Feasibility, Acceptability and Limitations of Speech and Language Telerehabilitation during COVID-19 Lockdown: A Qualitative Research Study on Clinicians’ Perspectives
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Outcomes
- Level of knowledge and familiarity with TR before COVID-19 pandemic, that we called “familiarity”.
- Opinion about the importance of providing treatments through TR systems in the context of the country lockdown, that we called “importance”.
- Opinion on the feasibility of TR treatments in different fields of speech-language rehabilitation, that we called “feasibility”.
- Opinion on the use of TR as an alternative form of speech-language treatment. This was called “alternative form”.
- SLTs’ judgements on the comparison between TR and face-to-face treatment, that was called “comparison”.
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Between Group Comparison
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Rutkowska, A.; Kacperak, K.; Rutkowski, S.; Cacciante, L.; Kiper, P.; Szczegielniak, J. The Impact of Isolation Due to COVID-19 on Physical Activity Levels in Adult Students. Sustainability 2021, 13, 446. [Google Scholar] [CrossRef]
- Dorsey, E.R.; Topol, E.J. State of Telehealth. N. Engl. J. Med. 2016, 375, 154–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brennan, D.; Tindall, L.; Theodoros, D.; Brown, J.; Campbell, M.; Christiana, D.; Smith, D.; Cason, J.; Lee, A. A blueprint for telerehabilitation guidelines. Int. J. Telerehabil. 2010, 2, 31–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howe, T.J.; Worrall, L.E.; Hickson, L.M.H. Observing people with aphasia: Environmental factors that influence their community participation. Aphasiology 2008, 22, 618–643. [Google Scholar] [CrossRef]
- Mashima, P.A.; Doarn, C.R. Overview of telehealth activities in speech-language pathology. Telemed. J. E. Health 2008, 14, 1101–1117. [Google Scholar] [CrossRef] [PubMed]
- Cherney, L.R.; van Vuuren, S. Telerehabilitation, virtual therapists, and acquired neurologic speech and language disorders. Semin. Speech Lang. 2012, 33, 243–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hall, N.; Boisvert, M.; Steele, R. Telepractice in the assessment and treatment of individuals with aphasia: A systematic review. Int. J. Telerehabil. 2013, 5, 27–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Constantinescu, G.; Theodoros, D.; Russell, T.; Ward, E.; Wilson, S.; Wootton, R. Assessing disordered speech and voice in Parkinson’s disease: A telerehabilitation application. Int. J. Lang. Commun. Disord. 2010, 45, 630–644. [Google Scholar] [CrossRef] [PubMed]
- Agostini, M.; Garzon, M.; Benavides-Varela, S.; De Pellegrin, S.; Bencini, G.; Rossi, G.; Rosadoni, S.; Mancuso, M.; Turolla, A.; Meneghello, F.; et al. Telerehabilitation in poststroke anomia. BioMed Res. Int. 2014, 2014, 706909. [Google Scholar] [CrossRef]
- Ora, H.P.; Kirmess, M.; Brady, M.C.; Sorli, H.; Becker, F. Technical Features, Feasibility, and Acceptability of Augmented Telerehabilitation in Post-stroke Aphasia-Experiences From a Randomized Controlled Trial. Front. Neurol. 2020, 11, 671. [Google Scholar] [CrossRef]
- Latimer, N.R.; Dixon, S.; Palmer, R. Cost-utility of self-managed computer therapy for people with aphasia. Int. J. Technol. Assess Health Care 2013, 29, 402–409. [Google Scholar] [CrossRef]
- Wilson, L.; Onslow, M.; Lincoln, M. Telehealth adaptation of the Lidcombe Program of Early Stuttering Intervention: Five case studies. Am. J. Speech Lang. Pathol. 2004, 13, 81–93. [Google Scholar] [CrossRef]
- O’Brian, S.; Packman, A.; Onslow, M. Telehealth delivery of the Camperdown Program for adults who stutter: A phase I trial. J. Speech Lang. Hear. Res. 2008, 51, 184–195. [Google Scholar] [CrossRef]
- Sicotte, C.; Lehoux, P.; Fortier-Blanc, J.; Leblanc, Y. Feasibility and outcome evaluation of a telemedicine application in speech-language pathology. J. Telemed. Telecare 2003, 9, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Rettinger, L.; Klupper, C.; Werner, F.; Putz, P. Changing attitudes towards teletherapy in Austrian therapists during the COVID-19 pandemic. J. Telemed. Telecare 2021, 1357633X20986038. [Google Scholar] [CrossRef]
- Scott Kruse, C.; Karem, P.; Shifflett, K.; Vegi, L.; Ravi, K.; Brooks, M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J. Telemed. Telecare 2018, 24, 4–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for Reporting Qualitative Research: A Synthesis of Recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Preedy, V.R.; Watson, R.R. Likert Scale. In Handbook of Disease Burdens and Quality of Life Measures; Preedy, V.R., Watson, R.R., Eds.; Springer: New York, NY, USA, 2010; p. 4248. [Google Scholar]
- Bland, J.M.; Altman, D.G. Statistics notes: Cronbach’s alpha. BMJ 1997, 314, 572. [Google Scholar] [CrossRef] [Green Version]
- Litosseliti, L.; Leadbeater, C. Speech and language therapy/pathology: Perspectives on a gendered profession. Int. J. Lang. Commun. Disord. 2013, 48, 90–101. [Google Scholar] [CrossRef]
- Bergmann, S.; Toussaint, K.A.; Niland, H.; Sansing, E.M.; Armshaw, G.; Baltazar, M. Adapting Direct Services for Telehealth: A Practical Tutorial. Behav. Anal. Pract. 2021, 13, 306–311. [Google Scholar] [CrossRef]
- Miller, M.J.; Pak, S.S.; Keller, D.R.; Barnes, D.E. Evaluation of Pragmatic Telehealth Physical Therapy Implementation During the COVID-19 Pandemic. Phys. Ther. 2021, 101, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Donzelli, S.; Negrini, A.; Negrini, A.; Romano, M.; Zaina, F. Feasibility and Acceptability of Telemedicine to Substitute Outpatient Rehabilitation Services in the COVID-19 Emergency in Italy: An Observational Everyday Clinical-Life Study. Arch. Phys. Med. Rehabil. 2020, 101, 2027–2032. [Google Scholar] [CrossRef]
- Aggarwal, K.; Patel, R.; Ravi, R. Uptake of telepractice among speech-language therapists following COVID-19 pandemic in India. Speech Lang. Hear. 2020, 24, 1–7. [Google Scholar] [CrossRef]
- Mair, F.S.; May, C.; O’Donnell, C.; Finch, T.; Sullivan, F.; Murray, E. Factors that promote or inhibit the implementation of e-health systems: An explanatory systematic review. Bull. World Health Organ. 2012, 90, 357–364. [Google Scholar] [CrossRef] [Green Version]
- Plaete, J.; Crombez, G.; DeSmet, A.; Deveugele, M.; Verloigne, M.; De Bourdeaudhuij, I. What do general practitioners think about an online self-regulation programme for health promotion? Focus group interviews. BMC Fam. Pract. 2015, 16, 3. [Google Scholar] [CrossRef] [Green Version]
- Silva, G.S.; Farrell, S.; Shandra, E.; Viswanathan, A.; Schwamm, L.H. The status of telestroke in the United States: A survey of currently active stroke telemedicine programs. Stroke 2012, 43, 2078–2085. [Google Scholar] [CrossRef]
- Abbott-Gaffney, C.; Jacobs, K. Telehealth in school-based practice: Perceived viability to bridge global OT practitioner shortages prior to COVID-19 global health emergency. Work 2020, 67, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Ora, H.P.; Kirmess, M.; Brady, M.C.; Partee, I.; Hognestad, R.B.; Johannessen, B.B.; Thommessen, B.; Becker, F. The effect of augmented speech-language therapy delivered by telerehabilitation on poststroke aphasia-a pilot randomized controlled trial. Clin. Rehabil. 2020, 34, 369–381. [Google Scholar] [CrossRef]
- Agostini, M.; Moja, L.; Banzi, R.; Pistotti, V.; Tonin, P.; Venneri, A.; Turolla, A. Telerehabilitation and recovery of motor function: A systematic review and meta-analysis. J. Telemed. Telecare 2015, 21, 202–213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cotelli, M.; Manenti, R.; Brambilla, M.; Gobbi, E.; Ferrari, C.; Binetti, G.; Cappa, S.F. Cognitive telerehabilitation in mild cognitive impairment, Alzheimer’s disease and frontotemporal dementia: A systematic review. J. Telemed. Telecare 2019, 25, 67–79. [Google Scholar] [CrossRef]
- Cacciante, L.; Kiper, P.; Garzon, M.; Baldan, F.; Federico, S.; Turolla, A.; Agostini, M. Telerehabilitation for people with aphasia: A systematic review and meta-analysis. J. Commun. Disord. 2021, 92, 106111. [Google Scholar] [CrossRef] [PubMed]
- Molfenter, T.; Boyle, M.; Holloway, D.; Zwick, J. Trends in telemedicine use in addiction treatment. Addict. Sci. Clin. Pract. 2015, 10, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ross, J.; Stevenson, F.; Lau, R.; Murray, E. Exploring the challenges of implementing e-health: A protocol for an update of a systematic review of reviews. BMJ Open 2015, 5, e006773. [Google Scholar] [CrossRef] [PubMed]
- Stroetmann, K.A.; Artmann, J.; Stroetmann, V. Developing national eHealth infrastructures—Results and lessons from Europe. AMIA Annu. Symp. Proc. 2011, 2011, 1347–1354. [Google Scholar] [PubMed]
- Llorens, R.; Noe, E.; Colomer, C.; Alcaniz, M. Effectiveness, usability, and cost-benefit of a virtual reality-based telerehabilitation program for balance recovery after stroke: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2015, 96, 418–425.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molini-Avejonas, D.R.; Rondon-Melo, S.; Amato, C.A.; Samelli, A.G. A systematic review of the use of telehealth in speech, language and hearing sciences. J. Telemed. Telecare 2015, 21, 367–376. [Google Scholar] [CrossRef]
| Characteristics | Participants Data | Respondents (Percentage) |
|---|---|---|
| Sex (n/%) | Men | 9 (6.6%) |
| Women | 127 (93.4%) | |
| Year (n/%) | 22–30 | 69 (50.7%) |
| 31–39 | 28 (20.6%) | |
| 40–48 | 22 (16.2%) | |
| 49–57 | 13 (9.6%) | |
| 58–66 | 4 (2.9%) | |
| Field of intervention (n/%) | Adult and geriatric | 19 (14%) |
| Paedriatic | 117 (86%) | |
| Type of patients treated (n/%) | SLI | 111 (81.6%) |
| Learning disorders | 101 (74.3%) | |
| ASD | 75 (55.1%) | |
| Aphasia | 33 (24.3%) | |
| Dysarthria | 33 (24.3%) | |
| Dysphonia | 32 (23.5%) | |
| Hearing loss | 30 (22.1%) | |
| Dysphagia | 29 (21.3%) | |
| Deafness | 25 (18.4%) | |
| Apraxia | 22 (16.2%) | |
| Intellectual disability | 2 (1.5%) | |
| Others | 1 (1%) |
| Domains | Answers | Total (n = 136) | TR (n = 117) | Traditional (n = 19) | p-Value * |
|---|---|---|---|---|---|
| Familiarity | Very Low | 66 (48.53) | 57 (48.72) | 9 (47.36) | 0.91 |
| Low | 36 (26.47) | 31 (26.50) | 5 (26.32) | 0.98 | |
| Neutral | 20 (14.71) | 18 (15.38) | 2 (10.53) | 0.58 | |
| High | 9 (6.62) | 7 (5.98) | 2 (10.53) | 0.46 | |
| Very High | 5 (3.68) | 4 (3.42) | 1 (5.26) | 0.69 | |
| Importance | Very Low | 2 (1.47) | 0 (0.00) | 2 (10.53) | - |
| Low | 6 (4.41) | 3 (2.56) | 3 (15.79) | 0.01 | |
| Neutral | 21 (15.44) | 15 (12.82) | 6 (31.57) | 0.04 | |
| High | 40 (29.41) | 37 (31.63) | 3 (15.79) | 0.16 | |
| Very High | 67 (49.26) | 62 (52.99) | 5 (26.32) | 0.03 | |
| Feasibility | Very Low | 7 (5.15) | 2 (1.71) | 5 (26.32) | <0.01 |
| Low | 19 (13.97) | 12 (10.26) | 7 (36.84) | <0.01 | |
| Neutral | 56 (41.18) | 49 (41.88) | 7 (36.84) | 0.68 | |
| High | 49 (36.03) | 49 (41.88) | 0 (0.00) | - | |
| Very High | 5 (3.68) | 5 (4.27) | 0 (0.00) | - | |
| Alternative form | Very Low | 8 (5.88) | 3 (2.56) | 5 (26.32) | <0.01 |
| Low | 14 (10.29) | 11 (9.40) | 3 (15.79) | 0.40 | |
| Neutral | 42 (30.88) | 36 (30.77) | 6 (31.57) | 0.94 | |
| High | 47 (34.56) | 42 (35.90) | 5 (26.32) | 0.42 | |
| Very High | 25 (18.38) | 25 (21.37) | 0 (0.00) | - | |
| Comparison | Much Worse | 6 (4.41) | 2 (1.71) | 4 (21.05) | <0.01 |
| Worse | 102 (75.00) | 87 (74.36) | 15 (78.95) | 0.67 | |
| Neutral | 26 (19.12) | 26 (22.22) | 0 (0.00) | - | |
| Better | 2 (1.47) | 2 (1.71) | 0 (0.00) | - | |
| Much Better | 0 (0.00) | 0 (0.00) | 0 (0.00) | - |
| Domains | Answers | TR (n = 117) | Traditional (n = 19) | p-Value * |
|---|---|---|---|---|
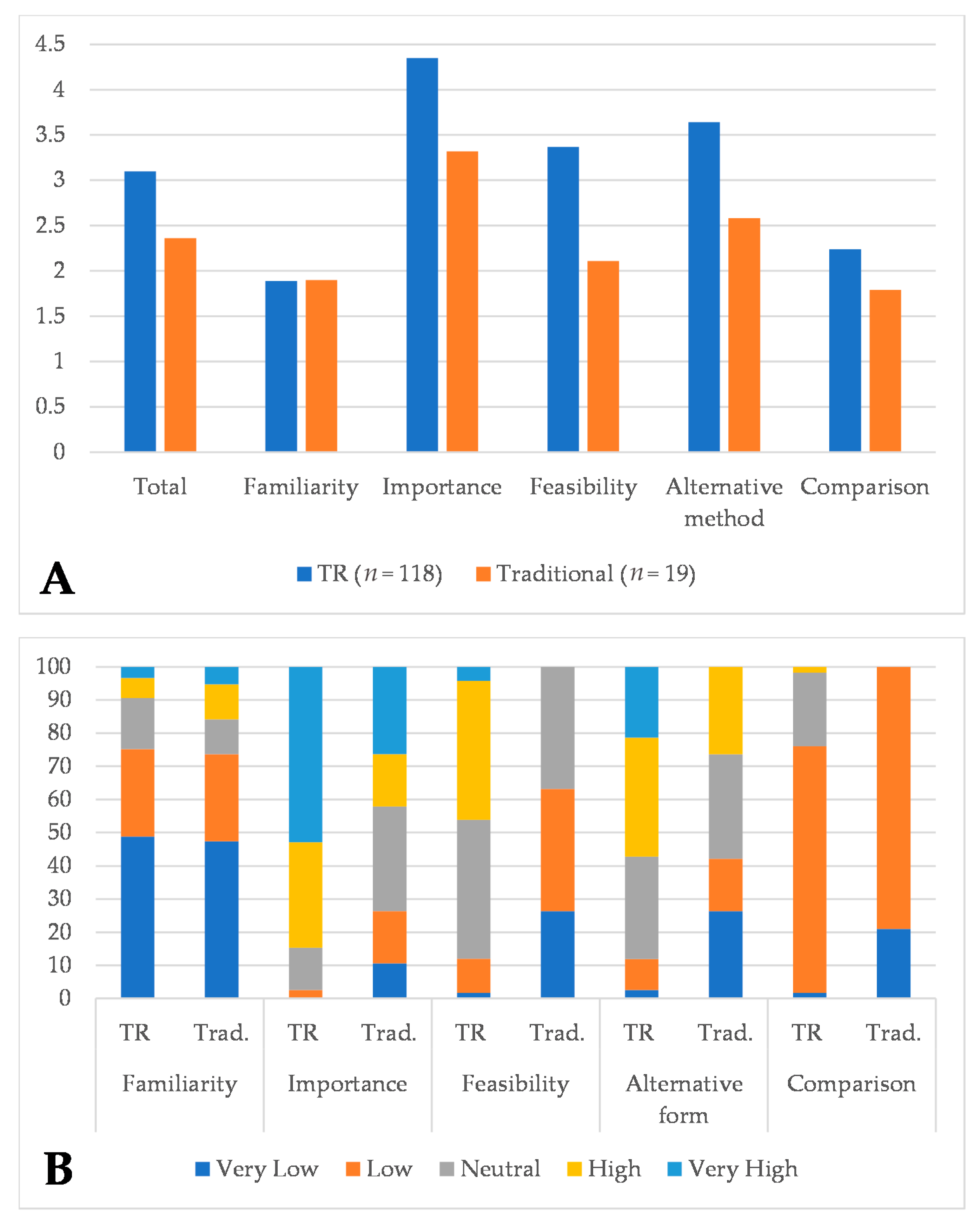
| Total | Mean (SD) | 3.10 (0.60) | 2.36 (0.65) | <0.001 |
| Median (IQR) | 3.20 (2.6–3.6) | 2.60 (2.0–2.8) | ||
| Familiarity | Mean (SD) | 1.89 (1.09) | 1.90 (1.04) | 0.81 |
| Median (IQR) | 2 (1.0–2.5) | 2 (1.0–3.0) | ||
| Importance | Mean (SD) | 4.35 (0.80) | 3.32 (1.34) | 0.001 |
| Median (IQR) | 5 (4.0–5.0) | 3 (2.0–5.0) | ||
| Feasibility | Mean (SD) | 3.37 (0.79) | 2.11 (0.81) | <0.001 |
| Median (IQR) | 3 (3.0–4.0) | 2 (1.0–3.0) | ||
| Alternative method | Mean (SD) | 3.64 (1.00) | 2.58 (1.17) | 0.001 |
| Median (IQR) | 4 (3.0–4.0) | 3 (1.0–4.0) | ||
| Comparison | Mean (SD) | 2.24 (0.50) | 1.79 (0.42) | <0.001 |
| Median (IQR) | 2 (2.0–2.00) | 2 (2.0–2.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cacciante, L.; Cieślik, B.; Rutkowski, S.; Rutkowska, A.; Kacperak, K.; Kuligowski, T.; Kiper, P. Feasibility, Acceptability and Limitations of Speech and Language Telerehabilitation during COVID-19 Lockdown: A Qualitative Research Study on Clinicians’ Perspectives. Healthcare 2021, 9, 1503. https://doi.org/10.3390/healthcare9111503
Cacciante L, Cieślik B, Rutkowski S, Rutkowska A, Kacperak K, Kuligowski T, Kiper P. Feasibility, Acceptability and Limitations of Speech and Language Telerehabilitation during COVID-19 Lockdown: A Qualitative Research Study on Clinicians’ Perspectives. Healthcare. 2021; 9(11):1503. https://doi.org/10.3390/healthcare9111503
Chicago/Turabian StyleCacciante, Luisa, Błażej Cieślik, Sebastian Rutkowski, Anna Rutkowska, Katarzyna Kacperak, Tomasz Kuligowski, and Pawel Kiper. 2021. "Feasibility, Acceptability and Limitations of Speech and Language Telerehabilitation during COVID-19 Lockdown: A Qualitative Research Study on Clinicians’ Perspectives" Healthcare 9, no. 11: 1503. https://doi.org/10.3390/healthcare9111503
APA StyleCacciante, L., Cieślik, B., Rutkowski, S., Rutkowska, A., Kacperak, K., Kuligowski, T., & Kiper, P. (2021). Feasibility, Acceptability and Limitations of Speech and Language Telerehabilitation during COVID-19 Lockdown: A Qualitative Research Study on Clinicians’ Perspectives. Healthcare, 9(11), 1503. https://doi.org/10.3390/healthcare9111503







