Periodontal Treatment Needs of Hemodialized Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Exclusion Criteria
2.3. Methods
- Periodontal Probing Depth (PPD) The measurement was recorded with the periodontal probe, which was introduced to sulcus or pocket with a little pressure (10–20 g). A probe was introduced parallel to root surface into the sulcus. The first incision seen above the sulcus was its size.
- Clinical Attachment Lost (CAL). This is defined as a distance between cementum enamel junction (CEJ) and gingival margin (GM). It was measured with the usage of periodontal probe. Received value was then added to the value of PPD: CAL = PPD + (CEJ + GM).
- Bleeding Index or Bleeding on Probing Index (BI or BOP). The assessment was undertaken with a dental probe. All four surfaces of each tooth were assessed. Providing that a patient had all teeth, maximally 128 surfaces (32 teeth × 4 surfaces) were assessed. In patients diagnosed with end- stage chronic disease the index was checked before heparin was given. In the case of small bleeding the dental floss was used. It was placed near the tooth surface in labial- lingual direction to the bottom of the sulcus. Then it was moved twice in apex to crown direction. In the next stage, floss was removed and the assessed region observed for 15 s (bleeding or no bleeding). If no bleeding was observed the noted value was 0, if there was bleeding 1. For each patient, the index was calculated by summing the values received for all teeth. Maximal index value was 128 and minimal 0. The lower the value, the better the sulcus condition.
- Community Periodontal Index for Treatment Needs (CPITN) by Ainamo, Barmes, Beadre et al. This index makes it possible to assess quickly and precisely the condition of periodontium, treatment needs and time for their realization. Teeth were divided into 6 sextants (17–14; 13–23, 24–27; 47–44; 43–33; 34–37). The examination was undertaken with a dental mirror, periodontal probe and dental probe. In each sextant all teeth were examined but only the highest value was noted.
- 0-
- healthy periodontium;
- 1-
- bleeding on probing, no periodontal pockets, no calculus nor overhanging restorations;
- 2-
- periodontal pockets to 3 mm, calculus or dental plaque above and below the gum level, overhanging restorations;
- 3-
- periodontal pockets 3.5–5.5 mm, bleeding on probing;
- 4-
- periodontal pockets ≥ 6 mm.
2.4. Statistical Analysis
3. Results
CPITN Index
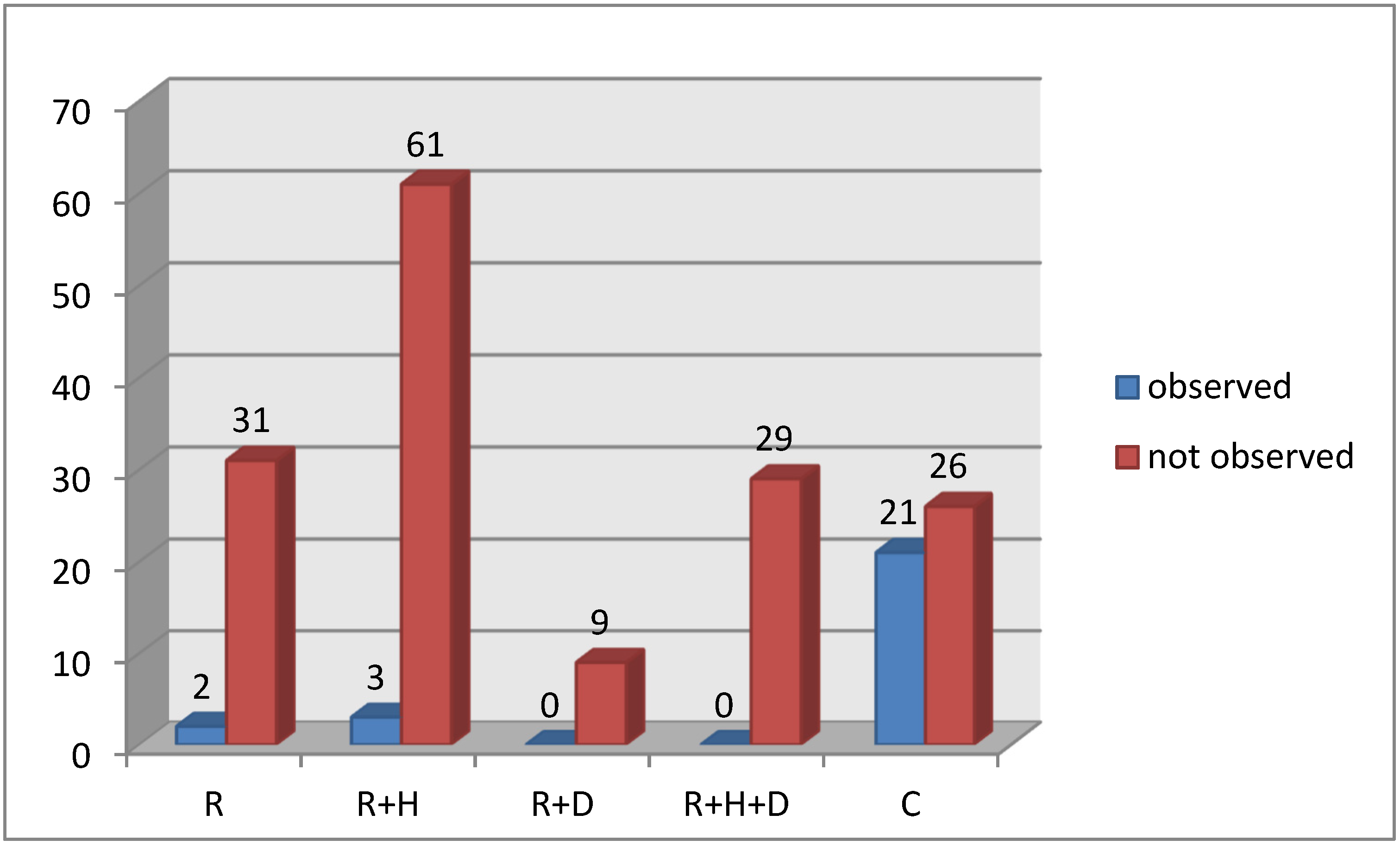
- In examined group there was significantly lower percentage of patients with healthy periodontium and higher percentage of patients with periodontal pockets >3.5 mm and the periodontal attachment lost was 5 mm and more in comparison to the control group. While comparing particular subgroups in examined one it was observed that the highest percentage of patients with healthy periodontium was in R and R + H groups and the lowest with the highest number of people with advanced changes in the periodontium were in the R + D subgroup.
- The average values of bleeding index were significantly lower in patients belonging to control group than in the hemodialized group.
- In the control group a higher percentage of patients without or with moderate changes in periodontium (CPI 0, 1 and 2) was observed, while in the examined groups most of the patients had CPI 2 and higher, which classified them for specialist treatment.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zdrojewski, Z.; Ziętkiewicz, M. Choroby nerek u ludzi w podeszłym wieku. Gerontol Pol. 2005, 13, 222–229. [Google Scholar]
- Małyszko, J. Przewlekła niewydolność nerek–problem tylko nefrologów? Choroby Serca i Naczyń 2005, 2, 78–83. [Google Scholar]
- Eknoyan, G. The wonderful apparatus of John Jacob Abel called the artificial kidney. Semin. Dial. 2009, 22, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Auglienė, R.; Dalinkevičienė, E.; Kuzminskis, V.; Jievaltas, M.; Peleckaitė, L.; Gryguc, A.; Stankevičius, E.; Bumblytė, I.A. Factors influencing renal graft survival: 7-Year experience of a single center. Medicina 2017, 53, 224–232. [Google Scholar] [CrossRef]
- Bayraktar, G.; Kazancioglu, R.; Bozfakioglu, S.; Yildiz, A.; Ark, E. Evaluation of salivary parameters and dental status in adult hemodialysis patients. Clin. Nephrol. 2004, 62, 380–383. [Google Scholar] [CrossRef] [PubMed]
- De la Rosa, G.E.; Mondragon, P.A.; Aranda, R.S.; Bustamante, R.M.A. Oral mucosa symptoms, signs and leasions in-end stage renal disease, and non-end stage renal disease diabetic patients. Med. Oral Patol. Oral Cir. Bucal. 2006, 11, 467–473. [Google Scholar]
- Trzcionka, A.; Twardawa, H.; Mocny-Pachońska, K.; Tanasiewicz, M. Oral cavity status of long-term hemodialized patients vs. their socio-economic status. Med. Pr. 2020, 71, 279–288. [Google Scholar] [CrossRef]
- Sokołowska-Trelka, A.; Grzebieluch, W.; Dubiński, B. Problemy stomatologiczne u chorych na schyłkową niewydolność nerek. Dent. Med. Probl. 2005, 42, 351–356. [Google Scholar]
- Klassen, J.T.; Krasko, B.M. The dental health status of dialysis patients. J. Can. Dent. Assoc. 2002, 68, 34–38. [Google Scholar]
- De Rossi, S.S.; Glick, M. Dental consideration for the patient with renal disease receiving hemodialysis. J. Am. Dent. Assoc. 1996, 127, 211–219. [Google Scholar] [CrossRef]
- Conntaldo, M.; Boccellino, M.; Zannini, G.; Romano, A.; Sciarra, A.; Sacco, A.; Settembre, G.; Coppola, M.; Di Carlo, A.; D’Angelo, L.; et al. Sex hormones and inflammation role in oral cancer progression. A molecular and biological point of view. J. Oncol. 2020, 2020, 9587971. [Google Scholar] [CrossRef] [PubMed]
- Ninomiya, M.; Hashimoto, M.; Yamanouchi, K.; Fukumura, Y.; Nagata, T.; Naruishi, K. Relationship of oral conditions to the incidence of infective endocarditis in periodontitis patients with valvular heart disease: A cross-sectional study. Clin. Oral Investig. 2020, 24, 833–840. [Google Scholar] [CrossRef] [PubMed]
- Ioannidou, E.; Shaqman, M.; Burleson, J.; Dongari-Bagtzoglou, A. Periodontitis case definition affects the association with renal function in kidney transplant recipients. Oral Dis. 2010, 16, 636–642. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Riche, E.L.; Boggess, K.A.; Lieff, S.; Murtha, A.P.; Auten, R.L.; Beck, J.D.; Offenbacher, S. Periodontal disease increases the risk of preterm delivery among preeclamptic women. Ann. Periodontol. 2002, 7, 95–101. [Google Scholar] [CrossRef]
- Siribamrungwong, M.; Puangpanngam, K. Treatment of Periodontal Diseases Reduces Chronic Systemic Inflammation in Maintenance Hemodialysis Patients. Ren. Fail. 2012, 34, 171–175. [Google Scholar] [CrossRef]
- Kshirsagar, A.V.; Craig, R.G.; Beck, J.D. Severe periodontitis is associated with low serum albumin among patients on maintenance hemodialysis therapy. Clin. J. Am. Soc. Nephrol. 2007, 2, 239–244. [Google Scholar] [CrossRef]
- Fletcher, P.D.; Scopp, I.W.; Hersh, R.A. Oral manifestations of secondary hyperparathyroidism related to longterm hemodialysis therapy. Oral Surg. Oral Med. Oral Pathol. 1977, 43, 218–226. [Google Scholar] [CrossRef]
- Hutton, C.E. Intradental lesions and their reversal in a patient being treated for end-stage renal disease. Oral Surg. Oral Med. Oral Pathol. 1985, 60, 258–261. [Google Scholar] [CrossRef]
- Wilczyńska-Borawska, M.; Zbroch, E.; Małyszko, J.; Myśliwiec, M.; Stokowska, W. Stan uzębienia i przyzębia chorych na cukrzycę pacjentów hemodializowanych z terenu północno- wschodniej Polski. Post. Nauk Med. 2013, 3, 195–200. [Google Scholar]
- Teratani, G.; Awano, S.; Soh, I.; Yoshida, A.; Kinoshita, N.; Hamasaki, T.; Takata, Y.; Sonoki, K.; Nakamura, H.; Ansai, T. Oral health in patients on haemodialysis for diabetic nephropathy in chronic glomerulonephris. Clin. Oral Investig. 2013, 17, 483–489. [Google Scholar] [CrossRef]
- Jenabian, N.; Mirsaeed, A.M.G.; Ehsani, H.; Kiakojori, A. Periodontal status of patient’s underwent hemodialysis therapy. Caspian J. Intern. Med. 2013, 4, 658–661. [Google Scholar] [PubMed]
- Chhokra, M.; Manocha, S.; Dodwad, V.; Gupta, U.; Vaish, S. Establishing an Association between Renal Failure and Periodontal Health: A Cross Sectional Study. J. Clin. Diagn Res. 2013, 7, 2348–2350. [Google Scholar] [PubMed]
- Swapna, L.A.; Reddy, R.S.; Ramesh, T.; Reddy, R.L.; Vijayalaxmi, N.; Karmakar, P.; Pradeep, K. Oral health status in haemodialysis patients. J. Clin. Diagn Res. 2013, 7, 2047–2050. [Google Scholar] [CrossRef]
- Vesterinen, M.; Ruokonen, H.; Furuholm, J.; Honkanen, E.; Meurman, J.H. Oral health in predialysis patients with emphasis on diabetic nephropathy. Clin. Oral Investig. 2011, 15, 99–104. [Google Scholar] [CrossRef]
- Parkar, S.M.; Ajithkrishnan, C.G. Periodontal status in patients undergoing hemodialysis. Indian J. Nephrol. 2012, 22, 246–250. [Google Scholar] [CrossRef]




| Clinical Assessment | Category of Treatment Needs According to CPITN |
|---|---|
| 0 1 | I. Oral hygiene instructions. |
| 2 3 | II. Oral hygiene instructions. Periodontal treatment consisted of removal of supra–and subgingival microbial deposits via scaling using hand and ultrasonic instruments. Correction of overhanging restorations. |
| 4 | III. Oral hygiene instructions. Periodontal treatment consisted of removal of supra–and subgingival microbial deposits via scaling and root planning (SRP) under local anesthesia using hand and ultrasonic instruments. Correction of overhanging restorations. Complex periodontal treatment. |
| Group | Sex | Avarage Age | |
|---|---|---|---|
| Men [n] | Women [n] | ||
| C | 15 | 33 | 52.71 |
| R | 25 | 17 | 67.21 |
| R + H | 48 | 31 | 62.54 |
| R + D | 10 | 6 | 70.19 |
| R + H + D | 27 | 16 | 72.86 |
| When Did You Last Visit a Dentist? | C | R | R + H | R + D | R + H + D | |
|---|---|---|---|---|---|---|
| less than 3 months ago | number [n] | 34 | 8 | 17 | 3 | 4 |
| % of group | 71% | 19% | 22% | 19% | 9% | |
| 3–6 months ago | number [n] | 5 | 6 | 13 | 2 | 9 |
| % of group | 10% | 14% | 17% | 13% | 21% | |
| a year ago | number [n] | 7 | 13 | 17 | 7 | 11 |
| % of group | 15% | 31% | 22% | 44% | 26% | |
| I do not remember | number [n] | 2 | 15 | 30 | 4 | 19 |
| % of group | 4% | 36% | 39% | 25% | 36% | |
| Group | Description |
|---|---|
| P1 | patients with PPD ≤ 0.5 mm and CAL ≤ 2 mm, no periodontium treatment needed |
| P2 | patients with PPD ≤ 3.5 mm and CAL 3–4 mm, periodontist consultation needed and constant control of a dentist |
| P3 | patients with PPD > 3.5 mm and CAL ≥ 5 mm, specialist periodontium treatment needed |
| Variable | Result of Chi-Quadrat Test | |||
|---|---|---|---|---|
| X2 | df | p | η | |
| P1 | 48.43 | 4 | 0.000 | 0.52 |
| P2 | 3.15 | 4 | 0.533 | 0.13 |
| P3 | 53.64 | 4 | 0.000 | 0.54 |
| Group | Periodontal Symptoms CPI | ||||
|---|---|---|---|---|---|
| Frequency (Percentage Distribution) | |||||
| 0 | 1 | 2 | 3 | 4 | |
| R | 2 (6%) | 7 (21%) | 13 (39%) | 3 (9%) | 8 (24%) |
| R + H | 4 (6%) | 19 (30%) | 19 (30%) | 8 (13%) | 14 (22%) |
| R + D | 0 (0%) | 1 (11%) | 6 (67%) | 0 (0%) | 2 (22%) |
| R + H + D | 0 (0%) | 3 (10%) | 12 (41%) | 6 (21%) | 8 (28%) |
| C | 13 (28%) | 14 (30%) | 10 (21%) | 6 (13%) | 4 (9%) |
| Group | Treatment Needs TN | ||
|---|---|---|---|
| Frequency (Percentage Distribution) | |||
| I | II | III | |
| R | 9 (28%) | 16 (48%) | 8 (24%) |
| R + H | 23 (35%) | 27 (42%) | 14 (22%) |
| R + D | 1 (11%) | 6 (67%) | 2 (22%) |
| R + H + D | 3 (10%) | 18 (62%) | 8 (28%) |
| C | 27 (57%) | 16 (34%) | 4 (9%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trzcionka, A.; Twardawa, H.; Mocny-Pachońska, K.; Tanasiewicz, M. Periodontal Treatment Needs of Hemodialized Patients. Healthcare 2021, 9, 139. https://doi.org/10.3390/healthcare9020139
Trzcionka A, Twardawa H, Mocny-Pachońska K, Tanasiewicz M. Periodontal Treatment Needs of Hemodialized Patients. Healthcare. 2021; 9(2):139. https://doi.org/10.3390/healthcare9020139
Chicago/Turabian StyleTrzcionka, Agata, Henryk Twardawa, Katarzyna Mocny-Pachońska, and Marta Tanasiewicz. 2021. "Periodontal Treatment Needs of Hemodialized Patients" Healthcare 9, no. 2: 139. https://doi.org/10.3390/healthcare9020139
APA StyleTrzcionka, A., Twardawa, H., Mocny-Pachońska, K., & Tanasiewicz, M. (2021). Periodontal Treatment Needs of Hemodialized Patients. Healthcare, 9(2), 139. https://doi.org/10.3390/healthcare9020139






