Prevalence, New Incidence, Course, and Risk Factors of PTSD, Depression, Anxiety, and Panic Disorder during the Covid-19 Pandemic in 11 Countries
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Procedure and Measures
2.3. Statistical Analysis
3. Results
3.1. Sample Description
3.2. Prevalence and Incidence of PTSD, Anxiety, Depression and Panic Disorder
3.3. Course of PTSD, Anxiety, Depression, and Panic Disorder
3.4. Associated Factors with PTSD, Anxiety, Depression, and Panic Disorder
3.4.1. Factors Associated with PTSD
3.4.2. Factors Associated with Anxiety
3.4.3. Factors Associated with Depression
3.4.4. Factors Associated with Panic Disorder
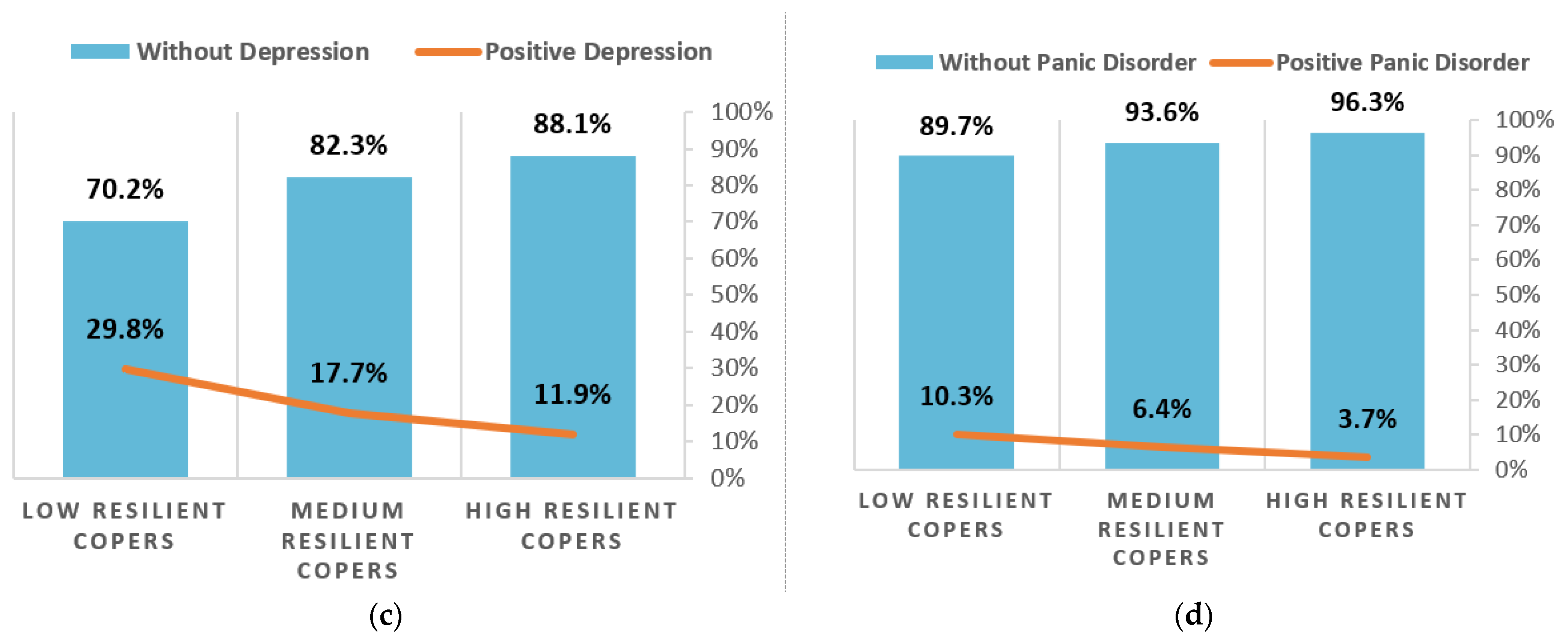
3.5. Resilience and PTSD, Anxiety, Depression, and Panic Disorder
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UN Chief Says COVID-19 is Worst Crisis Since World War II. Available online: https://apnews.com/article/asia-pacific-united-nations-virus-outbreak-financial-markets-us-news-dd1b9502802f03f88d56c34f7d95270c (accessed on 2 June 2021).
- Seddighi, H. COVID-19 as a natural disaster: Focusing on exposure and vulnerability for response. Disaster Med. Public Health Prep. 2020, 14, e42–e43. [Google Scholar] [CrossRef]
- Bromet, E. Psychiatric Problems Related to Natural and Human-Made Disasters. In Contemporary Psychiatry; Springer: Berlin/Heidelberg, Germany, 2001; pp. 1015–1025. [Google Scholar] [CrossRef]
- Galea, S.; Nandi, A.; Vlahov, D. The Epidemiology of Post-Traumatic Stress Disorder after Disasters. Epidemiol. Rev. 2005, 27, 78–91. [Google Scholar] [CrossRef] [Green Version]
- Berenz, E.C.; York, T.P.; Bing-Canar, H.; Amstadter, A.B.; Mezuk, B.; Gardner, C.O.; Roberson-Nay, R. Time course of panic disorder and posttraumatic stress disorder onsets. Soc. Psychiatry Psychiatr. Epidemiol. 2019, 54, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, H.; Roser, M. “Mental Health”, Published online at OurWorldInData.org. 2018. Available online: https://ourworldindata.org/mental-health (accessed on 15 April 2021).
- Javelot, H.; Weiner, L. Panic and pandemic: Narrative review of the literature on the links and risks of panic disorder as a consequence of the SARS-CoV-2 pandemic. Lencephale 2021, 47, 38–42. [Google Scholar] [CrossRef]
- De Boni, R.B.; Balanzá-Martínez, V.; Mota, J.C.; Cardoso, T.D.A.; Ballester, P.; Atienza-Carbonell, B.; Bastos, F.I.; Kapczinski, F. Depression, Anxiety, and Lifestyle Among Essential Workers: A Web Survey From Brazil and Spain During the COVID-19 Pandemic. J. Med. Internet Res. 2020, 22, e22835. [Google Scholar] [CrossRef]
- Alzueta, E.; Perrin, P.; Baker, F.C.; Caffarra, S.; Ramos-Usuga, D.; Yuksel, D.; Arang-Lasprilla, J.C. How the COVID-19 pandemic has changed our lives: A study of psychological correlates across 59 countries. J. Clin. Psychol. 2021, 77. [Google Scholar] [CrossRef] [PubMed]
- Barzilay, R.; Moore, T.M.; Greenberg, D.M.; DiDomenico, G.E.; Brown, L.A.; White, L.K.; Gur, R.C.; Gur, R.E. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl. Psychiatry 2020, 10, 1–8. [Google Scholar] [CrossRef]
- Cénat, J.M.; Dalexis, R.D.; Guerrier, M.; Noorishad, P.-G.; Derivois, D.; Bukaka, J.; Birangui, J.-P.; Adansikou, K.; Clorméus, L.A.; Kokou-Kpolou, C.K. Frequency and correlates of anxiety symptoms during the COVID-19 pandemic in low-and middle-income countries: A multinational study. J. Psychiatr. Res. 2021, 132, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Cénat, J.M.; Noorishad, P.-G.; Kokou-Kpolou, C.K.; Dalexis, R.D.; Hajizadeh, S.; Guerrier, M.; Clorméus, L.A.; Bukaka, J.; Birangui, J.-P.; Adansikou, K. Prevalence and correlates of depression during the COVID-19 pandemic and the major role of stigmatization in low-and middle-income countries: A multinational cross-sectional study. Psychiatry Res. 2021, 297, 113714. [Google Scholar] [CrossRef]
- Shah, S.M.A.; Mohammad, D.; Qureshi, M.F.H.; Abbas, M.Z.; Aleem, S. Prevalence, Psychological Responses and Associated Correlates of Depression, Anxiety and Stress in a Global Population, During the Coronavirus Disease (COVID-19) Pandemic. Community Ment. Health J. 2021, 57, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Arafa, A.; Mohammed, Z.; Mahmoud, O.; Elshazley, M.; Ewis, A. Depressed, anxious, and stressed: What have healthcare workers on the frontlines in Egypt and Saudi Arabia experienced during the COVID-19 pandemic? J. Affect. Disord. 2021, 278, 365–371. [Google Scholar] [CrossRef]
- Sigurvinsdottir, R.; Thorisdottir, I.E.; Gylfason, H.F. The impact of COVID-19 on mental health: The role of locus on control and internet use. Int. J. Environ. Res. Public Health 2020, 17, 6985. [Google Scholar] [CrossRef] [PubMed]
- Cag, Y.; Erdem, H.; Gormez, A.; Ankarali, H.; Hargreaves, S.; Ferreira-Coimbra, J.; Rubulotta, F.; Belliato, M.; Berger-Estilita, J.; Pelosi, P. Anxiety among front-line health-care workers supporting patients with COVID-19: A global survey. Gen. Hosp. Psychiatry 2021, 68, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Codagnone, C.; Bogliacino, F.; Gómez, C.; Charris, R.; Montealegre, F.; Liva, G.; Lupiáñez-Villanueva, F.; Folkvord, F.; Veltri, G.A. Assessing concerns for the economic consequence of the COVID-19 response and mental health problems associated with economic vulnerability and negative economic shock in Italy, Spain, and the United Kingdom. PLoS ONE 2020, 15, e0240876. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, E.W.; Beyl, R.A.; Fearnbach, S.N.; Altazan, A.D.; Martin, C.K.; Redman, L.M. The impact of COVID-19 stay-at-home orders on health behaviors in adults. Obesity 2021, 29, 438–445. [Google Scholar] [CrossRef]
- Nelson, B.W.; Pettitt, A.; Flannery, J.E.; Allen, N.B. Rapid assessment of psychological and epidemiological correlates of COVID-19 concern, financial strain, and health-related behavior change in a large online sample. PLoS ONE 2020, 15, e0241990. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, H.; Kim, J.E.; Moon, S.J.; Nam, E.W. Analysis of personal and national factors that influence depression in individuals during the COVID-19 pandemic: A web-based cross-sectional survey. Glob. Health 2021, 17, 1–12. [Google Scholar] [CrossRef]
- Islam, M.S.; Ferdous, M.Z.; Potenza, M.N. Panic and generalized anxiety during the COVID-19 pandemic among Bangladeshi people: An online pilot survey early in the outbreak. J. Affect. Disord. 2020, 276, 30–37. [Google Scholar] [CrossRef]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.-G.; Mukunzi, J.N.; McIntee, S.-E.; Dalexis, R.D.; Goulet, M.-A.; Labelle, P. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef]
- Lechat, M.F. Disasters and public health. Bull. World Health Organ. 1979, 57, 11. [Google Scholar] [PubMed]
- Georgieva, I.; Lantta, T.; Lickiewicz, J.; Pekara, J.; Wikman, S.; Loseviča, M.; B N, R.; Mihai, A.; Lepping, P. Perceived Effectiveness, Restrictiveness and Compliance with Containment Measures Against the Covid-19 Pandemic: An International Comparative Study in 11 Countries. Int. J. Environ. Res. Public Health 2021, 18, 3806. [Google Scholar] [CrossRef]
- Morina, N.; Kip, A.; Hoppen, T.H.; Priebe, S.; Meyer, T. Potential impact of physical distancing on physical and mental health: A rapid narrative umbrella review of meta-analyses on the link between social connection and health. BMJ Open 2021, 11, e042335. [Google Scholar] [CrossRef] [PubMed]
- Prins, A.; Bovin, M.J.; Smolenski, D.J.; Marx, B.P.; Kimerling, R.; Jenkins-Guarnieri, M.A.; Kaloupek, D.G.; Schnurr, P.P.; Kaiser, A.P.; Leyva, Y.E. The primary care PTSD screen for DSM-5 (PC-PTSD-5): Development and evaluation within a veteran primary care sample. J. Gen. Intern. Med. 2016, 31, 1206–1211. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef]
- Forsell, E.; Kraepelien, M.; Blom, K.; Isacsson, N.; Jernelöv, S.; Svanborg, C.; Rosén, A.; Kaldo, V. Development of a very brief scale for detecting and measuring panic disorder using two items from the Panic Disorder Severity Scale-Self report. J. Affect. Disord. 2019, 257, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Arroll, B.; Goodyear-Smith, F.; Crengle, S.; Gunn, J.; Kerse, N.; Fishman, T.; Falloon, K.; Hatcher, S. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann. Fam. Med. 2010, 8, 348–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manea, L.; Gilbody, S.; Hewitt, C.; North, A.; Plummer, F.; Richardson, R.; Thombs, B.D.; Williams, B.; McMillan, D. Identifying depression with the PHQ-2: A diagnostic meta-analysis. J. Affect. Disord. 2016, 203, 382–395. [Google Scholar] [CrossRef]
- Sinclair, V.G.; Wallston, K.A. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef]
- Zhang, W.R.; Wang, K.; Yin, L.; Zhao, W.F.; Xue, Q.; Peng, M.; Min, B.Q.; Tian, Q.; Leng, H.X.; Du, J.L.; et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 2020, 89, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Harper, C.A.; Satchell, L.P.; Fido, D.; Latzman, R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addict. 2020, 1–14. [Google Scholar] [CrossRef]
- Sher, L. The impact of the COVID-19 pandemic on suicide rates. QJM Mon. J. Assoc. Physicians 2020, 113, 707–712. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Druss, B.G.; Zhao, L.; Von Esenwein, S.; Morrato, E.H.; Marcus, S.C. Understanding excess mortality in persons with mental illness: 17-year follow up of a nationally representative US survey. Med. Care 2011, 599–604. [Google Scholar] [CrossRef] [PubMed]
- Joukamaa, M.; HeliöVaara, M.; Knekt, P.; Aromaa, A.; Raitasalo, R.; Lehtinen, V. Mental disorders and cause-specific mortality. Br. J. Psychiatry 2001, 179, 498–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nordentoft, M.; Wahlbeck, K.; Hällgren, J.; Westman, J.; Ösby, U.; Alinaghizadeh, H.; Gissler, M.; Laursen, T.M. Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLoS ONE 2013, 8, e55176. [Google Scholar]
- Plana-Ripoll, O.; Pedersen, C.B.; Agerbo, E.; Holtz, Y.; Erlangsen, A.; Canudas-Romo, V.; Andersen, P.K.; Charlson, F.J.; Christensen, M.K.; Erskine, H.E.; et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: A nationwide, register-based cohort study. Lancet 2019, 394, 1827–1835. [Google Scholar] [CrossRef]
- Doran, C.M.; Kinchin, I. A review of the economic impact of mental illness. Aust. Health Rev. 2019, 43, 43–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plancke, L.; Coton, C.; Amariei, A.; Kharfallah, R.; Duhem, S.; Danel, T.; Charrel, C.L. Suicide mortality in people with mental disorders: A register-based study in north France. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 1503–1512. [Google Scholar] [CrossRef]
- Tanaka, T.; Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 2021, 5, 229–238. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Lee, Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020, 290, 113104. [Google Scholar] [CrossRef] [PubMed]
- BNN Baltic News Network. Latvia’s Government to Invest EUR 7.12 Million to Improve Public Mental Health. BNN Baltic News Network. 7 April 2021. Available online: https://bnn-news.com/latvias-government-to-invest-eur-7-12-million-to-improve-public-mental-health-220624 (accessed on 15 May 2021).
- World Health Organization. World Health Organization Pandemic Influenza Preparedness and Response. Retrieved Dec. 2009, 23, 2010. [Google Scholar]
- Kaim, A.; Jaffe, E.; Siman-Tov, M.; Khairish, E.; Adini, B. Impact of a Brief Educational Intervention on Knowledge, Perceived Knowledge, Perceived Safety, and Resilience of the Public During COVID-19 Crisis. Int. J. Environ. Res. Public Health 2020, 17, 5971. [Google Scholar] [CrossRef]
- Rens, E.; Smith, P.; Nicaise, P.; Lorant, V.; Van den Broeck, K. Mental Distress and Its Contributing Factors Among Young People During the First Wave of COVID-19: A Belgian Survey Study. Front. Psychiatry 2021, 12. [Google Scholar] [CrossRef]
- Lorant, V.; Smith, P.; Van den Broeck, K.; Nicaise, P. Psychological distress associated with the COVID-19 pandemic and suppression measures during the first wave in Belgium. BMC Psychiatry 2021, 21, 112. [Google Scholar] [CrossRef] [PubMed]
- The Lancet. India under COVID-19 lockdown. Lancet 2020, 395, 1315. [Google Scholar] [CrossRef]
- Auxier, B.; Anderson, M. Social Media Use in 2021. 7 April 2021. Available online: https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/ (accessed on 3 May 2021).
- Wang, C.; Song, W.; Hu, X.; Yan, S.; Zhang, X.; Wang, X.; Chen, W. Depressive, anxiety, and insomnia symptoms between population in quarantine and general population during the COVID-19 pandemic: A case-controlled study. BMC Psychiatry 2021, 21, 1–9. [Google Scholar] [CrossRef]



Factor | Type of Mental Disorder | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PTSD Correct Class = 79% N = 5288 | GAD Correct Class = 80% N = 5288 | Depression Correct Class = 78% N = 5288 | Panic Disorder Correct Class = 89% N = 5162 | |||||||||
| Effect | p-Value | Exp (B) | Effect | p-Value | Exp (B) | Effect | p-Value | Exp (B) | Effect | p-Value | Exp (B) | |
| Gender (Female = 0) | − | 0.010 | 0.82 | |||||||||
| Age | − | <0.001 | 0.98 | − | <0.001 | 0.99 | − | <0.001 | 0.99 | |||
| Country (Bulgaria = 0) | <0.001 | 0.00 | <0.001 | <0.001 | ||||||||
| United Kingdom | + | 0.023 | 1.49 | + | 0.002 | 1.74 | + | <0.001 | 1.96 | + | 0.031 | 1.65 |
| Belgium | + | 0.001 | 2.16 | + | <0.001 | 3.18 | + | <0.001 | 3.01 | |||
| Netherlands | + | 0.008 | 1.63 | + | <0.001 | 2.09 | + | <0.001 | 1.79 | |||
| Czech Republic | + | <0.001 | 3.58 | + | <0.001 | 3.99 | + | <0.001 | 2.68 | + | <0.001 | 2.97 |
| Finland | + | 0.001 | 1.87 | + | 0.015 | 1.94 | ||||||
| India | + | 0.002 | 1.71 | + | <0.001 | 2.51 | + | <0.001 | 1.54 | + | 0.009 | 1.78 |
| Latvia | + | <0.001 | 1.94 | + | <0.001 | 2.26 | + | <0.001 | 2.28 | + | <0.001 | 2.19 |
| Poland | + | 0.026 | 1.36 | + | <0.001 | 3.01 | + | <0.001 | 2.91 | + | <0.001 | 2.68 |
| Romania | − | 0.003 | 0.70 | |||||||||
| Sweden | + | <0.001 | 2.65 | + | 0.004 | 1.83 | ||||||
| Education (Lower education = 0) | <0.001 | |||||||||||
| Professional and College education | − | 0.014 | 0.66 | |||||||||
| High education | − | <0.001 | 0.54 | |||||||||
| Type Staff (Medical Staff = 0) | 0.041 | 0.027 | 0.003 | |||||||||
| Other essential staff | + | 0.011 | 1.56 | + | 0.001 | 1.75 | ||||||
| Nonessential staff | + | 0.012 | 1.43 | + | 0.013 | 1.44 | + | 0.016 | 1.38 | |||
| Lost Job with Compensation (No Lost Job = 0) | 0.003 | <0.001 | ||||||||||
| Lost job & no payment | + | <0.001 | 1.43 | |||||||||
| Lost job & payment | + | 0.002 | 1.70 | |||||||||
| Covid Infected (No = 0) | ||||||||||||
| Family Infected | ||||||||||||
| Concerned Family | + | <0.001 | 1.06 | |||||||||
| Trust Medical Care | − | 0.002 | 0.96 | |||||||||
| Living alone (Alone = 0) | − | 0.021 | 0.82 | |||||||||
| With Major Life Event (No = 0) | + | <0.001 | 1.71 | + | <0.001 | 1.67 | + | 0.004 | 1.33 | |||
| With Preexisting Mental Disorder (No symptoms = 0) | + | <0.001 | 1.73 | + | <0.001 | 2.87 | + | <0.001 | 2.58 | + | <0.001 | 3.46 |
| Health Condition (No conditions = 0) | ||||||||||||
| Stress Outbreak | + | <0.001 | 1.46 | + | <0.001 | 1.45 | + | <0.001 | 1.28 | + | <0.001 | 1.31 |
| Fear of Infection (None = 0) | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Mild | + | <0.001 | 2.22 | + | 0.002 | 1.39 | + | 0.001 | 1.37 | + | <0.001 | 2.84 |
| Moderate | + | <0.001 | 3.72 | + | <0.001 | 2.58 | + | <0.001 | 2.27 | + | <0.001 | 10.35 |
| Severe | + | <0.001 | 6.50 | + | <0.001 | 5.05 | + | <0.001 | 3.66 | + | <0.001 | 13.28 |
| Extreme | + | <0.001 | 6.00 | + | <0.001 | 9.99 | + | <0.001 | 9.65 | + | <0.001 | 19.10 |
| Trust Government | − | 0.002 | 0.99 | − | <0.001 | 0.95 | ||||||
| Reaction Government | + | 0.015 | 1.03 | |||||||||
| Truthful Government | − | 0.033 | 0.98 | |||||||||
| Time News | + | <0.001 | 1.08 | + | <0.001 | 1.08 | + | <0.001 | 1.08 | |||
| Average Restrictiveness | + | <0.001 | 1.11 | + | <0.001 | 1.06 | + | <0.001 | 1.11 | |||
| Average Compliance | ||||||||||||
| Average Effectiveness | − | <0.001 | 0.92 | − | 0.001 | 0.93 | ||||||
| Number Measures | + | <0.001 | 1.02 | + | 0.014 | 1.02 | ||||||
| Exposure Time Measures | + | 0.008 | 1.01 | |||||||||
 Not significant factors (p ≥ 0.05);
Not significant factors (p ≥ 0.05);  Factors excluded from the analyses due to stepwise selection; “+”factor’s positive effect on the mental disorder; ‘-’ factor’s negative effect on the mental disorder.
Factors excluded from the analyses due to stepwise selection; “+”factor’s positive effect on the mental disorder; ‘-’ factor’s negative effect on the mental disorder.Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Georgieva, I.; Lepping, P.; Bozev, V.; Lickiewicz, J.; Pekara, J.; Wikman, S.; Loseviča, M.; Raveesh, B.N.; Mihai, A.; Lantta, T. Prevalence, New Incidence, Course, and Risk Factors of PTSD, Depression, Anxiety, and Panic Disorder during the Covid-19 Pandemic in 11 Countries. Healthcare 2021, 9, 664. https://doi.org/10.3390/healthcare9060664
Georgieva I, Lepping P, Bozev V, Lickiewicz J, Pekara J, Wikman S, Loseviča M, Raveesh BN, Mihai A, Lantta T. Prevalence, New Incidence, Course, and Risk Factors of PTSD, Depression, Anxiety, and Panic Disorder during the Covid-19 Pandemic in 11 Countries. Healthcare. 2021; 9(6):664. https://doi.org/10.3390/healthcare9060664
Chicago/Turabian StyleGeorgieva, Irina, Peter Lepping, Vasil Bozev, Jakub Lickiewicz, Jaroslav Pekara, Sofia Wikman, Marina Loseviča, Bevinahalli Nanjegowda Raveesh, Adriana Mihai, and Tella Lantta. 2021. "Prevalence, New Incidence, Course, and Risk Factors of PTSD, Depression, Anxiety, and Panic Disorder during the Covid-19 Pandemic in 11 Countries" Healthcare 9, no. 6: 664. https://doi.org/10.3390/healthcare9060664
APA StyleGeorgieva, I., Lepping, P., Bozev, V., Lickiewicz, J., Pekara, J., Wikman, S., Loseviča, M., Raveesh, B. N., Mihai, A., & Lantta, T. (2021). Prevalence, New Incidence, Course, and Risk Factors of PTSD, Depression, Anxiety, and Panic Disorder during the Covid-19 Pandemic in 11 Countries. Healthcare, 9(6), 664. https://doi.org/10.3390/healthcare9060664







