Short-Term Learning Effects of a Cardiopulmonary Resuscitation Program with Focus on the Relationship between Learning Effect and Trainees’ Perceived Competence
Abstract
:1. Introduction
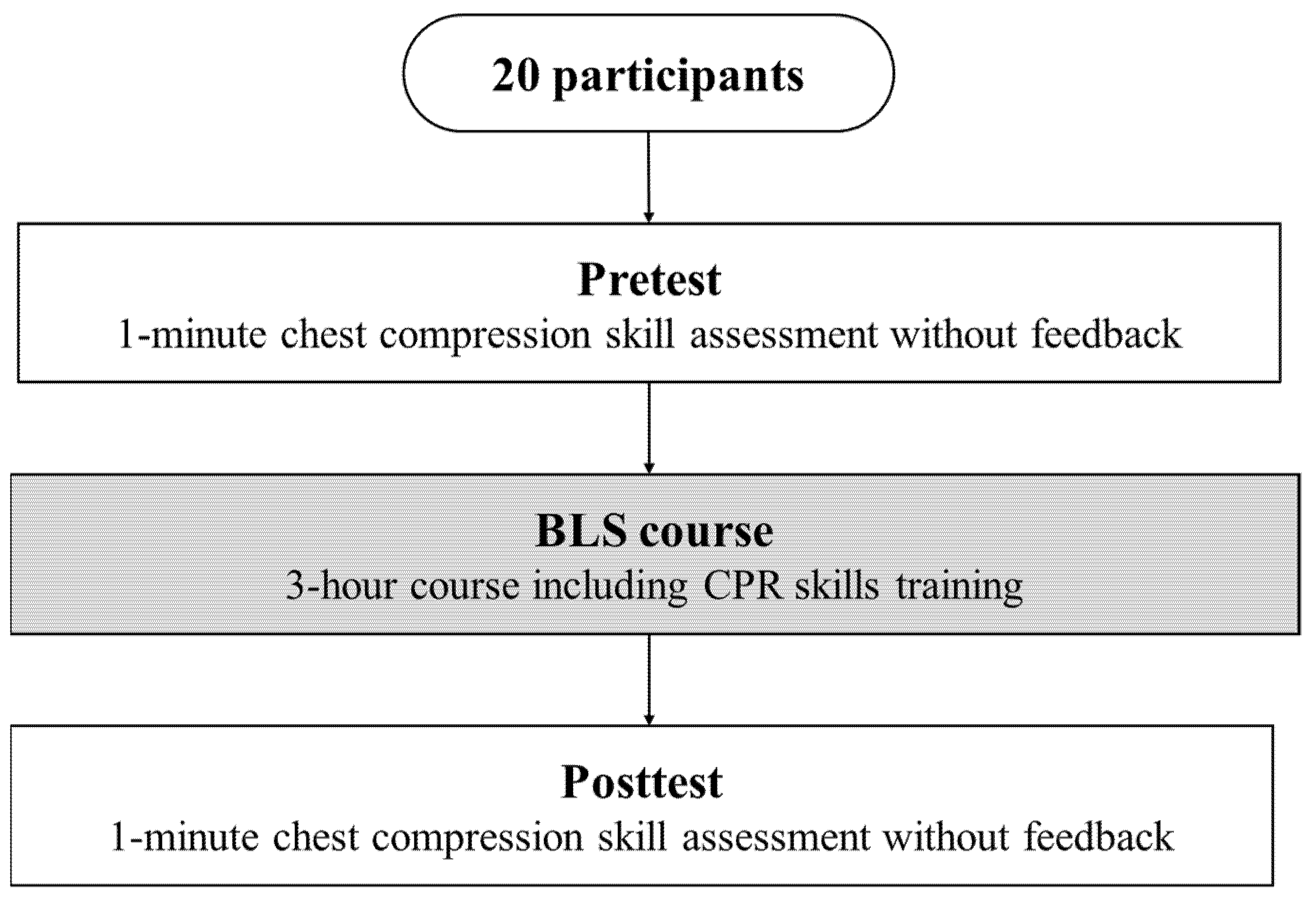
2. Materials and Methods
2.1. Study Design and Participants
2.2. Equipment and Measurement Outcome
2.3. Study Procedures
2.4. Outcomes
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nolan, J.P. High-quality cardiopulmonary resuscitation. Curr. Opin. Crit. Care 2014, 20, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Abella, B.S. High-quality cardiopulmonary resuscitation: Current and future directions. Curr. Opin. Crit. Care 2016, 22, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Wallace, S.K.; Abella, B.S.; Becker, L.B. Quantifying the effect of cardiopulmonary resuscitation quality on cardiac arrest outcome: A systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes 2013, 6, 148–156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talikowska, M.; Tohira, H.; Finn, J. Cardiopulmonary resuscitation quality and patient survival outcome in cardiac arrest: A systematic review and meta-analysis. Resuscitation 2015, 96, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Olasveengen, T.M.; Semeraro, F.; Ristagno, G.; Castren, M.; Handley, A.; Kuzovlev, A.; Monsieurs, K.G.; Raffay, V.; Smyth, M.; Soar, J.; et al. European Resuscitation Council Guidelines 2021: Basic Life Support. Resuscitation 2021, 161, 98–114. [Google Scholar] [CrossRef]
- Vadeboncoeur, T.; Stolz, U.; Panchal, A.; Silver, A.; Venuti, M.; Tobin, J.; Smith, G.; Nunez, M.; Karamooz, M.; Spaite, D.; et al. Chest compression depth and survival in out-of-hospital cardiac arrest. Resuscitation 2014, 85, 182–188. [Google Scholar] [CrossRef]
- Stiell, I.G.; Brown, S.P.; Christenson, J.; Cheskes, S.; Nichol, G.; Powell, J.; Bigham, B.; Morrison, L.J.; Larsen, J.; Hess, E.; et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit. Care Med. 2012, 40, 1192–1198. [Google Scholar] [CrossRef] [Green Version]
- Stiell, I.G.; Brown, S.P.; Nichol, G.; Cheskes, S.; Vaillancourt, C.; Callaway, C.W.; Morrison, L.J.; Christenson, J.; Aufderheide, T.P.; Davis, T.P.; et al. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation 2014, 130, 1962–1970. [Google Scholar] [CrossRef] [Green Version]
- Hellevuo, H.; Sainio, M.; Nevalainen, R.; Huhtala, H.; Olkkola, K.T.; Tenhunen, J.; Hoppu, S. Deeper chest compression–more complications for cardiac arrest patients? Resuscitation 2013, 84, 760–765. [Google Scholar] [CrossRef]
- Zuercher, M.; Hilwig, R.W.; Ranger-Moore, J.; Nysaether, J.; Nadkarni, V.M.; Berg, M.D.; Kern, K.B.; Sutton, R.; Berg, R.A. Leaning during chest compressions impairs cardiac output and left ventricular myocardial blood flow in piglet cardiac arrest. Crit. Care Med. 2010, 38, 1141–1146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Idris, A.H.; Guffey, D.; Aufderheide, T.P.; Brown, S.; Morrison, L.J.; Nichols, P.; Powell, J.; Daya, M.; Bigham, B.L.; Atkins, D.L.; et al. Relationship between chest compression rates and outcomes from cardiac arrest. Circulation 2012, 125, 3004–3012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kovács, E.; Jenei, Z.M.; Csordás, K.; Fritúz, G.; Hauser, B.; Gyarmathy, V.A.; Zima, E.; Gal, J. The timing of testing influences skill retention after basic life support training: A prospective quasi-experimental study. BMC Med. Educ. 2019, 19, 452. [Google Scholar] [CrossRef] [Green Version]
- Cortegiani, A.; Russotto, V.; Montalto, F.; Iozzo, P.; Meschis, R.; Pugliesi, M.; Mariano, D.; Benenati, V.; Raineri, S.M.; Gregoretti, C.; et al. Use of a real-time training software (Laerdal QCPR®) compared to instructor-based feedback for high-quality chest compressions acquisition in secondary school students: A randomized trial. PLoS ONE 2017, 12, e0169591. [Google Scholar] [CrossRef] [Green Version]
- Baldi, E.; Cornara, S.; Contri, E.; Epis, F.; Fina, D.; Zelaschi, B.; Dosenna, C.; Fichtner, F.; Tonani, M.; Maggio, M.D.; et al. Real-time visual feedback during training improves laypersons’ CPR quality: A randomized controlled manikin study. CJEM 2017, 19, 480–487. [Google Scholar] [CrossRef] [Green Version]
- Akizuki, K.; Yamamoto, R.; Yamaguchi, K.; Yabuki, J.; Ohashi, Y. The effects of feedback timing and frequency on the acquisition of cardiopulmonary resuscitation skills of health sciences undergraduate students: A 2 x 2 factorial quasi randomized study. PLoS ONE 2019, 14, e0220004. [Google Scholar] [CrossRef] [Green Version]
- Wutzler, A.; Bannehr, M.; von Ulmenstein, S.; Loehr, L.; Förster, J.; Kühnle, Y.; Finn, A.; Storm, C.; Haverkamp, W. Performance of chest compressions with the use of a new audio-visual feedback device: A randomized manikin study in health care professionals. Resuscitation 2015, 87, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Smereka, J.; Szarpak, L.; Czekajlo, M.; Abelson, A.; Zwolinski, P.; Plusa, T.; Dunder, D.; Dabrowski, M.; Weisneiwska, Z.; Robak, O.; et al. The TrueCPR device in the process of teaching cardiopulmonary resuscitation: A randomized simulation trial. Medicine (Baltimore) 2019, 98, e15995. [Google Scholar] [CrossRef]
- Gruenerbl, A.; Pirkl, G.; Monger, E.; Gobbi, M.; Lukowicz, P. Smart-watch life saver: Smart-watch interactive-feedback system for improving bystander CPR. In Proceedings of the 2015 ACM International Symposium on Wearable Computers, Osaka, Japan, 7–11 September 2015; pp. 19–26. [Google Scholar] [CrossRef]
- Ahn, C.; Lee, J.; Oh, J.; Song, Y.; Chee, Y.; Lim, T.H.; Kang, H.; Shin, H. Effectiveness of feedback with a smartwatch for high-quality chest compressions during adult cardiac arrest: A randomized controlled simulation study. PLoS ONE 2017, 12, e0169046. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Song, Y.; Oh, J.; Chee, Y.; Ahn, C.; Shin, H.; Kang, H.; Lim, T.H. Smartwatch feedback device for high-quality chest compressions by a single rescuer during infant cardiac arrest: A randomized, controlled simulation study. Eur J. Emerg. Med. 2019, 26, 266–271. [Google Scholar] [CrossRef]
- Wulf, G.; Lewthwaite, R. Optimizing performance through intrinsic motivation and attention for learning: The OPTIMAL theory of motor learning. Psychon Bull. Rev. 2016, 23, 1382–1414. [Google Scholar] [CrossRef] [PubMed]
- García, J.A.; Carcedo, R.J.; Castaño, J.L. The influence of feedback on competence, motivation, vitality, and performance in a throwing task. Res. Q Exerc. Sport 2019, 90, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Ghorbani, S. Motivational effects of enhancing expectancies and autonomy for motor learning: An examination of the OPTIMAL theory. J. Gen. Psychol. 2019, 46, 79–92. [Google Scholar] [CrossRef]
- Saemi, E.; Porter, J.M.; Ghotbi-Varzaneh, A.; Zarghami, M.; Maleki, F. Knowledge of results after relatively good trials enhances self-efficacy and motor learning. Psychol. Sport Exerc. 2012, 13, 378–382. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy—The Exercise of Control; WH Freeman & Co: New York, NY, USA, 1997. [Google Scholar]
- Deci, E.L.; Ryan, R.M. The" what" and" why" of goal pursuits: Human needs and the self-determination of behavior. Psychol. Inq. 2000, 11, 227–268. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Self-determination theory: A macrotheory of human motivation, development, and health. Can. Psychol. 2008, 49, 182–185. [Google Scholar] [CrossRef] [Green Version]
- Rodgers, W.M.; Markland, D.; Selzler, A.M.; Murray, T.C.; Wilson, P.M. Distinguishing perceived competence and self-efficacy: An example from exercise. Res. Q Exerc. Sport 2014, 85, 527–539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roh, Y.S.; Issenberg, S.B. Association of cardiopulmonary resuscitation psychomotor skills with knowledge and self-efficacy in nursing students. Int. J. Nurs. Pract. 2014, 20, 674–679. [Google Scholar] [CrossRef]
- Gonzi, G.; Sestigiani, F.; D’errico, A.; Vezzani, A.; Bonfanti, L.; Noto, G.; Artioli, G. Correlation between quality of cardiopulmonary resuscitation and self-efficacy measured during in-hospital cardiac arrest simulation; preliminary results. Acta. Biomed. 2015, 86, 40–45. [Google Scholar]
- Mac Giolla Phadraig, C.; Ho, J.D.; Guerin, S.; Yeoh, Y.L.; Mohamed Medhat, M.; Doody, K.; Hwang, S.; Hania, M.; Boggs, S.; Nolan, A.; et al. Neither basic life support knowledge nor self-efficacy are predictive of skills among dental students. Eur. J. Dent. Educ. 2017, 21, 187–192. [Google Scholar] [CrossRef] [PubMed]
- McAuley, E.; Duncan, T.; Tammen, V.V. Psychometric properties of the Intrinsic Motivation Inventory in a competitive sport setting: A confirmatory factor analysis. Res. Q. Exerc. Sport 1989, 60, 48–58. [Google Scholar] [CrossRef]
- Badami, R.; VaezMousavi, M.; Wulf, G.; Namazizadeh, M. Feedback after good versus poor trials affects intrinsic motivation. Res. Q. Exerc. Sport 2011, 82, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Abbas, Z.A.; North, J.S. Good-vs. poor-trial feedback in motor learning: The role of self-efficacy and intrinsic motivation across levels of task difficulty. Learn. Instr. 2018, 55, 105–112. [Google Scholar] [CrossRef] [Green Version]
- Japan Resuscitation Council. 2015 Japanese Guidelines for Emergency Care and Cardiopulmonary Resuscitation; Igaku-Shoin: Tokyo, Japan, 2016. [Google Scholar]
- Nishiyama, C.; Iwami, T.; Kawamura, T.; Ando, M.; Yonemoto, N.; Hiraide, A.; Nonogi, H. Quality of chest compressions during continuous CPR: Comparison between chest compression-only CPR and conventional CPR. Resuscitation 2010, 81, 1152–1155. [Google Scholar] [CrossRef] [PubMed]
- Yeung, J.; Meeks, R.; Edelson, D.; Gao, F.; Soar, J.; Perkins, G.D. The use of CPR feedback/prompt devices during training and CPR performance: A systematic review. Resuscitation 2009, 80, 743–751. [Google Scholar] [CrossRef] [Green Version]
- Partiprajak, S.; Thongpo, P. Retention of basic life support knowledge, self-efficacy and chest compression performance in Thai undergraduate nursing students. Nurse Educ. Pract. 2016, 16, 235–241. [Google Scholar] [CrossRef]
- Ro, Y.S.; Do Shin, S.; Song, K.J.; Hong, S.O.; Kim, Y.T.; Lee, D.W.; Cho, S. Public awareness and self-efficacy of cardiopulmonary resuscitation in communities and outcomes of out-of-hospital cardiac arrest: A multi-level analysis. Resuscitation 2016, 102, 17–24. [Google Scholar] [CrossRef]
- Magill, R.A.; Anderson, D.I. Motor Learning and Control, 12th ed.; McGraw Hill LLC: New York, NY, USA, 2021. [Google Scholar]
- Spooner, B.B.; Fallaha, J.F.; Kocierz, L.; Smith, C.M.; Smith, S.C.; Perkins, G.D. An evaluation of objective feedback in basic life support (BLS) training. Resuscitation 2007, 73, 417–424. [Google Scholar] [CrossRef]
- Brennan, E.E.; McGraw, R.C.; Brooks, S.C. Accuracy of instructor assessment of chest compression quality during simulated resuscitation. CJEM 2016, 18, 276–282. [Google Scholar] [CrossRef] [Green Version]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akizuki, K.; Koeda, H. Short-Term Learning Effects of a Cardiopulmonary Resuscitation Program with Focus on the Relationship between Learning Effect and Trainees’ Perceived Competence. Healthcare 2021, 9, 598. https://doi.org/10.3390/healthcare9050598
Akizuki K, Koeda H. Short-Term Learning Effects of a Cardiopulmonary Resuscitation Program with Focus on the Relationship between Learning Effect and Trainees’ Perceived Competence. Healthcare. 2021; 9(5):598. https://doi.org/10.3390/healthcare9050598
Chicago/Turabian StyleAkizuki, Kazunori, and Hideki Koeda. 2021. "Short-Term Learning Effects of a Cardiopulmonary Resuscitation Program with Focus on the Relationship between Learning Effect and Trainees’ Perceived Competence" Healthcare 9, no. 5: 598. https://doi.org/10.3390/healthcare9050598
APA StyleAkizuki, K., & Koeda, H. (2021). Short-Term Learning Effects of a Cardiopulmonary Resuscitation Program with Focus on the Relationship between Learning Effect and Trainees’ Perceived Competence. Healthcare, 9(5), 598. https://doi.org/10.3390/healthcare9050598





