Multidomain Social Determinants of Depressive Symptoms for the Elderly with Chronic Diseases: Evidence from the China Health and Retirement Longitudinal Study
Abstract
:1. Introduction
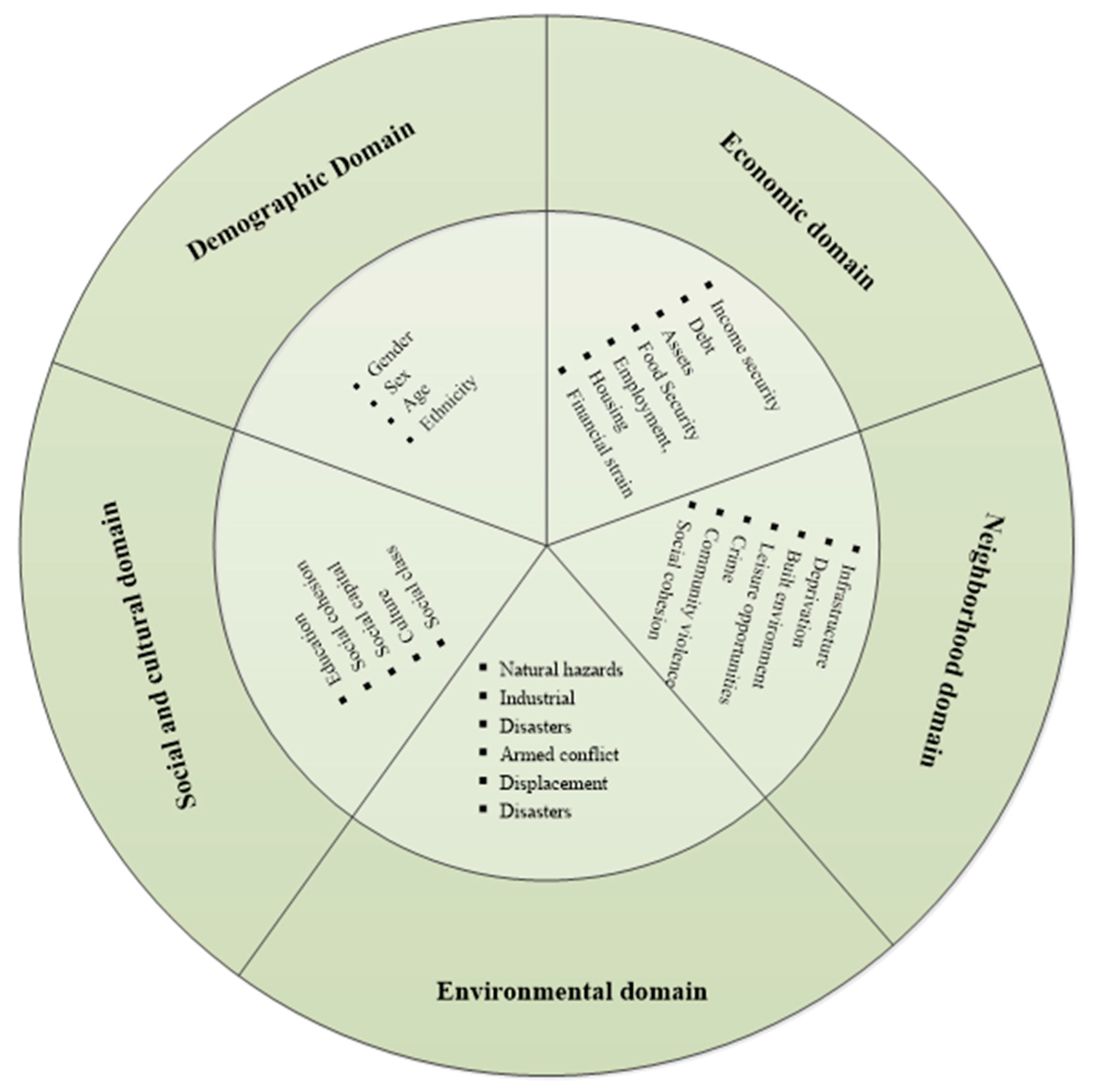
Conceptual Framework—Multidomain Social Determinants of Mental Disorders
2. Materials and Methods
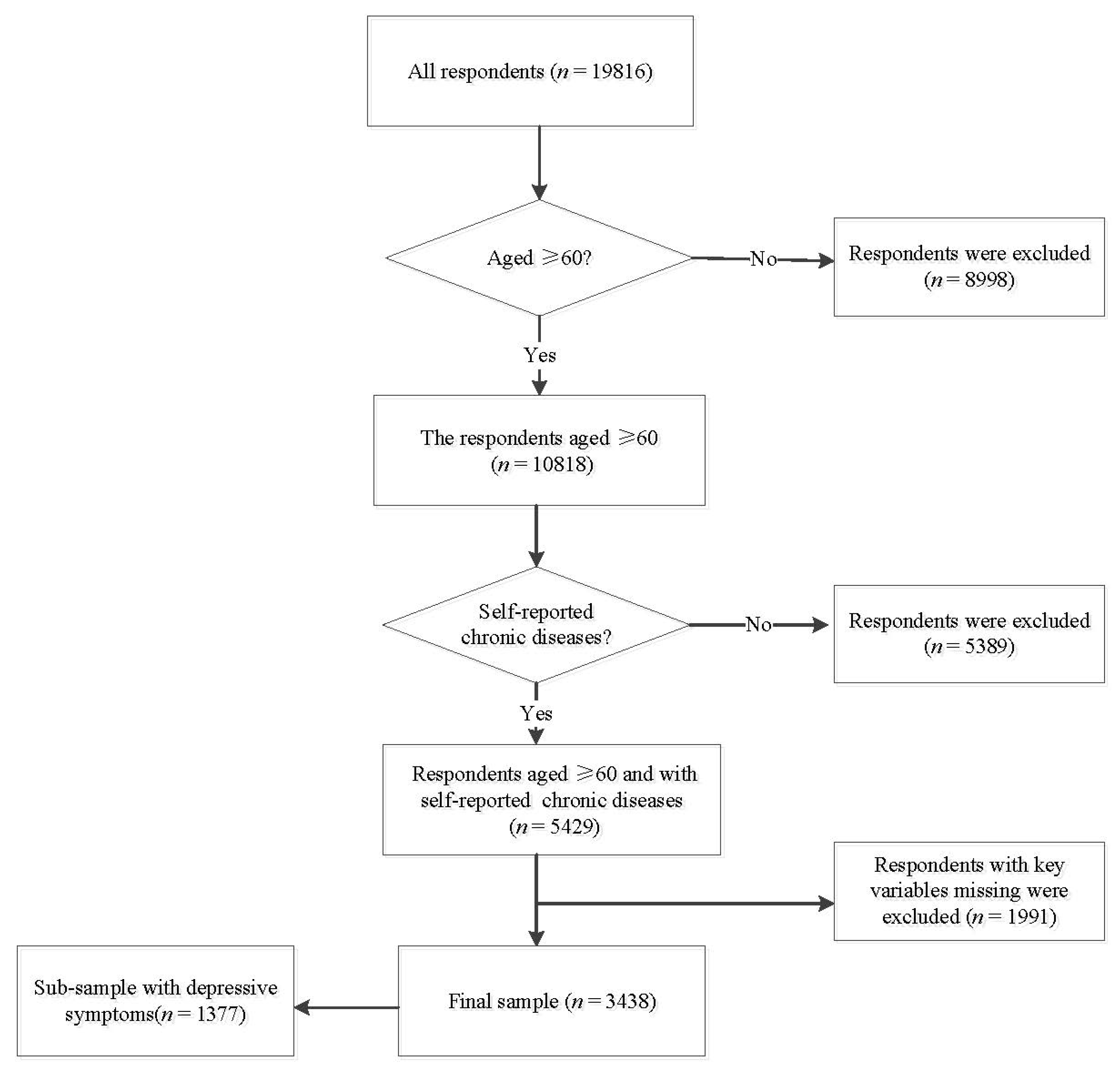
2.1. Sample
2.2. Outcome Variables
2.3. Independent Variables
2.4. Data Analysis
2.4.1. Stage One: Logistic Regression Model and Shapley Value Decomposition
2.4.2. Stage Two: Quantile Regression Models
3. Results
3.1. Characteristics of Respondents
3.2. Multidomain Social Determinants of Depressive Symptoms: Results from Logistic Regression and Shapley Value Regression
3.3. Association of Social Determinants on Varying Degrees of Depressive Symptoms: Results from Quantile Regressions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Xu, Y.; Yang, J.; Gao, J.; Zhou, Z.; Tao, Z. Decomposing socioeconomic inequalities in depressive symptoms among the elderly in China. BMC Public Health 2016, 16, 1214. [Google Scholar] [CrossRef] [Green Version]
- Fu, F.; Liang, Y.; An, Y.; Zhao, F. Self-efficacy and psychological well-being of nursing home residents in China: The mediating role of social engagement. Asia Pac. J. Soc. Work. Dev. 2018, 28, 128–140. [Google Scholar] [CrossRef]
- Xie, H.; Cheng, C.; Tao, Y.; Zhang, J.; Robert, D.; Jia, J.; Su, Y. Quality of life in Chinese family caregivers for elderly people with chronic diseases. Health Qual. Life Outcomes 2016, 14, 99. [Google Scholar] [CrossRef] [Green Version]
- Sinclair, J.A.C. China’s Healthcare Reform. China Bus. Rev. 2009, 36, 32–36. [Google Scholar]
- Khuwaja, A.K.; Lalani, S.; Dhanani, R.; Azam, I.S.; Rafique, G.; White, F. Anxiety and depression among outpatients with type 2 diabetes: A multi-centre study of prevalence and associated factors. Diabetol. Metab. Syndr. 2010, 2, 72. [Google Scholar] [CrossRef] [Green Version]
- Zhou, X.; Li, J.; Gu, W.; Wang, J.; Zhu, Y.; Zhang, G.; Ding, Y.; Tang, Y. Prevalence and associated factors of anxiety and depression among patients with chronic respiratory diseases in eight general hospitals in Jiangsu Province of China: A cross-sectional study. Psychiatry Res. 2017, 251, 48–53. [Google Scholar] [CrossRef]
- Li, D.; Zhang, D.J.; Shao, J.J.; Qi, X.D.; Tian, L. A meta-analysis of the prevalence of depressive symptoms in Chinese older adults. Arch. Gerontol. Geriatr. 2014, 58, 1–9. [Google Scholar] [CrossRef]
- Ling, Z.; Xu, Y.; Nie, H.; Zhang, Y.; Yan, W. The prevalence of depressive symptoms among the older in China: A meta-analysis. Int. J. Geriatr. Psychiatry 2012, 27, 900–906. [Google Scholar]
- Ayerbe, L.; Ayis, S.; Wolfe, C.; Rudd, A.G. Natural history, predictors and outcomes of depression after stroke: Systematic review and meta-analysis. Br. J. Psychiatry J. Ment. Sci. 2013, 202, 14–21. [Google Scholar] [CrossRef]
- Strine, T.W.; Mokdad, A.H.; Balluz, L.S.; Berry, J.T.; Gonzalez, O. Impact of depression and anxiety on quality of life, health behaviors, and asthma control among adults in the United States with asthma, 2006. J. Asthma Res. 2008, 45, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.; Lopez, A.D. Evidence-Based Health Policy--Lessons from the Global Burden of Disease Study. Science 1996, 274, 740–743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salimah, O.; Rahmah, M.A.; Rosdinom, R.; Azhar, S.S. A case control study on factors that influence depression among the elderly in Kuala Lumpur Hospital and Universiti Kebangsaan Malaysia Hospital. Med. J. Malays. 2008, 63, 395. [Google Scholar]
- Lund, C.; Brooke-Sumner, C.; Baingana, F.; Baron, E.C.; Breuer, E.; Chandra, P.; Haushofer, J.; Herrman, H.; Jordans, M.; Kieling, C. Social determinants of mental disorders and the Sustainable Development Goals: A systematic review of reviews. Lancet Psychiatry 2018, 5, 357–369. [Google Scholar] [CrossRef]
- Gao, S.; Jin, Y.; Unverzagt, F.W.; Liang, C.; Hendrie, H.C. Correlates of depressive symptoms in rural elderly Chinese. Int. J. Geriatr. Psychiatry 2010, 24, 1358–1366. [Google Scholar] [CrossRef] [Green Version]
- Liu, Q.; Cai, H.; Yang, L.H.; Xiang, Y.B.; Yang, G.; Li, H.; Gao, Y.T.; Zheng, W.; Susser, E.; Shu, X.O. Depressive symptoms and their association with social determinants and chronic diseases in middle-aged and elderly Chinese people. Sci. Rep. 2018, 8, 3841. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Birnbaum, H.G.; Shahly, V.; Bromet, E.; Hwang, I.; McLaughlin, K.A.; Stein, D.J. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: Results from the WHO World Mental Health Survey Initiative. Depress. Anxiety 2010, 27, 351–364. [Google Scholar] [CrossRef] [Green Version]
- Pan, A.; Franco, O.H.; Wang, Y.-F.; Yu, Z.-J.; Ye, X.-W.; Lin, X. Prevalence and geographic disparity of depressive symptoms among middle-aged and elderly in China. J. Afferctive Disord. 2008, 105, 167–175. [Google Scholar] [CrossRef]
- Lorant, V.; Croux, C.; Weich, S.; Deliège, D.; Mackenbach, J.; Ansseau, M. Depression and socio-economic risk factors: 7-year longitudinal population study. Br. J. Psychiatry 2007, 190, 293–298. [Google Scholar] [CrossRef]
- Usman, S.; Chaudhary, H.R.; Asif, A.; Yahya, M.I. Severity and risk factors of depression in Alzheimer’s disease. J. Coll. Physicians Surg. Pak. 2010, 20, 327–330. [Google Scholar] [PubMed]
- Chou, K.L.; Chi, I. Prevalence and correlates of depression in Chinese oldest-old. Int. J. Geriatr. Psychiatry 2005, 20, 41–50. [Google Scholar] [CrossRef]
- Cao, W.; Li, L.; Zhou, X.; Zhou, C. Social capital and depression: Evidence from urban elderly in China. Aging Ment. Health 2015, 19, 418–429. [Google Scholar] [CrossRef]
- Lu, S.; Nicola, R.; Zhou, J.; Jian, S.; Pan, X.; Xiang, Q.; Zhang, Y.; Brian, O.; Wu, M. Depression among the general adult population in Jiangsu Province of China: Prevalence, associated factors and impacts. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 1051–1061. [Google Scholar] [CrossRef] [Green Version]
- Qiu, P.; Caine, E.D.; Hou, F.; Catherine, C.; Wittink, M.N.; Jin, L.; Ali, M. The Prevalence of Distress and Depression among Women in Rural Sichuan Province. PLoS ONE 2016, 11, e0161097. [Google Scholar] [CrossRef]
- Yu, C.; Hicks, A.; While, A.E. Depression and related factors in older people in China: A systematic review. Rev. Clin. Gerontol. 2012, 22, 52–67. [Google Scholar]
- Truong, K.D.; Ma, S. A systematic review of relations between neighborhoods and mental health. J. Ment. Health Policy Econ. 2006, 9, 137–154. [Google Scholar] [PubMed]
- Roberts, B.; Browne, J. A systematic review of factors influencing the psychological health of conflict-affected populations in low- and middle-income countries. Glob. Public Health 2011, 6, 814–829. [Google Scholar] [CrossRef]
- North, C.S.; Pfefferbaum, B. Mental health response to community disasters: A systematic review. J. Am. Med Assoc. 2013, 310, 507–518. [Google Scholar] [CrossRef] [PubMed]
- Goldmann, E.; Galea, S. Mental Health Consequences of Disasters. Annu. Rev. Public Health 2013, 35, 169. [Google Scholar] [CrossRef]
- Huang, C.-Q.; Wang, Z.-R.; Li, Y.-H.; Xie, Y.-Z.; Liu, Q.-X. Education and risk for late life depression: A meta-analysis of published literature. Int. J. Psychiatry Med. 2010, 40, 109–124. [Google Scholar]
- Santini, Z.I.; Koyanagi, A.; Tyrovolas, S.; Mason, C.; Haro, J.M. The association between social relationships and depression: A systematic review. J. Affect. Disord. 2015, 175, 53–65. [Google Scholar] [CrossRef]
- Nyqvist, F.; Forsman, A.K.; Giuntoli, G.; Cattan, M. Social capital as a resource for mental well-being in older people: A systematic review. Aging Ment. Health 2013, 17, 394–410. [Google Scholar] [CrossRef]
- Chen, X.; Smith, J.; Strauss, J.; Wang, Y.; Zhao, Y. China Health and Retirement Longitudinal Study (CHARLS); Springer: Singapore, 2017. [Google Scholar]
- Chang, F.; Li, Z.; Mao, Z. Association between Social Activities and Cognitive Function among the Elderly in China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2018, 15, 231. [Google Scholar]
- Huang, Q.; Wang, X.; Gong, C. Reliability and Validity of 10-item CES-D among Middle Aged and Older Adults in China. China J. Health Psychol. 2015, 23, 1036–1041. [Google Scholar]
- Yu, S.C.; Lin, Y.H.; Hsu, W.H. Applying structural equation modeling to report psychometric properties of Chinese version 10-item CES-D depression scale. Qual. Quant. 2011, 47, 1511–1518. [Google Scholar] [CrossRef]
- Noori, A.D.; Janet, L. Relation between depression and sociodemographic factors. Int. J. Ment. Health Syst. 2007, 1, 4. [Google Scholar]
- Eastwood, J.G.; Phung, H.; Barnett, B. Postnatal depression and socio-demographic risk: Factors associated with Edinburgh Depression Scale scores in a metropolitan area of New South Wales, Australia. Aust. N. Z. J. Psychiatry 2011, 45, 1040–1046. [Google Scholar] [CrossRef] [PubMed]
- Tannous, L.; Gigante, L.P.; Fuchs, S.C.; Busnello, E. Postnatal depression in Southern Brazil: Prevalence and its demographic and socioeconomic determinants. BMC Psychiatry 2008, 8, 1. [Google Scholar] [CrossRef] [Green Version]
- Lamu, A.N.; Olsen, J.A. The relative importance of health, income and social relations for subjective well-being: An integrative analysis. Soc. Sci. Med. 2016, 152, 176–185. [Google Scholar] [CrossRef] [Green Version]
- Sheikh, M.A.; Birgit, A.; Olsen, J.A. Clarifying Associations between Childhood Adversity, Social Support, Behavioral Factors, and Mental Health, Health, and Well-Being in Adulthood: A Population-Based Study. Front. Psychol. 2016, 7, 727. [Google Scholar] [CrossRef]
- Shorrocks, A.F. Decomposition procedures for distributional analysis: A unified framework based on the Shapley value. J. Econ. Inequal. 2013, 11, 99–126. [Google Scholar] [CrossRef] [Green Version]
- Borgoni, R.; Bianco, P.D.; Salvati, N.; Schmid, T.; Tzavidis, N. Modelling the distribution of health-related quality of life of advanced melanoma patients in a longitudinal multi-centre clinical trial using M-quantile random effects regression. Discuss. Pap. 2015, 27, 549–563. [Google Scholar] [CrossRef] [PubMed]
- Koenker, R. Quantile Regression. J. Econ. Perspect. 2015, 15, 143–156. [Google Scholar] [CrossRef]
- Kyung, K.E.; Ok, K.H.; Min, P.Y.; Jong, P.C.; Su, Y.D.; Young, L.J. Prevalence and Risk Factors of Depression in Geriatric Patients with Dermatological Diseases. Ann. Dermatol. 2013, 25, 278–284. [Google Scholar]
- Nolen-Hoeksema, S. Gender Differences in Depression. Curr. Dir. Psychol. Sci. 2001, 10, 173–176. [Google Scholar] [CrossRef] [Green Version]
- Zhou, X.; Bo, B.; Zheng, L.; Zhao, L.; Yang, H.; Song, H.; Sun, Y. The Prevalence and Risk Factors for Depression Symptoms in a Rural Chinese Sample Population. PLoS ONE 2014, 9, e99692. [Google Scholar] [CrossRef] [Green Version]
- Qin, X.; Wang, S.; Hsieh, C.R. The prevalence of depression and depressive symptoms among adults in China: Estimation based on a National Household Survey. China Econ. Rev. 2016, 20, S1043951X16300396. [Google Scholar] [CrossRef]
- Theofilou, P. Depression and Anxiety in Patients with Chronic Renal Failure: The Effect of Sociodemographic Characteristics. Int. J. Nephrol. 2011, 2011, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerogianni, G.; Lianos, E.; Kouzoupis, A.; Polikandrioti, M.; Grapsa, E. The role of socio-demographic factors in depression and anxiety of patients on hemodialysis: An observational cross-sectional study. Int. Urol. Nephrol. 2018, 50, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Kwong, E.; Kwok, T.T.Y.; Sumerlin, T.S.; Goggins, W.B.; Leung, J.; Kim, J.H. Does subjective social status predict depressive symptoms in Chinese elderly? A longitudinal study from Hong Kong. J. Epidemiol. Community Health 2020, 74, 882–891. [Google Scholar] [CrossRef]
- Krach, S.; Paulus, F.M.; Bodden, M.; Kircher, T. The rewarding nature of social interactions. Front. Behav. Neurosci. 2010, 4, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, J.; Aamodt, S.M.; Townsend, M.; Constantine-Paton, M. Developmental depression of glutamate neurotransmission by chronic low-level activation of NMDA receptors. J. Neurosci. 2001, 21, 6233–6244. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Chang, G.H. Disparity in Health Resource Allocation Between Rural and Urban Areas in China: Is It Getting Worse? Chin. Econ. 2008, 41, 45–55. [Google Scholar] [CrossRef]
- Hu, H.; Cao, Q.; Shi, Z.; Lin, W.; Jiang, H.; Hou, Y. Social Support and Depressive Symptom Disparity between Urban and Rural Older Adults in China. J. Affect. Disord. 2018, 237, S016503271830301X. [Google Scholar] [CrossRef] [PubMed]
- Egede, L.E. Diabetes, Major Depression, and Functional Disability Among U.S. Adults. Diabetes Care 2004, 27, 421–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Domain | Variables | n/Mean | %/S.D. |
|---|---|---|---|
| Demographic | Gender | ||
| Male | 1932 | 56.2 | |
| Female | 1506 | 43.8 | |
| Age (year) | 68.6 | 6.4 | |
| Marriage status | |||
| Married | 2435 | 70.8 | |
| Others | 1003 | 29.1 | |
| Economic | Annual income (CNY) | ||
| <20,000 | 3159 | 91.9 | |
| ≥20,000 | 279 | 8.1 | |
| Working status | |||
| Working | 403 | 11.7 | |
| Not working | 3035 | 88.3 | |
| Neighborhood | Residence | ||
| Urban | 637 | 18.5 | |
| Rural | 2801 | 81.5 | |
| Access to physical examination | |||
| Yes | 1179 | 34.3 | |
| No | 2259 | 65.7 | |
| Environmental events | Working age (year) | ||
| <18 | 3159 | 91.9 | |
| ≥18 | 279 | 8.1 | |
| Disability experience | |||
| No | 1932 | 56.2 | |
| Yes | 1506 | 43.8 | |
| Social and cultural | Education | ||
| Illiteracy | 961 | 28.0 | |
| Primary school | 1675 | 48.7 | |
| Middle school or above | 802 | 23.3 | |
| Living in family house | |||
| Yes | 3354 | 97.6 | |
| No | 84 | 2.4 | |
| Amount of social security | |||
| No | 1141 | 33.2 | |
| One | 2087 | 60.7 | |
| Two or above | 210 | 6.1 | |
| Outcome 1 | Occurrence of depressive symptoms | ||
| No | 2061 | 59.9 | |
| Yes | 1377 | 40.1 | |
| Outcome 2 | Degree of depressive symptoms | 16.1 | 4.9 |
| Domain | Variables | β | p | 95%CI | Shapley Value | Contribution to R2 (%) |
|---|---|---|---|---|---|---|
| Demographic | Gender (ref. = male) | 0.0224 | 33.52 | |||
| Female | 0.606 | <0.001 | (0.436, 0.777) | |||
| Age | −0.027 | <0.001 | (−0.041, −0.013) | |||
| Marriage status (ref. = married) | ||||||
| Others | 0.221 | 0.020 | (0.034, 0.408) | |||
| Economic | Annual income (ref. = ≥20,000) | 0.0178 | 26.53 | |||
| <20,000 | 0.437 | 0.041 | (0.023, 0.897) | |||
| Working status (ref. = working) | ||||||
| Not working | 0.249 | 0.046 | (0.004, 0.495) | |||
| Neighborhood | Residence (ref. = urban) | 0.0067 | 10.81 | |||
| Rural | 0.235 | 0.040 | (0.011, 0.460) | |||
| Access to physical examination (ref. = yes) | ||||||
| No | 0.014 | 0.954 | (−0.472, 0.501) | |||
| Environmental event | Working age (ref. = ≥18) | 0.0007 | 1.06 | |||
| <18 | 0.079 | 0.381 | (−0.098, 0.256) | |||
| Disability experience (ref. = no) | ||||||
| Yes | 0.457 | <0.001 | (0.303, 0.612) | |||
| Social and cultural | Education (ref. = illiteracy) | 0.0193 | 28.81 | |||
| Primary school | −0.054 | 0.609 | (−0.264, 0.155) | |||
| Middle school or above | −0.471 | 0.001 | (−0.738, −0.204) | |||
| Living in family house (ref. = yes) | ||||||
| No | 0.225 | 0.512 | (−0.448, 0.899) | |||
| Amount of social security (ref. = none) | ||||||
| One | −0.181 | 0.029 | (−0.343, −0.019) | |||
| Two or above | 0.037 | 0.833 | (−0.311, 0.386) | |||
| χ2 | 507.271 | <0.001 | ||||
| R2 | 0.281 | |||||
| Variables | Q10 | Q50 | Q90 | |||
|---|---|---|---|---|---|---|
| β | 95%CI | β | 95%CI | β | 95%CI | |
| Gender (ref. = male) | ||||||
| Female | 0.489 * | (0.010, 0.967) | 0.604 * | (0.143, 1.865) | −0.144 | (−1.508, 1.220) |
| Age | 0.005 | (−0.025, 0.036) | −0.018 | (−0.088, 0.501) | −0.092 * | (−0.177, −0.007) |
| Marriage status (ref. = married) | ||||||
| Others | 0.087 | (−0.335, 0.510) | 0.971 * | (0.030, 1.913) | 0.651 * | (0.081, 3.222) |
| Annual income (ref. = ≥20,000) | ||||||
| <20,000 | 0.203 | (−0.278, 0.684) | −0.561 | (−1.467, 0.346) | 0.201 | (−1.290, 1.691) |
| Working status (ref. = working) | ||||||
| Not working | −0.280 | (−0.744, 0.183) | −0.876 | (−2.226, 0.473) | −0.977 | (−3.151, 1.197) |
| Residence (ref. = urban) | ||||||
| Rural | −0.159 | (−0.874, 0.556) | −0.077 | (−1.156, 1.002) | 0.589 | (−0.825, 2.004) |
| Access to physical examination (ref. = yes) | ||||||
| No | −0.296 | (−1.657, 1.063) | −0.366 | (−3.016, 2.282) | −0.308 | (−6.711, 2.093) |
| Working age (ref. = ≥18) | ||||||
| <18 | 0.34 | (−0.848, 1.529) | 0.021 | (−5.074, 5.116) | −0.488 | (−6.242, 1.265) |
| Disability experience (ref. = no) | ||||||
| Yes | 0.258 | (−0.115, 0.632) | 0.100 * | (0.093, 1.806) | 0.259 * | (0.008, 2.511) |
| Education (ref. = illiteracy) | ||||||
| Primary school | 0.076 | (−0.415, 0.569) | −0.799 | (−1.927, 0.329) | −0.242 | (−1.823, 1.339) |
| Middle school or above | 0.697 | (−0.527, 1.922) | −0.179 * | (−5.512, −0.847) | −0.591* | (−8.848, −0.333) |
| Living in family house (ref. = yes) | ||||||
| No | −0.769 | (−2.182, 0.643) | −0.766 | (−4.526, 0.993) | −0.924 | (−5.796, 3.948) |
| Amount of social security (ref. = none) | ||||||
| One | −0.043 | (−0.425, 0.337) | 0.537 | (−0.257, 1.332) | 0.172 | (−1.180, 1.525) |
| Two or above | −0.642 | (−1.487, 0.202) | −0.102 | (−1.963, 1.757) | −0.274 | (−2.547, 1.998) |
| Pseudo R2 | 0.213 | 0.242 | 0.216 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, T.; Wang, X.; Xu, Y. Multidomain Social Determinants of Depressive Symptoms for the Elderly with Chronic Diseases: Evidence from the China Health and Retirement Longitudinal Study. Healthcare 2021, 9, 1765. https://doi.org/10.3390/healthcare9121765
Zhang T, Wang X, Xu Y. Multidomain Social Determinants of Depressive Symptoms for the Elderly with Chronic Diseases: Evidence from the China Health and Retirement Longitudinal Study. Healthcare. 2021; 9(12):1765. https://doi.org/10.3390/healthcare9121765
Chicago/Turabian StyleZhang, Tao, Xiaohe Wang, and Yongjian Xu. 2021. "Multidomain Social Determinants of Depressive Symptoms for the Elderly with Chronic Diseases: Evidence from the China Health and Retirement Longitudinal Study" Healthcare 9, no. 12: 1765. https://doi.org/10.3390/healthcare9121765
APA StyleZhang, T., Wang, X., & Xu, Y. (2021). Multidomain Social Determinants of Depressive Symptoms for the Elderly with Chronic Diseases: Evidence from the China Health and Retirement Longitudinal Study. Healthcare, 9(12), 1765. https://doi.org/10.3390/healthcare9121765






