COVID-19 and Mental Health: A Study of Stress, Resilience, and Depression among the Older Population in Pakistan
Abstract
:1. Introduction
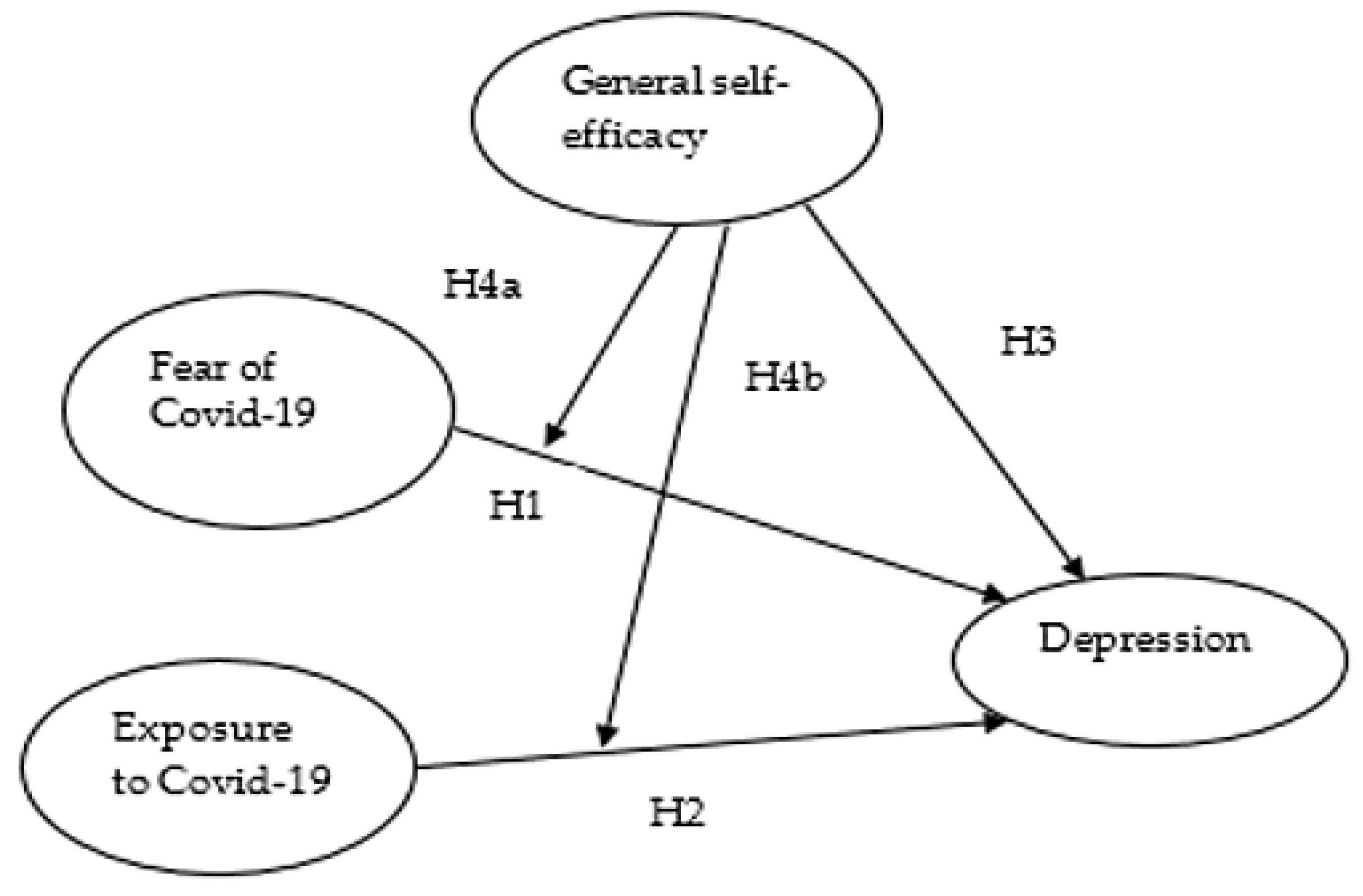
- Do COVID-19-related stressors, such as fear of and exposure to COVID-19, affect the mental health of elderly people?
- Do coping abilities like self-efficacy play a moderating role between fear of COVID-19, exposure to COVID-19 and depression?
2. Theoretical Background
2.1. Fear and Exposure of COVID-19
2.2. COVID-19 and Depression
2.3. COVID-19 and Self-Efficacy
3. Hypothesized Model
4. Methods of the Study
4.1. Sample and Data Collection
4.2. Measures and Instruments
4.3. Ethics
5. Results
5.1. Demographic Assessment
5.2. Descriptive Statistics
5.3. Regression Analysis and Interpretation
5.4. Moderation Analysis
Line Graph Interpretation
6. Discussion
7. Conclusions
Limitation of the Study and Future Direction
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Worldometer. Covid-19 Coronavirus Pandemic. Available online: https://www.worldometers.info/coronavirus (accessed on 5 April 2021).
- Yildirim, H.; Işik, K.; Aylaz, R. The effect of anxiety levels of elderly people in quarantine on depression during covid-19 pandemic. Soc. Work. Public Health 2021, 36, 194–204. [Google Scholar] [CrossRef]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.A.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef] [Green Version]
- Etxebarria, N.O.; Santamaria, M.D.; Gorrochategi, M.P.; Mondragon, N.I. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad. Saude Publica 2020, 36, e00054020. [Google Scholar] [CrossRef]
- Gorrochategi, M.P.; Munitis, A.E.; Santamaria, M.D.; Etxebarria, N.O. Stress, anxiety, and depression in people aged over 60 in the COVID-19 outbreak in a sample collected in Northern Spain. Am. J. Geriatr. Psychiatry 2020, 28, 993–998. [Google Scholar] [CrossRef]
- Guo, J.; Feng, X.L.; Wang, X.H.; van IJzendoorn, M.H. Coping with COVID-19: Exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int. J. Environ. Res. Public Health 2020, 17, 3857. [Google Scholar] [CrossRef] [PubMed]
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M.; Dörrie, N.; Schweda, A.; Skoda, E.-M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef]
- Tsang, S.; Avery, A.R.; Duncan, G.E. Fear and depression linked to COVID-19 exposure A study of adult twins during the COVID-19 pandemic. Psychiatry Res. 2021, 296, 113699. [Google Scholar] [CrossRef]
- Blackburn, L.; Owens, G.P. The effect of self-efficacy and meaning in life on posttraumatic stress disorder and depression severity among veterans. J. Clin. Psychol. 2015, 71, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.P.H.; Hui, B.P.H.; Wan, E.Y.F. Depression and Anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3740. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Xu, J.; Huang, S.; Li, P.; Lu, C.; Xie, S. Risk Perception and Depression in Public Health Crises: Evidence from the COVID-19 Crisis in China. Int. J. Environ. Res. Public Health 2020, 17, 5728. [Google Scholar] [CrossRef] [PubMed]
- Le, H.T.; Lai, A.J.X.; Sun, J.; Hoang, M.T.; Vu, L.G.; Pham, H.Q.; Nguyen, T.H.; Tran, B.X.; Latkin, C.A.; Le, X.T.T.; et al. Anxiety and Depression Among People Under the Nationwide Partial Lockdown in Vietnam. Front. Public Health 2020, 8, 589359. [Google Scholar] [CrossRef] [PubMed]
- Germani, A.; Buratta, L.; Delvecchio, E.; Mazzeschi, C. Emerging Adults and COVID-19: The Role of Individualism-Collectivism on Perceived Risks and Psychological Maladjustment. Int. J. Environ. Res. Public Health 2020, 17, 3497. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Salgado, J.; Andrés-Villas, M.; Domínguez-Salas, S.; Díaz-Milanés, D.; Ruiz-Frutos, C. Related Health Factors of Psychological Distress During the COVID-19 Pandemic in Spain. Int. J. Environ. Res. Public Health 2020, 17, 3947. [Google Scholar] [CrossRef] [PubMed]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef]
- Mumtaz, M. COVID-19 and mental health challenges in Pakistan. Int. J. Soc. Psychiatry 2020, 0020764020954487. [Google Scholar] [CrossRef]
- Bandura, A. The explanatory and predictive scope of self-efficacy theory. J. Soc. Clin. Psychol. 1986, 4, 359–373. [Google Scholar] [CrossRef]
- Taylor, S.E.; Brown, J.D. Illusion and well-being: A social psychological perspective on mental health. Psychol. Bull. 1988, 103, 193. [Google Scholar] [CrossRef]
- Bandura, A. The assessment and predictive generality of self-percepts of efficacy. J. Behav. Ther. Exp. Psychiatry 1982, 13, 195–199. [Google Scholar] [CrossRef]
- Gecas, V. The social psychology of self-efficacy. Ann. Rev. Sociol. 1989, 15, 291–316. [Google Scholar] [CrossRef]
- Benight, C.C.; Cieslak, R. Cognitive factors and resilience: How self-efficacy contributes to coping with. Resil. Ment. Health Chall. Lifesp. 2011, 45–55. [Google Scholar] [CrossRef]
- Newman, R. APA’s resilience initiative. Prof. Psychol. Res. Pract. 2005, 36, 227. [Google Scholar] [CrossRef]
- O’Leary, V.E. Strength in the face of adversity: Individual and social thriving. J. Soc. Issues 1998, 54, 425–446. [Google Scholar] [CrossRef]
- Santini, Z.I.; Jose, P.E.; Cornwell, E.Y.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef] [Green Version]
- Azeem, F.; Naz, M.A. Resilience, death anxiety, and depression among institutionalized and noninstitutionalized elderly. Pak. J. Psychol. Res. 2015, 30, 111–130. [Google Scholar]
- Shaabani, J.; Rahgoi, A.; Nourozi, K.; Rahgozar, M.; Shaabani, M. The relationship between self-efficacy and quality of life among elderly people. Iran. J. Ageing 2017, 11, 518–527. [Google Scholar] [CrossRef] [Green Version]
- Doba, N.; Tokuda, Y.; Saiki, K.; Kushiro, T.; Hirano, M.; Matsubara, Y.; Hinohara, S. Assessment of self-efficacy and its relationship with frailty in the elderly. Intern. Med. 2016, 55, 2785–2792. [Google Scholar] [CrossRef] [Green Version]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Satici, B.; Gocet-Tekin, E.; Deniz, M.E.; Satici, S.A. Adaptation of the Fear of COVID-19 Scale: Its association with psychological distress and life satisfaction in Turkey. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Andrade, E.F.; Pereira, L.J.; Oliveira, A.P.L.D.; Orlando, D.R.; Alves, D.A.G.; Guilarducci, J.D.S.; Castelo, P.M. Perceived fear of COVID-19 infection according to sex, age and occupational risk using the Brazilian version of the Fear of COVID-19 Scale. Death Stud. 2020, 1–10. [Google Scholar] [CrossRef]
- Reznik, A.; Gritsenko, V.; Konstantinov, V.; Khamenka, N.; Isralowitz, R. COVID-19 fear in Eastern Europe: Validation of the fear of COVID-19 scale. Int. J. Ment. Health Addict. 2020, 1–6. [Google Scholar] [CrossRef]
- Montazeri, A.; Vahdaninia, M.; Ebrahimi, M.; Jarvandi, S. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health Qual. Life Outcomes 2003, 1, 14. [Google Scholar] [CrossRef] [PubMed]
- Li, D.-J.; Ko, N.-Y.; Chen, Y.-L.; Wang, P.-W.; Chang, Y.-P.; Yen, C.-F.; Lu, W.-H. COVID-19-Related Factors Associated with Sleep Disturbance and Suicidal Thoughts among the Taiwanese Public: A Facebook Survey. Int. J. Environ. Res. Public Health 2020, 17, 4479. [Google Scholar] [CrossRef] [PubMed]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.; Guo, L.; Yu, M.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- Luszczynska, A.; Scholz, U.; Schwarzer, R. The general self-efficacy scale: Multicultural validation studies. J. Psychol. 2005, 139, 439–457. [Google Scholar] [CrossRef] [Green Version]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191. [Google Scholar] [CrossRef]
- Luszczynska, A.; Schwarzer, R.; Lippke, S.; Mazurkiewicz, M. Self-efficacy as a moderator of the planning–behaviour relationship in interventions designed to promote physical activity. Psychol. Health 2011, 26, 151–166. [Google Scholar] [CrossRef]
- Grau, R.; Salanova, M.; Peiro, J.M. Moderator effects of self-efficacy on occupational stress. Psychol. Spain 2001, 5, 63–74. [Google Scholar]
- Kuys, S.S.; Donovan, J.; Mattin, S.; Low Choy, N.L. Balance self-efficacy in older adults following inpatient rehabilitation. Int. J. Rehabil. Res. 2015, 38, 167–172. [Google Scholar] [CrossRef]
- Gilmartin, M.J.; Nokes, K. A self-efficacy scale for clinical nurse leaders®: Results of a pilot study. Nurs. Econ. 2015, 33, 133. [Google Scholar]
- Newman, D.A. Missing data: Five practical guidelines. Organ. Res. Methods 2014, 17, 372–411. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pieh, C.; Budimir, S.; Probst, T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. [Google Scholar] [CrossRef] [PubMed]
- Solomou, I.; Constantinidou, F. Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: Age and sex matter. Int. J. Environ. Res. Public Health 2020, 17, 4924. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. PROCESS: A Versatile Computational Tool for Observed Variable Mediation, Moderation, and Conditional Process Modeling; University of Kansas: Lawrence, KS, USA, 2012. [Google Scholar]
- Sahito, N.; Han, H.; Nguyen, T.V.T.; Kim, I.; Hwang, J.; Jameel, A. Examining the Quasi-Public Spaces in Commercial Complexes. Sustainability 2020, 12, 1830. [Google Scholar] [CrossRef] [Green Version]
- Manzoor, F.; Wei, L.; Hussain, A.; Asif, M.; Shah, S.I.A. Patient Satisfaction with Health Care Services; An Application of Physician’s Behavior as a Moderator. Int. J. Environ. Res. Public Health 2019, 16, 3318. [Google Scholar] [CrossRef] [Green Version]
- Aiken, L.S.; West, S.G.; Reno, R.R. Multiple Regression: Testing and Interpreting Interactions; Sage: Thousand Oaks, CA, USA, 1991. [Google Scholar]
- Manzoor, F.; Wei, L.; Nurunnabi, M.; Abdul Subhan, Q. Role of SME in Poverty Alleviation in SAARC Region via Panel Data Analysis. Sustainability 2019, 11, 6480. [Google Scholar] [CrossRef] [Green Version]
- Manzoor, F.; Wei, L.; Asif, M. The contribution of sustainable tourism to economic growth and employment in Pakistan. Int. J. Environ. Res. Public Health 2019, 16, 3785. [Google Scholar] [CrossRef] [Green Version]
- Wu, A.D.; Zumbo, B.D. Understanding and Using Mediators and Moderators. Soc. Indic. Res. 2007, 87, 367. [Google Scholar] [CrossRef]
- Manzoor, F.; Wei, L.; Bányai, T.; Nurunnabi, M.; Subhan, Q.A. An examination of sustainable HRM practices on job performance: An application of training as a moderator. Sustainability 2019, 11, 2263. [Google Scholar] [CrossRef] [Green Version]
- Manzoor, F.; Wei, L.; Nurunnabi, M.; Subhan, Q.A.; Shah, S.I.A.; Fallatah, S. The impact of transformational leadership on job performance and CSR as mediator in SMEs. Sustainability 2019, 11, 436. [Google Scholar] [CrossRef] [Green Version]
- Li, J.-B.; Yang, A.; Dou, K.; Cheung, R.Y.M. Self-Control Moderates the Association Between Perceived Severity of Coronavirus Disease 2019 (COVID-19) and Mental Health Problems Among the Chinese Public. Int. J. Environ. Res. Public Health 2020, 17, 4820. [Google Scholar] [CrossRef]
- Losada-Baltar, A.; Jiménez-Gonzalo, L.; Gallego-Alberto, L.; Pedroso-Chaparro, M.d.S.; Fernandes-Pires, J.; Márquez-González, M. “We Are Staying at Home.” Association of Self-perceptions of Aging, Personal and Family Resources, and Loneliness with Psychological Distress During the Lock-Down Period of COVID-19. J. Gerontol. Ser. B 2020, 76, e10–e16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef] [PubMed]



| Frequency | Percent | |
|---|---|---|
| Gender | ||
| Male | 211 | 68.1 |
| Female | 99 | 31.9 |
| Age | ||
| 50–60 | 39 | 12.6 |
| 60–70 | 135 | 43.5 |
| 70–80 | 113 | 36.5 |
| Above 80 | 23 | 7.4 |
| Work status | ||
| Employed | 133 | 42.9 |
| Retired/unemployed | 177 | 57.1 |
| Variable | Mean | Std. D | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| Fear of COVID-19 | 4.128 | 0.557 | 0.90 | |||
| Depression | 3.973 | 0.665 | 0.146 * | 0.85 | ||
| Self-efficacy | 1.502 | 0.829 | −0.241 ** | −0.150 ** | 0.94 | |
| COVID-19 exposure | 3.920 | 1.042 | 0.203 ** | 0.129 * | −0.260 ** | 0.95 |
| Variable | Coefficient | T-Statistic | p-Value | Lower Bound CI 95% | Upper Bound CI 95% |
|---|---|---|---|---|---|
| Constant | 3.321 | 11.268 | 0.000 | 2.706 | 3.808 |
| Fear of COVID-19 | 0.162 ** | 2.582 | 0.004 | 0.060 | 0.311 |
| Self-efficacy | −0.130 ** | −2.685 | 0.008 | −0.205 | −0.035 |
| Exposure to COVID-19 | 0.147 ** | 2.298 | 0.003 | 0.050 | 0.244 |
| Age | −0.105 ** | −1.712 | 0.008 | −0.188 | 0.013 |
| Gender | 0.185 *** | 3.315 | 0.001 | 0.107 | 0.420 |
| Work status | −0.214 ** | −3.576 | 0.004 | −0.445 | −0.129 |
| R-square | 0.163 | ||||
| R adjusted | 0.147 | ||||
| F-statistic | 9.852 (0.000) |
| Moderation Assessment | Coeff. | Std. Error | T-Statistic | p-Value | Lower Bound CI 95% | Upper Bound CI 95% | R2Δ |
|---|---|---|---|---|---|---|---|
| Moderation I (FOC*SE) | 0.268 | 0.046 | 5.743 | 0.000 | 0.176 | 0.359 | 0.093 |
| Moderation II (EC*SE) | 0.012 | 0.032 | 0.386 | 0.699 | −0.056 | 0.075 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mumtaz, A.; Manzoor, F.; Jiang, S.; Anisur Rahaman, M. COVID-19 and Mental Health: A Study of Stress, Resilience, and Depression among the Older Population in Pakistan. Healthcare 2021, 9, 424. https://doi.org/10.3390/healthcare9040424
Mumtaz A, Manzoor F, Jiang S, Anisur Rahaman M. COVID-19 and Mental Health: A Study of Stress, Resilience, and Depression among the Older Population in Pakistan. Healthcare. 2021; 9(4):424. https://doi.org/10.3390/healthcare9040424
Chicago/Turabian StyleMumtaz, Ayesha, Faiza Manzoor, Shaoping Jiang, and Mohammad Anisur Rahaman. 2021. "COVID-19 and Mental Health: A Study of Stress, Resilience, and Depression among the Older Population in Pakistan" Healthcare 9, no. 4: 424. https://doi.org/10.3390/healthcare9040424
APA StyleMumtaz, A., Manzoor, F., Jiang, S., & Anisur Rahaman, M. (2021). COVID-19 and Mental Health: A Study of Stress, Resilience, and Depression among the Older Population in Pakistan. Healthcare, 9(4), 424. https://doi.org/10.3390/healthcare9040424






