Pathways Linking Health Literacy to Self-Management in People with Type 2 Diabetes
Abstract
:1. Introduction
2. Methods
2.1. Sample and Data Collection
2.2. Ethical Considerations
2.3. Measures
2.3.1. Health Literacy
2.3.2. Social Isolation
2.3.3. Self-Efficacy
2.3.4. Self-Management
2.3.5. Demographic and Medical Information
2.4. Statistical Analyses
3. Results
3.1. Participant Characteristics and Study Variables
3.2. Correlations among Study Variables
3.3. Diabetes Education as a Covariate
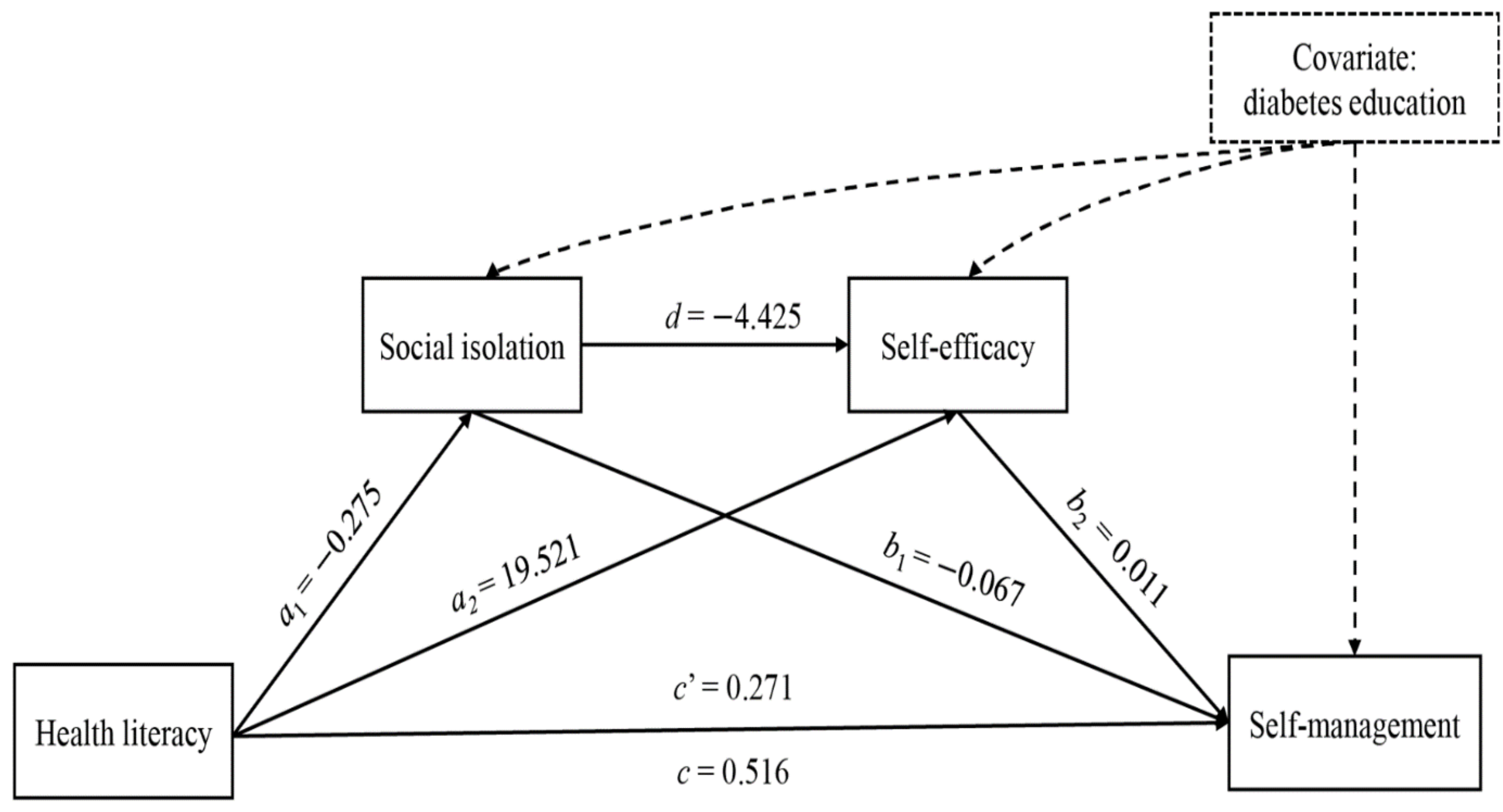
3.4. Mediation Model Analysis While Controlling for Diabetes Education
4. Discussion
Strength and Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Diabetes Federation. IDF Diabetes Atlas 2019. Available online: http://www.diabetesatlas.org (accessed on 5 July 2021).
- American Association of Diabetes Educators. An effective model of diabetes care and education: Revising the AADE7 self-care behaviors®. Diabetes Educ. 2020, 46, 139–160. [Google Scholar] [CrossRef]
- Nutbeam, D. Health promotion glossary. Health Promot. Int. 1998, 13, 349–364. [Google Scholar] [CrossRef]
- Paasche-Orlow, M.K.; Wolf, M.S. The causal pathways linking health literacy to health outcomes. Am. J. Health Behav. 2007, 31, S19–S26. [Google Scholar] [CrossRef]
- Guo, X.M.; Zhai, X.; Hou, B.R. Adequacy of health literacy and its effect on diabetes self-management: A meta-analysis. Aust. J. Prim. Health 2020, 26, 458–465. [Google Scholar] [CrossRef]
- Lee, E.H.; Lee, Y.W.; Chae, D.; Lee, K.W.; Chung, J.O.; Hong, S.; Kim, S.H.; Kang, E.H. A new self-management scale with a hierarchical structure for patients with type 2 diabetes. Asian Nurs. Res. 2020, 14, 249–256. [Google Scholar] [CrossRef]
- Bailey, S.C.; Brega, A.G.; Crutchfield, T.M.; Elasy, T.; Herr, H.; Kaphingst, K.; Karter, A.J.; Moreland-Russell, S.; Osborn, C.Y.; Pignon, M.; et al. Update on health literacy and diabetes. Diabetes Educ. 2014, 40, 581–604. [Google Scholar] [CrossRef] [PubMed]
- Fransen, M.P.; von Wagner, C.; Essink-Bot, M.-L. Diabetes self-management in patients with low health literacy: Ordering findings from literature in a health literacy framework. Patient Educ. Couns. 2012, 88, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; W.H. Freeman: New York, NY, USA, 1997. [Google Scholar]
- Lee, E.H.; Lee, Y.W.; Moon, S.H. A structural equation model linking health literacy to self-efficacy, self-care activities, and health-related quality of life in patients with type 2 diabetes. Asian Nurs. Res. 2016, 10, 82–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.M.; Shiyanbola, O.O.; Chan, H.Y. A path model linking health literacy, medication self-efficacy, medication adherence, and glycemic control. Patient Educ. Couns. 2018, 101, 1906–1913. [Google Scholar] [CrossRef] [PubMed]
- Al Sayah, F.; Majumdar, S.R.; Williams, B.; Robertson, S.; Johnson, J.A. Health literacy and health outcomes in diabetes: A systematic review. J. Gen. Intern. Med. 2013, 28, 444–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Squiers, L.; Peinado, S.; Berkman, N.; Boudewyns, V.; McCormack, L. The health literacy skills framework. J. Health Commun. 2012, 17, 30–54. [Google Scholar] [CrossRef] [PubMed]
- Bohanny, W.; Wu, S.F.V.; Liu, C.Y.; Yeh, S.H.; Tsay, S.L.; Wang, T.J. Health literacy, self-efficacy, and self-care behaviors in patients with type 2 diabetes mellitus. J. Am. Assoc. Nurse Pract. 2013, 25, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Cudjoe, J.; Delva, S.; Cajita, M.; Han, H.R. Empirically tested health literacy frameworks. Health Lit. Res. Pract. 2020, 4, e22–e44. [Google Scholar] [CrossRef] [Green Version]
- Shankar, A.; McMunn, A.; Banks, J.; Steptoe, A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 2011, 30, 377–385. [Google Scholar] [CrossRef] [Green Version]
- Sentell, T.L.; Agner, J.L.; Davis, J.; Mannem, S.; Seto, T.B.; Valente, T.W.; Varwer, M.; Taira, D.A. Social networks in patients hospitalized with preventable conditions for heart disease and diabetes in Hawai ‘i by health literacy. Chronic Illn. 2021, 1742395320987892. [Google Scholar] [CrossRef]
- Geboers, B.; Reijneveld, S.A.; Jansen, C.J.; de Winter, A.F. Health literacy is associated with health behaviors and social factors among older adults: Results from the lifelines cohort study. J. Health Commun. 2016, 21 (Suppl. 2), 45–53. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.G.; Jackson, S.E.; Kobayashi, L.C.; Steptoe, A. Social isolation, health literacy, and mortality risk: Findings from the English longitudinal study of ageing. Health Psychol. 2018, 37, 160–169. [Google Scholar] [CrossRef]
- Kobayashi, L.C.; Steptoe, A. Social isolation, loneliness, and health behaviors at older ages: Longitudinal cohort study. Ann Behav. Med. 2018, 52, 582–593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schrempft, S.; Jackowska, M.; Hamer, M.; Steptoe, A. Associations between social isolation, loneliness, and objective physical activity in older men and women. BMC Public Health 2019, 19, 74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kadirvelu, A.; Sadasivan, S.; Ng, S.H. Social support in type II diabetes care: A case of too little, too late. Diabetes Metab. Syndr. Obes. 2012, 5, 407–417. [Google Scholar] [CrossRef] [Green Version]
- Suhl, E.; Bonsignore, P. Diabetes self-management education for older adults: General principles and practical application. Diabetes Spectr. 2006, 19, 234–240. [Google Scholar] [CrossRef] [Green Version]
- Köbling, T.; Váradi, Z.; Katona, E.; Somodi, S.; Kempler, P.; Páll, D.; Zrinyi, M. Predictors of dietary self-efficacy in high glycosylated hemoglobin A1c type 2 diabetic patients. J. Int. Med. Res. 2020, 48, 1–12. [Google Scholar] [CrossRef]
- Wu, F.; Sheng, Y. Social support network, social support, self-efficacy, health-promoting behavior and healthy aging among older adults: A pathway analysis. Arch. Gerontol. Geriatr. 2019, 85, 103934. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 2nd ed.; Guilford Publications: New York, NY, USA, 2013. [Google Scholar]
- Tofighi, D.; Kelley, K. Indirect effects in sequential mediation models: Evaluating methods for hypothesis testing and confidence interval formation. Multivar. Behav. Res. 2020, 55, 188–210. [Google Scholar] [CrossRef]
- Pieters, R. Meaningful mediation analysis: Plausible causal inference and informative communication. J. Consum. Res. 2017, 44, 692–716. [Google Scholar] [CrossRef]
- Lee, E.H.; Lee, Y.W.; Lee, K.W.; Nam, M.; Kim, S.H. A new comprehensive diabetes health literacy scale: Development and psychometric evaluation. Int. J. Nurs. Stud. 2018, 88, 1–8. [Google Scholar] [CrossRef]
- Lee, E.H.; van der Bijl, J.; Shortridge-Baggett, L.M.; Han, S.J.; Moon, S.H. Psychometric properties of the diabetes management self-efficacy scale in Korean patients with type 2 diabetes. Int. J. Endocrinol. 2015, 2015, 780701. [Google Scholar] [CrossRef]
- van der Bijl, J.; Poelgeest-Eeltink, A.V.; Shortridge-Baggett, L. The psychometric properties of the diabetes management self-efficacy scale for patients with type 2 diabetes mellitus. J. Adv. Nurs. 1999, 30, 352–359. [Google Scholar] [CrossRef]
- Kim, S.; Love, F.; Quistberg, D.A.; Shea, J.A. Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care 2004, 27, 2980–2982. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mancuso, J.M. Impact of health literacy and patient trust on glycemic control in an urban USA population. Nurs. Health Sci. 2010, 12, 94–104. [Google Scholar] [CrossRef]
- Osborn, C.Y.; Bains, S.S.; Egede, L.E. Health literacy, diabetes self-care, and glycemic control in adults with type 2 diabetes. Diabetes Technol. Ther. 2010, 12, 913–919. [Google Scholar] [CrossRef] [Green Version]
- Nurss, J.; Parker, R.; Williams, M.; Baker, D. TOFHLA: Test of Functional Health Literacy in Adults, 2nd ed.; Peppercorn: Snow Camp, NC, USA, 2001. [Google Scholar]
- Bass, P.F.; Wilson, J.F.; Griffith, C.H. A shortened instrument for literacy screening. J. Gen. Intern. Med. 2003, 18, 1036–1038. [Google Scholar] [CrossRef] [Green Version]
- Lee, E.H.; Kim, C.J.; Lee, J.; Moon, S.H. Self-administered health literacy instruments for people with diabetes: Systematic review of measurement properties. J. Adv. Nurs. 2017, 73, 2035–2048. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Takeuchi, T.; Yano, E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care 2008, 31, 874–879. [Google Scholar] [CrossRef] [Green Version]
- Parikh, N.S.; Parker, R.M.; Nurss, J.R.; Baker, D.W.; Williams, M.V. Shame and health literacy: The unspoken connection. Patient Educ. Couns. 1996, 27, 33–39. [Google Scholar] [CrossRef]
- Lee, Y.J.; Shin, S.J.; Wang, R.H.; Lin, K.D.; Lee, Y.L.; Wang, Y.H. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ. Couns. 2016, 99, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Wolff, K.; Cavanaugh, K.; Malone, R.; Hawk, V.; Gregory, B.P.; Davis, D.; Wallston, K.; Rothman, R.L. The diabetes literacy and numeracy education toolkit (DLNET): Materials to facilitate diabetes education and management in patients with low literacy and numeracy skills. Diabetes Educ. 2009, 35, 233–245. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.H.; Lee, A. Health-literacy-sensitive diabetes self-management interventions: A systematic review and meta-analysis. Worldviews Evid.-Based Nurs. 2016, 13, 324–333. [Google Scholar] [CrossRef]
- Jiang, X.; Wang, J.; Lu, Y.; Jiang, H.; Li, M. Self-efficacy-focused education in persons with diabetes: A systematic review and meta-analysis. Psychol. Res. Behav. Manag. 2019, 12, 67–79. [Google Scholar] [CrossRef] [Green Version]
- Toobert, D.J.; Hampson, S.E.; Glasgow, R.E. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care 2000, 23, 943–950. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Lee, E.H.; Chae, D.; Kim, C.J. Patient-reported outcome measures for diabetes self-care: A systematic review of measurement properties. Int. J. Nurs. Stud. 2020, 105, 103498. [Google Scholar] [CrossRef]
- Lee, J.; Lee, E.H.; Chae, D. Self-efficacy instruments for type 2 diabetes self-care: A systematic review of measurement properties. J. Adv. Nurs. 2020, 76, 2046–2059. [Google Scholar] [CrossRef] [PubMed]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Sobel, M.E. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol. Methodol. 1982, 13, 290–312. [Google Scholar] [CrossRef]
- Hayes, A.F.; Montoya, A.K.; Rockwood, N.J. The analysis of mechanisms and their contingencies: PROCESS versus structural equation modeling. Australas. Mark. J. 2017, 25, 76–81. [Google Scholar] [CrossRef]
| Variable | Category | n (%) | Mean (SD) |
|---|---|---|---|
| Age, years | ≤30 | 7 (1.3) | 60.35 (11.19) |
| 31–40 | 15 (2.9) | ||
| 41–50 | 69 (13.2) | ||
| 51–60 | 163 (31.1) | ||
| 61–70 | 174 (33.2) | ||
| ≥71 | 96 (18.3) | ||
| Gender | Male | 336 (64.1) | |
| Female | 188 (35.9) | ||
| Education status | Elementary school | 50 (9.5) | |
| Middle school | 74 (14.1) | ||
| High school | 208 (39.7) | ||
| College and above | 187 (35.7) | ||
| Others | 5 (1.0) | ||
| Monthly income, KRW | ≤3,000,000 | 278 (53.1) | |
| >3,000,000 | 246 (46.9) | ||
| Treatment regimen | OHA | 396 (75.6) | |
| OHA + insulin | 119 (22.7) | ||
| Insulin | 9 (1.7) | ||
| HbA1c | Controlled (<6.5%) | 133 (25.4) | 7.30 (1.27) |
| Uncontrolled (≥6.5%) | 391 (74.6) | ||
| Duration of disease, years | 11.77 (8.72) | ||
| Diabetes education | Yes | 396 (75.6) | |
| No | 128 (24.4) | ||
| Health literacy | 2.53 (0.88) | ||
| Social isolation | 1.07 (1.03) | ||
| Self-efficacy | 110.45 (32.56) | ||
| Self-management | 2.20 (0.79) |
| Variable | Health Literacy | Social Isolation | Self-Efficacy |
|---|---|---|---|
| Social isolation | –0.25 (p < 0.001) | ||
| Self-efficacy | 0.57 (p < 0.001) | –0.28 (p < 0.001) | |
| Self-management | 0.59 (p < 0.001) | –0.29 (p < 0.001) | 0.65 (p < 0.001) |
| Study variable | Diabetes Education | |||
|---|---|---|---|---|
| Yes Mean (SD) | No Mean (SD) | t | p | |
| Social isolation | 0.99 (1.06) | 1.31 (1.06) | –3.03 a | 0.003 |
| Self-efficacy | 113.60 (30.27) | 100.74 (37.28) | 3.54 a | 0.001 |
| Self-management | 2.28 (0.78) | 1.96 (0.79) | 4.70 | <0.001 |
| Product of Coefficient | 95% Bootstrap CI | |||
|---|---|---|---|---|
| Point Estimate | SE | Lower CI Limit | Upper CI Limit | |
| Total effect | ||||
| c | 0.516 | 0.032 | 0.453 | 0.580 |
| Direct effect | ||||
| c’ | 0.271 | 0.034 | 0.203 | 0.339 |
| Indirect effects | ||||
| a1b1 | 0.018 | 0.008 | 0.004 | 0.036 |
| a2b2 | 0.214 | 0.026 | 0.165 | 0.266 |
| a1db2 | 0.013 | 0.004 | 0.006 | 0.023 |
| Total indirect effects | ||||
| a1b1 + a2b2 + a1db2 | 0.245 | 0.026 | 0.196 | 0.299 |
| Pairwise comparisons between indirect effects | ||||
| a1b1 − a2b2 | –0.195 | 0.028 | –0.253 | –0.141 |
| a1b1 − a1db2 | 0.005 | 0.009 | –0.012 | 0.023 |
| a2b2 − a1db2 | 0.200 | 0.026 | 0.151 | 0.253 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, E.-H.; Lee, Y.W.; Chae, D.; Lee, K.-W.; Hong, S.; Kim, S.H.; Chung, J.O. Pathways Linking Health Literacy to Self-Management in People with Type 2 Diabetes. Healthcare 2021, 9, 1734. https://doi.org/10.3390/healthcare9121734
Lee E-H, Lee YW, Chae D, Lee K-W, Hong S, Kim SH, Chung JO. Pathways Linking Health Literacy to Self-Management in People with Type 2 Diabetes. Healthcare. 2021; 9(12):1734. https://doi.org/10.3390/healthcare9121734
Chicago/Turabian StyleLee, Eun-Hyun, Young Whee Lee, Duckhee Chae, Kwan-Woo Lee, Seongbin Hong, So Hun Kim, and Jin Ook Chung. 2021. "Pathways Linking Health Literacy to Self-Management in People with Type 2 Diabetes" Healthcare 9, no. 12: 1734. https://doi.org/10.3390/healthcare9121734






