The Evaluation of Further Complications after the Extraction of the Third Molar Germ: A Pilot Study in Paediatric Dentistry
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Methodology
2.2. Sample Size Calculation
Dimension of Sample and Inclusion Criteria
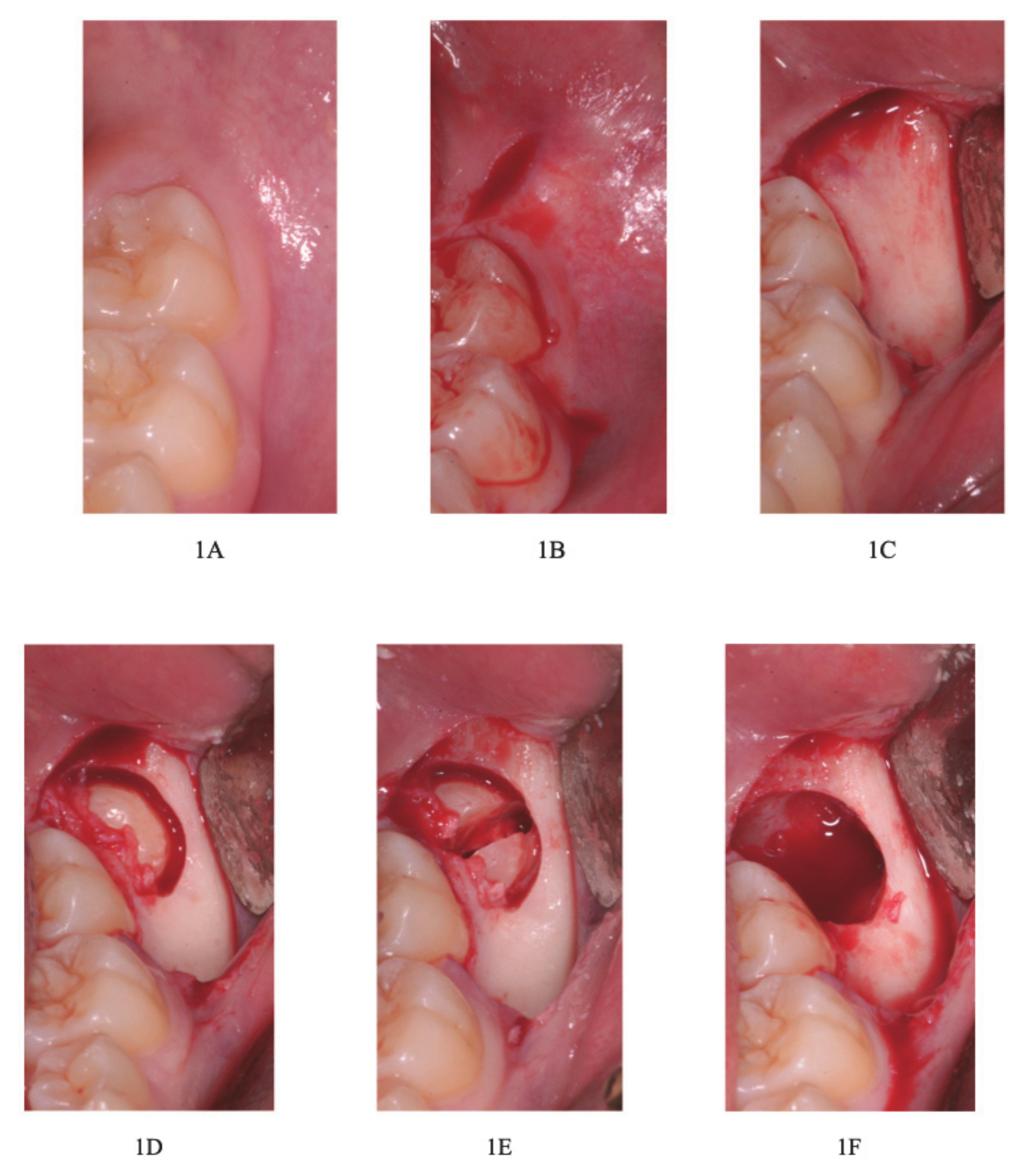
2.3. Surgical Protocol
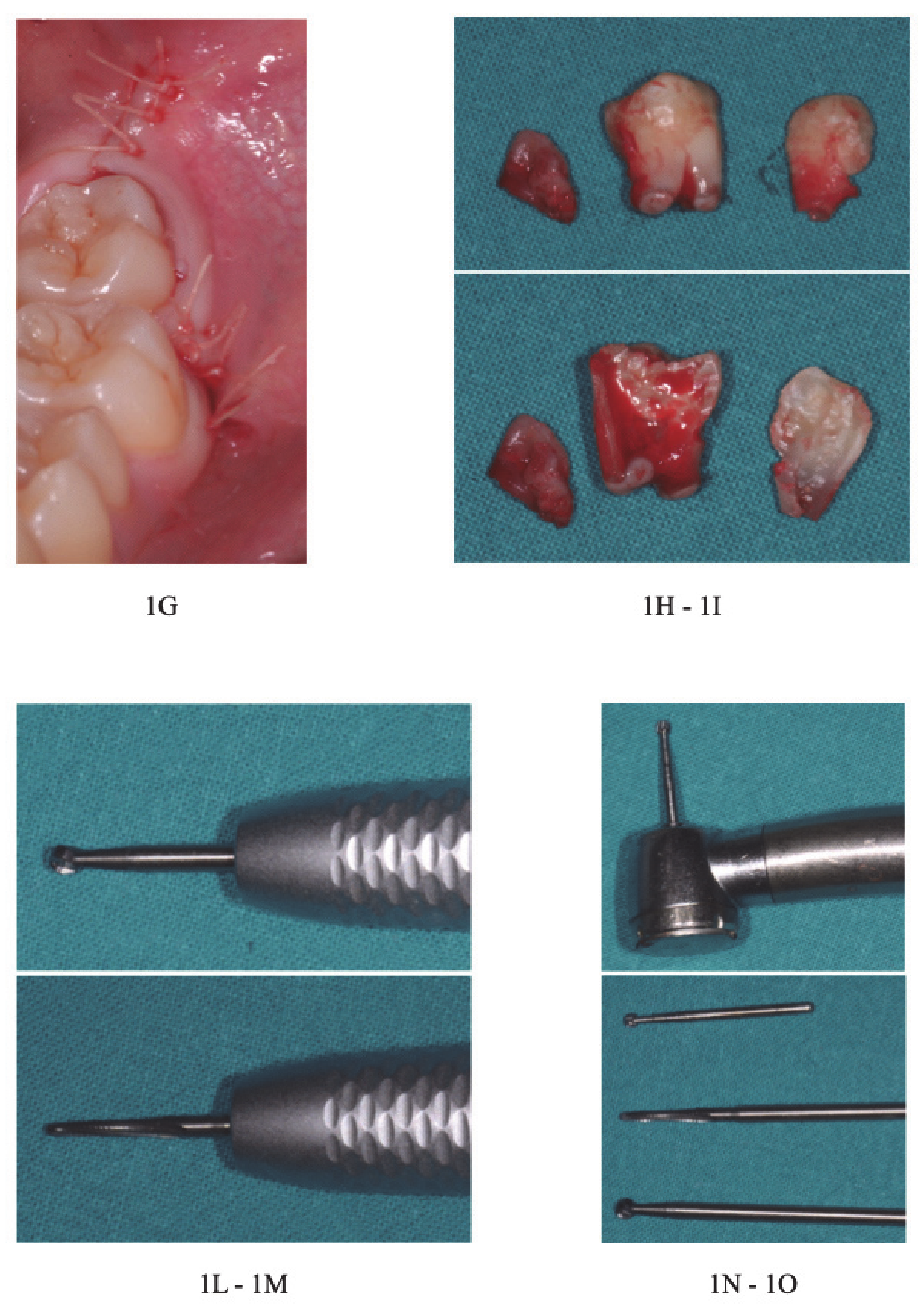
Description of the Combined Suture
2.4. Statistical Methodology
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Panzoni, E. Chirurgia Estrattiva; Masson: Milan, Italy, 1986. [Google Scholar]
- Lakhani, M.J.; Kadri, W.; Mehdi, H.; Sukhia, H.; Bano, A.; Yaqoob, S. Anterior arch crowding—A possible predictor for mandibular third molar impaction. J. Ayub Med. Coll. Abbottabad 2011, 23, 63–65. [Google Scholar] [PubMed]
- Carter, K.; Wortington, S. Predictors of third molar impaction: A systematic review and metaanalysis. J. Dent. Res. 2016, 95, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Gallini, G.; Raguso, C.; Contini, E. Pianificazione della germectomia dell’ottavo inferiore. Dent. Mod. 2004, 10, 71–85. [Google Scholar]
- Banu, A.M.; Şerban, D.M.; Pricop, M.O.; Urechescu, H.C.; Roi, C.I.; Şerban, C.L. Craniofacial morphology and its relation to the eruption pattern of permanent teeth in the supporting zone of the dentition in a group of Romanian children in Timişoara. J. Morphol. Embryol. 2018, 59, 491–497. [Google Scholar]
- Vercellotti, T. Piezoelectric Bone Surgery: A New Paradigm; Quintessence Publishing: Genova, Italy, 2020. [Google Scholar]
- Miclotte, A.; Franco, A.; Guerrero, M.E.; Willems, G.; Jacobs, R. The association between orthodontic treatment and third molar position, inferior alveolar nerve involvement, and prediction of wisdom tooth eruption. Surg. Radiol. Anat. 2015, 37, 333–339. [Google Scholar] [CrossRef]
- Maertens, J.K. Dissertations 25 years after date 47. Third molars in the lower jaw. Ned. Tijdschr. Tandheelkd. 2016, 123, 591–597. [Google Scholar] [CrossRef]
- Kaya, G.S.; Muzaffer, A.; Ömezli, M.M.; Dayi, E. Some morphological features related to mandibular third molar impaction. J. Clin. Exp. Dent. 2010, 2, e12–e17. [Google Scholar] [CrossRef]
- Passarelli, P.C.; Lopez, M.A.; De Santis, V.; Piccirillo, G.B.; Rella, E.; Giovannini, V.; Speranza, A.; De Leonardis, M.; Manicone, P.F.; Casale, M.; et al. Quality of life of patients with mandibular third molars and mild pericoronitis. A comparison between two different treatments: Extraction or periodontal approach. Antibiotics 2020, 9, 222. [Google Scholar] [CrossRef]
- Zawawi, K.H.; Melis, M. The role of mandibular third molars on lower anterior teeth crowding and relapse after orthodontic treatment: A systematic review. Sci. World J. 2014, 2014, 615429. [Google Scholar] [CrossRef]
- Satwik, A.; Naveed, N. Third molar impaction: Review. Res. J. Pharm. Techn. 2014, 7, 1498–1500. [Google Scholar]
- Akinbami, B.O.; Didia, B.C. Analysis of body mass index, the mandible and dental alveolar arch factors in prediction of mandibular third molar impaction: A pilot study. J. Contemp. Dent. Pract. 2010, 11, E041–E048. [Google Scholar] [CrossRef] [PubMed]
- Türköz, C.; Ulusoy, C. Effect of premolar extraction on mandibular third molar impaction in young adults. Angle Orthod. 2013, 83, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Sujon, M.K.; Alam, M.K.; Enezei, H.H.; Rahman, S.A. Third molar impaction and agenesis—A review. Int. J. Pharm. Bio Sci. 2015, 6, 1215–1221. [Google Scholar]
- Chaparro-Avendano, A.V.; Perez-Garcia, S.; Valmaseda-Castellon, E.; Berini Aytés, L.; Gay Escoda, C. Morbidity of third molar extraction in patients between 12 and 18 years of age. Med. Oral Patol. Oral Cir. Bucal. 2005, 10, 422. [Google Scholar] [PubMed]
- Bjørnland, T.; Haanaes, H.R.; Lind, P.O.; Zachrisson, B. Removal of third molar germs. Study of complications. Int. J. Oral Maxillofac. Surg. 1987, 16, 385–390. [Google Scholar] [CrossRef]
- Brunello, G.; De Biagi, M.; Crepaldi, G.; Rodrigues, F.I.; Sivolella, S. An observational cohort study on delayed-onset infections after mandibular third-molar extractions. Int. J. Dent. 2017, 1435348. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Crescentini, M.; Romanoni, G. Germectomy or delayed removal of mandibular impacted third molars. J. Oral Maxillofac. Surg. 1995, 53, 418–422. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; Consort Group. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010, 8, 18. [Google Scholar] [CrossRef]
- Barroso, M.; Arriola-Guillén, L.E.; Rodríguez-Cárdenas, Y.A.; Ruíz-Mora, G.A.; Guerrero, M.E.; Flores-Mir, C. Tridimensional assessment of the dental follicle dimensions of impacted mandibular third molars using cone-beam CT. J. Clin. Exp. Dent. 2018, 10, e726–e731. [Google Scholar] [CrossRef]
- Nolla, C.M. The development of permanent teeth. J. Dent. Child. 1960, 27, 254–266. [Google Scholar]
- Nandlal, B.; Karthikeya, P.; Ravi, S. Estimation of dental age by Nolla’s method using orthopantomographs among rural free residential school children. Int. J. Med. Res. Health Sci. 2014, 3, 273. [Google Scholar] [CrossRef]
- Canellas, J.V.D.S.; Ritto, F.G.; Medeiros, P.J.D. Evaluation of postoperative complications after mandibular third molar surgery with the use of platelet-rich fibrin: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 1138–1146. [Google Scholar] [CrossRef] [PubMed]
- Gümrükçü, Z. The effects of piezosurgery and submucosal dexamethasone injection on post-operative complications after third molar surgery. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 182–187. [Google Scholar] [CrossRef]
- Sandro, S. Suturing Techniques in Oral Surgery; Quintessenza Edizioni: Milan, Italy, 2008. [Google Scholar]
- Trombelli, L.; Farina, R.; Marzola, A.; Bozzi, L.; Liljenberg, B.; Lindhe, J. Modeling and remodeling of human extraction sockets. J. Clin. Periodontol. 2008, 35, 630–639. [Google Scholar] [CrossRef] [PubMed]
- Araújo, M.G.; Silva, C.O.; Misawa, M.; Sukekava, F. Alveolar socket healing: What can we learn? Periodontol. 2000 2015, 68, 122–134. [Google Scholar] [CrossRef]
- Zara, F.; De Sanctis, C.M.; DeDe, F.C.; Bossù, M.; Sfasciotti, G.L. A split-mouth study comparing piezo electric surgery and traditional rotary burs on impacted third molars in young patients: An intraoperative and postoperative evaluation. Minerva Stomatol. 2020, 69, 278–285. [Google Scholar] [CrossRef]
- Annibali, S.; Pippi, R.; Sfasciotti, G.L. Chirurgia Orale a Scopo Ortodontico; Elsevier—Masson: Roma, Italy, 2007. [Google Scholar]
- Annibali, S.; De Biase, A.; Pippi, R.; Sfasciotti, G.L. A consensus conference on management of the lower third molar. Italian Society of Odontostomatological Surgery. Minerva Stomatol. 2011, 60, 509–527. [Google Scholar]
- Zachrisson, B.U. Mandibular third molars and late lower arch crowding—The evidence base. World J. Orthod. 2005, 6, 180–186. [Google Scholar]
- Kavadia, S.; Antoniades, K.; Kaklamanos, E.; Antoniades, V.; Markovitsi, E.; Zafiriadis, L. Early extraction of the mandibular third molar in case of eruption disturbances of the second molar. J. Dent. Child. 2003, 70, 29–32. [Google Scholar]
- Clauser, C. Germectomie dei terzi molari inferiori: Una tecnica alteruativa, la via distale alta. Mondo Ortod. 1985, 3, 23. [Google Scholar]
- Smailienė, D.; Trakinienė, G.; Beinorienė, A.; Tutlienė, U. Relationship between the position of impacted third molars and external root resorption of adjacent second molars: A retrospective CBCT study. Medicina (Kaunas) 2019, 55, 305. [Google Scholar] [CrossRef] [PubMed]
- Monaco, G.; Cecchini, S.; Gatto, M.R.; Pelliccioni, G.A. Delayed onset infections after lower third molar germectomy could be related to the space distal to the second molar. Int. J. Oral Maxillofac. Surg. 2016, 46, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, R.; Valmaseda-Castellon, E.; Berini-Aytes, L.; Gay-Escoda, C. Delayed-onset infections after lower third molar extraction: A case-control study. J. Oral Maxillofac. Surg. 2007, 65, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, R.; Valmaseda-Castellon, E.; Berini- Aytes, L.; Gay-Escoda, C. Incidence and clinical features of delayed-onset infections after extraction of lower third molars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 99, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Sainz de Baranda, B.; Silvestre, F.J.; Silvestre-Rangil, J. Relationship between surgical difficulty of third molar extraction under local anesthesia and the postoperative evolution of clinical and blood parameters. J. Oral Maxillofac. Surg. 2019, 77, 1337–1345. [Google Scholar] [CrossRef] [PubMed]
- Candotto, V.; Oberti, L.; Gabrione, F.; Scarano, A.; Rossi, D.; Romano, M. Complication in third molar extractions. J. Biol. Regul. Homeost. Agents 2019, 33, 169–172. [Google Scholar] [PubMed]
- Bello, S.A.; Adeyemo, W.L.; Bamgbose, B.O.; Obi, E.V.; Adeyinka, A.A. Effect of age, impaction types and operative time on inflammatory tissue reactions following lower third molar surgery. Head Face Med. 2011, 7, 8. [Google Scholar] [CrossRef] [PubMed]
- Sayed, N.; Bakathir, A.; Pasha, M.; Al-Sudairy, S. Complications of third molar extraction: A retrospective study from a tertiary healthcare centre in Oman. Sultan Qaboos Univ. Med. J. 2019, 19, e230–e235. [Google Scholar] [CrossRef]
- Halpern, L.R.; Dodson, T.B. Does prophylactic administration of systemic antibiotics prevent postoperative inflammatory complications after third molar surgery. J. Oral Maxillofac. Surg. 2007, 65, 177–185. [Google Scholar] [CrossRef]
- Punwutikorn, J.; Waikakul, A.; Ochareon, P. Symptoms of unerupted mandibular third molars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 87, 305. [Google Scholar] [CrossRef]
- Kaminishi, R.M.; Kaminishi, K.S. New considerations in the treatment of compromised third molars. J. Calif Dent. Assoc. 2004, 32, 823–825. [Google Scholar] [PubMed]
- De Jong, K.J.; Oosting, J.; Abraham-Inpijn, L. Medical risk classification of dental patients in the Netherlands. J. Public Health Dent. 1993, 53, 219–222. [Google Scholar] [CrossRef] [PubMed]
- La Monaca, G.; Vozza, I.; Giardino, R.; Annibali, S.; Pranno, N.; Cristalli, M.P. Prevention of neurological injuries during mandibular third molar surgery: Technical notes. Ann. Stomatol. (Roma) 2017, 8, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Sun, R.; Cai, Y.; Yuan, Y.; Zhao, J.H. The characteristics of adjacent anatomy of mandibular third molar germs: A CBCT study to assess the risk of extraction. Sci. Rep. 2017, 7, 14154. [Google Scholar] [CrossRef]
- D’Angeli, G.; Messineo, D.; Riminucci, M.; Corsi, A.; Celli, M.; Vozza, I.; Sfasciotti, G.L. The characteristics of adjacent anatomy of mandibular third molar germs: A CBCT pilot study in patients with osteogenesis imperfecta. Healthcare (Basel) 2020, 8, 372. [Google Scholar] [CrossRef]
- Yadav, S.; Verma, A.; Sachdeva, A. Assessment of lingual nerve injury using different surgical variables for mandibular third molar surgery: A clinical study. Int. J. Oral Maxillofac. Surg. 2014, 43, 889–893. [Google Scholar] [CrossRef]
- Park, W.; Choi, J.W.; Kim, J.Y.; Kim, B.C.; Kim, H.J.; Lee, S.H. Cortical integrity of the inferior alveolar canal as a predictor of paresthesia after third-molar extraction. J. Am. Dent. Assoc. 2010, 141, 271–278. [Google Scholar] [CrossRef]
- Tolstunov, L.; Brickeen, M.; Kamanin, V.; Susarla, S.M.; Selvi, F. Is the angulation of mandibular third molars associated with the thickness of lingual bone? Br. J. Oral Maxillofac. Surg. 2016, 54, 914–919. [Google Scholar] [CrossRef]
- Zhang, Q.B.; Zhang, Z.Q. Early extraction: A silver bullet to avoid nerve injury in lower third molar removal. Int. J. Oral Maxillofac. Surg. 2012, 41, 1280–1283. [Google Scholar] [CrossRef]
- Chuang, S.K.; Perrott, D.H.; Susarla, S.M.; Dodson, T.B. Age as a risk factor for third molar surgery complications. J. Oral Maxillofac. Surg. 2007, 65, 1685–1692. [Google Scholar] [CrossRef]
- Bui, C.H.; Seldin, E.B.; Dodson, T.B. Types, frequencies, and risk factors for complications after third molar extraction. J. Oral Maxillofac. Surg. 2003, 61, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- Queral-Godoy, E.; Figueiredo, R.; Valmaseda-Castellon, E.; Berini-Aytés, L.; Gay-Escoda, C. Frequency and evolution of lingual nerve lesions following third molar extraction. J. Oral Maxillofac. Surg. 2006, 64, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Barone, R.; Clauser, C.; Testori, T.; Del Fabbro, M. Self-assessed neurological disturbances after surgical removal of impacted lower third molar: A pragmatic prospective study on 423 surgical extractions in 247 consecutive patients. Clin. Oral Investig. 2019, 23, 3257–3265. [Google Scholar] [CrossRef] [PubMed]
- Yadav, S.; Mittal, H.C.; Malik, S.; Dhupar, V.; Sachdeva, A.; Malhotra, V.; Singh, G. Post-traumatic and postoperative neurosensory deficits of the inferior alveolar nerve in mandibular fracture: A prospective study. J. Korean Assoc. Oral Maxillofac. Surg. 2016, 42, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Al-Khateeb, T.H.; Bataineh, A.B. Pathology associated with impacted mandibular third molars in a group of Jordanians. J. Oral Maxillofac. Surg. 2006, 64, 1598–1602. [Google Scholar] [CrossRef] [PubMed]
- Su, N.; van Wijk, A.; Berkhout, E.; Sanderink, G.; De Lange, J.; Wang, H.; van der Heijden, G.J.M.G. Predictive value of pan-oramic radiography for injury of inferior alveolar nerve after mandibular third molar surgery. J. Oral Maxillofac. Surg. 2017, 75, 663–679. [Google Scholar] [CrossRef]
- Chossegros, C.; Guyot, L.; Cheynet, F.; Belloni, D.; Blanc, J.L. Is lingual nerve protection necessary for lower third molar germectomy? A prospective study of 300 procedures. Int. J. Oral Maxillofac. Surg. 2002, 31, 620–624. [Google Scholar] [CrossRef] [PubMed]
- Kaminishi, R.M.; Lam, P.S.; Kaminishi, K.S.; Marshall, M.W.; Hochwald, D.A. A 10-year comparative study of the incidence of third molar removal in the aging population. J. Oral Maxillofac. Surg. 2006, 64, 173–174. [Google Scholar] [CrossRef]
- Ghaeminia, H.; Perry, J.; Nienhuijs, M.E.; Toedtling, V.; Tummers, M.; Hoppenreijs, T.J.; Van der Sanden, W.J.; Mettes, T.G. Surgical removal versus retention for the management of asymptomatic impacted wisdom teeth. Cochrane Database Syst Rev. 2016, 8, CD003879. [Google Scholar] [CrossRef]
| COMPLICATIONS | MALES N = 27 teeth (%) | FEMALES N = 19 teeth (%) |
|---|---|---|
| Swelling | 0% | 0% |
| Delayed oneset infections | 1 (3.7%) | 0% |
| Alveolar Osteitis | 0% | 0% |
| Paresthesia of IAN | 0% | 0% |
| Lingual Paresthesia | 0% | 0% |
| Bleeding and Hemorrhage | 1 (3.7%) | 0% |
| Pain | 0% | 0% |
| 2 molar restoration damage | 0% | 0% |
| Severe trisma | 0% | 0% |
| COMPLICATIONS | B N = 44 teeth (%) | C N = 2 teeth (%) |
|---|---|---|
| Swelling | 0% | 0% |
| Delayed oneset infections | 1 (2.3%) | 0% |
| Alveolar Osteitis | 0% | 0% |
| Paresthesia of IAN | 0% | 0% |
| Lingual Paresthesia | 0% | 0% |
| Bleeding and Hemorrhage | 1 (2.3%) | 0% |
| Pain | 0% | 0% |
| 2 molar restoration damage | 0% | 0% |
| Severe trisma | 0% | 0% |
| COMPLICATIONS | Immediately after the Germectomy | 1 week | 1 month | 1 year | 2 year |
|---|---|---|---|---|---|
| Swelling | X | X | X | X | X |
| Delayed oneset infections | X | X | V | X | X |
| Alveolar Osteitis | X | X | X | X | X |
| Paresthesia of IAN | X | X | X | X | X |
| Lingual Paresthesia | X | X | X | X | X |
| Bleeding and Hemorrhage | V | X | X | X | X |
| Pain | X | X | X | X | X |
| 2 molar restoration damage | X | X | X | X | X |
| Severe trisma | X | X | X | X | X |
| COMPLICATIONS | 5 | 6 | 7 | 8 |
|---|---|---|---|---|
| Swelling | 0% | 0% | 0% | 0% |
| Delayed oneset infections | 0% | 0% | 1 (7.7%) | 0% |
| Alveolar Osteitis | 0% | 0% | 0% | 0% |
| Paresthesia of IAN | 0% | 0% | 0% | 0% |
| Lingual Paresthesia | 0% | 0% | 0% | 0% |
| Bleeding and Hemorrhage | 0% | 1 (7.7%) | 0% | 0% |
| Pain | 0% | 0% | 0% | 0% |
| 2 molar restoration damage | 0% | 0% | 0% | 0% |
| Severe trisma | 0% | 0% | 0% | 0% |
| Delayed Onset | χ2 | Df | P |
|---|---|---|---|
| Gender | 0.719 | 1 | 0.369 |
| Nolla’s classification | 2.595 | 3 | 0.658 |
| Winter’s classification | 0.046 | 2 | 0.829 |
| Bleeding | χ2 | Df | P |
|---|---|---|---|
| Gender | 0.719 | 1 | 0.369 |
| Noll’s classification | 2.595 | 3 | 0.658 |
| Winter’s classification | 0.046 | 2 | 0.829 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Angeli, G.; Zara, F.; Vozza, I.; D’Angeli, F.M.; Sfasciotti, G.L. The Evaluation of Further Complications after the Extraction of the Third Molar Germ: A Pilot Study in Paediatric Dentistry. Healthcare 2021, 9, 121. https://doi.org/10.3390/healthcare9020121
D’Angeli G, Zara F, Vozza I, D’Angeli FM, Sfasciotti GL. The Evaluation of Further Complications after the Extraction of the Third Molar Germ: A Pilot Study in Paediatric Dentistry. Healthcare. 2021; 9(2):121. https://doi.org/10.3390/healthcare9020121
Chicago/Turabian StyleD’Angeli, Giacomo, Francesca Zara, Iole Vozza, Francesco Maria D’Angeli, and Gian Luca Sfasciotti. 2021. "The Evaluation of Further Complications after the Extraction of the Third Molar Germ: A Pilot Study in Paediatric Dentistry" Healthcare 9, no. 2: 121. https://doi.org/10.3390/healthcare9020121
APA StyleD’Angeli, G., Zara, F., Vozza, I., D’Angeli, F. M., & Sfasciotti, G. L. (2021). The Evaluation of Further Complications after the Extraction of the Third Molar Germ: A Pilot Study in Paediatric Dentistry. Healthcare, 9(2), 121. https://doi.org/10.3390/healthcare9020121







