Association between Cerebral Infarction Risk and Medication Adherence in Atrial Fibrillation Patients Taking Direct Oral Anticoagulants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Assessment of Adherence to DOAC
2.3. Assessment of DOAC Dosage
2.4. Data Collection
2.5. Statistical Analyses
3. Results
3.1. Patients’ Characteristics
3.2. Medication Adherence and other Patients’ Background on the Risk of Cerebral Infarction
4. Discussion
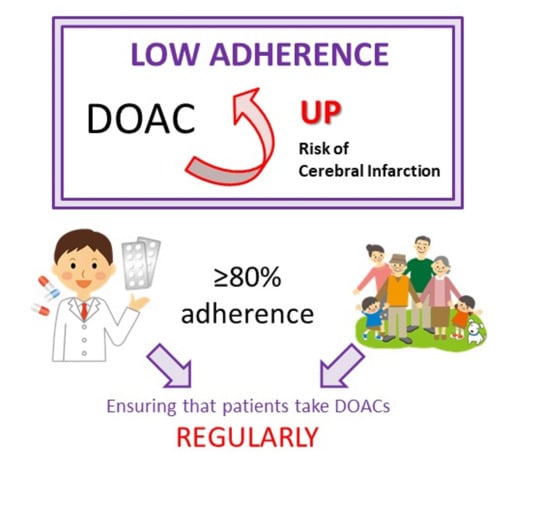
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.C.; Heidbuchel, H.; Hendriks, J.; et al. ESC Scientific Document Group. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2896–2962. [Google Scholar] [CrossRef] [Green Version]
- Hata, J.; Tanizaki, Y.; Kiyohara, Y.; Kato, I.; Kubo, M.; Tanaka, K.; Okubo, K.; Nakamura, H.; Oishi, Y.; Ibayashi, S.; et al. Ten year recurrence after first ever stroke in a Japanese community: The Hisayama study. J. Neurol. Neurosurg. Psychiatry 2005, 76, 368–372. [Google Scholar] [CrossRef]
- Aosaki, M.; Iwade, K.; Echizen, H. Information on Proper Use of Warfarin, 3rd ed.; Eisai Co., Ltd: Tokyo, Japan, 2006; pp. 170–513. [Google Scholar]
- Mekaj, Y.H.; Mekaj, A.Y.; Duci, S.B.; Miftari, E.I. New oral anticoagulants: Their advantages and disadvantages compared with vitamin K antagonists in the prevention and treatment of patients with thromboembolic events. Ther. Clin. Risk. Manag. 2015, 11, 967–977. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raparelli, V.; Proietti, M.; Cangemi, R.; Lip, G.Y.; Lane, D.A.; Basili, S. Adherence to oral anticoagulant therapy in patients with atrial fibrillation. Focus on non-vitamin K antagonist oral anticoagulants. Thromb. Haemost. 2017, 117, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Akagi, Y.; Chiba, T.; Uekusa, S.; Kato, H.; Yamamura, S.; Aoki, Y.; Enoki, M.; Ogawara, Y.; Kasahara, T.; Kimura, Y.; et al. Retrospective cohort study of the efficacy and safety of dabigatran: Real-life dabigatran use including very low-dose 75 mg twice daily administration. J. Pharm. Health Care Sci. 2019, 5, 17. [Google Scholar] [CrossRef]
- Goto, K.; Nakai, K.; Shizuta, S.; Morimoto, T.; Shiomi, H.; Natsuaki, M.; Yahata, M.; Ota, C.; Ono, K.; Makiyama, T.; et al. CREDO-Kyoto Registry Cohort-2 Investigators. Anticoagulant and antiplatelet therapy in patients with atrial fibrillation undergoing percutaneous coronary intervention. Am. J. Cardiol. 2014, 114, 70–78. [Google Scholar] [CrossRef] [Green Version]
- Shore, S.; Carey, E.P.; Turakhia, M.P.; Jackevicius, C.A.; Cunningham, F.; Pilote, L.; Bradley, S.M.; Maddox, T.M.; Grunwald, G.K.; Barón, A.E.; et al. Adherence to dabigatran therapy and longitudinal patient outcomes: Insights from the veterans health administration. Am. Heart J. 2014, 167, 810–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernandez, I.; He, M.; Brooks, M.M.; Saba, S.; Gellad, W.F. Adherence to anticoagulation and risk of stroke among Medicare Beneficiaries newly diagnosed with atrial fibrillation. Am. J. Cardiovasc. Drugs 2020, 20, 199–207. [Google Scholar] [CrossRef]
- Murata, N.; Okumura, Y.; Yokoyama, K.; Matsumoto, N.; Tachibana, E.; Kuronuma, K.; Oiwa, K.; Matsumoto, M.; Kojima, T.; Hanada, S.; et al. Clinical outcomes of off-Label dosing of direct oral anticoagulant therapy among Japanese patients with atrial fibrillation identified from the SAKURA AF registry. Circ. J. 2019, 83, 727–735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- JCS Joint Working Group. Guidelines for pharmacotherapy of atrial fibrillation (JCS 2013). Circ. J. 2014, 78, 1997–2021. [Google Scholar] [CrossRef] [Green Version]
- The Package Insert of Xarelto® in Japan. Bayer Yakuhin, Ltd. Available online: https://www.info.pmda.go.jp/go/pack/3339003F1024_1_18/ (accessed on 1 May 2020).
- The Package Insert of Eliquis® in Japan. Bristol-Myers Squibb Company. Available online: https://www.info.pmda.go.jp/go/pack/3339004F1029_1_13/ (accessed on 1 May 2020).
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, P.M.; Bryson, C.L.; Rumsfeld, J.S. Medication adherence: Its importance in cardiovascular outcomes. Circulation 2009, 119, 3028–3035. [Google Scholar] [CrossRef] [PubMed]
- Borne, R.T.; O’Donnell, C.; Turakhia, M.P.; Varosy, P.D.; Jackevicius, C.A.; Marzec, L.N.; Masoudi, F.A.; Hess, P.L.; Maddox, T.M.; Ho, P.M. Adherence and outcomes to direct oral anticoagulants among patients with atrial fibrillation: Findings from the veterans health administration. BMC Cardiovasc. Disord. 2017, 17, 236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osterberg, L.; Blaschke, T. Adherence to medication. N. Engl. J. Med. 2005, 353, 487–497. [Google Scholar] [CrossRef] [Green Version]
- Glader, E.L.; Sjölander, M.; Eriksson, M.; Lundberg, M. Persistent use of secondary preventive drugs declines rapidly during the first 2 years after stroke. Stroke 2010, 41, 397–401. [Google Scholar] [CrossRef]
- Manzoor, B.S.; Lee, T.A.; Sharp, L.K.; Walton, S.M.; Galanter, W.L.; Nutescu, E.A. Real-World Adherence and Persistence with Direct Oral Anticoagulants in Adults with Atrial Fibrillation. Pharmacotherapy 2017, 37, 1221–1230. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Caravaca, J.M.; Esteve-Pastor, M.A.; Roldán, V.; Marín, F.; Lip, G.Y.H. Non-vitamin K antagonist oral anticoagulants: Impact of non-adherence and discontinuation. Expert Opin. Drug Saf. 2017, 16, 1051–1062. [Google Scholar] [CrossRef] [PubMed]
- Shiga, T.; Naganuma, M.; Nagao, T.; Maruyama, K.; Suzuki, A.; Murasaki, K.; Hagiwara, N. Persistence of non-vitamin K antagonist oral anticoagulant use in Japanese patients with atrial fibrillation: A single-center observational study. J. Arrhythm. 2015, 31, 339–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kimmel, S.E.; Chen, Z.; Price, M.; Parker, C.S.; Metlay, J.P.; Christie, J.D.; Brensinger, C.M.; Newcomb, C.W.; Samaha, F.F.; Gross, R. The influence of patient adherence on anticoagulation control with warfarin: Results from the International Normalized Ratio Adherence and Genetics (IN-RANGE) Study. Arch. Intern. Med. 2007, 167, 229–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deshpande, C.G.; Kogut, S.; Laforge, R.; Willey, C. Impact of medication adherence on risk of ischemic stroke, major bleeding and deep vein thrombosis in atrial fibrillation patients using novel oral anticoagulants. Curr. Med. Res. Opin. 2018, 34, 1285–1292. [Google Scholar] [CrossRef] [PubMed]
- Obamiro, K.O.; Chalmers, L.; Bereznicki, L.R. A summary of the literature evaluating adherence and persistence with oral anticoagulants in atrial fibrillation. Am. J. Cardiovasc. Drugs. 2016, 16, 349–363. [Google Scholar] [CrossRef]
- Kneeland, P.P.; Fang, M.C. Current issues in patient adherence and persistence: Focus on anticoagulants for the treatment and prevention of thromboembolism. Patient Prefer. Adherence 2010, 4, 51–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashjian, E.; Kurtz, B.; Renner, E.; Yeshe, R.; Barnes, G.D. Evaluation of a pharmacist-led outpatient direct oral anticoagulant service. Am. J. Health Syst. Pharm. 2017, 74, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Shore, S.; Ho, P.M.; Lambert-Kerzner, A.; Glorioso, T.J.; Carey, E.P.; Cunningham, F.; Longo, L.; Jackevicius, C.; Rose, A.; Turakhia, M.P. Site-level variation in and practices associated with dabigatran adherence. JAMA 2015, 313, 1443–1450. [Google Scholar] [CrossRef] [PubMed]
- Steffel, J.; Verhamme, P.; Potpara, T.S.; Albaladejo, P.; Antz, M.; Desteghe, L.; Haeusler, K.G.; Oldgren, J.; Reinecke, H.; Roldan-Schilling, V.; et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur. Heart J. 2018, 39, 1330–1393. [Google Scholar] [CrossRef] [Green Version]

| Characteristics | Cerebral Infarction Cases (before Matching) | Controls (before Matching) | p Value |
|---|---|---|---|
| (N = 86, Mean ± S.D.) | (N = 380, Mean ± S.D.) | ||
| Age | 81.4 ± 6.6 | 77.6 ± 9.5 | <0.001 ** |
| Sex M/F | 51/35 | 250/130 | 0.256 * |
| Creatinine clearance (CCr, mL/min) | 53.0 ± 20.7 | 55.3 ± 26.3 | 0.471 ** |
| DOAC | |||
| Dabigatran | 10 | 42 | 0.519 * |
| Rivaroxaban | 35 | 125 | |
| Apixaban | 21 | 103 | |
| Edoxaban | 20 | 110 | |
| CHADS2 score | 2.90 ± 1.15 | 2.53 ± 1.30 | 0.018 ** |
| With antiplatelets | 11 (12.8%) | 61 (16.0%) | 0.450 * |
| History of cancer | 11 (12.8%) | 108 (28.4%) | 0.003 * |
| DOAC | Overdose | Appropriate Dose | Underdose | |
|---|---|---|---|---|
| Appropriate Standard Dose | Appropriate Low Dose | |||
| Dose/Criteria | Standard/Low | Standard/Standard | Low/Low | Low/Standard |
| Dabigatran | 150 mg twice a day | 150 mg twice a day | 110 mg twice a day | 110 mg twice a day |
| Age ≥ 70 | Does not meet the low-dose criteria | Age ≥ 70 | Does not meet the low-dose criteria | |
| 30 ≤ CCr ≤ 50 mL/min | 30 ≤ CCr ≤ 50 mL/min | |||
| Rivaroxaban | 15 mg once a day | 15 mg once a day | 10 mg once a day | 10 mg once a day |
| 15 ≤ CCr ≤ 50 mL/min | Does not meet the low-dose criteria | 15 ≤ CCr ≤ 50 mL/min | Does not meet the low-dose criteria | |
| Apixaban | 5 mg twice a day | 5 mg twice a day | 2.5 mg twice a day | 2.5 mg twice a day |
| Age ≥ 80 | Does not meet the low-dose criteria | Age ≥ 80 | Does not meet the low-dose criteria | |
| BW ≤ 60 kg | BW ≤ 60 kg | |||
| SCr ≥ 1.5 mg/dL | SCr ≥ 1.5 mg/dL | |||
| Edoxaban | 60 mg once a day | 60 mg once a day | 30 mg once a day | 30 mg once a day |
| BW ≤ 60 kg | Does not meet the low-dose criteria | BW ≤ 60 kg | Does not meet the low-dose criteria | |
| 15 ≤ CCr ≤ 50 mL/min | 15 ≤ CCr ≤ 50 mL/min | |||
| Characteristics | Cerebral Infarction Matched Cases | Matched Controls | p Value |
|---|---|---|---|
| (N = 58, Mean ± S.D.) | (N = 232, Mean ± S.D.) | ||
| Age | 78.7 ± 6.5 | 78.0 ± 10.0 | 0.206 ** |
| Over 80 years old | 30 | 120 | 1.000 * |
| Sex M/F | 37/21 | 143/89 | 0.762 * |
| Creatinine clearance (CCr, mL/min) | 53.2 ± 20.3 | 55.7 ± 26.3 | 0.703 ** |
| DOAC | |||
| Dabigatran | 8 | 22 | 0.271 * |
| Rivaroxaban | 26 | 88 | |
| Apixaban | 11 | 63 | |
| Edoxaban | 13 | 66 | |
| CHADS2 score | 2.60 ± 1.12 | 2.60 ± 1.11 | 1.000 ** |
| With antiplatelets | 6 (10.3%) | 43 (18.5%) | 0.137 * |
| History of cancer | 6 (10.3%) | 24 (10.3%) | 1.000 * |
| Factor | Adjusted Odds Ratio | p Value |
|---|---|---|
| (95% CI) | ||
| Medication adherence (II)/(I) | 1.69 (0.62–4.60) | 0.301 |
| Medication adherence (III)/(I) | 9.69 (3.86–24.3) | <0.001 * |
| Medication adherence (III)/(II) | 5.72 (1.64–19.9) | 0.006 * |
| DOAC dosage (b)/(a) | 0.82 (0.25–2.74) | 0.758 |
| DOAC dosage (c)/(a) | 0.46 (0.11–1.84) | 0.271 |
| DOAC dosage (c)/(b) | 0.55 (0.23–1.32) | 0.183 |
| One dose package service for dispensing | 0.70 (0.35–1.42) | 0.330 |
| Living alone (absence of a medication supporter) | 0.93 (0.46–1.88) | 0.845 |
| Number of daily doses (twice or more) | 1.41 (0.71–2.83) | 0.330 |
| Over 80 years old | 0.91 (0.45–1.85) | 0.794 |
| CHADS2 score | 1.03 (0.74–1.43) | 0.850 |
| History of cancer | 1.32 (0.47–3.65) | 0.597 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akagi, Y.; Iketaki, A.; Nakamura, R.; Yamamura, S.; Endo, M.; Morikawa, K.; Oikawa, S.; Ohta, T.; Tatsumi, S.; Suzuki, T.; et al. Association between Cerebral Infarction Risk and Medication Adherence in Atrial Fibrillation Patients Taking Direct Oral Anticoagulants. Healthcare 2021, 9, 1313. https://doi.org/10.3390/healthcare9101313
Akagi Y, Iketaki A, Nakamura R, Yamamura S, Endo M, Morikawa K, Oikawa S, Ohta T, Tatsumi S, Suzuki T, et al. Association between Cerebral Infarction Risk and Medication Adherence in Atrial Fibrillation Patients Taking Direct Oral Anticoagulants. Healthcare. 2021; 9(10):1313. https://doi.org/10.3390/healthcare9101313
Chicago/Turabian StyleAkagi, Yuuki, Akiko Iketaki, Reiko Nakamura, Shigeo Yamamura, Minori Endo, Keisuke Morikawa, Shun Oikawa, Takahiro Ohta, Shimpei Tatsumi, Takafumi Suzuki, and et al. 2021. "Association between Cerebral Infarction Risk and Medication Adherence in Atrial Fibrillation Patients Taking Direct Oral Anticoagulants" Healthcare 9, no. 10: 1313. https://doi.org/10.3390/healthcare9101313
APA StyleAkagi, Y., Iketaki, A., Nakamura, R., Yamamura, S., Endo, M., Morikawa, K., Oikawa, S., Ohta, T., Tatsumi, S., Suzuki, T., Mizushima, A., Koido, K., & Takahashi, T. (2021). Association between Cerebral Infarction Risk and Medication Adherence in Atrial Fibrillation Patients Taking Direct Oral Anticoagulants. Healthcare, 9(10), 1313. https://doi.org/10.3390/healthcare9101313