Discovery of Association Rules Patterns and Prevalence of Comorbidities in Adult Patients Hospitalized with Mental and Behavioral Disorders
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Dataset
2.2. Study Papulation
2.3. Principal Diagnosis and Comorbidities
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Papulation
3.2. Distribution and Frequent of Comorbidities
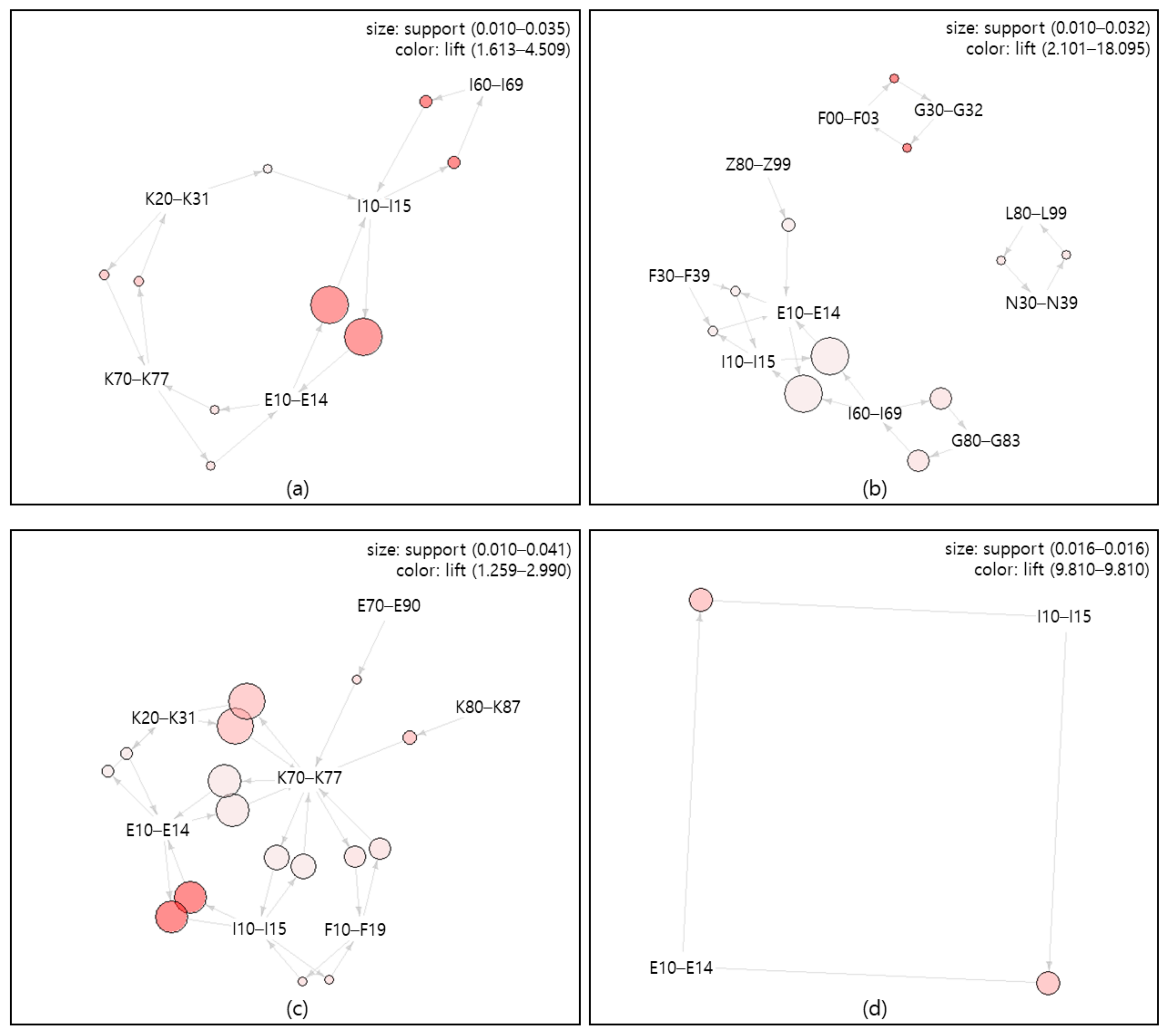
3.3. Association Rules among Comorbidities
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Mental Health. Available online: https://www.who.int/health-topics/mental-health#tab=tab_2 (accessed on 14 March 2021).
- World Health Organization. Mental Health in the Western Pacific. Available online: https://www.who.int/westernpacific/health-topics/mental-health (accessed on 14 March 2021).
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines; World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]
- Ministry of Culture, Sports and Tourism. The Survey of Mental Disorders in Korea. Available online: https://www.korea.kr/archive/expDocView.do?docId=37547 (accessed on 15 March 2021).
- Jeon, J.A. Current Status and Policy Tasks of Comorbidity. Available online: https://webcache.googleusercontent.com/search?q=cache:T4BKmtH1fXgJ:https://www.kihasa.re.kr/common/filedown.do%3Fseq%3D32867+&cd=1&hl=ko&ct=clnk&gl=kr (accessed on 15 March 2021).
- Ronaldson, A.; Elton, L.; Jayakumar, S.; Jieman, A.; Halvorsrud, K.; Bhui, K. Severe Mental Illness and Health Service Utilisation for Nonpsychiatric Medical Disorders: A Systematic Review and Meta-analysis. PLoS Med. 2020, 17, e1003284. [Google Scholar] [CrossRef]
- Kim, J.; Chae, J.-H. Strategies for Reducing Mental Disorder Treatment Gap in Korea. J. Korean Neuropsychiatr. Assoc. 2020, 59, 208–214. [Google Scholar] [CrossRef]
- Janssen, E.M.; McGinty, E.E.; Azrin, S.T.; Juliano-Bult, D.; Daumit, G.L. Review of the Evidence: Prevalence of Medical Conditions in the United States Population with Serious Mental Illness. Gen. Hosp. Psychiatry 2015, 37, 199–222. [Google Scholar] [CrossRef] [PubMed]
- Cabassa, L.J.; Humensky, J.; Druss, B.; Lewis-Fernández, R.; Gomes, A.P.; Wang, S.; Blanco, C. Do Race, Ethnicity, and Psychiatric Diagnoses Matter in the Prevalence of Multiple Chronic Medical Conditions? Med. Care 2013, 51, 540–547. [Google Scholar] [CrossRef] [PubMed]
- Scott, K.M.; Lim, C.; Al-Hamzawi, A.; Alonso, J.; Bruffaerts, R.; Caldas-de-Almeida, J.M.; Florescu, S.; de Girolamo, G.; Hu, C.; de Jonge, P.; et al. Association of Mental Disorders With Subsequent Chronic Physical Conditions: World Mental Health Surveys From 17 Countries. JAMA Psychiatry 2016, 73, 150–158. [Google Scholar] [CrossRef]
- Van Oudheusden, L.J.B.; Meynen, G.; van Balkom, A.J.L.M. Psychiatric Comorbidity: Theoretical and Clinical Dilemmas. Tijdschr. Psychiatr. 2015, 57, 664–671. [Google Scholar]
- World Health Organization. Depression and Other Common Mental Disorders. Available online: https://www.who.int/mental_health/management/depression/prevalence_global_health_estimates/en/ (accessed on 15 March 2021).
- Feng, J.; Mu, X.-M.; Ma, L.-L.; Wang, W. Comorbidity Patterns of Older Lung Cancer Patients in Northeast China: An Association Rules Analysis Based on Electronic Medical Records. Int. J. Environ. Res. Public Health 2020, 17, 9119. [Google Scholar] [CrossRef] [PubMed]
- Lakshmi, K.S.; Vadivu, G. A Novel Approach for Disease Comorbidity Prediction Using Weighted Association Rule Mining. J. Ambient Intell. Human Comput. 2019. [Google Scholar] [CrossRef]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial Intelligence in Healthcare: Past, Present and Future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef]
- Hahsler, M. arulesViz: Interactive Visualization of Association Rules with R. R J. 2017, 9, 163. [Google Scholar] [CrossRef]
- Kim, S.-S. A Study on Database Construction for Efficient Utilization of Korean National Hospital Discharge In-depth Injury Survey Data. J. Health Inform. Stat. 2020, 45, 44–51. [Google Scholar] [CrossRef]
- KCDC. Korean National Hospital Discharge In-Depth Injury Survey Guidebook; Korea Centers for Disease Control & Prevention: Cheongju, Korea, 2016.
- Aiello, F.A.; Roddy, S.P. Inpatient coding and the diagnosis-related group. J. Vasc. Surg. 2017, 66, 1621–1623. [Google Scholar] [CrossRef] [PubMed]
- Sukanya, C. Validity of Principal Diagnoses in Discharge Summaries and ICD-10 Coding Assessments Based on National Health Data of Thailand. Health Inform. Res. 2017, 23, 293–303. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kim, S.-S. Analysis of Variation of Length of Stay According to Comorbidities in Cancer Inpatient. J. Health Inform. Stat. 2020, 45, 80–90. [Google Scholar] [CrossRef]
- Tammemagi, C.M.; Neslund-Dudas, C.; Simoff, M.; Kvale, P. Impact of Comorbidity on Lung Cancer Survival. Int. J. Cancer 2003, 103, 792–802. [Google Scholar] [CrossRef]
- Ngene, N.C.; Moodley, J. Assigning Appropriate and Comprehensive Diagnosis for Scientific Report. Med. Hypotheses 2014, 83, 681–684. [Google Scholar] [CrossRef] [PubMed]
- Alonso, S.G.; de la Torre-Díez, I.; Hamrioui, S.; López-Coronado, M.; Barreno, D.C.; Nozaleda, L.M.; Franco, M. Data Mining Algorithms and Techniques in Mental Health: A Systematic Review. J. Med. Syst. 2018, 42, 161. [Google Scholar] [CrossRef]
- Thitithamawat, S.; Chertchom, P.; Buraphawichit, P.; Thothong, T. Association rules to analyze hospital resources with mortality rates. In Proceedings of the 2018 5th International Conference on Business and Industrial Research (ICBIR), Bangkok, Thailand, 17–18 May 2018; pp. 51–56. [Google Scholar]
- Abdel-Basset, M.; Mohamed, M.; Smarandache, F.; Chang, V. Neutrosophic Association Rule Mining Algorithm for Big Data Analysis. Symmetry 2018, 10, 106. [Google Scholar] [CrossRef]
- Hernández, B.; Reilly, R.B.; Kenny, R.A. Investigation of Multimorbidity and Prevalent Disease Combinations in Older Irish Adults Using Network Analysis and Association Rules. Sci. Rep. 2019, 9, 14567. [Google Scholar] [CrossRef]
- Kim, S.; An, Y.; Lee, K.; Jung, S.; Cho, W. Using Association Analysis to Find Diseases Related to Childhood Obesity. In Proceedings of the 2017 Ninth International Conference on Ubiquitous and Future Networks (ICUFN), Milan, Italy, 4–7 July 2017; pp. 847–850. [Google Scholar]
- Scott, K.M.; Oakley Browne, M.A.; McGee, M.A.; Elisabeth Wells, J. Mental-Physical Comorbidity in Te Rau Hinengaro: The New Zealand Mental Health Survey. Aust. N. Z. J. Psychiatry 2006, 40, 882–888. [Google Scholar] [CrossRef]
- Seo, E.-W.; Choi, S.; Lee, K.-S. The Differences of Outpatient Service Uses by Depression: Focusing on the Hypertension and/or Diabetes Patients. J. Korean Public Health Assoc. 2017, 43, 21–34. [Google Scholar]
- Joo, Y.H. Surgical Comorbidity in Schizophrenia. Available online: http://www.kisep.com/data1/3/htm/200109.htm (accessed on 14 March 2021).
- Brink, M.; Green, A.; Bojesen, A.B.; Lamberti, J.S.; Conwell, Y.; Andersen, K. Excess Medical Comorbidity and Mortality across the Lifespan in Schizophrenia: A Nationwide Danish Register Study. Schizophr. Res. 2019, 206, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Ee, C.; Lake, J.; Firth, J.; Hargraves, F.; de Manincor, M.; Meade, T.; Marx, W.; Sarris, J. An Integrative Collaborative Care Model for People with Mental Illness and Physical Comorbidities. Inter. J. Ment. Health Syst. 2020, 14, 83. [Google Scholar] [CrossRef]
- Wang, C.-H.; Lee, T.-Y.; Hui, K.-C.; Chung, M.-H. Mental disorders and medical comorbidities: Association rule mining approach. Perspect. Psychiatr. Care 2019, 55, 517–526. [Google Scholar] [CrossRef]
- Government of the United Kingdom. Dementia: Comorbidities in Patients—Data Briefing. Available online: https://www.gov.uk/government/publications/dementia-comorbidities-in-patients/dementia-comorbidities-in-patients-data-briefing (accessed on 14 March 2021).
- Alcohol and Drug Support Line. Alcohol and the Digestive System. Available online: https://alcoholthinkagain.com.au/alcohol-your-health/alcohol-and-long-term-health/alcohol-and-the-digestive-system/ (accessed on 14 March 2021).
- Gabilondo, A.; Alonso-Moran, E.; Nuño-Solinis, R.; Orueta, J.F.; Iruin, A. Comorbidities with Chronic Physical Conditions and Gender Profiles of Illness in Schizophrenia. Results from PREST, a New Health Dataset. J. Psychosom. Res. 2017, 93, 102–109. [Google Scholar] [CrossRef]
- Pan, Y.; Cai, W.; Cheng, Q.; Dong, W.; An, T.; Yan, J. Association between Anxiety and Hypertension: A Systematic Review and meta-analysis of epidemiological studies. Neuropsychiatr. Dis. Treat. 2015, 11, 1121–1130. [Google Scholar] [CrossRef]
- Grigsby, A.B.; Anderson, R.J.; Freedland, K.E.; Clouse, R.E.; Lustman, P.J. Prevalence of anxiety in adults with diabetes: A sysTematic Review. J. Psychosom. Res. 2002, 53, 1053–1060. [Google Scholar] [CrossRef]
- Choi, W.J.; Lee, B.W.; Kim, D.W.; Lee, H.; Lee, S.; Oh, S.T.; Kim, W.J.; Park, J.Y. Current Status and Characteristics of Sleep Disorders and Associated Diseases: National Health Insurance Data. Available online: https://www.nhimc.or.kr/lab/project/sub03_012015.do (accessed on 16 March 2021).
- Parmar, A.; Kaloiya, G. Comorbidity of Personality Disorder among Substance Use Disorder Patients: A Narrative Review. Indian J. Psychol. Med. 2018, 40, 517–527. [Google Scholar] [CrossRef]

| Variable | Comorbid Disease | Total | x2 or t | p | |
|---|---|---|---|---|---|
| With | Without | ||||
| Sex | 3.342 | 0.068 | |||
| Male | 5545 (62.69) | 3300 (37.31) | 8845 (42.75) | ||
| Female | 7278 (61.44) | 4567 (38.56) | 11,845 (57.25) | ||
| Age (year) | 51.19 ± 1.88 | 43.57 ± 16.29 | 48.29 ± 17.69 | −31.434 | <0.001 |
| Age group | 830.972 | <0.001 | |||
| 19–44 | 4836 (52.34) | 4403 (47.66) | 9239 (44.65) | ||
| 45–64 | 4607 (65.08) | 2472 (34.92) | 7079 (34.21) | ||
| 65–74 | 1856 (76.38) | 574 (23.62) | 2430 (11.74) | ||
| ≥75 | 1524 (78.48) | 418 (21.52) | 1942 (9.39) | ||
| Insurance type | 14.299 | 0.003 | |||
| National health | 10,116 (61.38) | 6364 (38.62) | 16,480 (79.65) | ||
| Medicaid I | 1972 (64.23) | 1098 (35.77) | 3070 (14.84) | ||
| Medicaid II | 311 (62.08) | 190 (37.92) | 501 (2.42) | ||
| Others | 424 (66.35) | 215 (33.65) | 639 (3.09) | ||
| Admission route | 0.725 | 0.696 | |||
| Emergency | 4227 (62.27) | 2561 (37.73) | 6788 (32.81) | ||
| Outpatient | 8589 (61.84) | 5300 (38.16) | 13,889 (67.13) | ||
| Others | 7 (53.85) | 6 (46.15) | 13 (0.06) | ||
| Treatment outcome | 89.196 | <0.001 | |||
| Improved | 11,706 (62.46) | 7037 (37.54) | 18,743 (90.59) | ||
| Not improved | 973 (54.79) | 803 (45.21) | 1776 (8.58) | ||
| Death | 105 (93.75) | 7 (6.25) | 112 (0.54) | ||
| Others | 39 (66.10) | 20 (33.90) | 59 (0.29) | ||
| LOS(day) | 37.72 ± 132.55 | 32.59 ± 147.63 | 35.77 ± 138.50 | −2.522 | 0.012 |
| No. of comorbidity | 2.30 ± 1.71 | - | 1.42 ± 1.74 | N/A | N/A |
| Bed size | 90.503 | <0.001 | |||
| 100–299 | 3174 (66.15) | 1624 (33.85) | 4798 (23.19) | ||
| 300–499 | 1609 (60.58) | 1047 (39.42) | 2656 (12.84) | ||
| 500–999 | 6273 (62.32) | 3793 (37.68) | 10,066 (48.65) | ||
| ≥1000 | 1767 (55.74) | 1403 (44.26) | 3170 (15.32) | ||
| Total | 12,823 (61.98) | 7867 (38.02) | 20,690 (100) | ||
| ICD-10 | Principal Diagnosis | Comorbid Disease | Total | x2 | p | |
|---|---|---|---|---|---|---|
| With | Without | |||||
| F00–F03 | Dementia | 1124 (82.59) | 237 (17.41) | 1361 (6.58) | 958.193 | <0.001 |
| F10–F19 | Mental and behavioral disorders due to psychoactive substance use | 2401 (69.45) | 1056 (30.55) | 3457 (16.71) | ||
| F20–F29 | Schizophrenia, schizotypal and delusional disorders | 2073 (45.67) | 2466 (54.33) | 4539 (21.94) | ||
| F30–F39 | Mood (affective) disorders | 3930 (59.83) | 2639 (40.17) | 6569 (31.75) | ||
| F40–F48 | Neurotic, stress-related and somatoform disorders | 2919 (69.35) | 1290 (30.65) | 4209 (20.34) | ||
| F50–F59 | Behavioral syndromes associated with physiological disturbances and physical factors | 212 (69.51) | 93 (30.49) | 305 (1.47) | ||
| F60–F69 | Disorders of adult personality and behavior | 164 (65.60) | 86 (34.40) | 250 (1.21) | ||
| Total | 12,823 (61.98) | 7867 (38.02) | 20,690 (100) | |||
| ICD-10 | Comorbid Disease | N | % |
|---|---|---|---|
| I10–I15 | Hypertensive diseases | 2289 | 11.06 |
| F30–F39 | Mood (affective) disorders | 1725 | 8.34 |
| E10–E14 | Diabetes mellitus | 1651 | 7.98 |
| K20–K31 | Diseases of esophagus, stomach and duodenum | 1456 | 7.04 |
| F40–F48 | Neurotic, stress-related and somatoform disorders | 1383 | 6.68 |
| F00–F03 | Dementia | 1361 | 6.58 |
| K70–K77 | Diseases of liver | 1098 | 5.31 |
| G40–G47 | Episodic and paroxysmal disorders | 797 | 3.85 |
| F10–F19 | Mental and behavioral disorders due to psychoactive substance use | 662 | 3.20 |
| E70–E90 | Metabolic disorders | 590 | 2.85 |
| F20–F29 | Schizophrenia, schizotypal and delusional disorders | 575 | 2.78 |
| K55–K64 | Other diseases of intestines | 552 | 2.67 |
| I60–I69 | Cerebrovascular diseases | 540 | 2.61 |
| F60–F69 | Disorders of adult personality and behavior | 523 | 2.53 |
| M40–M54 | Dorsopathies | 520 | 2.51 |
| Z80–Z99 | Persons with potential health hazards related to family and personal history and certain conditions influencing health status | 503 | 2.43 |
| L20–L30 | Dermatitis and eczema | 423 | 2.04 |
| R50–R69 | General symptoms and signs | 398 | 1.92 |
| M60–M79 | Soft tissue disorders | 358 | 1.73 |
| M00–M25 | Arthropathies | 344 | 1.66 |
| N30–N39 | Other diseases of the urinary system | 340 | 1.64 |
| F50–F59 | Behavioral syndromes associated with physiological disturbances and physical factors | 329 | 1.59 |
| E00–E07 | Disorders of thyroid gland | 316 | 1.53 |
| J00–J06 | Acute upper respiratory infections | 314 | 1.52 |
| I30–I52 | Other forms of heart disease | 271 | 1.31 |
| B35–B49 | Mycoses | 265 | 1.28 |
| K00–K14 | Diseases of oral cavity, salivary glands and jaws | 263 | 1.27 |
| G20–G26 | Extrapyramidal and movement disorders | 262 | 1.27 |
| J40–J47 | Chronic lower respiratory diseases | 254 | 1.23 |
| M80–M94 | Osteopathies and chondropathies | 238 | 1.15 |
| I20–I25 | Ischemic heart diseases | 236 | 1.14 |
| L80–L99 | Other disorders of the skin and subcutaneous tissue | 227 | 1.10 |
| N40–N51 | Diseases of male genital organs | 219 | 1.06 |
| J09–J18 | Influenza and pneumonia | 211 | 1.02 |
| J30–J39 | Other diseases of upper respiratory tract | 208 | 1.01 |
| Rules | No. of Patients | Support | Confidence | Lift | IS Scale |
|---|---|---|---|---|---|
| Mental and behavioral disorders(F00–F69) with comorbid diseases (n = 20,690) | |||||
| E10–E14 → I10–I15 | 585 | 0.035 | 0.433 | 4.203 | 0.386 |
| I10–I15 → E10–E14 | 585 | 0.035 | 0.345 | 4.203 | 0.386 |
| I10–I15 → I60–I69 | 210 | 0.013 | 0.124 | 4.509 | 0.240 |
| I60–I69 → I10–I15 | 210 | 0.013 | 0.465 | 4.509 | 0.240 |
| K70–K77 → K20–K31 | 183 | 0.011 | 0.180 | 2.974 | 0.182 |
| K20–K31 → K70–K77 | 183 | 0.011 | 0.183 | 2.974 | 0.182 |
| K70–K77 → E10–E14 | 168 | 0.010 | 0.166 | 2.019 | 0.143 |
| E10–E14 → K70–K77 | 168 | 0.010 | 0.124 | 2.019 | 0.143 |
| K20–K31 → I10–I15 | 166 | 0.010 | 0.166 | 1.613 | 0.127 |
| F00–F03 with comorbid diseases (n = 1361) | |||||
| E10–E14 → I10–I15 | 152 | 0.112 | 0.639 | 1.994 | 0.472 |
| I10–I15 → E10–E14 | 152 | 0.112 | 0.349 | 1.994 | 0.472 |
| F00–F03 → G30–G32 | 14 | 0.010 | 0.519 | 18.095 | 0.431 |
| G30–G32 → F00–F03 | 14 | 0.010 | 0.359 | 18.095 | 0.431 |
| I60–I69 → I10–I15 | 118 | 0.087 | 0.442 | 1.380 | 0.346 |
| I10–I15 → I60–I69 | 118 | 0.087 | 0.271 | 1.380 | 0.346 |
| F10–F19 with comorbid diseases (n = 3457) | |||||
| I10–I15 → E10–E14 | 124 | 0.036 | 0.097 | 2.990 | 0.327 |
| E10–E14 → I10–I15 | 124 | 0.036 | 0.124 | 2.990 | 0.327 |
| K20–K31 → K70–K77 | 143 | 0.041 | 0.089 | 2.032 | 0.290 |
| K70–K77 → K20–K31 | 143 | 0.041 | 0.229 | 2.032 | 0.290 |
| E10–E14 → K70–K77 | 129 | 0.037 | 0.124 | 1.319 | 0.222 |
| F20–F29 with comorbid diseases (n = 4539) | |||||
| I10–I15 → E10–E14 | 74 | 0.016 | 0.035 | 9.810 | 0.400 |
| E10–E14 → I10–I15 | 74 | 0.016 | 0.047 | 9.810 | 0.400 |
| F30–F39 with comorbid diseases (n = 6569) | |||||
| Z80–Z99 → I10–I15 | 67 | 0.010 | 0.032 | 2.881 | 0.171 |
| K20–K31 → I10–I15 | 93 | 0.014 | 0.066 | 1.917 | 0.165 |
| I10–I15 → K20–K31 | 93 | 0.014 | 0.111 | 1.917 | 0.165 |
| F40–F48 → I10–I15 | 76 | 0.012 | 0.095 | 1.098 | 0.113 |
| I10–I15 → F40–F48 | 76 | 0.012 | 0.111 | 1.098 | 0.113 |
| F40–F48 with comorbid diseases (n = 4209) | |||||
| E10–E14 → I10–I15 | 159 | 0.038 | 0.071 | 3.775 | 0.378 |
| I10–I15 → E10–E14 | 159 | 0.038 | 0.140 | 3.775 | 0.378 |
| E70–E90 → I10–I15 | 72 | 0.017 | 0.039 | 3.127 | 0.231 |
| I10–I15 → E70–E90 | 72 | 0.017 | 0.140 | 3.127 | 0.231 |
| K20–K31 → I10–I15 | 102 | 0.024 | 0.109 | 1.590 | 0.196 |
| F50–F59 with comorbid diseases (n = 305) | |||||
| E10–E14, I10–I15 → I60–I69 | 4 | 0.013 | 0.023 | 24.898 | 0.571 |
| F40–F48, K20–K31 → K55–K64 | 5 | 0.016 | 0.023 | 16.758 | 0.524 |
| I10–I15, I60–I69 → E10–E14 | 4 | 0.013 | 0.016 | 15.250 | 0.447 |
| F40–F48, K55–K64 → K20–K31 | 5 | 0.016 | 0.016 | 10.517 | 0.415 |
| K20–K31, K55–K64 → F40–F48 | 5 | 0.016 | 0.020 | 9.776 | 0.400 |
| F60–F69 with comorbid diseases (n = 250) | |||||
| F10–F19 → F50–F59 | 3 | 0.012 | 0.060 | 6.250 | 0.274 |
| F50–F59 → F10–F19 | 3 | 0.012 | 0.032 | 6.250 | 0.274 |
| F30–F39 → F60–F69 | 7 | 0.028 | 0.276 | 1.951 | 0.234 |
| F60–F69 → F30–F39 | 7 | 0.028 | 0.052 | 1.951 | 0.234 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cha, S.; Kim, S.-S. Discovery of Association Rules Patterns and Prevalence of Comorbidities in Adult Patients Hospitalized with Mental and Behavioral Disorders. Healthcare 2021, 9, 636. https://doi.org/10.3390/healthcare9060636
Cha S, Kim S-S. Discovery of Association Rules Patterns and Prevalence of Comorbidities in Adult Patients Hospitalized with Mental and Behavioral Disorders. Healthcare. 2021; 9(6):636. https://doi.org/10.3390/healthcare9060636
Chicago/Turabian StyleCha, Sunkyung, and Sung-Soo Kim. 2021. "Discovery of Association Rules Patterns and Prevalence of Comorbidities in Adult Patients Hospitalized with Mental and Behavioral Disorders" Healthcare 9, no. 6: 636. https://doi.org/10.3390/healthcare9060636
APA StyleCha, S., & Kim, S.-S. (2021). Discovery of Association Rules Patterns and Prevalence of Comorbidities in Adult Patients Hospitalized with Mental and Behavioral Disorders. Healthcare, 9(6), 636. https://doi.org/10.3390/healthcare9060636






