Cost–Utility Analysis of Home Mechanical Ventilation in Patients with Amyotrophic Lateral Sclerosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Cost Identification
2.2. Utility Identification
2.3. Selection of Initial Distribution of Patients
2.4. Cost–Utility Analysis
2.5. Sensitivity Analysis
2.6. Scenario Analysis
3. Results
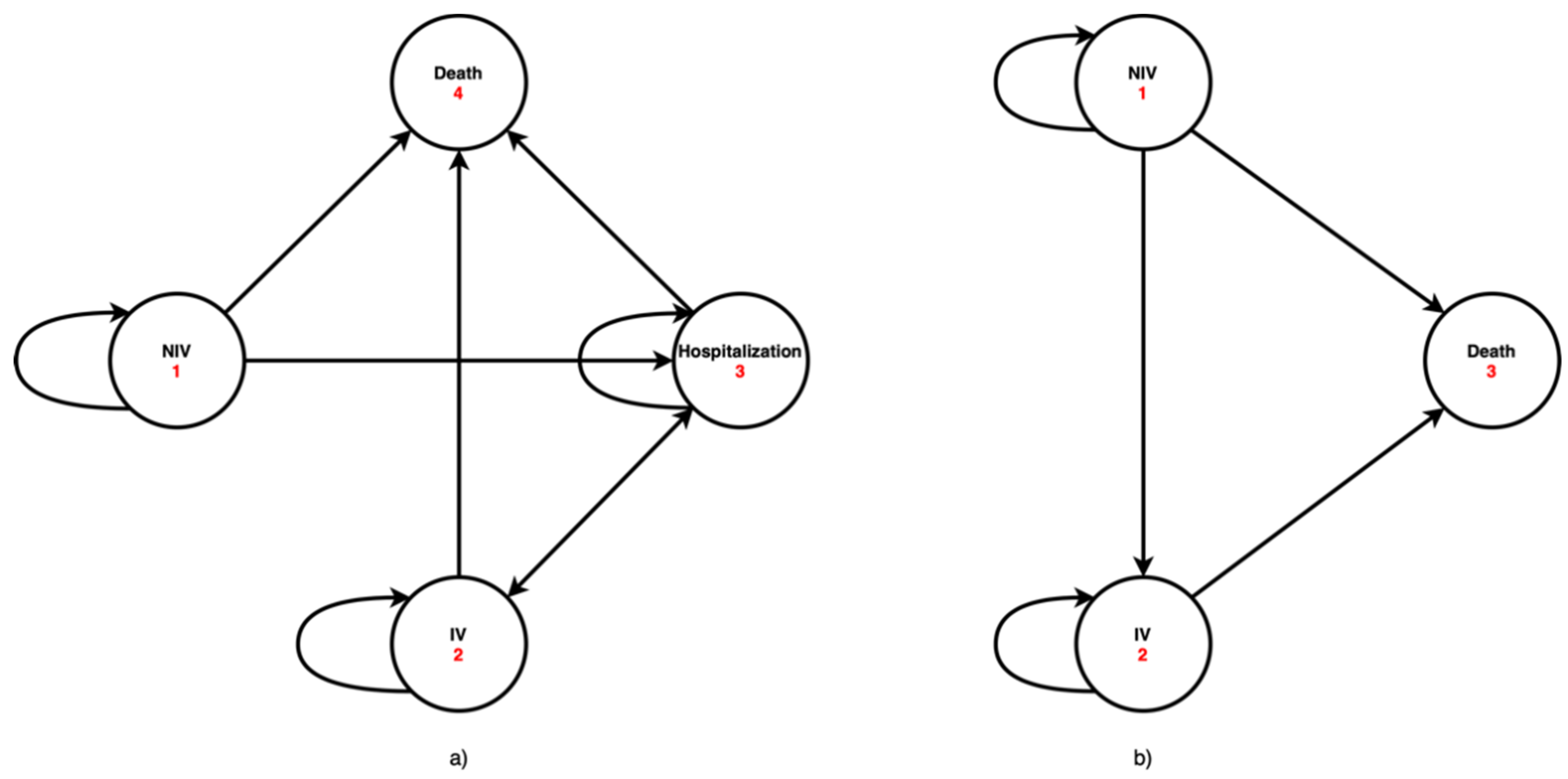
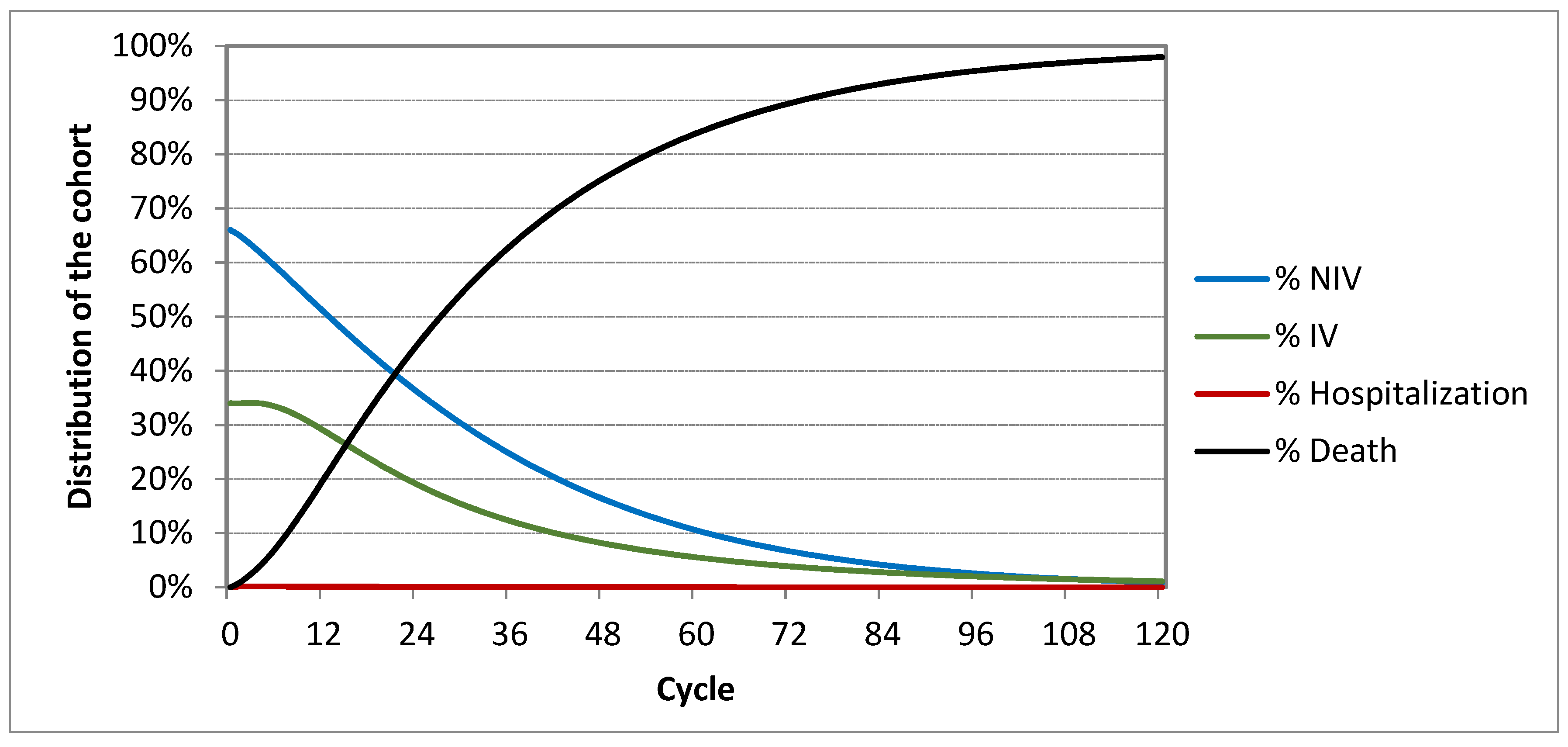
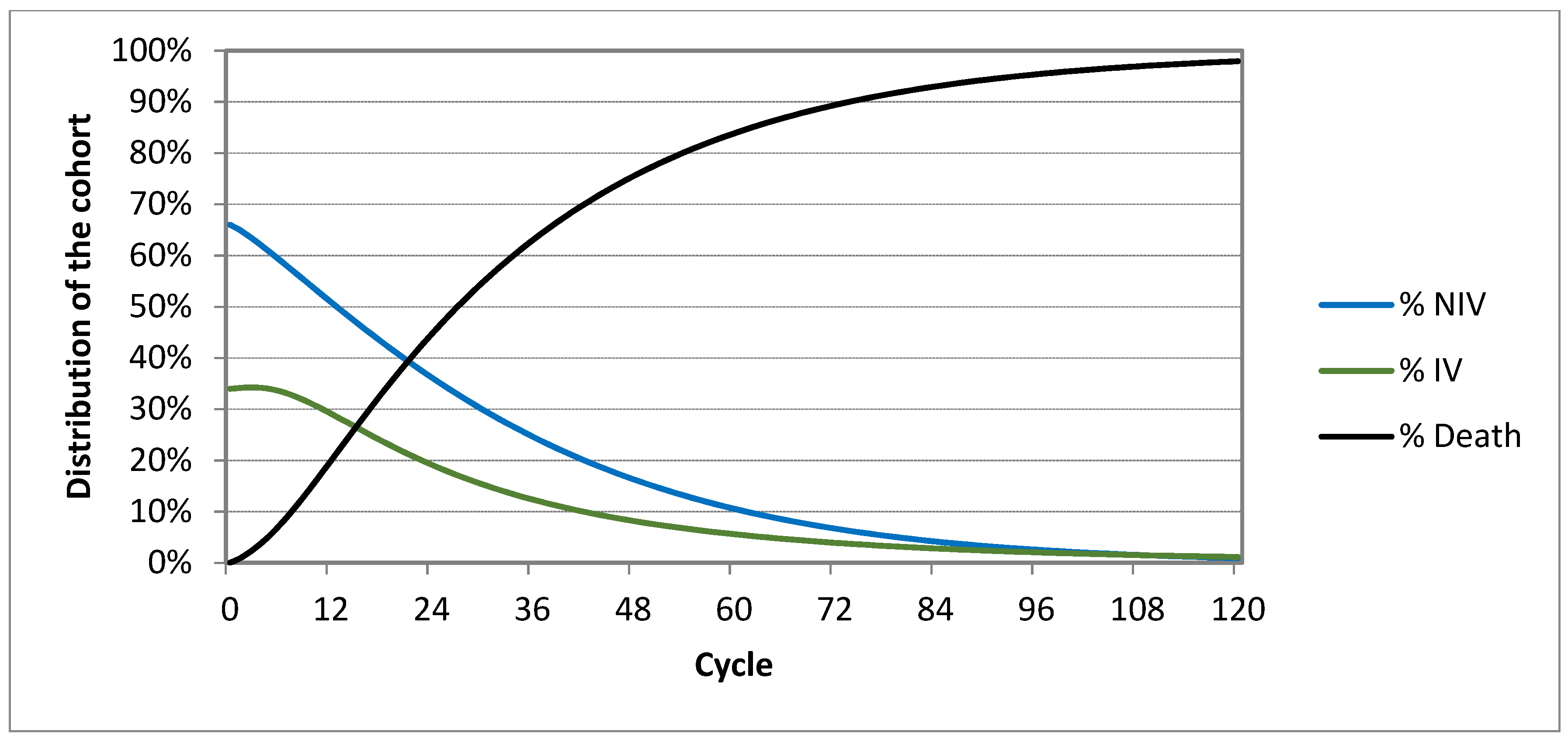
3.1. Markov Models Analysis
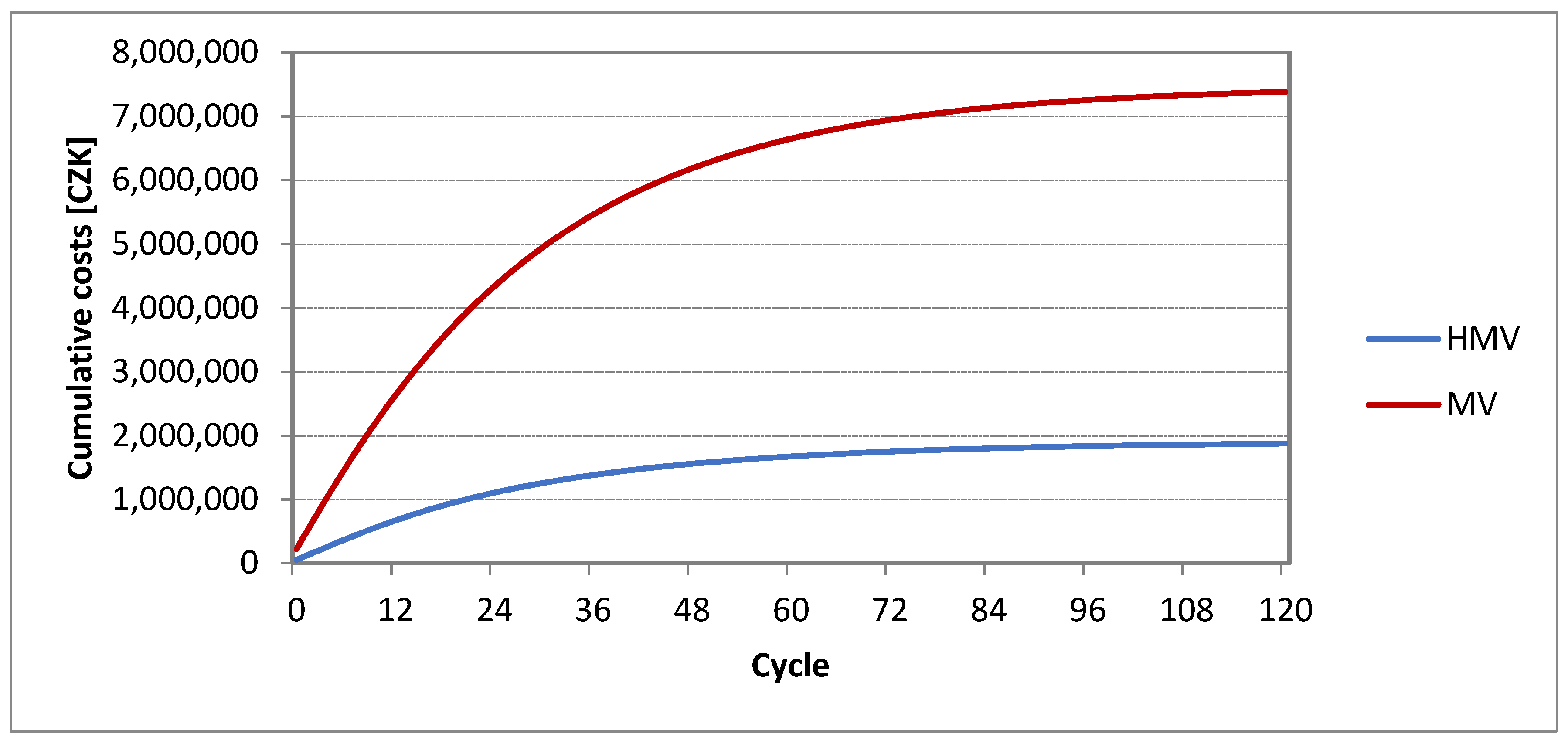
3.2. Cost–Utility Analysis
3.3. Sensitivity Analysis
3.4. Scenario Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rimmer, K.P.; Kaminska, M.; Nonoyama, M.; Giannouli, E.; Maltais, F.; Morrison, D.L.; O’Connell, C.; Petrof, B.J.; McKim, D.A. Home mechanical ventilation for patients with Amyotrophic Lateral Sclerosis: A Canadian Thoracic Society clinical practice guideline. Can. J. Respir. Crit. Care Sleep Med. 2019, 3, 9–27. [Google Scholar] [CrossRef]
- Andersen, P.M.; Abrahams, S.; Borasio, G.D.; de Carvalho, M.; Chio, A.; Van Damme, P.; Hardiman, O.; Kollewe, K.; Morrison, K.E.; Petri, S.; et al. EFNS guidelines on the Clinical Management of Amyotrophic Lateral Sclerosis (MALS)—Revised report of an EFNS task force. Eur. J. Neurol. 2012, 19, 360–375. [Google Scholar] [CrossRef]
- Radunovic, A.; Annane, D.; Rafiq, M.K.; Brassington, R.; Mustfa, N. Mechanical ventilation for amyotrophic lateral sclerosis / motor neuron disease. Cochrane Database Syst. Rev. 2017, 28, CD004427. [Google Scholar] [CrossRef]
- Sorrentino, P.; Rucco, R.; Francesca, J.; Trojsi, F.; Anna, L.; BaseliceFabio, F.; Femiano, C.; Santangelo, G.; Granata, C.; Vettoliere, A.; et al. Brain functional networks become more connected as amyotrophic lateral sclerosis progresses: A source level magnetoencephalographic study. NeuroImage Clin. 2018, 20, 564–571. [Google Scholar] [CrossRef]
- Marchese, S.; Lo Coco, D.; Lo Coco, A. Outcome and attitudes toward home tracheostomy ventilation of consecutive patients: A 10-year experience. Respir. Med. 2008, 102, 430–436. [Google Scholar] [CrossRef]
- MacIntyre, E.J.; Asadi, L.; Mckim, D.A.; Bagshaw, S.M. Clinical Outcomes Associated with Home Mechanical Ventilation: A Systematic Review. Can. Respir. J. 2016, 2016, 1–10. [Google Scholar] [CrossRef]
- Čabanová, A. Doma by mohlo žít víc ventilovaných pacientů. Med. Trib. 2018, 18, 1–2. [Google Scholar]
- Windisch, W.; Geiseler, J.; Simon, K.; Walterspacher, S.; Dreher, M.; Windisch, W.; Dreher, M.; Geiseler, J.; Siemon, K.; Brambring, J.; et al. German National Guideline for Treating Chronic Respiratory Failure with Invasive and Non-Invasive Ventilation—Revised Edition 2017: Part 2. Respiration 2018, 96, 171–203. [Google Scholar] [CrossRef] [PubMed]
- Windisch, W.; Geiseler, J.; Simon, K.; Walterspacher, S.; Dreher, M.; Brambring, J.; Dellweg, D.; Grolle, B.; Hirschfeld, S.; Köhnlein, T.; et al. German National Guideline for Treating Chronic Respiratory Failure with Invasive and Non-Invasive Ventilation: Revised Edition 2017—Part 1. Respiration 2018, 96, 66–97. [Google Scholar] [CrossRef] [PubMed]
- McKim, D.A.; Road, J.; Avendano, M.; Abdool, S.; Côté, F.; Duguid, N.; Fraser, J.; Maltais, F.; Morrison, D.L.; O’Connell, C.; et al. Home mechanical ventilation: A Canadian Thoracic Society clinical practice guideline. Can. Respir. J. 2011, 18, 197–215. [Google Scholar] [CrossRef] [PubMed]
- Make, B.J.; Hill, N.S.; Goldberg, A.I.; Bach, J.R.; Dunne, P.E.; Heffner, J.E.; Keens, T.G.; O’Donohue, W.J.; Oppenheimer, E.A.; Robert, D. Mechanical Ventilation Beyond the Intensive Care Unit. Chest 1998, 113, 289S–344S. [Google Scholar] [CrossRef] [PubMed]
- Všeobecná zdravotní pojišťovna ČR. Úhradový katalog VZP-ZP-Metodika; VZP ČR: Prague, Czech Republic, 2020. [Google Scholar]
- Simonds, A.K. Home Mechanical Ventilation: An Overview. Ann. Am. Thorac. Soc. 2016, 13, 2035–2044. [Google Scholar] [CrossRef] [PubMed]
- Valko, L.; Baglyas, S.; Gal, J.; Lorx, A. National survey: Current prevalence and characteristics of home mechanical ventilation in Hungary. BMC Pulm. Med. 2018, 18, 754. [Google Scholar] [CrossRef] [PubMed]
- Garner, D.J.; Berlowitz, D.J.; Douglas, J.; Harkness, N.; Howard, M.; Mcardle, N.; Naughton, M.T.; Neill, A.; Piper, A.; Yeo, A.; et al. Home mechanical ventilation in Australia and New Zealand. Eur. Respir. J. 2013, 41, 39–45. [Google Scholar] [CrossRef]
- Dreyer, P.; Lorenzen, C.K.; Schou, L.; Felding, M. Survival in ALS with home mechanical ventilation non-invasively and invasively: A 15-year cohort study in west Denmark. Amyotroph. Lateral Scler. Front. Degener. 2014, 15, 62–67. [Google Scholar] [CrossRef]
- Hirose, T.; Kimura, F.; Tani, H.; Ota, S.; Tsukahara, A.; Sano, E.; Shigekiyo, T.; Nakamura, Y.; Kakiuchi, K.; Motoki, M.; et al. Clinical characteristics of long-term survival with noninvasive ventilation and factors affecting the transition to invasive ventilation in amyotrophic lateral sclerosis. Muscle Nerve 2018, 58, 770–776. [Google Scholar] [CrossRef]
- TreeAge Pro Healthcare R2.1, Software for health economic modelling to analyze medical treatment decisions; TreeAge Software: Williamstown, MA, USA, 2020.
- A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020.
- Parlament České Republiky. Zákon Č. 48/1997 Sb., o Veřejném Zdravotním Pojištění a o Změně a Doplnění Některých Souvisejících Zákonů; Tiskárna Ministerstva Vnitra: Prague, Czech Republic, 1997; pp. 1–118.
- Všeobecná Zdravotní Pojišťovna ČR. METODIKA—Postup Při Realizaci Invazivní Domácí Umělé Plicní Ventilace (DUPV) u Nových Pacientů; VZP ČR: Prague, Czech republic, 2019. [Google Scholar]
- Všeobecná Zdravotní Pojišťovna ČR. Zdravotní Výkony. Available online: https://www.vzp.cz/poskytovatele/ciselniky/zdravotni-vykony (accessed on 20 March 2020).
- Ministerstvo Zdravotnictví ČR. Vyhláška Č. 201/2018 Sb., o Stanovení Hodnot Bodu, Výše Úhrad Hrazených Služeb a Regulačních Omezení Pro Rok 2019; Tiskárna Ministerstva Vnitra: Prague, Czech Republic, 2019. [Google Scholar]
- Mičudová, E.; Lorenc, V. Srovnání Ekonomických Nákladů Na Pacienta v Programu Domácí Umělá Plicní Ventilace a Pacienta Hospitalizovaného Na Jednotce Dlouhodobé Intenzivní Péče; FN Brno: Brno, Czech Republic, 2012. [Google Scholar]
- Česká Farmakoekonomická Společnost. Doporučené Postupy Pro Zdravotně-Ekonomická Hodnocení v ČR: Česká Společnost Pro Farmakoekonomiku a Hodnocení Zdravotnických Technologií (ČFES); Česká Farmakoekonomická Společnost: Prague, Czech Republic, 2020. [Google Scholar]
- Český statistický úřad Inflace-druhy, definice, tabulky. Available online: https://www.czso.cz/csu/czso/mira_inflace (accessed on 20 March 2020).
- Parlament České Republiky. Zákon Č. 372/2011 Sb., o Zdravotních Službách a Podmínkách Jejich Poskytování (Zákon o Zdravotních Službách); Tiskárna Ministerstva Vnitra: Prague, Czech Republic, 2011.
- Ministerstvo Zdravotnictví ČR. Vyhláška Č. 134/1998 Sb., Kterou Se Vydává Seznam Zdravotních Výkonů s Bodovými Hodnotami; Tiskárna Ministerstva Vnitra: Praga, Czech Republic, 1998. [Google Scholar]
- Ministerstvo zdravotnictví ČR Zákon č. 268/2019 Sb., o stanovení hodnot bodu, výše úhrad hrazených služeb a regulačních omezení pro rok 2020; Tiskárna Ministerstva Vnitra: Praha, Czech Republic, 2019. [Google Scholar]
- Goodman, C.S. HTA 101: Introduction to the health technology assessment; National Library of Medicine: Bethesda, MD, USA, 2014.
- Nauffal, D.; Doménech, R.; Martinéz García, M.A.; Compte, L.; Macián, V.; Perpiná, M. Noninvasive positive pressure home ventilation in restrictive disorders: Outcome and impact on health-related quality of life. Respir. Med. 2002, 96, 777–783. [Google Scholar] [CrossRef][Green Version]
- Ara, R.; Brazier, J. Deriving an algorithm to convert the eight mean SF-36 dimension scores into a mean EQ-5D preference-based score from published studies (where patient level data are not available). Value Health. 2008, 11, 1131–1143. [Google Scholar] [CrossRef]
- Rousseau, M.C.; Pietra, S.; Blaya, J.; Catala, A. Quality of life of ALS and LIS patients with and without invasive mechanical ventilation. J. Neurol. 2011, 258, 1801–1804. [Google Scholar] [CrossRef]
- Chatwin, M.; Nickol, A.H.; Morrell, M.J.; Polkey, M.I.; Simonds, A.K. Randomised trial of inpatient versus outpatient initiation of home mechanical ventilation in patients with nocturnal hypoventilation. Respir. Med. 2008, 102, 1528–1535. [Google Scholar] [CrossRef]
- Windisch, W. Impact of home mechanical ventilation on health-related quality of life. Eur. Respir. J. 2008, 32, 1328–1336. [Google Scholar] [CrossRef] [PubMed]
- López-Campos, J.L.; Failde, I.; Jiménez, A.L.; Jiménez, F.M.; Cortés, E.B.; Benítez Moya, J.M.; García, R.A.; Windischg, W. Health-Related Quality of Life of Patients Receiving Home May Mechanical Ventilation: The Spanish Version of the Severe Respiratory Insufficiency Questionnaire. Arch. Bronconeumol. 2006, 42, 588–593. [Google Scholar] [CrossRef]
- Euteneuer, S.; Windisch, W.; Suchi, S.; Köhler, D.; Jones, P.W.; Schönhofer, B. Health-related quality of life in patients with chronic respiratory failure after long-term mechanical ventilation. Respir. Med. 2006, 100, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Doménech-Clar, R.; Nauffal-Manssur, D.; Compte-Torrero, L.; Rosales-Almazán, M.D.; Martínez-Pérez, E.; Soriano-Melchor, E. Adaptation and follow-up to noninvasive home mechanical ventilation: Ambulatory versus hospital. Respir. Med. 2008, 102, 1521–1527. [Google Scholar] [CrossRef] [PubMed]
- Doménech-Clar, R.; Nauffal-Manzur, D.; Perpiñá-Tordera, M.; Compte-Torrero, L.; Macián-Gisbert, V. Home mechanical ventilation for restrictive thoracic diseases: Effects on patient quality-of-life and hospitalizations. Respir. Med. 2003, 97, 1320–1327. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Oga, T.; Windisch, W.; Handa, T.; Hirai, T.; Chin, K. Health-related quality of life measurement in patients with chronic respiratory failure. Respir. Investig. 2018, 56, 214–221. [Google Scholar] [CrossRef]
- Huttmann, S.E.; Windisch, W.; Storre, J.H. Invasive home mechanical ventilation: Living conditions and health-related quality of life. Respiration 2015, 89, 312–321. [Google Scholar] [CrossRef]
- Huttmann, S.E.; Magnet, F.S.; Karagiannidis, C.; Storre, J.H.; Windisch, W. Quality of life and life satisfaction are severely impaired in patients with long-term invasive ventilation following ICU treatment and unsuccessful weaning. Ann. Intensive Care 2018, 8. [Google Scholar] [CrossRef]
- Lloyd-Owen, S.J.; Donaldson, G.C.; Ambrosino, N.; Escarabill, J.; Farre, R.; Fauroux, B.; Robert, D.; Schoenhofer, B.; Simonds, A.K.; Wedzicha, J.A. Patterns of home mechanical ventilation use in Europe: Results from the Eurovent survey. Eur. Respir. J. 2005, 25, 1025–1031. [Google Scholar] [CrossRef]
- Chandra, K.; Blackhouse, G.; McCurdy, B.R.; Bornstein, M.; Campbell, K.; Costa, V.; Franek, J.; Kaulback, K.; Levin, L.; Sehatzadeh, S.; et al. Cost-effectiveness of interventions for chronic obstructive pulmonary disease (COPD) using an Ontario policy model. Ont. Health Technol. Assess. Ser. 2012, 12, 1–61. [Google Scholar]
- Masefield, S.; Vitacca, M.; Dreher, M.; Kampelmacher, M.; Escarrabill, J.; Paneroni, M.; Powell, P.; Ambrosino, N. Attitudes and preferences of home mechanical ventilation users from four European countries: An ERS/ELF survey. ERJ Open Res. 2017, 3. [Google Scholar] [CrossRef] [PubMed]
- Pomares, X. Noninvasive Mechanical Ventilation. Reflections on Home. 2014, 50, 85–86. [Google Scholar]
- Fernández-Alvarez, R.; Rubinos-Cuadrado, G.; Cabrera-Lacalzada, C.; Galindo-Morales, R.; Gullón-Blanco, J.A.; González-Martín, I. Home mechanical ventilation: Dependency and burden of care in the home. Arch. Bronconeumol. 2009, 45, 383–386. [Google Scholar] [CrossRef]
- Moss, A.H.; Oppenheimer, E.A.; Casey, P.; Cazzolli, P.A.; Roos, R.P.; Stocking, C.B.; Siegler, M. Patients with amyotrophic lateral sclerosis receiving long-term mechanical ventilation: Advance care planning and outcomes. Chest 1996, 110, 249–255. [Google Scholar] [CrossRef]
- Luján, M.; Moreno, A.; Veigas, C.; Pomares, X.; Domingo, C. Non-invasive home mechanical ventilation: Effectiveness and efficiency of an outpatient initiation protocol compared with the standard in-hospital model. Respir. Med. 2007, 101, 1177–1182. [Google Scholar] [CrossRef]
- Pallero, M.; Puy, C.; Güell, R.; Pontes, C.; Martí, S.; Torres, F.; Antón, A.; Munoz, X. Ambulatory adaptation to noninvasive ventilation in restrictive pulmonary disease: A randomized trial with cost assessment. Respir. Med. 2014, 1014–1022. [Google Scholar] [CrossRef]
- Geiseler, J.; Karg, O.; Börger, S.; Becker, K.; Zimolong, A. Invasive home mechanical ventilation, mainly focused on neuromuscular disorders. GMS Health Technol. Assess. 2010, 6, 1–10. [Google Scholar]
- Bach, J.R. The ventilator-assisted individual. Cost analysis of institutionalization vs rehabilitation and in-home management. Chest 2015. [Google Scholar] [CrossRef]
- MacIntyre, N.R.; Epstein, S.K.; Carson, S.; Muldoon, S.R. Management of patients requiring prolonged mechanical ventilation: Report of a NAMDRC Consensus Conference. Chest 2006, 128. [Google Scholar] [CrossRef]
- Vianello, A.; Arcaro, G.; Palmieri, A.; Ermani, M.; Braccioni, F.; Gallan, F.; Soraru’, G.; Pegoraro, E. Survival and quality of life after tracheostomy for acute respiratory failure in patients with amyotrophic lateral sclerosis. J. Crit. Care 2011, 26. [Google Scholar] [CrossRef]
- Bourke, S.C.; Tomlinson, M.; Williams, T.L.; Bullock, R.E.; Shaw, P.J.; Gibson, G.J. Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: A randomised controlled trial. Lancet Neurol. 2006, 5, 140–147. [Google Scholar] [CrossRef]
- Ackrivo, J.; Hansen-Flaschen, J.; Jones, B.L.; Paul Wileyto, E.; Schwab, R.J.; Elman, L.; Kawut, S.M. Classifying Patients with Amyotrophic Lateral Sclerosis by Changes in FVC A Group-based Trajectory Analysis. Am. J. Respir. Crit. Care Med. 2019, 200, 1513–1521. [Google Scholar] [CrossRef]
- Kaub-Wittemer, D.; Von Steinbüchel, N.; Wasner, M.; Laier-Groeneveld, G.; Borasio, G.D. Quality of life and psychosocial issues in ventilated patients with amyotrophic lateral sclerosis and their caregivers. J. Pain Symptom Manage. 2003, 26, 890–896. [Google Scholar] [CrossRef]
- Mustfa, N.; Walsh, E.; Bryant, V.; Lyall, R.A.; Addington-Hall, J.; Goldstein, L.H.; Donaldson, N.; Polkey, M.I.; Moxham, J.; Leigh, P.N. The effect of noninvasive ventilation on ALS patients and their caregivers. Neurology 2006, 66, 1211–1217. [Google Scholar] [CrossRef] [PubMed]
- Gelinas, D.F.; O’Connor, P.; Miller, R.G. Quality of life for ventilator-dependent ALS patients and their caregivers. J. Neurol. Sci. 1998, 160, 134–136. [Google Scholar] [CrossRef]

| Health State HMV | Branch | Probability | Data Source | Health State | Probability | Data Source |
| NIV | Survival | Evaluation to the sum of 1 | -- | NIV | 0.99812 | [17] |
| Hospitalization | 0.00188 | [17] | ||||
| Death | Weibull probability | [16] | Death | -- | -- | |
| IV | Survival | Evaluation to the sum of 1 | -- | IV | 0.999 | Expert estimation 1 |
| Hospitalization | 0.001 | Expert estimation 1 | ||||
| Death | Log-normal probability | [16] | Death | -- | -- | |
| Hospitalization | -- | -- | -- | Hospitalization | 0.01 | Expert estimation 1 |
| -- | -- | -- | IV | 0.95 | Expert estimation 1 | |
| -- | -- | -- | Death | 0.04 | Expert estimation 1 | |
| Death | -- | -- | -- | -- | -- | -- |
| Health state MV | Branch | Probability | Data source | Health state | Probability | Data source |
| NIV | Survival | Evaluation to the sum of 1 | -- | NIV | 0.99812 | [17] |
| IV | 0.00188 | [17] | ||||
| Death | Weibull probability | [16] | Death | -- | -- | |
| IV | -- | -- | -- | IV | Evaluation to the sum of 1 | [16] |
| -- | -- | -- | Death | Log-normal probability | [16] | |
| Death | -- | -- | -- | --- | -- | -- |
| Type of Costs | 1 Day | 1 Month (30 Days) | 1 Year (365 Days) |
|---|---|---|---|
| Technical support | CZK45 | CZK 1338 | CZK 16,286 |
| Nursing care and other costs | CZK 524 | CZK 15,720 | CZK 191,266 |
| Total | CZK 569 | CZK 17,058 | CZK 207,552 |
| Mobile Patient | Immobile Patient | |||
|---|---|---|---|---|
| Type of Costs | 1 Month (30 Days) | 1 Year (365 Days) | 1 Month (30 Days) | 1 Year (365 Days) |
| Technical support | CZK 20,550 | CZK 250,025 | CZK 23,550 | CZK 286,525 |
| Nursing care | CZK 38,809 | CZK 472,175 | CZK 38,809 | CZK 472,175 |
| Other costs | CZK 68,192 | CZK 829,671 | CZK 68,192 | CZK 829,671 |
| Total | CZK 127,551 | CZK 1,552,006 | CZK 130,551 | CZK 1,588,371 |
| Performance Code | Medical Performance | Point Value | Payment for 1 Day |
|---|---|---|---|
| OD 00017 | Follow-up intensive care | 9364 | CZK 11,276 |
| OD 00015 | Follow-up ventilation care | 6150 | CZK 7483 |
| Type of Costs | Costs |
|---|---|
| Medical performance | CZK 2055.46 |
| Transport services | CZK 2725.68 |
| Separately charged material or medication | CZK 450 |
| Total | CZK 5231.14 |
| Health State HMV | Costs Per Month (30 Days) |
| NIV | CZK 17,058 |
| IV | CZK 129,051 |
| Hospitalization | 1st to 3rd month CZK 333,277 (NIP), following months CZK 224,502 (NVP) |
| Transfer | CZK 5231.14 |
| Death | -- |
| Health state MV | Costs per month (30 days) |
| NIV | CZK 224,502 (NVP 1) |
| IV | CZK 224,502 (NVP 1) |
| Death | -- |
| Strategy | Costs [CZK] | Incremental Costs [CZK] | Utilities [QALY] | Incremental Utilities [QALY] | C/QALY [CZK] | ICUR [CZK] |
|---|---|---|---|---|---|---|
| HMV | 1,877,076 | 0 | 12.57 | 0 | 149,292 | 0 |
| MV | 7,386,629 | −5,509,554 | 11.32 | 1.25 | 652,418 | −4,403,259 |
| Strategy | Costs [CZK] | Utilities [QALY] | ICUR [CZK] | |
|---|---|---|---|---|
| −30% | HMV | 1,877,076 | 12.57 | 0 |
| MV | 7,386,629 | 8.81 | −1,463,995 | |
| −20% | HMV | 1,877,076 | 12.57 | 0 |
| MV | 7,386,629 | 10.06 | −2,197,399 | |
| −10% | HMV | 1,877,076 | 12.57 | 0 |
| MV | 7,386,629 | 11.32 | −4,403,259 | |
| 0% | HMV | 1,877,076 | 12.58 | 0 |
| MV | 7,386,629 | 12.58 | 1,143,504,522 1 | |
| +10% | HMV | 1,877,076 | 12.58 | 0 |
| MV | 7,386,629 | 13.84 | 4,369,607 | |
| +20% | HMV | 1,877,076 | 12.58 | 0 |
| MV | 7,386,629 | 15.10 | 2,188,986 | |
| +30% | HMV | 1,877,076 | 12.58 | 0 |
| MV | 7,386,629 | 16.35 | 1,460,256 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gajdoš, O.; Rožánek, M.; Donin, G.; Kamenský, V. Cost–Utility Analysis of Home Mechanical Ventilation in Patients with Amyotrophic Lateral Sclerosis. Healthcare 2021, 9, 142. https://doi.org/10.3390/healthcare9020142
Gajdoš O, Rožánek M, Donin G, Kamenský V. Cost–Utility Analysis of Home Mechanical Ventilation in Patients with Amyotrophic Lateral Sclerosis. Healthcare. 2021; 9(2):142. https://doi.org/10.3390/healthcare9020142
Chicago/Turabian StyleGajdoš, Ondřej, Martin Rožánek, Gleb Donin, and Vojtěch Kamenský. 2021. "Cost–Utility Analysis of Home Mechanical Ventilation in Patients with Amyotrophic Lateral Sclerosis" Healthcare 9, no. 2: 142. https://doi.org/10.3390/healthcare9020142
APA StyleGajdoš, O., Rožánek, M., Donin, G., & Kamenský, V. (2021). Cost–Utility Analysis of Home Mechanical Ventilation in Patients with Amyotrophic Lateral Sclerosis. Healthcare, 9(2), 142. https://doi.org/10.3390/healthcare9020142






