Public Trust and Policy Compliance during the COVID-19 Pandemic: The Role of Professional Trust
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Variable Construction and Measures
2.3. Statistical Analyses
3. Results
3.1. Sample Characteristics
3.2. Characteristics of Study Variables
3.3. Hierarchical Regression Results
4. Discussion
Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Scholz, J.T. Trust, taxes, and compliance. In Trust and Governance; Braithwaite, V., Levi, M., Eds.; Russell Sage Foundation: New York, NY, USA, 1998; pp. 135–166. [Google Scholar]
- Shi, T. Cultural Values and Political Trust: A Comparison of the People’s Republic of China and Taiwan. Comp. Polit. 2001, 33, 401. [Google Scholar] [CrossRef]
- Levi, M.; Stoker, L. Political Trust and Trustworthiness. Annu. Rev. Polit. Sci. 2000, 3, 475–507. [Google Scholar] [CrossRef]
- Dalton, R.J. Democratic Challenges, Democratic Choices: The Erosion of Political Support in Advanced Industrial Democracies; Oxford University Press: Oxford, UK, 2004. [Google Scholar]
- Murphy, K. Regulating More Effectively: The Relationship between Procedural Justice, Legitimacy, and Tax Non-compliance. J. Law Soc. 2005, 32, 562–589. [Google Scholar] [CrossRef]
- Tyler, T.R. Why people Obey the Law? Princeton University Press: Princeton, NJ, USA, 2006. [Google Scholar]
- Chanley, V.A.; Rudolph, T.J.; Rahn, W.M. The Origins and Consequences of Public Trust in Government. Public Opin. Q. 2000, 64, 239–256. [Google Scholar] [CrossRef] [PubMed]
- Cui, E.; Tao, R.; Warner, T.J.; Yang, D.L. How Do Land Takings Affect Political Trust in Rural China? Polit. Stud. 2015, 63, 91–109. [Google Scholar] [CrossRef]
- Güzel, S.A.; Özer, G.; Özcan, M. The effect of the variables of tax justice perception and trust in government on tax compliance: The case of Turkey. J. Behav. Exp. Econ. 2019, 78, 80–86. [Google Scholar] [CrossRef]
- Marien, S.; Hooghe, M. Does political trust matter? An empirical investigation into the relation between political trust and support for law compliance. Eur. J. Polit. Res. 2011, 50, 267–291. [Google Scholar] [CrossRef]
- Earle, T.C.; Siegrist, M.; Gutscher, H. Trust, Risk Perception and the TCC Model of Cooperation. In Trust in Cooperative Risk Management; Routledge: London, UK, 2010; pp. 18–66. [Google Scholar] [CrossRef]
- Gilles, I.; Bangerter, A.; Clémence, A.; Green, E.G.T.; Krings, F.; Staerklé, C.; Wagner-Egger, P. Trust in medical organizations predicts pandemic (H1N1) 2009 vaccination behavior and perceived efficacy of protection measures in the Swiss public. Eur. J. Epidemiol. 2011, 26, 203–210. [Google Scholar] [CrossRef] [Green Version]
- Van Der Weerd, W.; Timmermans, D.R.; Beaujean, D.J.; Oudhoff, J.; Van Steenbergen, J.E. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in the Netherlands. BMC Public Health 2011, 11, 575. [Google Scholar] [CrossRef] [Green Version]
- Deurenberg-Yap, M.; Foo, L.L.; Low, Y.Y.; Chan, S.P.; Vijaya, K.; Lee, M. The Singaporean response to the SARS outbreak: Knowledge sufficiency versus public trust. Health Promot. Int. 2005, 20, 320–326. [Google Scholar] [CrossRef]
- Bangerter, A.; Krings, F.; Mouton, A.; Gilles, I.; Green, E.G.T.; Clémence, A. Longitudinal Investigation of Public Trust in Institutions Relative to the 2009 H1N1 Pandemic in Switzerland. PLoS ONE 2012, 7, e49806. [Google Scholar] [CrossRef] [Green Version]
- Blair, R.A.; Morse, B.S.; Tsai, L.L. Public health and public trust: Survey evidence from the Ebola Virus Disease epidemic in Liberia. Soc. Sci. Med. 2017, 172, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Vinck, P.; Pham, P.N.; Bindu, K.K.; Bedford, J.; Nilles, E.J. Institutional trust and misinformation in the response to the 2018–19 Ebola outbreak in North Kivu, DR Congo: A population-based survey. Lancet Infect. Dis. 2019, 19, 529–536. [Google Scholar] [CrossRef] [Green Version]
- Woskie, L.R.; Fallah, M. Overcoming distrust to deliver universal health coverage: Lessons from Ebola. BMJ 2019, 366, l5482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexopoulos, A.N.; Buckley, F. What Trust Matters When. Group Organ. Manag. 2013, 38, 361–391. [Google Scholar] [CrossRef]
- Siegrist, M.; Zingg, A. The Role of Public Trust During Pandemics. Eur. Psychol. 2014, 19, 23–32. [Google Scholar] [CrossRef]
- Quevauviller, P.; Balabanis, P.; Fragakis, C.; Weydert, M.; Oliver, M.; Kaschl, A.; Arnold, G.; Kroll, A.; Galbiati, L.; Zaldivar, J.M.; et al. Science-policy integration needs in support of the implementation of the EU Water Framework Directive. Environ. Sci. Policy 2005, 8, 203–211. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Freimuth, V.S.; Jamison, A.; An, J.; Hancock, G.R.; Quinn, S.C. Determinants of trust in the flu vaccine for African Americans and Whites. Soc. Sci. Med. 2017, 193, 70–79. [Google Scholar] [CrossRef]
- Fu, L.Y.; Zimet, G.D.; Latkin, C.A.; Joseph, J.G. Associations of trust and healthcare provider advice with HPV vaccine acceptance among African American parents. Vaccine 2017, 35, 802–807. [Google Scholar] [CrossRef] [Green Version]
- Giambi, C.; Fabiani, M.; D’Ancona, F.; Ferrara, L.; Fiacchini, D.; Gallo, T.; Martinelli, D.; Pascucci, M.G.; Prato, R.; Filia, A.; et al. Parental vaccine hesitancy in Italy—Results from a national survey. Vaccine 2018, 36, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Ahlers, A.L. Blue sky fabrication in China: Science-policy integration in air pollution regulation campaigns for mega-events. Environ. Sci. Policy 2019, 94, 135–142. [Google Scholar] [CrossRef] [Green Version]
- Cheng, Y.; Yu, J.; Shen, Y.; Huang, B. Coproducing Responses to COVID-19 with Community-Based Organizations: Lessons from Zhejiang Province, China. Public Adm. Rev. 2020, 80, 866–873. [Google Scholar] [CrossRef] [PubMed]
- Shahbari, N.A.E.; Gesser-Edelsburg, A.; Mesch, G.S. Perceived trust in the health system among mothers and nurses and its relationship to the issue of vaccinations among the Arab population of Israel: A qualitative research study. Vaccine 2020, 38, 29–38. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 31 January 2021).
- JHU CSSE. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. 2020. Available online: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 (accessed on 31 December 2020).
- World Health Organization Thailand. Point of Entry Screening and Quarantine Systems Enabled Thailand to Control COVID-19 2020. Available online: https://www.who.int/thailand/news/feature-stories/detail/point-of-entry-screening-and-quarantine-systems-enabled-thailand-to-control-covid-19 (accessed on 31 January 2021).
- Department of Disease Control. Coronavirus Disease (COVID-19) 2020. Available online: https://ddc.moph.go.th/viralpneumonia/index.php (accessed on 31 January 2021).
- Almutairi, A.F.; Banimustafa, A.; Alessa, Y.M.; Almutairi, S.B.; Almaleh, Y. Public Trust and Compliance with the Precautionary Measures Against COVID-19 Employed by Authorities in Saudi Arabia. Health Policy Polit. Sante 2020, 13, 753–760. [Google Scholar] [CrossRef]
- Bargain, O.; Aminjonov, U. Trust and compliance to public health policies in times of COVID-19. J. Public Econ. 2020, 192, 104316. [Google Scholar] [CrossRef]
- Chan, H.F.; Brumpton, M.; MacIntyre, A.; Arapoc, J.; Savage, D.A.; Skali, A.; Stadelmann, D.; Torgler, B. How confidence in health care systems affects mobility and compliance during the COVID-19 pandemic. PLoS ONE 2020, 15, e0240644. [Google Scholar] [CrossRef]
- Nivette, A.; Ribeaud, D.; Murray, A.; Steinhoff, A.; Bechtiger, L.; Hepp, U.; Shanahan, L.; Eisner, M. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Soc. Sci. Med. 2021, 268, 113370. [Google Scholar] [CrossRef]
- Brouard, S.; Vasilopoulos, P.; Becher, M. Sociodemographic and Psychological Correlates of Compliance with the COVID-19 Public Health Measures in France. Can. J. Polit. Sci. 2020, 53, 253–258. [Google Scholar] [CrossRef] [Green Version]
- Fink, A. The Survey Handbook; Indian Institute of Management Kozhikode: Kerala, India, 2003. [Google Scholar]
- Pan-ngum, W.; Poomchaichote, T.; Peerawaranun, P.; Kulpijit, N.; Osterrieder, A.; Waithira, N.; Mukaka, M.; Naemiratch, B.; Chanviriyavuth, R.; Asarath, S.; et al. Perspectives on public health interventions in the management of the COVID-19 pandemic in Thailand. Wellcome Open Res. 2020, 5, 245. [Google Scholar] [CrossRef]
- National Statistical Office. Average Number of Employees, Wages 2020. Available online: http://service.nso.go.th/nso/web/statseries/statseries05.html (accessed on 31 January 2021).
- IBM Corp. IBM SPSS Statistics for Windows, Version 23.0. IBM Corp: Armonk, NY, 2015.
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Nunnally, J.; Bernstein, I. Psychometric Theory; Tata McGraw-Hill Education: New Delhi, India, 2010. [Google Scholar]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Shuja, K.H.; Aqeel, M.; Jaffar, A.; Ahmed, A. COVID-19 Pandemic and Impending Global Mental Health Implications. Psychiatr. Danub. 2020, 32, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Bodas, M.; Peleg, K. Self-Isolation Compliance in the COVID-19 Era Influenced by Compensation: Findings from a Recent Survey in Israel. Health Aff. 2020, 39, 936–941. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, X.; Yu, J. Public governance mechanism in the prevention and control of the COVID-19: Information, decision-making and execution. J. Chin. Gov. 2020, 5, 178–197. [Google Scholar] [CrossRef] [Green Version]
- JakovljeviĆ, M.; Bjedov, S.; Jaksic, N.; Jakovljevic, I. Covid-19 Pandemia and Public and Global Mental Health from the Perspective of Global Health Security. Psychiatr. Danub. 2020, 32, 6–14. [Google Scholar] [CrossRef]
- Gu, E.; Li, L. Crippled community governance and suppressed scientific/professional communities: A critical assessment of failed early warning for the COVID-19 outbreak in China. Journal of Chinese governance. J. Chin. Gov. 2020, 5, 160–177. [Google Scholar] [CrossRef] [Green Version]
- Huang, H.; Peng, Z.; Wu, H.; Xie, Q. A big data analysis on the five dimensions of emergency management information in the early stage of COVID-19 in China. J. Chin. Gov. 2020, 5, 213–233. [Google Scholar] [CrossRef]
- Thomas, C.W. Maintaining and Restoring Public Trust in Government Agencies and their Employees. Adm. Soc. 1998, 30, 166–193. [Google Scholar] [CrossRef] [Green Version]
- Prado, B. COVID-19 in Brazil: “So what?”. Lancet 2020, 395, 1461. [Google Scholar] [CrossRef]
| Variable | Category | n (%) |
|---|---|---|
| Gender | Male | 312 (38.6) |
| Female | 497 (61.4) | |
| Age | <18 | 33 (4.1) |
| 18–29 | 214 (26.5) | |
| 30–39 | 330 (40.8) | |
| 40–59 | 212 (26.2) | |
| 60 and above | 20 (2.5) | |
| Marital Status | Single | 474 (58.6) |
| Divorced | 40 (4.9) | |
| Married | 295 (36.5) | |
| Education | Below college degree | 206 (25.5) |
| College degree and above | 603 (74.5) | |
| Residence | Bangkok | 452 (55.9) |
| Non-Bangkok | 357 (44.1) | |
| Personal Monthly Income (THB) | <5000 (very low) | 66 (8.2) |
| 5000–15,000 (low income) | 191 (31.8) | |
| 15,000–30,000 (lower-middle) | 247 (30.5) | |
| 30,000–50,000 (upper-middle) | 201 (24.8) | |
| >50,000 (high income) | 104 (12.9) | |
| Perceived vulnerability | Worried | 591 (73.1) |
| Affected | 413 (51.1) |
| Variable | Cronbach’s α | n (%) |
|---|---|---|
| Trust in the Government | 0.82 | |
| Trusts the central government | 170 (21.0) | |
| Trusts the local government | 126 (15.6) | |
| Trusts the Ministry of Public Health | 392 (48.5) | |
| Believes the government to have an effective policy | 218 (26.9) | |
| Believes health system to handle the crisis effectively | 338 (41.8) | |
| Believes health system to provide effective screening services | 268 (33.1) | |
| Believes health system to provide effective treatment services | 368 (45.5) | |
| Trust in Professional Healthcare Workers | 0.85 | |
| Trusts doctor | 651 (80.5) | |
| Trusts dentist | 623 (77.0) | |
| Trusts pharmacist | 567 (70.1) | |
| Trusts nurse | 548 (67.7) | |
| Believes healthcare workers to handle the crisis effectively | 431 (53.3) | |
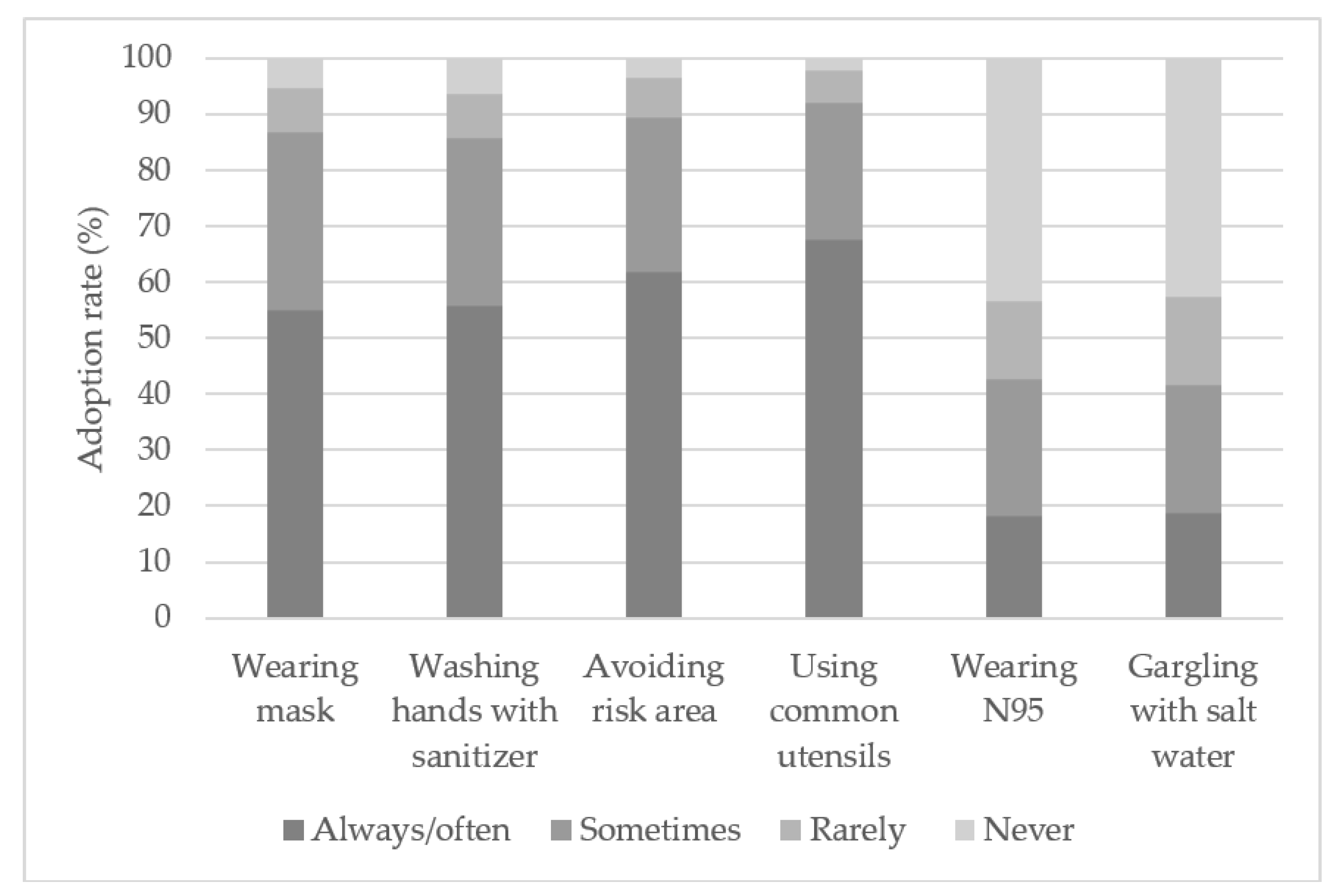
| Compliance with the COVID-19 Control Measures | 0.70 | |
| Wears surgical/facial mask | 765 (94.6) | |
| Washes hands with an alcohol-based sanitizer | 758 (93.7) | |
| Avoids risk area | 780 (96.4) | |
| Uses common utensils when eating with others | 792 (97.9) |
| Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Measures’ compliance | 3.67 | 0.75 | 1 | |||||||||
| 2. Trust in the government | 3.06 | 0.68 | 0.07 * | 1 | ||||||||
| 3. Professional trust | 3.79 | 0.63 | 0.25 ** | 0.39 ** | 1 | |||||||
| 4. Male | 0.39 | 0.49 | −0.04 | 0.09 ** | 0.06 | 1 | ||||||
| 5. Age | 2.97 | 0.89 | 0.02 | 0.04 | 0.03 | 0.01 | 1 | |||||
| 6. Married | 0.36 | 0.48 | 0.09 ** | 0.01 | −0.04 | 0.01 | 0.38 ** | 1 | ||||
| 7. Education | 0.75 | 0.44 | 0.07 | −0.06 | 0.10 ** | −0.14 ** | 0.16 ** | −0.02 | 1 | |||
| 8. Income | 3.11 | 1.15 | 0.05 | −0.09 * | 0.09 * | -0.06 | 0.43 ** | 0.18 ** | 0.50 ** | 1 | ||
| 9. Bangkok | 0.56 | 0.50 | 0.07 * | 0.00 | -0.06 | 0.04 | 0.04 | −0.01 | −0.01 | 0.13 ** | 1 | |
| 10. Worry | 4.01 | 0.91 | 0.22 ** | −0.17 ** | -0.03 | −0.11 ** | −0.05 | −0.01 | 0.05 | 0.02 | 0.10 ** | 1 |
| Group | Wearing Mask | Not Wearing Mask |
|---|---|---|
| Elderly group | 71.4% (25) | 28.6% (10) |
| Non-elderly group | 87.5% (677) | 12.5% (97) |
| Count | 86.8% (702) | 13.2% (107) |
| Variable | Professional Trust | Adoption of Personal Protective Measures | ||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 (Model 1 + Trust in the Government) | Model 3 | Model 4 (Model 3 + Trust in Government) | Model 5 (Model 3 + Professional Trust) | Model 6 (Model 3 + Trust in the Government + Professional Trust) | |
| Control variables | ||||||
| Male | 0.098 * (0.046) | 0.063 (0.042) | −0.020 (0.053) | −0.032 (0.053) | −0.051 (0.052) | −0.052 (0.052) |
| Age | 0.005 (0.029) | −0.020 (0.027) | −0.013 (0.034) | −0.022 (0.034) | −0.014 (0.033) | −0.015 (0.033) |
| Married | −0.068 (0.049) | −0.069 (0.045) | 0.162 ** (0.058) | 0.161 ** (0.057) | 0.183 ** (0.056) | 0.183 ** (0.056) |
| Education | 0.107 (0.059) | 0.100 (0.054) | 0.106 (0.069) | 0.104 (0.069) | 0.072 (0.067) | 0.072 (0.067) |
| Income | 0.038 (0.025) | 0.067 ** (0.023) | −0.001 (0.029) | 0.009 (0.029) | −0.013 (0.028) | −0.012 (0.028) |
| Bangkok | −0.089 * (0.045) | −0.101 * (0.041) | 0.076 (0.053) | 0.072 (0.052) | 0.105 * (0.051) | 0.104 * (0.051) |
| Worry | −0.016 (0.024) | 0.029 (0.022) | 0.176 *** (0.028) | 0.192 *** (0.029) | 0.182 *** (0.027) | 0.183 *** (0.028) |
| Predictors | ||||||
| Trust in the government | 0.373 *** (0.030) | 0.133 ** (0.038) | 0.015 (0.040) | |||
| Professional trust | 0.322 *** (0.040) | 0.316 *** (0.044) | ||||
| Constant | 3.678 *** (0.133) | 2.364 *** (0.161) | 2.836 *** (0.156) | 2.368 *** (0.205) | 1.651 *** (0.210) | 1.622 *** (0.224) |
| F value | 2.982 ** | 22.501 *** | 8.041 *** | 8.654 *** | 15.762 *** | 14.011 *** |
| R2 | 0.025 | 0.184 | 0.066 | 0.080 | 0.136 | 0.136 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saechang, O.; Yu, J.; Li, Y. Public Trust and Policy Compliance during the COVID-19 Pandemic: The Role of Professional Trust. Healthcare 2021, 9, 151. https://doi.org/10.3390/healthcare9020151
Saechang O, Yu J, Li Y. Public Trust and Policy Compliance during the COVID-19 Pandemic: The Role of Professional Trust. Healthcare. 2021; 9(2):151. https://doi.org/10.3390/healthcare9020151
Chicago/Turabian StyleSaechang, Orachorn, Jianxing Yu, and Yong Li. 2021. "Public Trust and Policy Compliance during the COVID-19 Pandemic: The Role of Professional Trust" Healthcare 9, no. 2: 151. https://doi.org/10.3390/healthcare9020151







