Effects of a Lifestyle Intervention on Health-Promoting Behavior, Psychological Distress and Reproductive Health of Overweight and Obese Female College Students
Abstract
1. Introduction
2. Materials and Methods
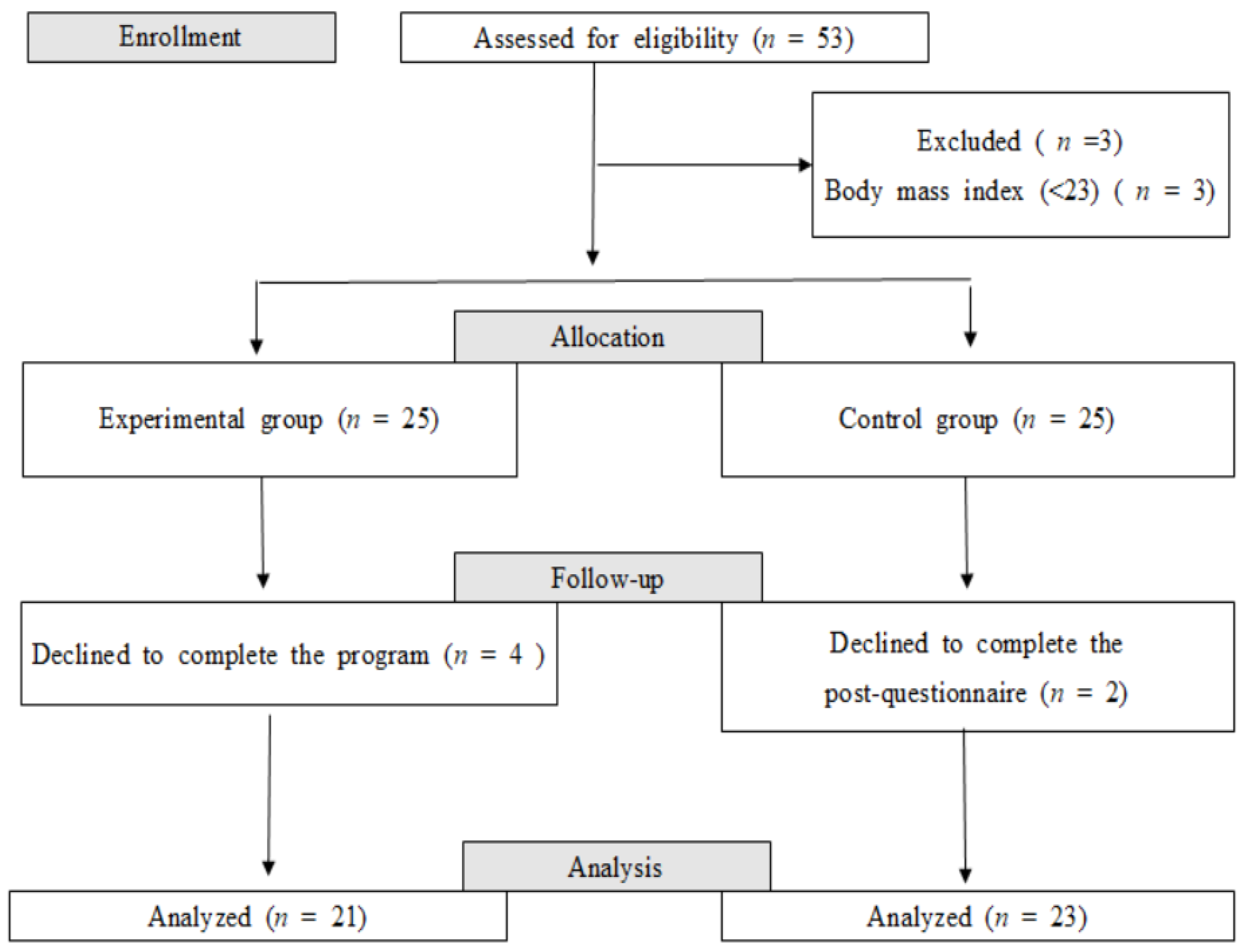
2.1. Design
2.2. Participants
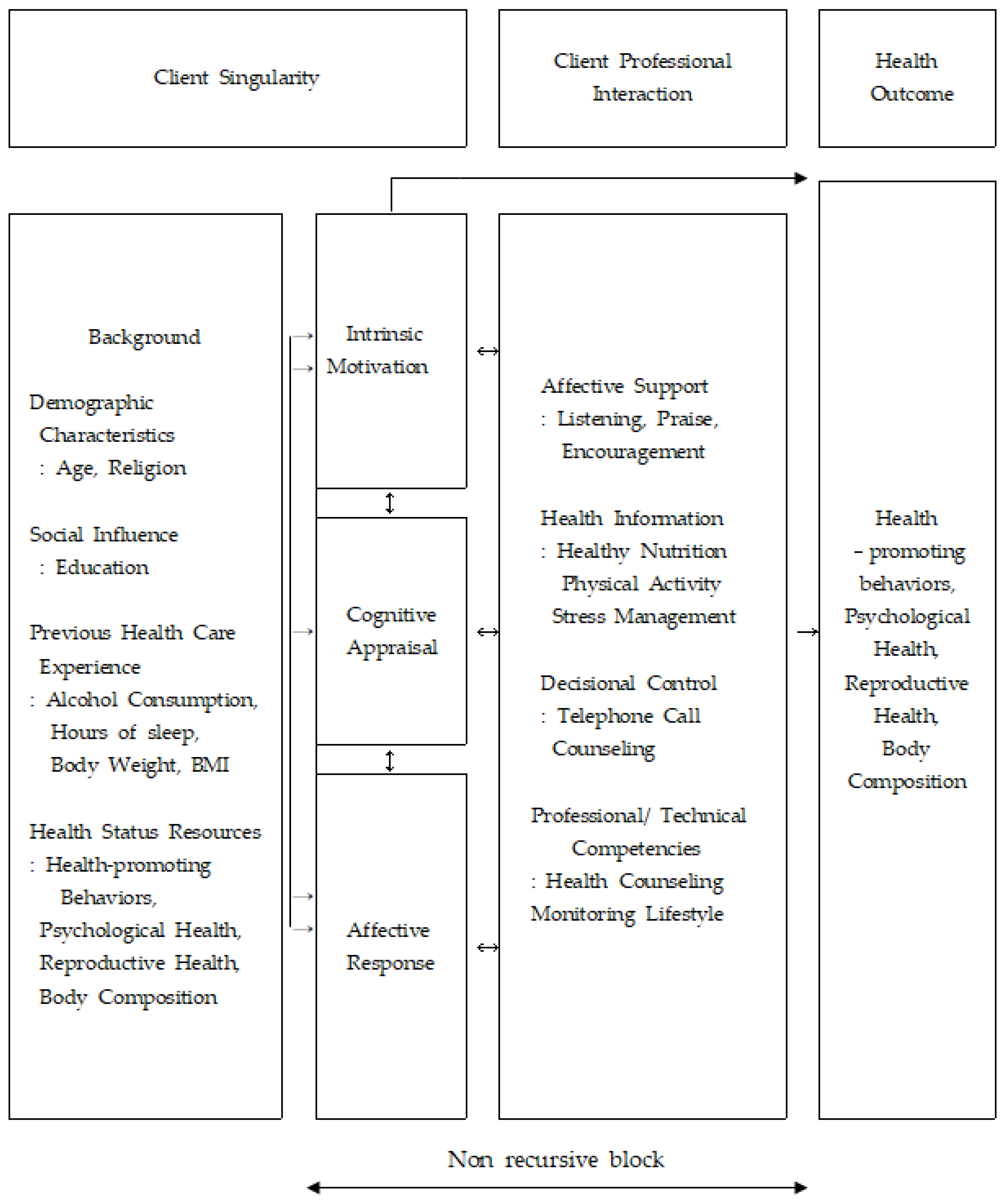
2.3. Conceptual Framework
2.4. Lifestyle Intervention based on the Interaction Model of Client Health Behavior
2.5. Outcome Measures
2.5.1. Health-Promoting Lifestyle Profile II (HPLP II)
2.5.2. Depression, Anxiety, and Stress Scale-21 (DASS-21)
2.5.3. Reproductive Health
2.5.4. Body Composition
2.6. Ethical Considerations and Statistical Analysis
3. Results
3.1. Homogeneity Test for General Characteristics and Variables between Groups
3.2. Effects of the Lifestyle Intervention Based on the Interaction Model of Client Health Behavior
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity among Adults and Youth: United States, 2015–2016. In NCHS Data Brief; No 288; National Center for Health Statistics: Hyattsville, MD, USA, 2017. [Google Scholar]
- Korean Statistical Information Service. Obesity Prevalence Trend. Available online: http://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_11702_N101&vw_cd=MT_ZTITLE&list_id=117_11702_B01&seqNo=&lang_mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=MT_ZTITLE (accessed on 5 March 2020).
- Egger, G.; Binns, A.; Rössner, S.; Sagner, M. Lifestyle Medicine: Lifestyle, the Environment, and Preventive Medicine in Health and Disease, 3nd ed.; Elsevier: London, UK, 2017. [Google Scholar]
- Zhang, Y.-X.; Wang, S.-R.; Zhao, J.-S.; Chu, Z.-H. Prevalence of overweight and central obesity and their relationship with blood pressure among college students in Shandong, China. Blood Press. Monit. 2016, 21, 251–254. [Google Scholar] [CrossRef]
- Desai, M.N.; Miller, W.C.; Staples, B.; Bravender, T. Risk Factors Associated with Overweight and Obesity in College Students. J. Am. Coll. Health 2008, 57, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Odlaug, B.L.; Lust, K.; Wimmelmann, C.L.; Chamberlain, S.R.; Mortensen, E.L.; Derbyshire, K.; Christenson, G.; Grant, J.E. Prevalence and correlates of being overweight or obese in college. Psychiatry Res. 2015, 227, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Chu, S.Y.; Kim, S.Y.; Lau, J.; Schmid, C.H.; Dietz, P.M.; Callaghan, W.M.; Curtis, K.M. Maternal obesity and risk of stillbirth: A metaanalysis. Am. J. Obstet. Gynecol. 2007, 197, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Maheshwari, A.; Stofberg, L.; Bhattacharya, S. Effect of overweight and obesity on assisted reproductive technology—A systematic review. Hum. Reprod. Updat. 2007, 13, 433–444. [Google Scholar] [CrossRef]
- Greaney, M.L.; Less, F.D.; White, A.A.; Dayton, S.F.; Riebe, D.; Blissmer, B.; Shoff, S.; Walsh, J.R.; Greene, G.W. College Students’ Barriers and Enablers for Healthful Weight Management: A Qualitative Study. J. Nutr. Educ. Behav. 2009, 41, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Jakubiec, D.; Kornafel, D.; Cygan, A.; Górska-Kłęk, L.; Chromik, K. Lifestyle of students from different universities in Wroclaw, Poland. Roczniki Państwowego Zakładu Higieny 2015, 66, 337–344. [Google Scholar] [PubMed]
- Yahia, N.; Wang, D.; Rapley, M.; Dey, R. Assessment of weight status, dietary habits and beliefs, physical activity, and nutritional knowledge among university students. Perspect. Public Health 2016, 136, 231–244. [Google Scholar] [CrossRef]
- Ahn, S.-H.; Um, Y.-J.; Kim, Y.-J.; Kim, H.-J.; Oh, S.-W.; Lee, C.M.; Kwon, H.; Joh, H.-K. Association between Physical Activity Levels and Physical Symptoms or Illness among University Students in Korea. Korean J. Fam. Med. 2016, 37, 279–286. [Google Scholar] [CrossRef]
- Nho, J.-H.; Kim, H.S. Gender Differences and Relationships among Lifestyle and Reproductive Health in University Students. Korean J. Women Health Nurs. 2019, 25, 446–458. [Google Scholar] [CrossRef]
- Nho, J.-H.; Yoo, S.-H. Relationships among Lifestyle, Depression, Anxiety, and Reproductive Health in Female University Students. Korean J. Women Health Nurs. 2018, 24, 80–89. [Google Scholar] [CrossRef]
- Bavil, D.A.; Dolatian, M.; Mahmoodi, Z.; Baghban, A.A. Comparison of lifestyles of young women with and without primary dysmenorrhea. Electron. Physician 2016, 8, 2107–2114. [Google Scholar] [CrossRef]
- Sabharwal, A.M. Effectiveness of Lifestyle Interventions among College Students: An Overview. J. Nutr. Food Sci. 2014, 5, 1000363. [Google Scholar] [CrossRef]
- Dour, C.A.; Horacek, T.M.; Schembre, S.M.; Lohse, B.; Hoerr, S.; Kattelmann, K.; White, A.A.; Shoff, S.; Phillips, B.; Greene, G. Process Evaluation of Project WebHealth: A Nondieting Web-based Intervention for Obesity Prevention in College Students. J. Nutr. Educ. Behav. 2013, 45, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Shahril, M.R.; Dali, W.P.E.W.; Lua, P.L. A 10-Week Multimodal Nutrition Education Intervention Improves Dietary Intake among University Students: Cluster Randomised Controlled Trial. J. Nutr. Metab. 2013, 2013, 658642. [Google Scholar] [CrossRef]
- Baillot, A.; Romain, A.J.; Boisvert-Vigneault, K.; Audet, M.; Baillargeon, J.P.; Dionne, I.J.; Valiquette, L.; Chakra, C.N.A.; Avignon, A.; Langlois, M.-F. Effects of Lifestyle Interventions That Include a Physical Activity Component in Class II and III Obese Individuals: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0119017. [Google Scholar] [CrossRef]
- Cox, C.L. An interaction model of client health behavior: Theoretical prescription for nursing. Adv. Nurs. Sci. 1982, 5, 41–56. [Google Scholar] [CrossRef]
- Van Dammen, L.; Wekker, V.; De Rooij, S.R.; Groen, H.; Hoek, A.; Roseboom, T.J. A systematic review and meta-analysis of lifestyle interventions in women of reproductive age with overweight or obesity: The effects on symptoms of depression and anxiety. Obes. Rev. 2018, 19, 1679–1687. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.N.; Sechrist, K.R.; Pender, N.J. The Health-Promoting Lifestyle Profile: Development and psychometric characteristics. Nurs. Res. 1987, 36, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Noh, J.-W.; Yun, H.-Y.; Park, H.; Yu, S.-E. A Study of Predictive Factors Affecting Health: Promoting Behaviors of North Korean Adolescent Refugees. J. Prev. Med. Public Health 2015, 48, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Cha, E.S. Cha Korean Translation of the DASS21. Available online: http://www2.psy.unsw.edu.au/Groups/Dass/Korean/Korean%20Cha.htm (accessed on 13 January 2017).
- Park, M.N.; Choi, S.Y. Development of Reproductive Health Program and Identification of Effect for Married Women Immigrants. J. Korean Acad. Nurs. 2014, 44, 248–258. [Google Scholar] [CrossRef]
- Jo, H.Y.; Kim, Y.H.; Son, H.M. Development of a Scale to Measure Reproductive Health Promoting Behavior of Undergraduates. Korean J. Health Educ. Promot. 2014, 31, 29–43. [Google Scholar] [CrossRef][Green Version]
- World Health Organization. Sexual and Reproductive Health. Available online: https://www.who.int/reproductivehealth/en/ (accessed on 11 February 2017).
- Blank, S.; McCartney, C.; Marshall, J. The origins and sequelae of abnormal neuroendocrine function in polycystic ovary syndrome. Hum. Reprod. Updat. 2006, 12, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Ling, C.H.; de Craen, A.J.; Slagboom, P.E.; Gunn, D.A.; Stokkel, M.P.; Westendorp, R.G.; Maier, A.B. Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin. Nutr. (Edinb. Scotl.) 2011, 30, 610–615. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.K.; Lee, W.-Y.; Kang, J.-H.; Kang, J.-H.; Kim, B.T.; Kim, S.M.; Kim, E.M.; Suh, S.-H.; Shin, H.J.; Lee, K.R.; et al. 2014 Clinical Practice Guidelines for Overweight and Obesity in Korea. Endocrinol. Metab. 2014, 29, 405–409. [Google Scholar] [CrossRef]
- Díez, S.M.U.; Fortis, A.P.; Franco, S.F. Efficacy of a Health-Promotion Intervention for College Students: A Randomized Controlled Trial. Nurs. Res. 2012, 61, 121–132. [Google Scholar] [CrossRef]
- Korea Centers for Disease Control and Prevention. 2018 Korea Health Statistics Korea. Available online: https://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7 (accessed on 14 February 2020).
- Luppino, F.S.; De Wit, L.M.; Bouvy, P.F.; Stijnen, T.; Cuijpers, P.; Penninx, B.W.J.H.; Zitman, F.G. Overweight, Obesity, and Depression: A Systematic Review and Meta-Analysis of Longitudinal Studies. Arch. Gen. Psychiatry 2010, 67, 220–229. [Google Scholar] [CrossRef]
- De Wit, L.M.; Fokkema, M.; Van Straten, A.; Lamers, F.; Cuijpers, P.; Penninx, B.W.J.H. Depressive and anxiety disorders and the association with obesity, physical, and social activities. Depress. Anxiety 2010, 27, 1057–1065. [Google Scholar] [CrossRef]
- Booth, A.O.; Wang, X.; Turner, A.I.; Nowson, C.A.; Torres, S.J. Diet-Induced Weight Loss Has No Effect on Psychological Stress in Overweight and Obese Adults: A Meta-Analysis of Randomized Controlled Trials. Nutrients 2018, 10, 613. [Google Scholar] [CrossRef] [PubMed]
- Imayama, I.; Alfano, C.M.; Kong, A.; E Foster-Schubert, K.; E Bain, C.; Xiao, L.; Duggan, C.; Wang, C.-Y.; Campbell, K.L.; Blackburn, G.L.; et al. Dietary weight loss and exercise interventions effects on quality of life in overweight/obese postmenopausal women: A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 118. [Google Scholar] [CrossRef] [PubMed]
- Nho, J.-H.; Hwang, E.S. Effects of Multidisciplinary Lifestyle Modification Program on Health-promoting Behavior, Psychological Distress, Body Composition and Reproductive Symptoms among Overweight and Obese Middle-aged Women. Korean J. Adult Nurs. 2019, 31, 663–676. [Google Scholar] [CrossRef]
- DeUgarte, C.M.; A Bartolucci, A.; Azziz, R. Prevalence of insulin resistance in the polycystic ovary syndrome using the homeostasis model assessment. Fertil. Steril. 2005, 83, 1454–1460. [Google Scholar] [CrossRef] [PubMed]
- Malini, N.; George, K.R. Evaluation of different ranges of LH:FSH ratios in polycystic ovarian syndrome (PCOS)—Clinical based case control study. Gen. Comp. Endocrinol. 2018, 260, 51–57. [Google Scholar] [CrossRef] [PubMed]
| Session | Contents | Interaction | Method | Minutes |
|---|---|---|---|---|
| 1 | Introduction the program contents and schedule | Individual | ||
| Health information: the importance of a healthy lifestyle for physical, psychological and reproductive health Provision of an educational booklet including a diary for food and daily activity | Face-to-face | 60 | ||
| Affective support: encouragement and reinforcement for participating in the program | ||||
| 2 | Health information: nutrition for weight control (low-calorie diet, healthy diet) Lifestyle monitoring Affective support: encouragement and reinforcement of healthy lifestyle | IndividualGroup | Face-to-face | 60 |
| 3 | Individual health counseling: lifestyle patterns and body composition Lifestyle monitoring Affective support: encouragement and reinforcement of healthy lifestyle | Individual | Face-to-face | 60 |
| 4 | Health information: the importance of physical activity Physical activity: flexibility training, resistance training, neurovascular training Lifestyle monitoring | IndividualGroup | Face-to-face | 60 |
| Affective support: encouragement and reinforcement of healthy lifestyle | ||||
| 5 | Individual health counseling: physical activity Lifestyle monitoring Affective support: encouragement and reinforcement of healthy lifestyle | Individual | Face-to-face | 60 |
| 6 | Health information: stress management (knowing oneself) Lifestyle monitoring Affective support: encouragement and reinforcement of healthy lifestyle | IndividualGroup | Face-to-face | 60 |
| 7 | Individual health counseling: stress-related overweight or obesity Lifestyle monitoring Affective support: encouragement and reinforcement of healthy lifestyle | Individual | Face-to-face | 60 |
| 8 | Health information: nutrition for weight control (diet behaviors and recipes) Lifestyle monitoring Affective support: encouragement and reinforcement of healthy lifestyle | IndividualGroup | Face-to-face | 60 |
| 9 | Individual health counseling: overall health Lifestyle monitoring Affective support: encouragement and reinforcement of healthy lifestyle | Individual | Face-to-face | 60 |
| 10 | Health information: various methods of physical exercise Physical activity: flexibility training, resistance training, neurovascular training Affective support: encouragement and reinforcement of healthy lifestyle | IndividualGroup | Face-to-face | 60 |
| 11 | Health information: stress management (strategies for self-respecting) Lifestyle monitoring Affective support: encouragement and reinforcement of healthy lifestyle | IndividualGroup | Face-to-face | 60 |
| 12 | Lifestyle monitoring: support, reinforcement, and reward Evaluation of the program | Individual | Face-to-face | 60 |
| Characteristics | Classification | Exp (n = 21) | Cont (n = 23) | χ2, t or z | p |
|---|---|---|---|---|---|
| M ± SD or n (%) | M ± SD or n (%) | ||||
| General Characteristics | |||||
| Age (years) | 22.7 ± 2.5 | 22.1 ± 2.6 | 0.805 | 0.425 | |
| Religion | Yes | 8 (38.1) | 8 (34.8) | 0.052 | 1.000 |
| No | 13 (61.9) | 15 (65.2) | |||
| Smoking | Yes | 2 (9.5) | 1 (4.3) | 0.463 | 0.599 |
| No | 19 (90.5) | 22 (95.7) | |||
| Alcohol consumption | Yes | 4 (19.0) | 7 (30.4) | 0.759 | 0.494 |
| No | 17 (81.0) | 16 (69.6) | |||
| Hours of sleep | 6.55 ± 1.45 | 6.52 ± 1.51 | 0.058 | 0.954 | |
| Variables | |||||
| HPLP II | 2.42 ± 0.30 | 2.24 ± 0.39 | 1.684 | 0.100 | |
| HR | 2.13 ± 0.48 | 1.88 ± 0.49 | 1.684 | 0.100 | |
| PA | 2.08 ± 0.52 | 1.75 ± 0.49 | 2.182 | 0.035 | |
| NUT | 2.25 ± 0.43 | 1.90 ± 0.52 | 2.436 | 0.019 | |
| SG | 2.60 ± 0.40 | 2.52 ± 0.58 | 0.502 | 0.618 | |
| IR | 3.02 ± 047 | 3.16 ± 0.63 | −0.903 | 0.372 | |
| SM | 2.42 ± 0.43 | 2.20 ± 0.53 | 1.545 | 0.130 | |
| DASS-21 | 15.71 ± 6.96 | 15.09 ± 0.30 | 0.252 | 0.803 | |
| Depression | 4.19 ± 3.34 | 4.52 ± 3.02 | −0.346 | 0.731 | |
| Anxiety | 3.62 ± 3.11 | 3.52 ± 3.41 | 0.314 | 0.922 | |
| Stress | 7.91 ± 3.40 | 5.04 ± 4.82 | 0.679 | 0.501 | |
| Reproductive health | |||||
| Knowledge | 21.24 ± 4.38 | 22.48 ± 3.40 | −0.986 | 0.330 | |
| Attitude | 46.86 ± 5.24 | 48.61 ± 5.30 | −1.101 | 0.277 | |
| Behavior | 62.71 ± 3.49 | 61.83 ± 4.58 | 0.718 | 0.477 | |
| Dysmenorrhea | 3.93 ± 2.51 | 4.50 ± 2.54 | −0.749 | 0.458 | |
| Gynecologic symptom (n) | 0.71 ± 0.78 | 0.52 ± 0.90 | 0.755 | 0.455 | |
| Yes | 11 (52.4) | 7 (30.4) | 2.187 | 0.220 | |
| No | 10 (47.6) | 16 (69.6) | |||
| LH/FSH ratio | 0.67 ± 0.42 | 1.11 ± 0.52 | −3.082 | 0.004 | |
| Body composition | |||||
| BW (kg) | 68.65 ± 10.04 | 67.68 ± 9.68 | 0.326 | 0.746 | |
| BMI (kg/m2) | 26.33 ± 2.68 | 26.05 ± 3.57 | 0.295 | 0.770 | |
| Body fat (%) | 36.63 ± 4.40 | 35.93 ± 6.17 | 0.428 | 0.671 | |
| Abdominal fat (%) | 0.86 ± 0.05 | 0.88 ± 0.04 | −1.691 | 0.098 | |
| HDL | 56.38 ± 10.91 | 57.09 ± 14.10 | −0.184 | 0.855 | |
| LDL | 105.90 ± 30.87 | 107.00 ± 24.72 | −0.130 | 0.897 | |
| TG | 89.43 ± 38.42 | 91.48 ± 26.62 | −0.207 | 0.837 | |
| Glucose | 84.71 ± 8.64 | 84.09 ± 8.01 | 0.250 | 0.804 |
| Characteristics | Groups | Pretest (before LSI) | Posttest (after 12-Week LSI) | Difference (Post-Pre) | t, F, χ2, or z | p | Cohen’sd |
|---|---|---|---|---|---|---|---|
| M ± SD or n (%) | M ± SD or n (%) | M ± SD or n (%) | |||||
| HPLP II | Exp | 2.42 ± 0.30 | 2.65 ± 0.45 | 0.23 ± 0.32 | 2.311 | 0.026 | 0.70 |
| Cont | 2.24 ± 0.39 | 2.27 ± 0.42 | 0.02 ± 0.28 | ||||
| HR | Exp | 2.13 ± 0.48 | 2.26 ± 0.57 | 0.13 ± 0.42 | 0.937 | 0.354 | 0.28 |
| Cont | 1.88 ± 0.49 | 1.90 ± 0.47 | 0.02 ± 0.38 | ||||
| PA a | Exp | 2.08 ± 0.52 | 2.48 ± 0.68 | 0.40 ± 0.62 | 7.718 | 0.011 | 0.57 |
| Cont | 1.75 ± 0.49 | 1.80 ± −0.60 | 0.05 ± 0.61 | ||||
| NUT a | Exp | 2.25 ± 0.43 | 2.81 ± 0.96 | 0.56 ± 0.78 | 4.531 | 0.039 | 0.70 |
| Cont | 1.90 ± 0.52 | 2.02 ± 0.58 | 0.13 ± 0.41 | ||||
| SG | Exp | 2.60 ± 0.40 | 2.52 ± 0.62 | −0.08 ± 0.58 | −0.069 | 0.946 | 0.14 |
| Cont | 2.52 ± 0.58 | 2.53 ± 0.67 | 0.00 ± 0.53 | ||||
| IR | Exp | 3.02 ± 047 | 3.12 ± 0.49 | 0.10 ± 0.44 | 2.116 | 0.040 | 0.64 |
| Cont | 3.16 ± 0.63 | 3.00 ± 0.53 | −0.16 ± 0.37 | ||||
| SM | Exp | 2.42 ± 0.43 | 2.71 ± 0.60 | 0.29 ± 0.44 | 1.516 | 0.137 | 0.45 |
| Cot | 2.20 ± 0.53 | 2.29 ± 0.56 | 0.10 ± 0.40 | ||||
| DASS-21 | Exp | 15.71 ± 6.96 | 11.29 ± 8.91 | −5.48 ± 8.00 | −3.197 | 0.003 | 0.97 |
| Cont | 15.09 ± 0.30 | 16.26 ± 12.81 | 3.57 ± 10.47 | ||||
| Depression | Exp | 4.19 ± 3.34 | 2.95 ± 3.50 | −1.52 ± 2.80 | −2.504 | 0.016 | 0.75 |
| Cont | 4.52 ± 3.02 | 4.78 ± 4.75 | 1.13 ± 4.05 | ||||
| Anxiety | Exp | 3.62 ± 3.11 | 2.33 ± 1.91 | −1.29 ± 2.78 | −2.841 | 0.007 | 0.86 |
| Cont | 3.52 ± 3.41 | 4.48 ± 3.82 | 1.30 ± 3.23 | ||||
| Stress | Exp | 7.91 ± 3.40 | 6.00 ± 4.46 | −2.67 ± 4.78 | −2.638 | 0.012 | 0.80 |
| Cont | 5.04 ± 4.82 | 7.00 ± 5.54 | 1.13 ± 4.76 | ||||
| Reproductive health | |||||||
| Knowledge | Exp | 21.24 ± 4.38 | 23.52 ± 3.64 | 2.77 ± 3.74 | 3.180 | 0.003 | 0.96 |
| Cont | 22.48 ± 3.40 | 23.04 ± 4.48 | −0.39 ± 2.81 | ||||
| Attitude | Exp | 46.86 ± 5.24 | 48.95 ± 6.00 | 2.96 ± 3.29 | 2.731 | 0.009 | 0.82 |
| Cont | 48.61 ± 5.30 | 47.04 ± 9.55 | −2.17 ± 8.00 | ||||
| Behavior | Exp | 62.71 ± 3.49 | 65.24 ± 5.39 | 3.67 ± 4.69 | 2.167 | 0.036 | 0.66 |
| Cont | 61.83 ± 4.58 | 62.17 ± 7.20 | 0.26 ± 5.63 | ||||
| Dysmenorrhea | Exp | 3.93 ± 2.51 | 3.43 ± 2.51 | −0.50 ± 1.26 | −1.322 | 0.193 | 0.40 |
| Cont | 4.50 ± 2.54 | 4.48 ± 2.43 | 0.15 ± 1.91 | ||||
| Gyn symptom (n) | Exp | 0.71 ± 0.78 | 0.48 ± 0.60 | −0.24 ± 0.77 | −0.091 | 0.928 | 0.03 |
| Cont | 0.52 ± 0.90 | 0.30 ± 0.47 | −0.22 ± 0.74 | ||||
| Yes | Exp | 11 (52.4) | 9 (42.9) | 0.732 | 0.533 | ||
| Cont | 7 (30.4) | 7 (30.4) | |||||
| LH/FSH ratio a | Exp | 0.67 ± 0.42 | 0.96 ± 0.64 | 0.26 ± 0.54 | 0.032 | 0.586 | 0.53 |
| Con | 1.11 ± 0.52 | 1.05 ± 0.52 | −0.06 ± 0.66 | ||||
| Body composition | |||||||
| BW (kg) | Exp | 68.65 ± 10.04 | 66.97 ± 9.30 | −1.69 ± 2.43 | −4.087 | <0.001 | 1.23 |
| Cont | 67.68 ± 9.68 | 68.49 ± 9.62 | 0.81 ± 1.57 | ||||
| BMI (kg/m2) | Exp | 26.33 ± 2.68 | 25.68 ± 2.46 | −0.65 ± 0.89 | −4.235 | <0.001 | 1.28 |
| Cont | 26.05 ± 3.57 | 26.38 ± 3.70 | 0.33 ± 0.63 | ||||
| Body fat (%) | Exp | 36.63 ± 4.40 | 36.37 ± 4.94 | −0.26 ± 2.05 | −2.402 | 0.021 | 0.72 |
| Cont | 35.93 ± 6.17 | 37.70 ± 5.13 | 1.76 ± 3.32 | ||||
| Abdominal fat (%) | Exp | 0.86 ± 0.05 | 0.88 ± 0.04 | 0.02 ± 0.03 | −0.657 | 0.515 | 0.28 |
| Cont | 0.88 ± 0.04 | 0.91 ± 0.05 | 0.03 ± 0.04 | ||||
| HDL | Exp | 56.38 ± 10.91 | 59.19 ± 11.52 | 2.81 ± 8.23 | 0.588 | 0.559 | 0.18 |
| Cont | 57.09 ± 14.10 | 58.22 ± 11.06 | 1.13 ± 10.45 | ||||
| LDL | Exp | 105.90 ± 30.87 | 98.38 ± 27.38 | −7.53 ± 13.73 | −0.074 | 0.941 | 0.02 |
| Cont | 107.00 ± 24.72 | 99.87 ± 17.35 | −7.13 ± 20.33 | ||||
| TG | Exp | 89.43 ± 38.42 | 79.67 ± 27.75 | −9.76 ± 33.50 | −2.188 | 0.034 | 0.66 |
| Cont | 91.48 ± 26.62 | 101.00 ± 31.34 | 9.52 ± 24.66 | ||||
| Glucose | Exp | 84.71 ± 8.64 | 83.05 ± 8.68 | −1.67 ± 8.82 | −0.344 | 0.732 | 0.10 |
| Cont | 84.09 ± 8.01 | 83.48 ± 9.77 | −0.61 ± 11.28 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nho, J.-H.; Chae, S.-W. Effects of a Lifestyle Intervention on Health-Promoting Behavior, Psychological Distress and Reproductive Health of Overweight and Obese Female College Students. Healthcare 2021, 9, 309. https://doi.org/10.3390/healthcare9030309
Nho J-H, Chae S-W. Effects of a Lifestyle Intervention on Health-Promoting Behavior, Psychological Distress and Reproductive Health of Overweight and Obese Female College Students. Healthcare. 2021; 9(3):309. https://doi.org/10.3390/healthcare9030309
Chicago/Turabian StyleNho, Ju-Hee, and Soo-Wan Chae. 2021. "Effects of a Lifestyle Intervention on Health-Promoting Behavior, Psychological Distress and Reproductive Health of Overweight and Obese Female College Students" Healthcare 9, no. 3: 309. https://doi.org/10.3390/healthcare9030309
APA StyleNho, J.-H., & Chae, S.-W. (2021). Effects of a Lifestyle Intervention on Health-Promoting Behavior, Psychological Distress and Reproductive Health of Overweight and Obese Female College Students. Healthcare, 9(3), 309. https://doi.org/10.3390/healthcare9030309






