Mapping Evidence of Impacts of COVID-19 Outbreak on Sexual and Reproductive Health: A Scoping Review
Abstract
:1. Introduction
2. Materials and Method
2.1. Study Design
2.2. Research Question
2.3. Data sources and Literature Search
2.4. Study Selection
2.5. Eligibility Criteria
2.5.1. Inclusion Criteria
- Research articles reporting information regarding the impact of COVID-19 on family planning services, maternal and child health service, and sexual behavior.
- Articles that explored any study design published in peer-reviewed journals addressing the research question.
- Articles published in English.
- Articles published between December 2019 and October 2020.
2.5.2. Exclusion Criteria
2.6. Condition or Domain Being Studied
2.7. Participants/Population
2.8. Data Charting
2.9. Quality Assessment of the Included Studies
2.10. Collating, Summarizing, and Reporting the Results
3. Results
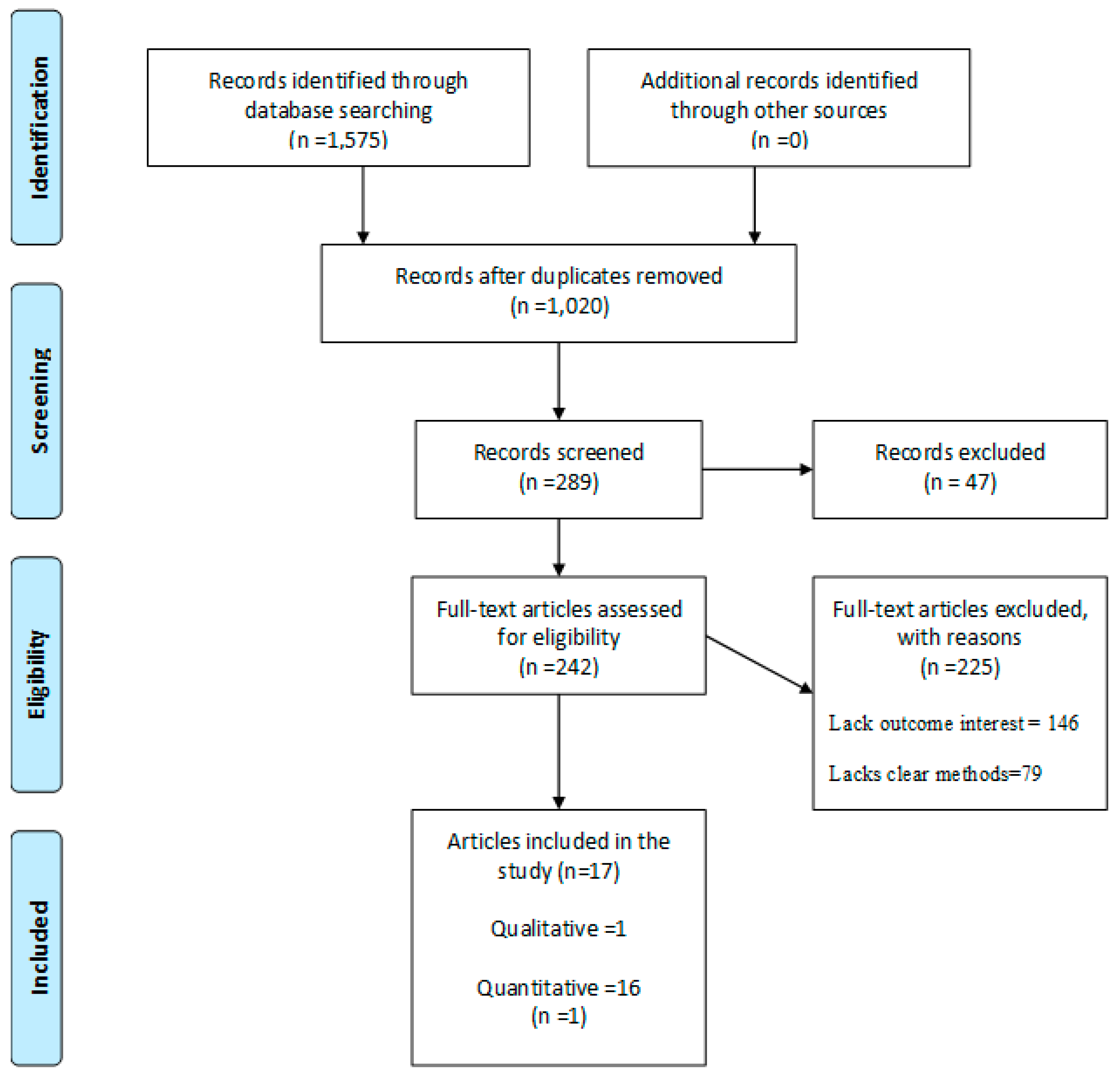
3.1. Screening Results
3.2. Characteristics of the Included Studies
3.3. Quality of Evidence from the Included Studies
3.4. Themes from Included Studies
3.4.1. COVID-19 and Family Planning Services
3.4.2. COVID-19 and Maternal and Child Services
3.4.3. COVID-19 and Sexual Behavior
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| COVID-19 | Coronavirus Disease 2019 |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-analyses |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews |
| ICPD | International Conference on Population and Development |
| STI | Sexually Transmitted Infections |
| AACODS | Authority, Accuracy, Coverage, Objectivity, Date, and Significance |
| OSF | Open Science Framework |
| PCC | Population, Concept, and Context |
| Embase | Excerpta Medica database |
| CINAHL | Cumulative Index of Nursing and Allied Health Literature |
| WOS | Web of Science |
| AJOL | Africa Journals Online |
| SARC | Short-Acting Reversible Contraception |
| MSM | Men who have sex with Men |
| MMR | Measles-mumps-rubella |
| IBD | Inflammatory Bowel Disease |
| PPE | Personal Protective Equipment |
| HIV | Human Immunodeficiency Virus |
| CAS | Condom-less Anal Sex |
| FSFI | Female Sexual; Function Index |
| LMICs | Low-Middle-Income Countries |
| HICs | High Income Countries; PrEP: Pre-Exposure Prophylaxis |
References
- World Health Organization. Coronavirus Disease (COVID-19) and Sexual and Reproductive Health; WHO website: Geneva, Switzaland, 2020. [Google Scholar]
- Church, K.; Gassner, J.; Elliott, M. Reproductive health under Covid-19-challenges of responding in a global crisis. Sex. Reprod. Health Matters 2020, 28, 1–3. [Google Scholar] [CrossRef]
- Purdy, C. Opinion: How Will COVID-19 Affect Global Access to Contraceptives—And What Can We Do About It? Devex: Washington, DC, USA, 2020. [Google Scholar]
- International Planned Parenthood Federation. COVID-19 Pandemic Cuts Access to Sexual and Reproductive Healthcare for Women around the World; IPPF: London, UK, 2020. [Google Scholar]
- Li, G.; Tang, D.; Song, B.; Wang, C.; Shen, Q.; Xu, C.; Geng, H.; Wu, H.; He, X.; Cao, Y. Impact of the COVID-19 pandemic on partner relationships and sexual and reproductive health: Cross-sectional, online survey study. J. Med. Internet Res. 2020, 22, 20961. [Google Scholar] [CrossRef] [PubMed]
- UN Department for Economic and Social Information and Policy Analysis. Population and Development: Programme of Action Adopted at the International Conference on Population and Development, Cairo, 5–13 September 1994; Department for Economic and Social Information and Policy Analysis: New York, NY, USA, 1995. [Google Scholar]
- Fathalla, M.F.; Fathalla, M.M. Sexual and reproductive health: Overview. Int. Encycl. Public Health 2008, 5, 695–705. [Google Scholar]
- Glasier, A.; Gülmezoglu, A.M.; Schmid, G.P.; Moreno, C.G.; Van Look, P.F. Sexual and reproductive health: A matter of life and death. Lancet 2006, 368, 1595–1607. [Google Scholar] [CrossRef]
- Shaw, D. The FIGO initiative for the prevention of unsafe abortion. Int. J. Gynecol. Obstet. 2010, 110, 17–19. [Google Scholar] [CrossRef] [PubMed]
- Shaukat, S.; Kazmi, A.H. Sexually transmitted infections and syndromic management. J. Pak. Assoc. Dermatol. 2016, 25, 159–161. [Google Scholar]
- Shaw, D. Access to sexual and reproductive health for young people: Bridging the disconnect between rights and reality. Int. J. Gynecol. Obs. 2009, 106, 132–136. [Google Scholar] [CrossRef]
- Yao, J.; Murray, A.T.; Agadjanian, V. A geographical perspective on access to sexual and reproductive health care for women in rural Africa. Soc. Sci. Med. 2013, 96, 60–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müller, S.; Spencer, T.M.; Daskilewicz, K. The no-go zone: A qualitative study of access to sexual and reproductive health services for sexual and gender minority adolescents in Southern Africa. Reprod. Health 2018, 15, 12. [Google Scholar] [CrossRef] [Green Version]
- Colombini, M.; Rechel, B.; Mayhew, S.H. Access of Roma to sexual and reproductive health services: Qualitative findings from Albania, Bulgaria and Macedonia. Glob. Public Health 2012, 7, 522–534. [Google Scholar] [CrossRef]
- World Health Organization. Responding to Community Spread of COVID-19: Interim Guidance; World Health Organization: Geneva, Switzerland, 7 March 2020. [Google Scholar]
- Tang, K.; Gaoshan, J.; Ahonsi, B.; Ali, M.; Bonet, M.; Broutet, N.; Kara, E.; Kim, C.; Thorson, A.; Thwin, S.S. Sexual and reproductive health (SRH): A key issue in the emergency response to the coronavirus disease (COVID-19) outbreak. Reprod. Health 2020, 17, 59. [Google Scholar] [CrossRef]
- Vora, K.S.; Saiyed, S.; Natesan, S. Impact of COVID-19 on family planning services in India. Sexual Reprod. Health Matters 2020, 28, 1785378. (In English) [Google Scholar] [CrossRef] [PubMed]
- Nagendra, G.; Carnevale, C.; Neu, N.; Cohall, A.; Zucker, J. The potential impact and availability of sexual health services during the COVID-19 pandemic. Sex. Transm. Dis. 2020, 47, 434. [Google Scholar] [CrossRef] [PubMed]
- Karkee, R.; Morgan, A. Providing maternal health services during the COVID-19 pandemic in Nepal. Lancet Glob. Health. 2020, 8, 1243–1244. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report, 70; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Riley, T.; Sully, E.; Ahmed, Z.; Biddlecom, A. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low-and middle-income countries. Int. Perspect. Sex. Reprod. Health 2020, 46, 46. [Google Scholar] [CrossRef] [PubMed]
- Graham, W.J.; Afolabi, B.; Benova, L.; Campbell, O.M.R.; Filippi, V.; Nakimuli, A.; Penn-Kekana, L.; Sharma, G.; Okomo, U.; Valongueiro, S.; et al. Protecting hard-won gains for mothers and newborns in low-income and middle-income countries in the face of COVID-19: Call for a service safety net. BMJ Glob. Health 2020, 5, 2754. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Joanna Briggs Institute. Systematic Review Resource Package; The Joanna Briggs Institute: Adelaide, Australia, 2015. [Google Scholar]
- Law, M.; Stewart, D.; Letts, L.; Pollock, N.; Bosch, J.; Westmorland, M. Guidelines for Critical Review of Qualitative Studies. Master’s Thesis, University Occupational Therapy Evidence-Based Practice Research Group, Hamilton, ON, Canada, 1988. [Google Scholar]
- Tyndall, J. The AACODS Checklist Is Designed to Enable Evaluation and Critical Appraisal of Grey Literature; Flinders Academic: Adelaide, Australia, 2010. [Google Scholar]
- Castleberry. NVivo 10 [Software Program]; Version 10; QSR International 2012: Burlington, VT, USA, 2014. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. RESEARCH METHODS & REPORTING-Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement-David Moher and colleagues introduce PRISMA, an update of the QUOROM guidelines for reporting systematic reviews and meta-analyses. Bmj (Cr)-Print 2009, 338, 332. [Google Scholar]
- Karavadra, B.; Stockl, A.; Prosser-Snelling, E.; Simpson, P.; Morris, E. Women’s perceptions of COVID-19 and their healthcare experiences: A qualitative thematic analysis of a national survey of pregnant women in the United Kingdom. BMC Pregnancy Childbirth 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jacob, L.; Smith, L.; Butler, L.; Barnett, L.; Grabovac, Y.; McDermott, I.; Armstrong, D.; Yakkundi, N.; Tully, M.A. Challenges in the practice of sexual medicine in the time of COVID-19 in the United Kingdom. J. Sex. Med. 2020, 17, 1229–1236. [Google Scholar] [CrossRef] [PubMed]
- McDonald, H.I.; Tessier, E.; White, J.M.; Woodruff, M.; Knowles, C.; Bates, C.; Parry, J.; Walker, J.L.; Scott, J.A.; Smeeth, L.; et al. Early impact of the coronavirus disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Eurosurveillance 2020, 25, 2000848. [Google Scholar]
- Ashton, J.J.; Kammermeier, J.; Spray, C.; Russell, R.K.; Hansen, R.; Howarth, L.J.; Deb, P.; Renji, E.; Muhammed, R.; Beattie, R.M.; et al. Impact of COVID-19 on diagnosis and management of paediatric inflammatory bowel disease during lockdown: A UK nationwide study. Arch. Dis. Child. 2020, 105, 1186–1191. [Google Scholar] [CrossRef] [PubMed]
- Torres, T.S.; Hoagland, B.; Bezerra, D.R.; Garner, A.; Jalil, E.M.; Coelho, L.E.; Benedetti, M.; Pimenta, C.; Grinsztejn, B.; Veloso, V.G. Impact of COVID-19 Pandemic on sexual minority populations in Brazil: An analysis of social/racial disparities in maintaining social distancing and a description of sexual behavior. AIDS Behav. 2020, 25, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, T.H.; Zlotorzynska, M.; Rai, M.; Baral, S.D. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. Aids Behav. 2020, 24, 2024–2032. [Google Scholar] [CrossRef]
- Stephenson, R.; Chavanduka, T.M.; Rosso, M.T.; Sullivan, S.P.; Pitter, R.A.; Hunter, A.S.; Rogers, E. Sex in the time of COVID-19: Results of an online survey of gay, bisexual and other men who have sex with men’s experience of sex and HIV prevention during the US COVID-19 epidemic. Aids Behav. 2021, 25, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Starks, T.J.; Jones, S.S.; Sauermilch, D.; Benedict, M.; Adebayo, T.; Cain, D.; Simpson, K.N. Evaluating the impact of COVID-19: A cohort comparison study of drug use and risky sexual behavior among sexual minority men in the USA. Drug Alcohol Depend. 2020, 216, 108260. [Google Scholar] [CrossRef]
- Gillespie, D.; Knapper, C.; Hughes, D.; Couzens, Z.; Wood, F.; De Bruin, M.; Ma, R.; Jones, A.T.; Williams, A.; Hood, K. Early impact of COVID-19 social distancing measures on reported sexual behaviour of HIV pre-exposure prophylaxis users in Wales. Sex. Transm. Infect. 2021, 97, 85–87. [Google Scholar] [CrossRef]
- Caruso, S.; Rapisarda, A.M.C.; Minona, P. Sexual activity and contraceptive use during social distancing and self-isolation in the COVID-19 pandemic. Eur. J. Contracept. Reprod. Health Care 2020, 25, 445–448. [Google Scholar] [CrossRef]
- Schiavi, M.C.; Spina, V.; Zullo, M.A.; Colagiovanni, V.; Luffarelli, P.; Rago, R.; Palazzetti, P. Love in the time of COVID-19: Sexual function and quality of life analysis during the social distancing measures in a group of Italian reproductive-age women. J. Sex. Med. 2020, 17, 1407–1413. [Google Scholar] [CrossRef] [PubMed]
- Shilo, G.; Mor, Z. COVID-19 and the Changes in the Sexual Behavior of Men Who Have Sex With Men: Results of an Online Survey. J. Sex. Med. 2020, 17, 1827–1834. (In English) [Google Scholar] [CrossRef]
- Lehmiller, J.J.; Garcia, J.R.; Gesselman, A.N.; Mark, K.P. Less sex, but more sexual diversity: Changes in sexual behavior during the COVID-19 coronavirus pandemic. Leis. Sci. 2020, 1–10. [Google Scholar] [CrossRef]
- Yuksel, B.; Ozgor, F. Effect of the COVID-19 pandemic on female sexual behavior. Int. J. Gynecol. Obstet. 2020, 150, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Ceulemans, M.; Verbakel, J.Y.; van Calsteren, K.; Eerdekens, A.; Allegaert, K.; Foulon, V. SARS-CoV-2 infections and impact of the COVID-19 pandemic in pregnancy and breastfeeding: Results from an observational study in primary care in Belgium. Int. J. Environ. Res. Public Health 2020, 17, 6766. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, A.; Matonóg, A.; Pilarska, J.; Sieradzka, P.; Szul, M.; Czuba, B.; Drosdzol-Cop, A. The impact of COVID− 19 on female sexual health. Int. J. Environ. Res. Public Health 2020, 17, 7152. [Google Scholar] [CrossRef] [PubMed]
- Anja, S.; Skirrow, H.; Kampmann, B. Impact of COVID-19 on Immunization Services for Maternal and Infant Vaccines: Results of a Survey Conducted by Imprint—The Immunising Pregnant Women and Infants Network. Vaccines 2020, 8, 556. [Google Scholar]
- Mbizvo, M.T.; Phillips, S.J. Family planning: Choices and challenges for developing countries. Best Pract. Res. Clin. Obstet. Gynaecol. 2014, 28, 931–943. [Google Scholar] [CrossRef] [PubMed]
- Olagunju, O.S.; Bolarinwa, O.A.; Babalola, T. Social distancing, lockdown obligatory, and response satisfaction during Covid-19 pandemic: Perception of Nigerian social media users. Adv. J. Soc. Sci. 2019, 7, 44–53. [Google Scholar] [CrossRef]
- Kates, J.; Michaud, J.; Tolbert, J. Stay-At-Home Orders to Fight COVID-19 in the United States: The Risks of a Scattershot Approach. 2020. Available online: https://www.kff.org/coronavirus-policy-watch/stay-at-home-orders-to-fight-COVID-19/ (accessed on 4 November 2020).
- Panzeri, M.; Ferrucci, R.; Cozza, A.; Fontanesi, L. Changes in sexuality and quality of couple relationship during the Covid-19 lockdown. Front. Psychol. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Lyons, H.; Manning, W.; Giordano, P.; Longmore, M. Predictors of heterosexual casual sex among young adults. Arch. Sex. Behav. 2013, 42, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Yip, P.S.; Zhang, H.; Lam, T.H.; Lam, K.F.; Lee, A.M.; Chan, J.; Fan, S. Sex knowledge, attitudes, and high-risk sexual behaviors among unmarried youth in Hong Kong. BMC Public Health 2013, 13, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lyons, H.A. Heterosexual casual sex and STI diagnosis: A latent class analysis. Int. J. Sex. Health 2017, 29, 32–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Criteria | Determinants | Description |
|---|---|---|
| P—Population | All population | All people whose sexual and reproductive health has been impacted by COVID-19. |
| C—Concept | Family planning services | This is determined by family planning service availability to people in any country. The service includes availability and access to contraceptive service of choice during the COVID-19 pandemic. |
| Maternal and child health service | This is determined by maternal and child health service availability to people in any country. The service includes availability and access to maternal and child health services of choice during the COVID-19 pandemic. | |
| Sexual behavior | This is to determine if there has been any change in sexual behavior in terms of engagement in non-use of condom, multiple sexual partners, or transactional sex during the COVID-19 pandemic. | |
| C—Context | All countries | Any country that reported the impact of COVID-19 on sexual and reproductive health between December 2019 and October 2020. |
| Countries Included in the Study | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| COVID-19 and SHR Services | United Kingdom | Brazil | United States | Wales | Italy | Israel | Turkey | Belgium | Poland | Multiple Countries |
| COVID-19 and family planning services | X * | X * | X * | |||||||
| COVID-19 and maternal and child services | XX *** | XX * | XX * | XX * | ||||||
| COVID-19 and sexual behavior | XXX * | XXX * | XXX *** | XXX * | XXX * | XXX* | XXX * | XXX * | XXX * | |
| Author and Year | Study Setting (Country) | Study Design | Population (n) (Sample Size and Target Pop) | COVID-19 and Family Planning Services | COVID-19 and Maternal and Child Services | COVID-19 and Sexual Behavior |
|---|---|---|---|---|---|---|
| Babu Karavadra et al. and 2020 [31] | United Kingdom | Cross-sectional (Web survey) | Women who were pregnant or delivered during COVID-19, n = 1451 |
| ||
| Thiago S. Torres et al. and 2020 [35] | Brazil | Cross-sectional (Web-survey) | n = 3486 among cismen |
| ||
| Travis H. Sanchez et al. and 2020 [36] | United States | Cross-sectional (Web survey) | Men who have sex with men n = 1051 |
|
| |
| David Gillespie et al. and 2020 [39] | Wales | Longitudinal survey (Web survey) | Participants were individuals accessing PrEP n = 56 |
| ||
| Salvatore Caruso and 2020 [40] | Italy | Cross-sectional (Web survey) | Among women known to be using hormonal contraceptives, n = 169 |
| ||
| Rob Stephenson et al. and 2020 [37] | United States | Cross-sectional (Web survey) | Among gay, bisexual, and other men who have sex with men, n = 518 |
| ||
| Guy Shilo and Zohar Mor and 2020 [42] | Israel | Cross-sectional (Web survey) | Among men who have sex with men, n = 2562 |
| ||
| Michele Carlo Schiavi and 2020 [41] | Italy | Cross-sectional | Women of reproductive age, n = 89 |
| ||
| Louis Jacob et al. and 2020 [32] | United Kingdom | Cross-sectional (Web survey) | n = 868 |
| ||
| Tyrel J. Starks et al. and 2020 [38] | United States | Cohort-control design | Among sexual minority men, n = 455 |
| ||
| Justin J. Lehmiller et al. and 2020 [43] | United States 73.4% Canada 6.0% United Kingdom 5.7% Australia 2.4% Other countries, 12.5% | Cross-sectional (Web survey) | Among participants 18 years of age or older, n = 1559 |
| ||
| Bahar Yuksel, Faruk Ozgor and 2020 [44] | Turkey | Cross-sectional (Telephone) | Among married patients who were older than 18 years and sexually active, n = 58 |
|
|
|
| Helen I McDonald et al. and 2020 [33] | United Kingdom | Cross-sectional | Vaccination among children n = 67,116 |
| ||
| Michael Ceulemans et al. and 2020 [45] | Belgium | Cross-sectional (Web survey) | 2647 pregnant and 3823 breastfeeding women, n = 6470 |
| ||
| Anna Fuchs et al. and 2020 [46] | Poland | Cross-sectional | 764 sexually active female patients and above 18 years |
| ||
| James John Ashton et al. 2020 [34] | United Kingdom | Cross-sectional | 20 tertiaries pediatric IBD centers |
| ||
| Anja Saso, Helen Skirrow and Beate Kampmann and 2020 [47] | LMICs and HICs | Cross-sectional (Web survey) | n = 48 |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bolarinwa, O.A.; Ahinkorah, B.O.; Seidu, A.-A.; Ameyaw, E.K.; Saeed, B.Q.; Hagan, J.E., Jr.; Nwagbara, U.I. Mapping Evidence of Impacts of COVID-19 Outbreak on Sexual and Reproductive Health: A Scoping Review. Healthcare 2021, 9, 436. https://doi.org/10.3390/healthcare9040436
Bolarinwa OA, Ahinkorah BO, Seidu A-A, Ameyaw EK, Saeed BQ, Hagan JE Jr., Nwagbara UI. Mapping Evidence of Impacts of COVID-19 Outbreak on Sexual and Reproductive Health: A Scoping Review. Healthcare. 2021; 9(4):436. https://doi.org/10.3390/healthcare9040436
Chicago/Turabian StyleBolarinwa, Obasanjo Afolabi, Bright Opoku Ahinkorah, Abdul-Aziz Seidu, Edward Kwabena Ameyaw, Balsam Qubais Saeed, John Elvis Hagan, Jr., and Ugochinyere Ijeoma Nwagbara. 2021. "Mapping Evidence of Impacts of COVID-19 Outbreak on Sexual and Reproductive Health: A Scoping Review" Healthcare 9, no. 4: 436. https://doi.org/10.3390/healthcare9040436








