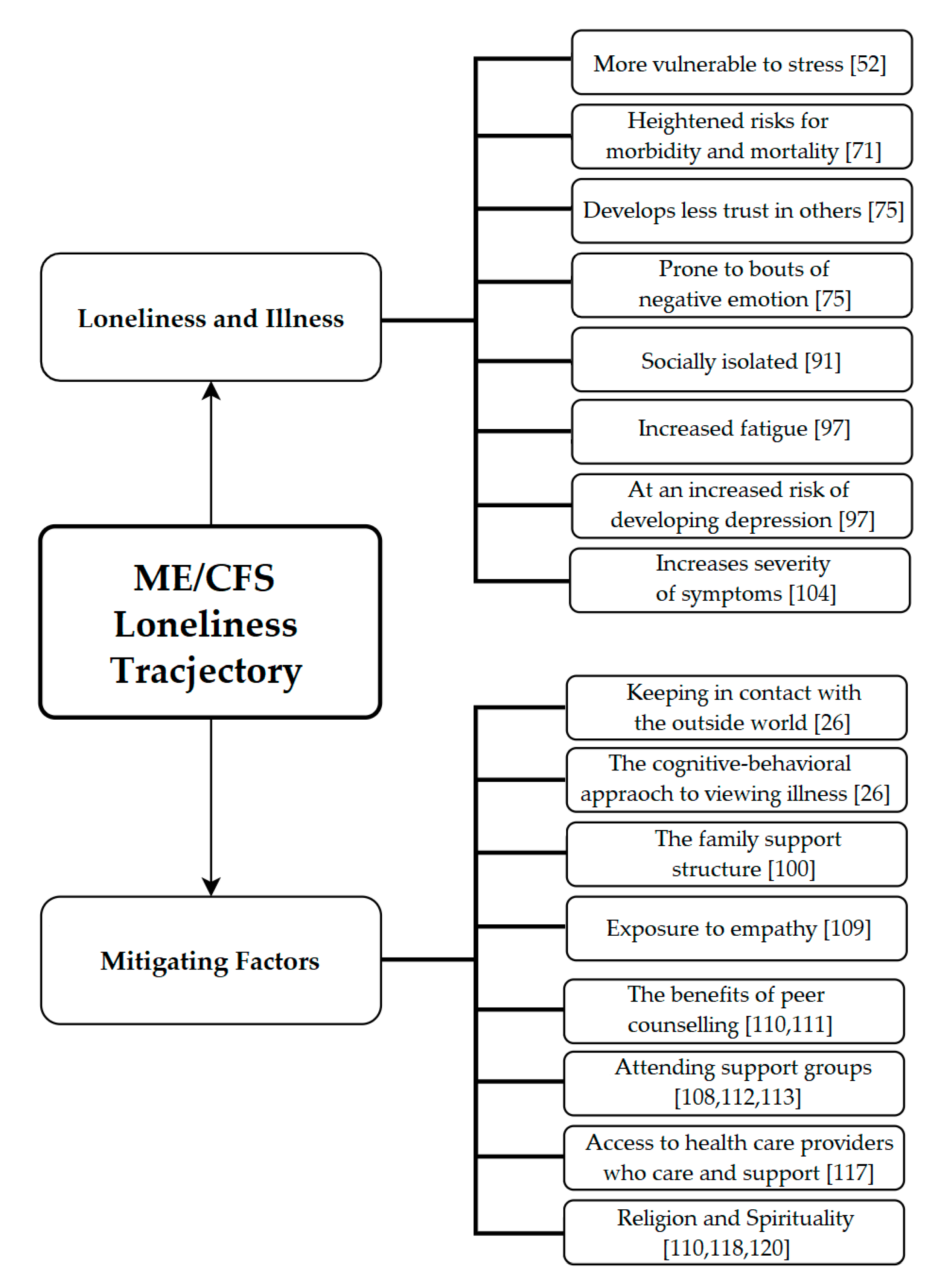
3. Results
3.1. Psychosocial Factors of ME/CFS
3.1.1. How ME/CFS Affects Sufferer’s Mental Health
3.1.2. Psychosocial Implications of ME/CFS during Adolescence
3.1.3. Psychosocial Implications of ME/CFS during Adulthood
3.1.4. Caring for Someone with ME/CFS
3.2. Loneliness
3.2.1. The Stigma of Loneliness
3.2.2. Loneliness and Illness
“Individuals who are satisfied with their lives and who experience frequent positive emotions—that is, individuals with high levels of subjective well-being … —not only feel good but may also have reduced risk for developing coronary heart disease … subjective well-being may buffer against the harmful health consequences of stress and exert direct influence on bodily systems or may motivate healthy behavior”(p. 1).
3.2.3. Illness Conceptualization
3.2.4. Loneliness, Chronic Illness and Pain
3.3. Coping with ME/CFS Induced Loneliness
3.3.1. The Power of Empathy
3.3.2. Keeping in Contact with the Outside World
3.3.3. Peer Counseling
3.3.4. Support Groups
3.3.5. Solitude
3.3.6. A Cognitive-Behavioral Approach to Illness
3.3.7. Religion
3.3.8. Spirituality
3.3.9. Health Care Providers Therapeutic Use of Self
4. Discussion
4.1. Summary
4.2. Future Directions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Nacul, L.; O’Boyle, S.; Palla, L.; Nacul, F.E.; Mudie, K.; Kingdon, C.C.; Cliff, J.M.; Clark, T.G.; Dockrell, H.M.; Lacerda, E.M. How Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Progresses: The Natural History of ME/CFS. Front. Neurol. 2020, 11, 826. [Google Scholar] [CrossRef] [PubMed]
- Costa, D.C.; Tannock, C.; Brostoff, J. Brainstem perfusion is impaired in chronic fatigue syndrome. QJM Int. J. Med. 1995, 88, 767–773. [Google Scholar] [CrossRef]
- Bradley, L.A.; McKendree-Smith, N.L.; Alberts, K.R.; Alarcón, G.S.; Mountz, J.M.; Deutsch, G. Use of neuroimaging to understand abnormal pain sensitivity in fibromyalgia. Curr. Rheumatol. Rep. 2000, 2, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Meeus, M.; Van Oosterwijck, J.; Ickmans, K.; Moorkens, G.; Hans, G.; De Clerck, L.S. In the mind or in the brain? Scientific evidence for central sensitisation in chronic fatigue syndrome. Eur. J. Clin. Investig. 2011, 42, 203–212. [Google Scholar] [CrossRef]
- Feltham, C.; Hanley, T.; Winter, L.A. (Eds.) The SAGE Handbook of Counselling and Psychotherapy; Sage: London, UK, 2017. [Google Scholar]
- Friedberg, F.; Bateman, L.; Bested, A.C.; Davenport, T.; Friedman, K.J.; Gurwitt, A.; Jason, L.A.; Lapp, C.W.; Stevens, S.R.; Underhill, R.A.; et al. ME/CFS: A Primer for Clinical Practitioners; International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis: Chicago, IL, USA, 2012. [Google Scholar]
- Neu, D.; Mairesse, O.; Montaña, X.; Gilson, M.; Corazza, F.; Lefèvre, N.; Linkowski, P.; Le Bon, O.; Verbanck, P. Dimensions of pure chronic fatigue: Psychophysical, cognitive and biological correlates in the chronic fatigue syndrome. Graefe’s Arch. Clin. Exp. Ophthalmol. 2014, 114, 1841–1851. [Google Scholar] [CrossRef]
- Friedman, K.J.; Bateman, L.; Bested, A.; Nahle, Z. Editorial: Advances in ME/CFS Research and Clinical Care. Front. Pediatr. 2019, 7, 370. [Google Scholar] [CrossRef]
- McEvedy, C.P.; Beard, A.W. Royal Free Epidemic of 1955: A Reconsideration. BMJ 1970, 1, 7–11. [Google Scholar] [CrossRef]
- Williams-Wilson, M. “I Had to Give Up So, So Much”: A Narrative Study to Investigate the Impact of Chronic Fatigue Syndrome (CFS) on the Lives of Young People. Ph.D. Thesis, Bournemouth University, Poole, UK, 2009. [Google Scholar]
- Canadian Institutes of Health Research. Government of Canada Invests $1.4M in Biomedical Research to Improve the Quality of Life of People Living with Myalgic Encephalomyelitis. 2019. Available online: https://www.canada.ca/en/institutes-health-research/news/2019/08/government-of-canada-invests-14m-in-biomedical-research-to-improve-the-quality-of-life-of-people-living-with-myalgic-encephalomyelitis.html (accessed on 14 July 2020).
- Committee on the Science of Changing Behavioral Health Social Norms; Division of Behavioral and Social Sciences and Education. Ending Discrimination Against People with Mental and Substance Use Disorders; The National Academies Press: Washington, DC, USA, 2016. [Google Scholar]
- Jason, L.A.; Sunnquist, M. The Development of the DePaul Symptom Questionnaire: Original, Expanded, Brief, and Pediatric Versions. Front. Pediatr. 2018, 6, 330. [Google Scholar] [CrossRef]
- Chu, L.; Valencia, I.J.; Garvert, D.W.; Montoya, J.G. Onset Patterns and Course of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Front. Pediatr. 2019, 7, 12. [Google Scholar] [CrossRef]
- Kerr, J.R. Epstein-Barr Virus Induced Gene-2 Upregulation Identifies a Particular Subtype of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Front. Pediatr. 2019, 7, 59. [Google Scholar] [CrossRef]
- Proal, A.D.; Marshall, T. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome in the Era of the Human Microbiome: Persistent Pathogens Drive Chronic Symptoms by Interfering with Host Metabolism, Gene Expression, and Immunity. Front. Pediatr. 2018, 6, 373. [Google Scholar] [CrossRef] [PubMed]
- Gandevia, S.C. Spinal and Supraspinal Factors in Human Muscle Fatigue. Physiol. Rev. 2001, 81, 1725–1789. [Google Scholar] [CrossRef] [PubMed]
- The Terminology of ME & CFS. Invest in ME Research. 2005. Available online: http://www.investinme.org/Article%20010-Encephalopathy%20Hooper.shtml (accessed on 14 July 2020).
- Catchpole, S.; Garip, G. Acceptance and identity change: An interpretative phenomenological analysis of carers’ experiences in myalgic encephalopathy/chronic fatigue syndrome. J. Health Psychol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Missen, A.; Hollingworth, W.; Eaton, N.; Crawley, E. The financial and psychological impacts on mothers of children with chronic fatigue syndrome (CFS/ME). Child Care Health Dev. 2011, 38, 505–512. [Google Scholar] [CrossRef]
- Parslow, R.M.; Harris, S.; Broughton, J.; Alattas, A.; Crawley, E.; Haywood, K.; Shaw, A. Children’s experiences of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): A systematic review and meta-ethnography of qualitative studies. BMJ Open 2017, 7, e01263. [Google Scholar] [CrossRef]
- Winger, A.; Ekstedt, M.; Wyller, V.B.; Helseth, S. ‘Sometimes it feels as if the world goes on without me’: Adolescents’ experiences of living with chronic fatigue syndrome. J. Clin. Nurs. 2013, 23, 2649–2657. [Google Scholar] [CrossRef]
- Åsbring, P.; Närvänen, A.-L. Women’s Experiences of Stigma in Relation to Chronic Fatigue Syndrome and Fibromyalgia. Qual. Health Res. 2002, 12, 148–160. [Google Scholar] [CrossRef]
- Fisher, H.; Crawley, E. Why do young people with CFS/ME feel anxious? A qualitative study. Clin. Child Psychol. Psychiatry 2012, 18, 556–573. [Google Scholar] [CrossRef]
- Skelly, M.; Walker, H.; Carson, R.; Schoen, D. Alternative Treatments for Fibromyalgia and Chronic Fatigue Syndrome; Hunter House Publishers: Nashville, TN, USA, 2006. [Google Scholar]
- Campling, F.; Sharpe, M. Chronic Fatigue Syndrome (ME/CFS); Oxford University Press: Oxford, UK, 2000. [Google Scholar]
- Morriss, R.K.; Ahmed, M.; Wearden, A.J.; Mullis, R.; Strickland, P.; Appleby, L.; Campbell, I.T.; Pearson, D. The role of depression in pain, psychophysiological syndromes and medically unexplained symptoms associated with chronic fatigue syndrome. J. Affect. Disord. 1999, 55, 143–148. [Google Scholar] [CrossRef]
- Maes, M. An intriguing and hitherto unexplained co-occurrence: Depression and chronic fatigue syndrome are manifestations of shared inflammatory, oxidative and nitrosative (IO&NS) pathways. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2011, 35, 784–794. [Google Scholar] [CrossRef]
- Nijs, J.; De Meirleir, K.; Duquet, W. Kinesiophobia in chronic fatigue syndrome: Assessment and associations with disability. Arch. Phys. Med. Rehabil. 2004, 85, 1586–1592. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Vanherberghen, K.; Duquet, W.; De Meirleir, K. Chronic Fatigue Syndrome: Lack of Association Between Pain-Related Fear of Movement and Exercise Capacity and Disability. Phys. Ther. 2004, 84, 696–705. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Meeus, M.; Nijs, J. Central sensitization: A biopsychosocial explanation for chronic widespread pain in patients with fibromyalgia and chronic fatigue syndrome. Clin. Rheumatol. 2006, 26, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Petrie, K.; Moss-Morris, R.; Weinman, J. The impact of catastrophic beliefs on functioning in chronic fatigue syndrome. J. Psychosom. Res. 1995, 39, 31–37. [Google Scholar] [CrossRef]
- Karayannis, N.V.; Baumann, I.; Sturgeon, J.A.; Melloh, M.; Mackey, S.C. The Impact of Social Isolation on Pain Interference: A Longitudinal Study. Ann. Behav. Med. 2018, 53, 65–74. [Google Scholar] [CrossRef]
- Zhang, M.; Zhang, Y.; Kong, Y. Interaction between social pain and physical pain. Brain Sci. Adv. 2019, 5, 265–273. [Google Scholar] [CrossRef]
- Collin, S.M.; Norris, T.; Nuevo, R.; Tilling, K.; Joinson, C.; Sterne, J.A.C.; Crawley, E. Chronic Fatigue Syndrome at Age 16 Years. Pediatrics 2016, 137, e20153434. [Google Scholar] [CrossRef]
- Nijhof, S.L.; Maijer, K.; Bleijenberg, G.; Uiterwaal, C.S.P.M.; Kimpen, J.L.L.; Van De Putte, E.M. Adolescent Chronic Fatigue Syndrome: Prevalence, Incidence, and Morbidity. Pediatrics 2011, 127, e1169–e1175. [Google Scholar] [CrossRef]
- Northam, E.A. Psychosocial impact of chronic illness in children. J. Paediatr. Child Health 1997, 33, 369–372. [Google Scholar] [CrossRef]
- Kearney, C.A.; Graczyk, P. A Response to Intervention Model to Promote School Attendance and Decrease School Absenteeism. Child Youth Care Forum 2013, 43, 1–25. [Google Scholar] [CrossRef]
- University of Bristol. 1 in 50 16-Year-Olds Affected by Chronic Fatigue Syndrome. 2015. Available online: https://www.sciencedaily.com/releases/2016/01/160125090619.htm (accessed on 27 May 2020).
- Vitulano, L.A. Psychosocial issues for children and adolescents with chronic illness: Self-esteem, school functioning and sports participation. Child Adolesc. Psychiatr. Clin. N. Am. 2003, 12, 585–592. [Google Scholar] [CrossRef]
- Kiliçkaya, C.; Asi Karakaş, S. The effect of illness perception on loneliness and coping with stress in patients with Chronic Obstructive Pulmonary Disease (COPD). Int. J. Caring Sci. 2016, 9, 481. [Google Scholar]
- Gureje, O.; Von Korff, M.; Simon, G.E.; Gater, R. Persistent Pain and Well-being. JAMA 1998, 280, 147–151. [Google Scholar] [CrossRef]
- Johannes, C.B.; Le, T.K.; Zhou, X.; Johnston, J.A.; Dworkin, R.H. The Prevalence of Chronic Pain in United States Adults: Results of an Internet-Based Survey. J. Pain 2010, 11, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.L.; Morrison, V.; Robinson, C.A. Exploring caregiving experiences: Caregiver coping and making sense of illness. Aging Ment. Health 2013, 18, 600–609. [Google Scholar] [CrossRef]
- Jason, L.A.; Benton, M.C.; Valentine, L.M.; Johnson, A.; Torres-Harding, S.R. The Economic impact of ME/CFS: Individual and societal costs. Dyn. Med. 2008, 7, 6. [Google Scholar] [CrossRef] [PubMed]
- Densham, S.; Williams, D.; Johnson, A.; Turner-Cobb, J.M. Enhanced psychological flexibility and improved quality of life in chronic fatigue syndrome/myalgic encephalomyelitis. J. Psychosom. Res. 2016, 88, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, R.; Kelly, B.J.; Foran, A.; Terry, D.; Whiting, J. Quality of life in chronic fatigue syndrome. Soc. Sci. Med. 1995, 41, 1367–1372. [Google Scholar] [CrossRef]
- Girgis, A.; Lambert, S.; Johnson, C.; Waller, A.; Currow, D. Physical, Psychosocial, Relationship, and Economic Burden of Caring for People with Cancer: A Review. J. Oncol. Pract. 2013, 9, 197–202. [Google Scholar] [CrossRef]
- Cruz, D.D.A.L.M.D.; Pimenta, C.A.M.; Kurita, G.P.; Oliveira, A.C. Caregivers of Patients with Chronic Pain: Responses to Care. Int. J. Nurs. Terminol. Classif. 2004, 15, 5–14. [Google Scholar] [CrossRef]
- Nacul, L.; Lacerda, E.; Pheby, D.; Campion, P.; Molokhia, M.; Fayyaz, S.; Leite, J.C.D.C.; Poland, F.; Howe, A.; Drachler, M.D.L. Prevalence of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) in three regions of England: A repeated cross-sectional study in primary care. BMC Med. 2011, 9, 91. [Google Scholar] [CrossRef] [PubMed]
- Houtzager, B.A.; Grootenhuis, M.A.; Caron, H.N.; Last, B.F. Sibling Self-Report, Parental Proxies, and Quality of Life: The Importance of Multiple Informants for Siblings of a Critically Ill Child. Pediatr. Hematol. Oncol. 2005, 22, 25–40. [Google Scholar] [CrossRef] [PubMed]
- Rokach, A. The Psychological Journey to and from Loneliness; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness and pathways to disease. Brain Behav. Immun. 2003, 17, 98–105. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Cacioppo, S.; Capitanio, J.P.; Cole, S.W. The Neuroendocrinology of Social Isolation. Annu. Rev. Psychol. 2015, 66, 733–767. [Google Scholar] [CrossRef] [PubMed]
- Danneel, S.; Maes, M.; Vanhalst, J.; Bijttebier, P.; Goossens, L. Developmental Change in Loneliness and Attitudes Toward Aloneness in Adolescence. J. Youth Adolesc. 2017, 42, 815. [Google Scholar] [CrossRef]
- Rokach, A. Three of humankind’s universal experiences: Loneliness, illness and death. In Lonelness in Life: Education, Business, Society; Kowalski, C., Rokach, A., Cangemi, J.P., Eds.; McGraw-Hill: New York, NY, USA, 2015; pp. 119–132. [Google Scholar]
- Rokach, A.; Sha’ked, A. Together and Lonely: Loneliness in Intimate Relationships—Causes and Coping; Nova Publishers: Hauppauge, NY, USA, 2013. [Google Scholar]
- Cacioppo, S.; Grippo, A.J.; London, S.; Goossens, L.; Cacioppo, J.T. Loneliness. Perspect. Psychol. Sci. 2015, 10, 238–249. [Google Scholar] [CrossRef]
- Friedman, R.L. Widening the therapeutic lens: Sense of belonging as an integral dimension of the human experience. (Doctoral dissertation). Diss. Abstr. Int. Sect. B Sci. Eng. 2007, 68, 3394. [Google Scholar]
- Loneliness can Directly Impair Immune System, Increase Risk of Death: Study. CTV News. 16 June 2020. Available online: https://www.ctvnews.ca/health/loneliness-can-directly-impair-immune-system-increase-risk-of-death-study-1.4986159 (accessed on 5 July 2020).
- Fallon, N.; Brown, C.; Twiddy, H.; Brian, E.; Frank, B.; Nurmikko, T.; Andrej Stancak, A. Adverse effects of COVID-19 related lockdown on pain, physical activity and psychological wellbeing in people with chronic pain. medRxiv 2020. [Google Scholar] [CrossRef]
- Perlman, D.; Joshi, P. The revelation of loneliness. J. Soc. Behav. Personal. 1987, 2, 63–76. [Google Scholar]
- Rokach, A. Loneliness and the Life Cycle. Psychol. Rep. 2000, 86, 629–642. [Google Scholar] [CrossRef]
- Lasgaard, M.; Friis, K.; Shevlin, M. “Where are all the lonely people?” A population-based study of high-risk groups across the life span. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 1373–1384. [Google Scholar] [CrossRef] [PubMed]
- Boehm, J.K.; Chen, Y.; Williams, D.R.; Ryff, C.D.; Kubzansky, L.D. Subjective well-being and cardiometabolic health: An 8-11year study of midlife adults. J. Psychosom. Res. 2016, 85, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Cameron, L.D.; Leventhal, H. Self-regulation, health and illness: An overview. In The Self-Regulation of Health and Illness Behaviour; Cameron, L.D., Leventhal, H., Eds.; Routledge: London, UK, 2003; pp. 1–13. [Google Scholar]
- Sullivan, M.D. The new subjective medicine: Taking the patient’s point of view on health care and health. Soc. Sci. Med. 2003, 56, 1595–1604. [Google Scholar] [CrossRef]
- Sellick, S.M.; Edwardson, A.D. Screening new cancer patients for psychological distress using the hospital anxiety and depression scale. Psycho Oncol. 2007, 16, 534–542. [Google Scholar] [CrossRef]
- Rokach, A. Health, Illness, and the Psychological Factors Affecting Them. J. Psychol. 2019, 153, 1–5. [Google Scholar] [CrossRef]
- Rattray, J.; Johnston, M.; Wildsmith, J.A.W. Predictors of emotional outcomes of intensive care. Anesthesia 2005, 60, 1085–1092. [Google Scholar] [CrossRef] [PubMed]
- Kiecolt-Glaser, J.K.; McGuire, L.; Robles, T.F.; Glaser, R. Psychoneuroimmunology: Psychological influences on immune function and health. J. Consult. Clin. Psychol. 2002, 70, 537–547. [Google Scholar] [CrossRef]
- Lauder, W.; Mummery, K.; Jones, M.; Caperchione, C.M. A comparison of health behaviours in lonely and non-lonely populations. Psychol. Health Med. 2006, 11, 233–245. [Google Scholar] [CrossRef]
- Bunker, S.J.; Colquhoun, D.M.; Esler, M.D.; Hickie, I.B.; Hunt, D.; Jelinek, V.M.; Oldenburg, B.F.; Peach, H.G.; Ruth, D.; Tennant, C.C.; et al. “Stress” and coronary heart disease: Psychosocial risk factors. Med. J. Aust. 2003, 178, 272–276. [Google Scholar] [CrossRef]
- Bramston, P.; Pretty, G.; Chipuer, H. Unravelling Subjective Quality of Life: An Investigation of Individual and Community Determinants. Soc. Indic. Res. 2002, 59, 261–274. [Google Scholar] [CrossRef]
- Ernst, J.M.; Cacioppo, J.T. Lonely hearts: Psychological perspectives on loneliness. Appl. Prev. Psychol. 1999, 8, 1–22. [Google Scholar] [CrossRef]
- Steptoe, A.; Owen, N.; Kunz-Ebrecht, S.R.; Brydon, L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology 2004, 29, 593–611. [Google Scholar] [CrossRef]
- Seeman, T.E.; Singer, B.H.; Ryff, C.D.; Love, G.D.; Levy-Storms, L. Social Relationships, Gender, and Allostatic Load Across Two Age Cohorts. Psychosom. Med. 2002, 64, 395–406. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, H.; Leventhal, E.A.; Cameron, L. Representations, procedures, and affect in illness self-regulation: A perceptual-cognitive model. In Handbook of Health Psychology; Baum, A., Revenson, T.A., Singer, J.E., Eds.; Earlbaum: Mahwah, NJ, USA, 2001; pp. 133–151. [Google Scholar]
- Glaser, R.; Kiecolt-Glaser, J.K.; Bonneau, R.H.; Malarkey, W.; Kennedy, S.; Hughes, J. Stress-induced modulation of the immune response to recombinant hepatitis B vaccine. Psychosom. Med. 1992, 54, 22–29. [Google Scholar] [CrossRef]
- Hagerty, B.M.; Williams, R.A.; Coyne, J.C.; Early, M.R. Sense of belonging and indicators of social and psychological functioning. Arch. Psychiatr. Nurs. 1996, 10, 235–244. [Google Scholar] [CrossRef]
- Brannon, L.; Feist, J. Health Psychology: An Introduction to Behavior and Health; Thomson Wadsworth: Belmont, CA, USA, 2004. [Google Scholar]
- REPRINT: Social Networks, Host Resistance, and Mortality: A Nine-Year Follow-up Study of Alameda County Residents. Am. J. Epidemiol. 2017, 185, 1070–1088. [CrossRef]
- Segrin, C.; Domschke, T. Social Support, Loneliness, Recuperative Processes, and Their Direct and Indirect Effects on Health. Health Commun. 2011, 26, 221–232. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Cacioppo, J.T. Aging and Loneliness. Curr. Dir. Psychol. Sci. 2007, 16, 187–191. [Google Scholar] [CrossRef]
- Segrin, C.; Passalacqua, S.A. Functions of Loneliness, Social Support, Health Behaviors, and Stress in Association With Poor Health. Health Commun. 2010, 25, 312–322. [Google Scholar] [CrossRef]
- Piotrowski, C. Chronic pain patients and loneliness: A systematic review of the literature. In Loneliness in Life: Education, Business, Society; Kowalski, C., Rokach, A., Cangemi, J.P., Eds.; McGraw-Hill: New York, NY, USA, 2015; pp. 189–202. [Google Scholar]
- Morrissey, M.B.Q. Phenomenology of Pain and Suffering at the End of Life: A Humanistic Perspective in Gerontological Health and Social Work. J. Soc. Work End-Of-Life Palliat. Care 2011, 7, 14–38. [Google Scholar] [CrossRef]
- Piotrowski, C. Assessment of Pain: A Survey of Practicing Clinicians. Percept. Mot. Skills 1998, 86, 181–182. [Google Scholar] [CrossRef] [PubMed]
- Turk, D.C.; Okifuji, A. Psychological factors in chronic pain: Evolution and revolution. J. Consult. Clin. Psychol. 2002, 70, 678–690. [Google Scholar] [CrossRef] [PubMed]
- Dansie, E.J.; Turk, D.C. Assessment of patients with chronic pain. Br. J. Anaesth. 2013, 111, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Newton, B.J.; Southall, J.L.; Raphael, J.H.; Ashford, R.L.; LeMarchand, K. A Narrative Review of the Impact of Disbelief in Chronic Pain. Pain Manag. Nurs. 2013, 14, 161–171. [Google Scholar] [CrossRef]
- Dewar, A. Assessment and management of chronic pain in the older person living in the community. Aust. J. Adv. Nurs. 2006, 24, 33–38. [Google Scholar]
- Tse, M.M.Y.; Wan, V.T.; Vong, S.K. Health-Related Profile and Quality of Life Among Nursing Home Residents: Does Pain Matter? Pain Manag. Nurs. 2013, 14, e173–e184. [Google Scholar] [CrossRef]
- Kool, M.B.; Geenen, R. Loneliness in Patients with Rheumatic Diseases: The Significance of Invalidation and Lack of Social Support. J. Psychol. 2012, 146, 229–241. [Google Scholar] [CrossRef]
- Asnani, M.; Fraser, R.; Lewis, N.A.; Reid, M. Depression and loneliness in Jamaicans with sickle cell disease. BMC Psychiatry 2010, 10, 40. [Google Scholar] [CrossRef]
- Sofaer, B.; Moore, A.P.; Holloway, I.; Lamberty, J.M.; Thorp, T.A.S.; Dwyer, J.O. Chronic pain as perceived by older people: A qualitative study. Age Ageing 2005, 34, 462–466. [Google Scholar] [CrossRef]
- Jaremka, L.M.; Fagundes, C.P.; Glaser, R.; Bennett, J.M.; Malarkey, W.B.; Kiecolt-Glaser, J.K. Loneliness predicts pain, depression, and fatigue: Understanding the role of immune dysregulation. Psychoneuroendocrinology 2013, 38, 1310–1317. [Google Scholar] [CrossRef]
- Benka, J.; Nagyova, I.; Rosenberger, J.; Čalfová, A.; Macejova, Z.; Middel, B.; Lazúrová, I.; Van Dijk, J.P.; Groothoff, J.W. Social support and psychological distress in rheumatoid arthritis: A 4-year prospective study. Disabil. Rehabil. 2011, 34, 754–761. [Google Scholar] [CrossRef]
- Zhou, X.; Gao, D.-G. Social Support and Money as Pain Management Mechanisms. Psychol. Inq. 2008, 19, 127–144. [Google Scholar] [CrossRef]
- Rosland, A.-M.; Heisler, M.; Piette, J.D. The impact of family behaviors and communication patterns on chronic illness outcomes: A systematic review. J. Behav. Med. 2011, 35, 221–239. [Google Scholar] [CrossRef] [PubMed]
- Hawkley, L.C.; Masi, C.M.; Berry, J.D.; Cacioppo, J.T. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol. Aging 2006, 21, 152–164. [Google Scholar] [CrossRef]
- Barlow, M.A.; Liu, S.Y.; Wrosch, C. Chronic illness and loneliness in older adulthood: The role of self-protective control strategies. Health Psychol. 2015, 34, 870–879. [Google Scholar] [CrossRef]
- Stringer, H. Unlocking the emotions of cancer. PsycEXTRA Dataset 2015, 45, 34–38. [Google Scholar] [CrossRef]
- Wolf, L.D.; Davis, M.C. Loneliness, daily pain, and perceptions of interpersonal events in adults with fibromyalgia. Health Psychol. 2014, 33, 929–937. [Google Scholar] [CrossRef] [PubMed]
- Wager, T.D.; Atlas, L.Y.; Lindquist, M.A.; Roy, M.; Woo, C.-W.; Kross, E. An fMRI-Based Neurologic Signature of Physical Pain. N. Engl. J. Med. 2013, 368, 1388–1397. [Google Scholar] [CrossRef]
- Vella-Baldacchino, M.D.; Schembri, M.; Vella-Baldacchino, M. Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Malta Med. J. 2014, 26, 17–22. [Google Scholar]
- Abrams, L. Chronic Fatigue Syndrome; Thomson Gale: Farmington Hills, MI, USA, 2003. [Google Scholar]
- Biordi, D.L. Social isolation. In Chronic Illness: Impact and Interventions; Lubkin, I., Larsen, P., Eds.; Jones and Bartlett: Burlington, MA, USA, 2002; pp. 119–147. [Google Scholar]
- Bharadvaj, D. Natural Treatments for Chronic Fatigue Syndrome; Greenwood Publishing Group: Westport, CT, USA, 2008. [Google Scholar]
- Riegel, B.; Carlson, B. Is Individual Peer Support a Promising Intervention for Persons With Heart Failure? J. Cardiovasc. Nurs. 2004, 19, 174–183. [Google Scholar] [CrossRef]
- Perese, E.F.; Wolf, M. Combating Loneliness Among Persons with Severe Mental Illness: Social Network Interventions’ Characteristics, Effectiveness, And Applicability. Issues Ment. Health Nurs. 2005, 26, 591–609. [Google Scholar] [CrossRef] [PubMed]
- Purk, J.K. Support Groups: Why Do People Attend? Rehabil. Nurs. 2004, 29, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.J.; Craig, D.; MacPherson, K.; Alexander, S. Promoting Positive Affect and Diminishing Loneliness of Widowed Seniors Through a Support Intervention. Public Health Nurs. 2001, 18, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Ali, N. Understanding Chronic Fatigue Syndrome: An Introduction for Patients and Caregivers; Rowman & Littlefield: Lanham, MD, USA, 2015. [Google Scholar]
- Brigden, A.; Barnett, J.; Parslow, R.M.; Beasant, L.; Crawley, E. Using the internet to cope with chronic fatigue syndrome/myalgic encephalomyelitis in adolescence: A qualitative study. BMJ Paediatr. Open 2018, 2, e000299. [Google Scholar] [CrossRef]
- Broadbent, S.; Coetzee, S.; Beavers, R.; Horstmanshof, L. Patient experiences and the psychosocial benefits of group aquatic exercise to reduce symptoms of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A pilot study. Fatigue Biomed. Health Behav. 2020, 8, 84–96. [Google Scholar] [CrossRef]
- Holley, U.A. Social Isolation: A Practical Guide for Nurses Assisting Clients with Chronic Illness. Rehabil. Nurs. 2007, 32, 51–58. [Google Scholar] [CrossRef]
- Warner, C.B.; Roberts, A.R.; Jeanblanc, A.B.; Adams, K.B. Coping resources, loneliness, and depressive symptoms of older women with chronic illness. J. Appl. Gerontol. 2007, 38, 1–29. [Google Scholar] [CrossRef]
- Han, J.; Richardson, V.E. The Relationship Between Depression and Loneliness Among Homebound Older Persons: Does Spirituality Moderate This Relationship? J. Relig. Spiritual. Soc. Work Soc. Thought 2010, 29, 218–236. [Google Scholar] [CrossRef]
- Walton, J.; Craig, C.; Derwinski-Robinson, B.; Weinert, C. I Am Not Alone: Spirituality of Chronically III Rural Dwellers. Rehabil. Nurs. 2004, 29, 164–168. [Google Scholar] [CrossRef]
- Boellinghaus, I.; Jones, F.W.; Hutton, J. The Role of Mindfulness and Loving-Kindness Meditation in Cultivating Self-Compassion and Other-Focused Concern in Health Care Professionals. Mindfulness 2012, 5, 129–138. [Google Scholar] [CrossRef]
- Davey, A.; Chilcot, J.; Driscoll, E.; McCracken, L.M. Psychological flexibility, self-compassion and daily functioning in chronic pain. J. Context. Behav. Sci. 2020, 17, 79–85. [Google Scholar] [CrossRef]
- Ray, C.; Jefferies, S.; Weir, W.R.C. Life-events and the course of chronic fatigue syndrome. Br. J. Med. Psychol. 1995, 68, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Vercoulen, J.H.; Swanink, C.M.; Fennis, J.F.; Galama, J.M.; Van Der Meer, J.W.; Bleijenberg, G. Prognosis in chronic fatigue syndrome: A prospective study on the natural course. J. Neurol. Neurosurg. Psychiatry 1996, 60, 489–494. [Google Scholar] [CrossRef] [PubMed]
- Endicott, J.; Nee, J.; Harrison, W.; Blumenthal, R. Quality of Life Enjoyment and Satisfaction Questionnaire: A new measure. Psychopharmacol. Bull. 1993, 29, 321–326. [Google Scholar]
- Weiss, D.J.; Dawis, R.V.; England, G.W. Manual for the Minnesota Satisfaction Questionnaire. Minn. Stud. Vocat. Rehabil. 1967, 22, 120. [Google Scholar]
- Hansen, T.; Slagsvold, B. Late-Life Loneliness in 11 European Countries: Results from the Generations and Gender Survey. Soc. Indic. Res. 2015, 129, 445–464. [Google Scholar] [CrossRef]
- Rokach, A. The Effect of Gender and Culture on Loneliness: A Mini Review. Emerg. Sci. J. 2018, 2, 59–64. [Google Scholar] [CrossRef]
- Triandis, H.C. The psychological measurement of cultural syndromes. Am. Psychol. 1996, 51, 407–415. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boulazreg, S.; Rokach, A. The Lonely, Isolating, and Alienating Implications of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Healthcare 2020, 8, 413. https://doi.org/10.3390/healthcare8040413
Boulazreg S, Rokach A. The Lonely, Isolating, and Alienating Implications of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Healthcare. 2020; 8(4):413. https://doi.org/10.3390/healthcare8040413
Chicago/Turabian StyleBoulazreg, Samir, and Ami Rokach. 2020. "The Lonely, Isolating, and Alienating Implications of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome" Healthcare 8, no. 4: 413. https://doi.org/10.3390/healthcare8040413
APA StyleBoulazreg, S., & Rokach, A. (2020). The Lonely, Isolating, and Alienating Implications of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Healthcare, 8(4), 413. https://doi.org/10.3390/healthcare8040413