Assessing the Psychological Impact of COVID-19 among College Students: An Evidence of 15 Countries
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol Registration
2.2. Eligibility Criteria
2.3. Sources of Information
2.4. Search Strategy
2.5. Selection Process
2.6. Data Collection
2.7. Assessment of Risk of Bias in Primary Studies
2.8. Measures of Effect and Data Analysis
2.9. Assessment of Evidence
3. Results
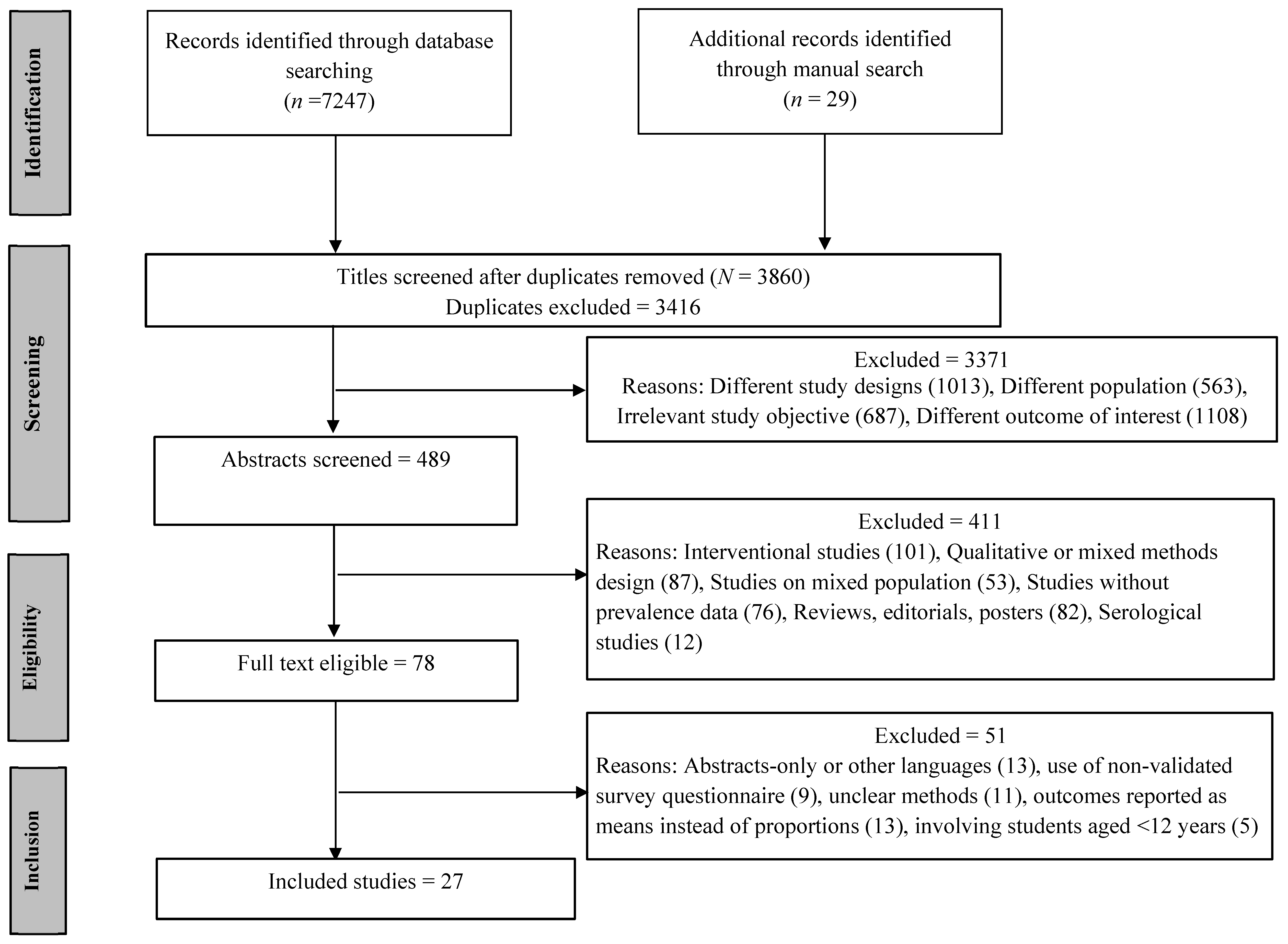
3.1. Selection of the Dtudies
3.2. Characteristics of Included Studies
3.3. Risk of Bias in the Included Studies
3.4. Meta-Analysis
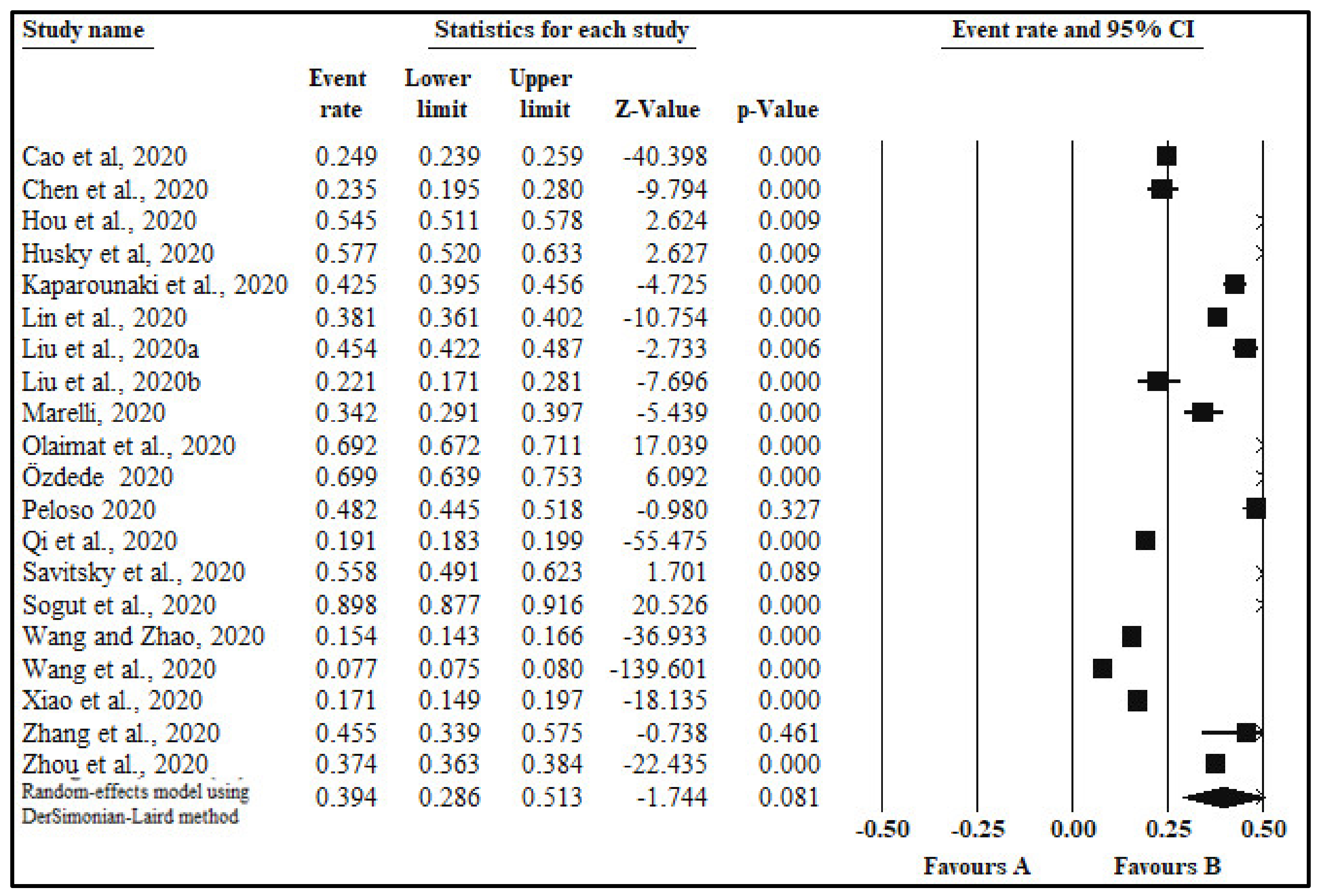
3.4.1. Anxiety
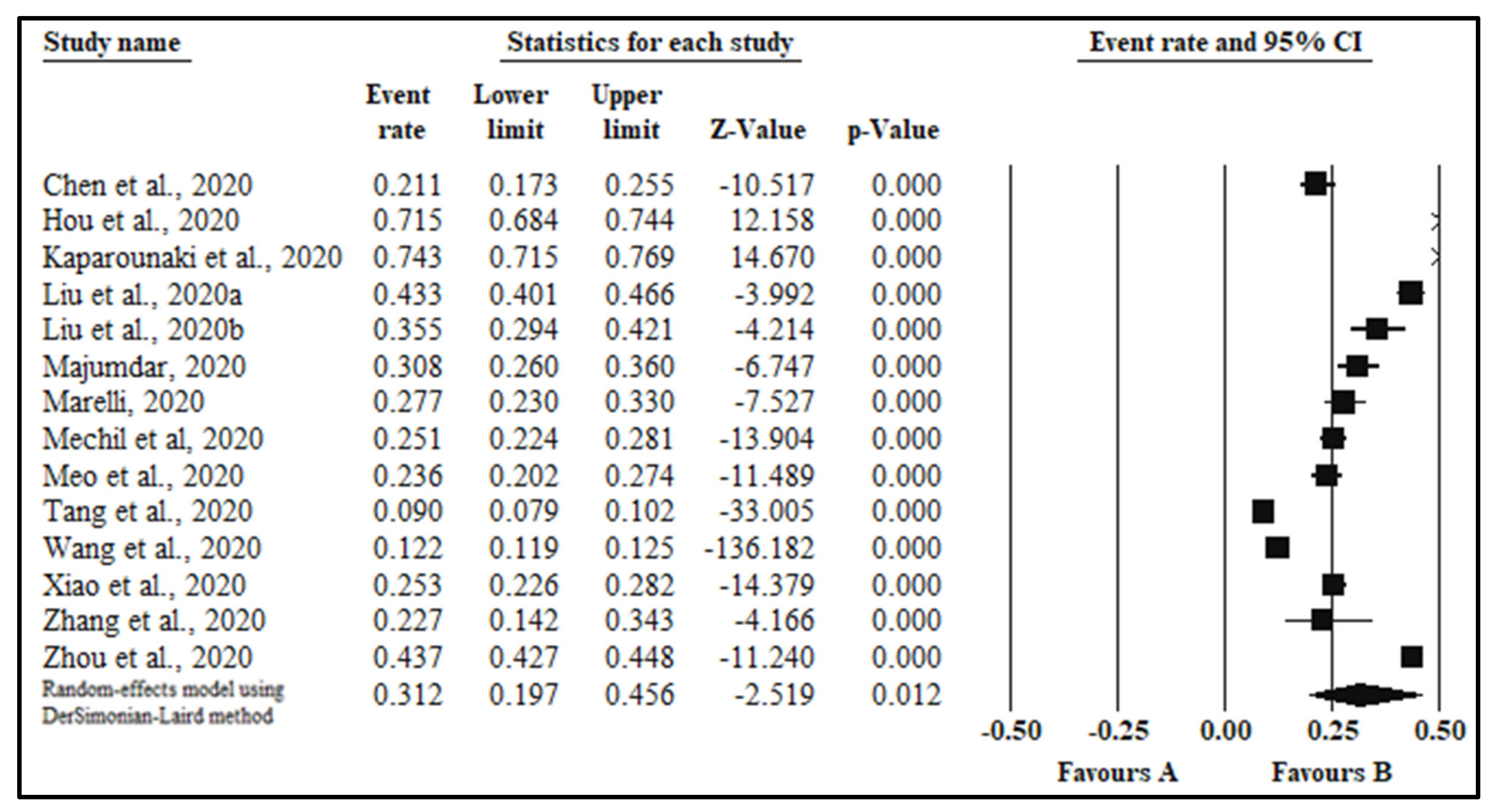
3.4.2. Depression
3.4.3. Other Psychological Outcomes
3.4.4. Publication Bias
3.4.5. Certainty of the Evidence
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Author/Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Final Quality Score | Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cao et al., 2020 [35] | Y | Y | Y | Y | NA | Y | N | N | Y | NA | Y | NA | NA | N | 7 | Good |
| Chen et al., 2020 [36] | Y | Y | N | N | NA | Y | N | N | Y | NA | Y | NA | NA | N | 5 | Fair |
| Gritsenko et al., 2020 [37] | Y | Y | N | N | NA | Y | N | N | Y | NA | Y | NA | NA | N | 5 | Fair |
| Hou et al., 2020 [38] | Y | Y | N | Y | NA | Y | Y | Y | Y | NA | N | NA | NA | N | 7 | Good |
| Husky et al., 2020 [39] | Y | Y | N | N | N | Y | N | N | Y | NA | Y | NA | NA | N | 5 | Fair |
| Kaparounaki et al., 2020 [40] | Y | Y | NR | N | NA | Y | N | N | Y | NA | NA | NA | NA | N | 4 | Fair |
| Li et al., 2020 [41] | Y | Y | Y | N | NA | Y | N | N | Y | NA | Y | NA | NA | N | 6 | Fair |
| Lin et al., 2020 [42] | Y | Y | NR | N | N | Y | Y | N | Y | NA | Y | NA | NA | N | 6 | Fair |
| Liu et al., 2020 [43] | Y | Y | Y | N | N | Y | N | N | Y | NA | Y | NA | NA | N | 6 | Fair |
| Liu et a., 2020 [44] | Y | Y | Y | Y | N | Y | N | N | Y | NA | Y | NA | NA | N | 7 | Good |
| Liu et al., 2020 [45] | Y | Y | NR | N | N | Y | N | Y | Y | NA | Y | NA | NA | N | 6 | Fair |
| Majumdar et al., 2020 [46] | Y | Y | N | N | N | Y | N | Y | NR | NA | Y | NA | NA | N | 5 | Fair |
| Author/Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Final quality score | Rating |
| Marelli et al., 2020 [47] | Y | Y | N | N | Y | Y | Y | N | Y | NA | Y | NA | NA | N | 7 | Good |
| Mechil et al., 2020 [48] | Y | Y | NR | N | Y | Y | Y | N | Y | NA | Y | NA | NA | N | 7 | Good |
| Meo et al., 2020 [49] | Y | Y | Y | N | N | Y | N | N | Y | NA | Y | NA | NA | N | 6 | Fair |
| Olaimat et al., 2020 [50] | Y | Y | Y | N | N | Y | N | N | Y | NA | Y | NA | NA | N | 6 | Fair |
| Ozdede et al., 2020 [51] | Y | Y | Y | N | N | Y | N | N | Y | NA | Y | NA | NA | N | 6 | Fair |
| Peloso et al., 2020 [52] | Y | Y | Y | N | N | Y | N | N | Y | NA | Y | NA | NA | N | 6 | Fair |
| Qi et al., 2020 [53] | Y | Y | N | N | N | Y | Y | N | Y | NA | Y | NA | NA | N | 6 | Fair |
| Savitsky et al., 2020 [54] | Y | Y | Y | N | N | Y | N | N | Y | NA | Y | NA | NA | N | 6 | Fair |
| Sogut et al., 2020 [55] | Y | Y | NR | N | N | Y | Y | N | Y | NA | Y | NA | NA | N | 6 | Fair |
| Tang et al., 2020 [25] | Y | Y | NR | Y | Y | Y | Y | N | Y | NA | Y | NA | NA | N | 8 | Good |
| Wang and Zhao et al., 2020 [56] | Y | Y | NR | N | Y | Y | Y | N | Y | NA | Y | NA | NA | N | 7 | Good |
| Wang et al., 2020 [19] | Y | Y | Y | N | N | Y | Y | Y | Y | NA | Y | NA | NA | N | 8 | Good |
| Xiao et al., 2020 [57] | Y | Y | NR | Y | N | Y | Y | N | Y | NA | N | NA | NA | N | 6 | Fair |
| Zhang et al., 2020 [58] | Y | Y | NR | N | Y | Y | Y | N | Y | NA | Y | NA | NA | N | 7 | Good |
| Zhou et al., 2020 [59] | Y | Y | Y | N | Y | Y | Y | N | Y | NA | Y | NA | NA | N | 8 | Good |
| Author/Year [Reference #] | Sample Size | Quality Score | Country | Male (%) | Survey Tool | Outcomes (%) | |
|---|---|---|---|---|---|---|---|
| (n) | |||||||
| Anxiety | Depression | ||||||
| Cao et al, 2020 [35] | 7143 | 7 | China | 30 | GAD7 | 24.9 | NA |
| −1776 | |||||||
| Chen et al., 2020 [36] | 383 | 5 | China | NA | DSRS-C | 23.5 | 21.2 |
| SCARED | −90 | −81 | |||||
| Gritsenko et al., 2020 [37] | 939 | 5 | Russia and Belarus | 19 | FCV-19S | NA | NA |
| Hou et al., 2020 [38] | 859 | 7 | China | 61 | PHQ9 | 54.5 | 71.5 |
| GAD7 | −468 | −614 | |||||
| IESR | |||||||
| Husky et al., 2020 [39] | 291 | 5 | France | 25 | World Mental Health International College Student Survey | 57.7 | NA |
| −168 | |||||||
| Kaparounaki et al., 2020 [40] | 1000 | 4 | Greece | 31 | STAI | 42.5 | 74.3 |
| CES-D | −425 | −743 | |||||
| RASS | |||||||
| Li et al., 2020 [41] | 1442 | 6 | China | NA | K6 | NA | NA |
| IESR | |||||||
| Lin et al., 2020 [42] | 2086 | 6 | China | NA | STAI | 38.1 | NA |
| −795 | |||||||
| Liu et al., 2020 [43] | 898 | 6 | USA | 14 | PHQ8 | 45.4 | 43.3 |
| GAD7 | −408 | −389 | |||||
| Liu et al., 2020 [44] | 217 | 7 | China | 41 | PHQ9 | 22.1 | 35.5 |
| GAD7 | −48 | −77 | |||||
| Liu et al., 2020 [45] | 198 | 6 | China | 34 | SSS | NA | NA |
| Author/Year | Sample Size | Country | Male (%) | Survey Tool | Outcomes (%) | Author/Year | |
| (n) | |||||||
| Anxiety | Depression | ||||||
| Majumdar et al., 2020 [46] | 325 | 5 | India | 39 | CES-D | NA | 30.77 |
| −100 | |||||||
| Marelli et al., 2020 [47] | 307 | 7 | Italy | 25 | BAI | 34.3 | 27.8 |
| BDI-II | −105 | −85 | |||||
| PSQI | |||||||
| ISI | |||||||
| Mechil et al, 2020 [48] | 863 | 7 | Albania | 11 | PHQ9 | NA | 25.2 |
| −217 | |||||||
| Meo et al., 2020 [49] | 530 | 6 | Saudi Arabia | 45 | Stress Allied Queries | NA | 23.6 |
| −125 | |||||||
| Olaimat et al., 2020 [50] | 2083 | 6 | Jordan | 25 | NA | 69.2 | NA |
| −1441 | |||||||
| Özdede et al., 2020 [51] | 249 | 6 | Turkey | 38 | STAI | 69.9 | NA |
| −174 | |||||||
| Peloso et al., 2020 [52] | 704 | 6 | Brazil (South America) | 20 | NA | 48.2 | NA |
| −339 | |||||||
| Qi et al., 2020 [53] | 9554 | 6 | China | NA | GAD7 | 19 | NA |
| −1814 | |||||||
| Savitsky et al., 2020 [54] | 215 | 6 | Israel | 12 | GAD7 | 55.9 | NA |
| −120 | |||||||
| Sogut et al., 2020 [55] | 972 | 6 | Turkey | 0 | BAI | −873 | NA |
| Tang et al., 2020 [25] | 2485 | 8 | China | 39 | PHQ9 | NA | 9 |
| −224 | |||||||
| Wang and Zhao, 2020 [56] | 3611 | 7 | China | 40 | SAS | −557 | NA |
| Author/Year | Sample Size | Country | Male (%) | Survey Tool | Outcomes (%) | Author/Year | |
| (n) | |||||||
| Anxiety | Depression | ||||||
| Wang et al., 2020 [19] | 44447 | 8 | China | 45 | SAS | 7.7 | 12.2 |
| CES-D | −3422 | −5422 | |||||
| Xiao et al., 2020 [57] | 933 | 6 | China | 30 | GAD7 | 17.1 | 25.3 |
| PHQ9 | −160 | −236 | |||||
| Zhang et al., 2020 [58] | 66 | 7 | China | 38 | DASS21 | −30 | −15 |
| PSQI | |||||||
| Zhou et al., 2020 [59] | 8079 | 8 | China | 46 | PHQ-9 | 37.4 | 43.7 |
| GAD-7 | −3020 | −3533 | |||||
References
- Liu, C.H.; Stevens, C.; Wong, S.H.M.; Yasui, M.; Chen, J.A. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: Implications for addressing disparities in service use. Depress. Anxiety 2019, 36, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Beiter, R.; Nash, R.; McCrady, M.; Rhoades, D.; Linscomb, M.; Clarahan, M.; Sammut, S. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J. Affect. Disord. 2015, 173, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Woodford, M.R.; Han, Y.; Craig, S.; Lim, C.; Matney, M.M. Discrimination and mental health among sexual minority college students: The type and form of discrimination does matter. J. Gay Lesbian Ment. Health 2014, 18, 142–163. [Google Scholar] [CrossRef]
- Stress: An Epidemic among College Students. The American Institute of Stress Website. 2019. Available online: https://www.stress.org/stress-an-epidemic-among-college-students (accessed on 12 January 2021).
- Mortier, P.; Auerbach, R.P.; Alonso, J.; Bantjes, J.; Benjet, C.; Cuijpers, P.; Ebert, D.D.; Green, J.G.; Hasking, P.; Nock, M.K.; et al. Suicidal thoughts and behaviors among First-Year college students: Results from the WMH-ICS Project. J. Am. Acad. Child Adolesc. Psychiatry 2018, 57, 263–273.e1. [Google Scholar] [CrossRef] [PubMed]
- Ebert, D.D.; Buntrock, C.; Mortier, P.; Auerbach, R.; Weisel, K.K.; Kessler, R.C.; Cuijpers, P.; Green, J.G.; Kiekens, G.; Nock, M.K.; et al. Prediction of major depressive disorder onset in college students. Depress. Anxiety 2019, 36, 294–304. [Google Scholar] [CrossRef]
- Bruffaerts, R.; Mortier, P.; Kiekens, G.; Auerbach, R.P.; Cuijpers, P.; Demyttenaere, K.; Green, J.G.; Nock, M.K.; Kessler, R.C. Mental health problems in college freshmen: Prevalence and academic functioning. J. Affect. Disord. 2018, 225, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, S.; Videla-Nash, G.; Foussias, G.; Segal, Z.V.; Zakzanis, K.K. On the nature of objective and perceived cognitive impairments in depressive symptoms and real-world functioning in young adults. Psychiatry Res. 2020, 287, 112932. [Google Scholar] [CrossRef] [PubMed]
- Kenney, S.R.; Lac, A.; Labrie, J.W.; Hummer, J.F.; Pham, A. Mental health, sleep quality, drinking motives, and alcohol-related consequences: A path-analytic model. J. Stud. Alcohol. Drugs. 2013, 74, 841–851. [Google Scholar] [CrossRef]
- Malla, A.; Shah, J.; Iyer, S.; Boksa, P.; Joober, R.; Andersson, N.; Lal, S.; Fuhrer, R. Youth mental health should be a top priority for health care in Canada. Can. J. Psychiatry 2018, 63, 216–222. [Google Scholar] [CrossRef]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 2010, 10, 113. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus disease (COVID-19) Pandemic. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 21 December 2020).
- Balhara, Y.P.S.; Kattula, D.; Singh, S.; Chukkali, S.; Bhargava, R. Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J. Public Health 2020, 64 (Supplement.), S172–S176. [Google Scholar] [CrossRef]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. 2020, 14, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Siddique, R.; Li, H.; Ali, A.; Shereen, M.A.; Bashir, N.; Xue, M. Impact of coronavirus outbreak on psychological health. J. Glob. Health 2020, 10, 010331. [Google Scholar] [CrossRef] [PubMed]
- Li, H.Y.; Cao, H.; Leung, D.Y.P.; Mak, Y.W. The Psychological impacts of a COVID-19 outbreak on college Students in China: A Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 3933. [Google Scholar] [CrossRef]
- Kaurani, P.; Batra, K.; Rathore-Hooja, H. Psychological impact of COVID-19 lockdown (Phase 2) among Indian general population: A cross-sectional analysis. Int. J. Sci. Res. 2020, 9, 51–56. [Google Scholar] [CrossRef]
- Zhai, Y.; Du, X. Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Res. 2020, 288, 113003. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.H.; Yang, H.L.; Yang, Y.Q.; Liu, D.; Li, Z.-H.; Zhang, X.-R.; Zhang, Y.-J.; Shen, D.; Chen, P.-L.; Song, W.-Q.; et al. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study [published correction appears in J Affect Disord. J Affect Disord. 2020, 275, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Son, C.; Hegde, S.; Smith, A.; Wang, X.; Sasangohar, F. Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. J. Med. Internet Res. 2020, 22, e21279. [Google Scholar] [CrossRef]
- Orben, A.; Tomova, L.; Blakemore, S.J. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc. Health. 2020, 4, 634–640. [Google Scholar] [CrossRef]
- Aylie, N.S.; Mekonen, M.A.; Mekuria, R.M. The psychological impacts of COVID-19 pandemic among College students in Bench-Sheko Zone, South-west Ethiopia: A community-based cross-sectional study. Psychol. Res. Behav. Manag. 2020, 13, 813–821. [Google Scholar] [CrossRef]
- Sundarasen, S.; Chinna, K.; Kamaludin, K.; Nurunnabi, M.; Baloch, G.M.; Khoshaim, H.B.; Hossain, S.F.A.; Sukayt, A. Psychological impact of COVID-19 and lockdown among College students in Malaysia: Implications and policy recommendations. Int. J. Environ. Res. Public Health 2020, 17, 6206. [Google Scholar] [CrossRef] [PubMed]
- Wathelet, M.; Duhem, S.; Vaiva, G.; Baubet, T.; Habran, E.; Veerapa, E.; Debien, C.; Molenda, S.; Horn, M.; Grandgenèvre, P.; et al. Factors associated with mental health disorders among College students in France confined during the COVID-19 pandemic. JAMA Netw. Open. 2020, 3, e2025591. [Google Scholar] [CrossRef]
- Tang, W.; Hu, T.; Hu, B.; Jin, C.; Wang, G.; Xie, C.; Chen, S.; Xu, J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese College students. J. Affect. Disord. 2020, 274, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Silva Junior, F.J.G.D.; Sales, J.C.E.S.; Monteiro, C.F.S.; Costa, A.P.C.; Campos, L.R.B.; Miranda, P.I.G.; Monteiro, T.A.D.S.; Lima, R.A.G.; Lopes-Junior, L.C. Impact of COVID-19 pandemic on mental health of young people and adults: A systematic review protocol of observational studies. BMJ Open 2020, 10, e039426. [Google Scholar] [CrossRef]
- Batra, K.; Singh, T.P.; Sharma, M.; Batra, R.; Schvaneveldt, N. Investigating the Psychological impact of COVID-19 among healthcare workers: A Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 9096. [Google Scholar] [CrossRef]
- Lakhan, R.; Agrawal, A.; Sharma, M. Prevalence of depression, anxiety, and stress during COVID-19 pandemic. J. Neurosci. Rural Pract. 2020, 11, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public-A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Chen, F.; Zheng, D.; Liu, J.; Gong, Y.; Guan, Z.; Lou, D. Depression and anxiety among adolescents during COVID-19: A cross-sectional study. Brain Behav. Immun. 2020, 88, 36–38. [Google Scholar] [CrossRef] [PubMed]
- Gritsenko, V.; Skugarevsky, O.; Konstantinov, V.; Khamenka, N.; Marinova, T.; Reznik, A.; Isralowitz, R. COVID 19 Fear, Stress, Anxiety, and Substance Use Among Russian and Belarusian College Students [published online ahead of print, 2020 May 21]. Int. J. Ment. Health Addict. 2020, 1–7. [Google Scholar] [CrossRef]
- Hou, T.Y.; Mao, X.F.; Dong, W.; Cai, W.P.; Deng, G.H. Prevalence of and factors associated with mental health problems and suicidality among senior high school students in rural China during the COVID-19 outbreak. Asian J. Psychiatr. 2020, 54, 102305. [Google Scholar] [CrossRef]
- Husky, M.M.; Kovess-Masfety, V.; Swendsen, J.D. Stress and anxiety among College students in France during COVID-19 mandatory confinement. Compr. Psychiatry 2020, 102, 152191. [Google Scholar] [CrossRef]
- Kaparounaki, C.K.; Patsali, M.E.; Mousa, D.V.; Papadopoulou, E.V.K.; Papadopoulou, K.K.K.; Fountoulakis, K.N. College students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020, 290, 113111. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, Y.; Jiang, J.; Valdimarsdóttir, U.A.; Fall, K.; Fang, F.; Song, H.; Lu, D.; Zhang, W. Psychological distress among health professional students during the COVID-19 outbreak. Psychol. Med. 2020, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Hu, Z.; Alias, H.; Wong, L.P. Influence of mass and social media on psychobehavioral responses among medical students during the downward trend of COVID-19 in Fujian, China: Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e19982. [Google Scholar] [CrossRef]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S.; Hahm, H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef]
- Liu, J.; Zhu, Q.; Fan, W.; Makamure, J.; Zheng, C.; Wang, J. Online mental health survey in a medical college in China during the COVID-19 outbreak. Front. Psychiatry 2020, 11, 459. [Google Scholar] [CrossRef]
- Liu, S.; Liu, Y.; Liu, Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: A cross-sectional survey. Psychiatry Res. 2020, 289, 113070. [Google Scholar] [CrossRef]
- Majumdar, P.; Biswas, A.; Sahu, S. COVID-19 pandemic and lockdown: Cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol Int. 2020, 37, 1191–1200. [Google Scholar] [CrossRef]
- Marelli, S.; Castelnuovo, A.; Somma, A.; Castronovo, V.; Mombelli, S.; Bottoni, D.; Leitner, C.; Fossati, A.; Ferini-Strambi, L. Impact of COVID-19 lockdown on sleep quality in College students and administration staff. J. Neurol. 2020, 268, 8–15. [Google Scholar] [CrossRef]
- Mechili, E.A.; Saliaj, A.; Kamberi, F.; Girvalaki, C.; Peto, E.; Patelarou, A.E.; Bucaj, J.; Patelarou, E. Is the mental health of young students and their family members affected during the quarantine period? Evidence from the COVID-19 pandemic in Albania. J. Psychiatr. Ment. Health Nurs. 2020. [Google Scholar] [CrossRef]
- Meo, S.A.; Abukhalaf, A.A.; Alomar, A.A.; Sattar, K.; Klonoff, D.C. COVID-19 pandemic: Impact of quarantine on medical students’ mental well-being and learning behaviors. Pak. J. Med. Sci. 2020, 36, S43–S48. [Google Scholar] [CrossRef]
- Olaimat, A.N.; Aolymat, I.; Elsahoryi, N.; Shahbaz, H.M.; Holley, R.A. Attitudes, anxiety, and behavioral practices regarding COVID-19 among College students in Jordan: A cross-sectional study. Am. J. Trop. Med. Hyg. 2020, 103, 1177–1183. [Google Scholar] [CrossRef]
- Özdede, M.; Sahin, S.C. Views and anxiety levels of Turkish dental students during the COVID-19 pandemic. J. Stomatol. 2020, 73, 123–128. [Google Scholar] [CrossRef]
- Peloso, R.M.; Ferruzzi, F.; Mori, A.A.; Camacho, D.P.; Franzin, L.C.D.S.; Teston, A.P.M.; Freitas, K.M.S. Notes from the field: Concerns of health-related higher education students in Brazil pertaining to distance learning during the Coronavirus pandemic. Eval. Health Prof. 2020, 43, 201–203. [Google Scholar] [CrossRef] [PubMed]
- Qi, H.; Liu, R.; Chen, X.; Yuan, X.; Li, Y.; Huang, H.; Zheng, Y.; Wang, G. Prevalence of anxiety and associated factors for Chinese adolescents during the COVID-19 outbreak. Psychiatry Clin. Neurosci. 2020, 74, 555–557. [Google Scholar] [CrossRef] [PubMed]
- Savitsky, B.; Findling, Y.; Ereli, A.; Hendel, T. Anxiety and coping strategies among nursing students during the covid-19 pandemic. Nurse Educ. Pract. 2020, 46, 102809. [Google Scholar] [CrossRef] [PubMed]
- Sögüt, S.; Dolu, İ.; Cangöl, E. The relationship between COVID-19 knowledge levels and anxiety states of midwifery students during the outbreak: A cross-sectional web-based survey. Perspect. Psychiatr. Care 2021, 57, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhao, H. The impact of COVID-19 on anxiety in Chinese College students. Front. Psychol. 2020, 11, 1–8. [Google Scholar] [CrossRef]
- Xiao, H.; Shu, W.; Li, M.; Li, Z.; Tao, F.; Wu, X.; Yu, Y.; Meng, H.; Vermund, S.H.; Hu, Y. Social Distancing among medical students during the 2019 Coronavirus disease pandemic in China: Disease awareness, anxiety disorder, depression, and behavioral activities. Int. J. Environ. Res. Public Health 2020, 17, 5047. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, H.; Ma, X.; Di, Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: A longitudinal study of college students in China. Int. J. Environ. Res. Public Health 2020, 17, 3722. [Google Scholar] [CrossRef]
- Zhou, S.J.; Zhang, L.G.; Wang, L.L.; Guo, Z.-C.; Wang, J.-Q.; Chen, J.-C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- American Council on Education. Mental Health, Strategies for Leaders to Support Campus Well-Being. 2019. Available online: https://www.acenet.edu/Documents/Mental-Health-Higher-Education-Covid-19.pdf (accessed on 1 January 2021).
- College Students’ Mental Health Is a Growing Concern, Survey Finds. Monitor on Psychology. American Psychological Association Website. 2013. Available online: http://www.apa.org/monitor/2013/06/college-students (accessed on 1 January 2021).
- World Health Organization. Adolescent Mental Health. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (accessed on 25 January 2020).
- Ozdin, S.; Ozdin, S.B. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar] [CrossRef]
- Wenjun, G.; Siqing, P.; Xinqiao, L. Gender differences in depression, anxiety, and stress among college students: A longitudinal study from China. J. Affect. Disord. 2020, 263, 292–300. [Google Scholar] [CrossRef]
- Chaplin, T.M.; Hong, K.; Bergquist, K.; Sinha, R. Gender differences in response to emotional stress: An assessment across subjective, behavioral, and physiological domains and relations to alcohol craving. Alcohol. Clin. Exp. Res. 2008, 32, 1242–1250. [Google Scholar] [CrossRef]
- Baldry, A.C.; Farrington, D. Protective Factors as Moderators of Risk Factors in Adolescence Bullying. Soc. Psychol. Educ. 2005, 8, 263–284. [Google Scholar] [CrossRef]
- Rasmussen, M.L.; Hjelmeland, H.; Dieserud, G. Barriers toward help-seeking among young men prior to suicide. Death Stud. 2018, 42, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Cianconi, P.; Lesmana, C.B.J.; Ventriglio, A.; Janiri, L. Mental health issues among indigenous communities and the role of traditional medicine. Int. J. Soc. Psychiatry 2019, 65, 289–299. [Google Scholar] [CrossRef] [PubMed]
| Overall | Number of Studies | Proportion (%) | 95% CI | I2 | p-Value | References | |
|---|---|---|---|---|---|---|---|
| Anxiety prevalence | 20 | 34.4% | 29.5,39.7 | 99.1% | <0.0001 | [19,35,36,38,39,40,42,43,44,47,50,51,52,53,54,55,56,57,58,59] | |
| Subgroup Analysis | |||||||
| Categories | Subgroups | Number of Studies | Proportion (%) | 95% CI | I2 | p-Value | References |
| Quality | Good | 9 | 29.3 | 16.8,45.8 | 99.8% | <0.0001 | [19,35,38,43,44,47,56,58,59] |
| Medium | 11 | 48.4 | 33.0,64.1 | 99.6% | <0.0001 | [36,39,40,42,50,51,52,53,54,55,57] | |
| Continents | Asia | 13 | 30.4 | 20.0,43.4 | 99.8% | <0.0001 | [19,35,36,38,42,44,50,53,54,56,57,58,59] |
| Other | 7 | 57.5 | 38.6,74.4 | 98.8% | <0.0001 | [39,40,43,47,51,52,55]. | |
| Countries | China | 11 | 25.5 | 16.7,36.9 | 99.8% | <0.0001 | [19,35,36,38,42,44,53,56,57,58,59] |
| Other | 9 | 58.7 | 44.0,72.0 | 98.7% | <0.0001 | [39,40,43,47,50,51,52,54,55] | |
| Assessment | GAD | 8 | 33.0 | 18.1,52.3 | 99.4% | <0.0001 | [35,38,43,44,53,54,57,59] |
| Other | 12 | 43.9 | 28.9,60.1 | 99.8% | <0.0001 | [19,36,39,40,42,47,50,51,52,55,56,58] | |
| Gender | Female | 5 | 34.6 | 20.5,52.0 | 99.0% | <0.0001 | [54,56,57,58,59] |
| Male | 5 | 22.9 | 36.3,52.5 | 98.3% | <0.0001 | [54,56,57,58,59] | |
| Level of Anxiety | Mild | 7 | 73.7 | 63.8,81.7 | 96.9 | <0.0001 | [44,53,54,55,56,57,59] |
| Moderate | 7 | 23.1 | 16.2,31.8 | 97.7 | <0.0001 | [44,53,54,55,56,57,59] | |
| Severe | 7 | 7.0 | 4.8,11.3 | 92.3 | <0.0001 | [44,53,54,55,56,57,59] | |
| Overall | Number of Studies | Proportion (%) | 95% CI | I2 | p-Value | References | |
|---|---|---|---|---|---|---|---|
| Depression prevalence | 14 | 31.2 | 19.7,45.6 | 99.8% | <0.0001 | [19,25,36,38,40,43,44,46,47,48,49,57,58,59] | |
| Subgroup Analysis | |||||||
| Categories | Subgroups | Number of Studies | Proportion (%) | 95% CI | I2 | p-Value | References |
| Quality | Good | 9 | 29.7 | 16.4,47.7 | 99.8% | <0.0001 | [19,25,38,43,44,47,48,58,59] |
| Medium | 5 | 34.0 | 15.6,59.0 | 99.3% | <0.0001 | [36,40,46,49,57] | |
| Continents | Asia | 10 | 27.3 | 15.6,43.2 | 99.8% | <0.0001 | [19,35,36,38,42,44,50,53,54,56,57,58,59] |
| Other | 4 | 42.2 | 19.3,69.1 | 99.3% | <0.0001 | [40,43,47,48] | |
| Countries | China | 8 | 27.3 | 14.4,45.6 | 99.8% | <0.0001 | [19,25,36,38,44,57,58,59] |
| Other | 6 | 36.8 | 18.8,59.5 | 99.1% | <0.0001 | [40,43,46,47,48,49] | |
| Assessment | PHQ | 7 | 33.9 | 18.3,53.9 | 99.5% | <0.0001 | [25,38,43,44,48,57,59] |
| Other | 7 | 28.7 | 14.9,48.0 | 99.6% | <0.0001 | [19,36,40,46,47,49,58] | |
| Gender | Female | 5 | 32.4 | 20.0,44.8 | 96.4% | <0.0001 | [44,49,57,58,59] |
| Male | 5 | 26.0 | 16.9,37.8 | 95.5% | <0.0001 | [44,49,57,58,59] | |
| Level of Anxiety | Mild | 4 | 55.6 | 35.8,73.7 | 90.5% | <0.0001 | [44,48,57,59] |
| Moderate | 4 | 30.4 | 17.5,47.5 | 97.4% | <0.0001 | [44,48,57,59] | |
| Severe | 4 | 16.1 | 8.2,29.3 | 96.9% | <0.0001 | [44,48,57,59] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Batra, K.; Sharma, M.; Batra, R.; Singh, T.P.; Schvaneveldt, N. Assessing the Psychological Impact of COVID-19 among College Students: An Evidence of 15 Countries. Healthcare 2021, 9, 222. https://doi.org/10.3390/healthcare9020222
Batra K, Sharma M, Batra R, Singh TP, Schvaneveldt N. Assessing the Psychological Impact of COVID-19 among College Students: An Evidence of 15 Countries. Healthcare. 2021; 9(2):222. https://doi.org/10.3390/healthcare9020222
Chicago/Turabian StyleBatra, Kavita, Manoj Sharma, Ravi Batra, Tejinder Pal Singh, and Nena Schvaneveldt. 2021. "Assessing the Psychological Impact of COVID-19 among College Students: An Evidence of 15 Countries" Healthcare 9, no. 2: 222. https://doi.org/10.3390/healthcare9020222
APA StyleBatra, K., Sharma, M., Batra, R., Singh, T. P., & Schvaneveldt, N. (2021). Assessing the Psychological Impact of COVID-19 among College Students: An Evidence of 15 Countries. Healthcare, 9(2), 222. https://doi.org/10.3390/healthcare9020222









