Towards an Open Medical School without Checkerboards during the COVID-19 Pandemic: How to Flexibly Self-Manage General Surgery Practices in Hospitals?
Abstract
:1. Introduction
2. Materials and Methods
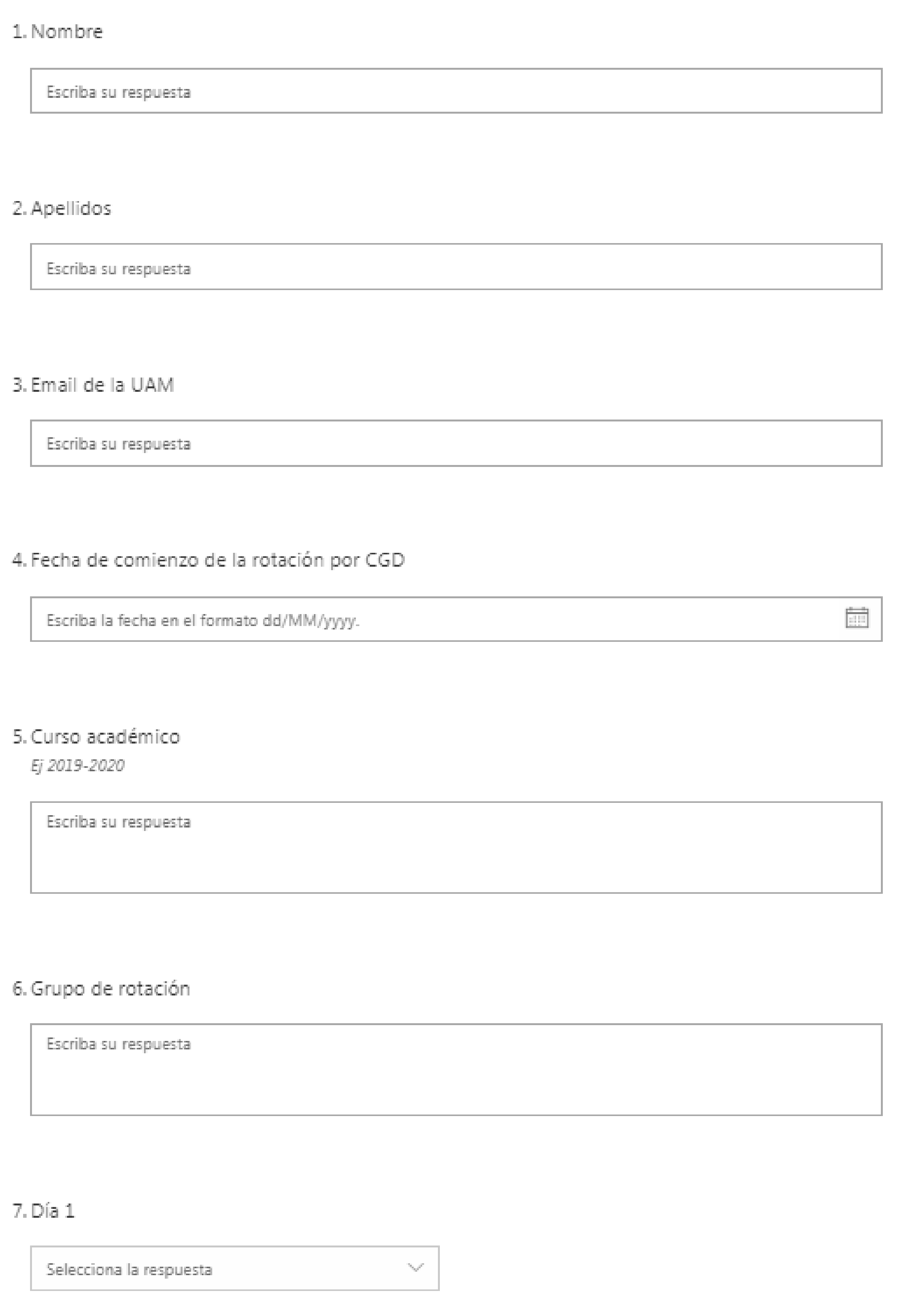
2.1. Pilot Test
2.2. Design
2.3. Participants and Selection Criteria in Each Phase
2.4. Analytical Strategy in Each Phase
2.4.1. Qualitative Analysis
2.4.2. Statistical Analysis
2.5. Ethics
3. Results
3.1. Qualitative Results from the Interviews
3.2. Quantitative Results from the Surveys
3.2.1. Common Student Perceptions of the Four Teaching Hospitals
3.2.2. The Different Student Perceptions of the Four Teaching Hospitals
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Khalifian, S.; Markman, T.; Sampognaro, P.; Mitchell, S.; Weeks, S.; Dattilo, J. Medical student appraisal: Searching on smartphones. Appl. Clin. Inf. 2013, 4, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Ventola, C.L. Mobile devices and apps for health care professionals: Uses and benefits. Pharm. Ther. 2014, 39, 356–364. [Google Scholar]
- Wong, G.; Greenhalgh, T.; Pawson, R. Internet-based medical education: A realist review of what works, for whom and in what circumstances. BMC Med. Educ. 2010, 10, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grainger, R.; Liu, Q.; Geertshuis, S. Learning technologies: A medium for the transformation of medical education? Med. Educ. 2020, 55, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Migliore, M. Smartphones or Tablets for a Better Communication and Education Between Residents and Consultant in a Teaching Hospital. J. Surg. Educ. 2013, 70, 437–438. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Resch, D.; Kovach, R. Educational Technology in Medical Education. Teach. Learn. Med. 2013, 25, S39–S43. [Google Scholar] [CrossRef]
- Koh, K.C.; Wan, J.K.; Selvanathan, S.; Vivekananda, C.; Lee, G.; Ng, C. Medical students’ perceptions regarding the impact of mobile medical applications on their clinical practice. J. Mob. Technol. Med. 2021, 3, 46–53. [Google Scholar] [CrossRef]
- O’Connor, P.; Byrne, D.; Butt, M.; Offiah, G.; Lydon, S.; Mc Inerney, K.; Stewart, B.; Kerin, M.J. Interns and their smartphones: Use for clinical practice. Postgrad. Med. J. 2014, 90, 75–79. [Google Scholar] [CrossRef] [Green Version]
- Rotgans, J. The themes, institutions, and people of medical education research 1988–2010: Content analysis of abstracts from six journals. Adv. Health Sci. Educ. 2012, 17, 515–527. [Google Scholar] [CrossRef]
- Fuller, R.; Joynes, V. Should mobile learning be compulsory for preparing students for learning in the work-place? Br. J. Educ. Technol. 2015, 46, 153–158. [Google Scholar] [CrossRef]
- Rose, S. Medical Student Education in the Time of COVID-19. JAMA Netw. Open 2020, 323, 2131–2132. [Google Scholar] [CrossRef]
- Sandholzer, M.; Deutsch, T.; Frese, T.; Winter, A. Medical students’ attitudes and wishes towards extending an educational general practice app to be suitable for practice: A cross-sectional survey from Leipzig, Germany. Eur. J. Gen. Pract. 2016, 22, 141–146. [Google Scholar] [CrossRef] [Green Version]
- Sandholzer, M.; Rurik, I.; Deutsch, T.; Frese, T. Medical Students’ Expectations Towards an Implementation of a Family Medicine Textbook as a Comprehensive App in Germany. J. Med. Syst. 2014, 38, 125. [Google Scholar] [CrossRef] [Green Version]
- Thistlethwaite, J.E.; Bartle, E.; Chong, A.A.; Dick, M.L.; King, D.; Mahoney, S.; Papinczak, T.; Tucker, G. A review of longitudinal community and hospital placements in medical education: BEME Guide No. 26. Med. Teach. 2013, 35, e1340–e1364. [Google Scholar] [CrossRef]
- Aziz, H.; James, T.; Remulla, D.; Sher, L.; Genyk, Y.; Sullivan, M.E.; Sheikh, M.R. Effect of COVID-19 on surgical training across the United States: A national survey of general surgery residents. J. Surg. Educ. 2021, 78, 431–439. [Google Scholar] [CrossRef]
- Bala, L.; Kinross, J.; Martin, G.; Koizia, L.J.; Kooner, A.S.; Shimshon, G.J.; Hurkxkens, T.J.; Pratt, P.J.; Sam, A.H. A remote access mixed reality teaching ward round. Clin. Teach. 2021, 1–5. [Google Scholar] [CrossRef]
- Ehrlich, H.; McKenney, M.; Elkbuli, A. We asked the experts: Virtual learning in surgical education during the COVID-19 pandemic—Shaping the future of surgical education and training. World J. Surg. 2020, 44, 2053–2055. [Google Scholar] [CrossRef]
- Bazan, D.; Nowicki, M.; Rzymski, P. Medical students as the volunteer workforce during the COVID-19 pandemic: Polish experience. Int. J. Disaster Risk Reduct. 2021, 55, 102109. [Google Scholar] [CrossRef]
- Casafont, C.; Fabrellas, N.; Rivera, P.; Olivé-Ferrer, M.C.; Querol, E.; Venturas, M.; Prats, J.; Cuzco, C.; Frías, C.E.; Pérez-Ortega, S.; et al. Experiences of nursing students as healthcare aid during the COVID-19 pandemic in Spain: A phemonenological research study. Nurse Educ. Today 2021, 97, 104711. [Google Scholar] [CrossRef]
- Shahsavari, H.; Yekta, Z.P.; Houser, M.L.; Ghiyasvandian, S. Perceived clinical constraints in the nurse student–instructor interactions: A qualitative study. Nurse Educ. Pract. 2013, 13, 546–552. [Google Scholar] [CrossRef]
- Varvara, G.; Bernardi, S.; Bianchi, S.; Sinjari, B.; Piattelli, M. Dental Education Challenges during the COVID-19 Pandemic Period in Italy: Undergraduate Student Feedback, Future Perspectives, and the Needs of Teaching Strategies for Professional Development. Healthcare 2021, 9, 454. [Google Scholar] [CrossRef] [PubMed]
- Palés, J.; Gual, A. Medical education in Spain: Current status and new challenges. Med. Teach. 2008, 30, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Martínez-López, J.Á.; Lázaro-Pérez, C.; Gómez-Galán, J.; Fernández-Martínez, M.M. Psychological Impact of COVID-19 Emergency on Health Professionals: Burnout Incidence at the Most Critical Period in Spain. J. Clin. Med. 2020, 9, 3029. [Google Scholar] [CrossRef] [PubMed]
- Custers, E.J.; Cate, O.T. The history of medical education in Europe and the United States, with respect to time and proficiency. Acad. Med. 2018, 93, S49–S54. [Google Scholar] [CrossRef]
- Grasha, A. A matter of style: The teacher as expert, formal authority, personal model, facilitator, and delegator. Coll. Teach. 1994, 42, 142–149. Available online: https://www.jstor.org/stable/27558675?origin=JSTOR-pdf&seq=1 (accessed on 4 June 2021). [CrossRef]
- Collins, K.; Onwuegbuzie, A.; Suttonm, I. A Model Incorporating the Rationale and Purpose for Conducting Mixed-Methods Research in Special Education and Beyond. Learn. Disabil. 2006, 4, 67–100. [Google Scholar]
- Greene, J.; Caracelli, V.; Graham, W. Toward a Conceptual Framework for Mixed-Method Evaluation Designs. Educ. Eval. Policy Anal. 1989, 11, 255–274. [Google Scholar] [CrossRef]
- Johnson, R.; Onwuegbuzie, A. Mixed Methods Research: A Research Paradigm Whose Time Has Come. Educ. Res. 2004, 33, 14–26. [Google Scholar] [CrossRef] [Green Version]
- Myers-Coffman, K.; Baker, F.; Daly, B.; Palisano, R.; Bradt, J. The Resilience Songwriting Program for Adolescent Bereavement: A Mixed Methods Exploratory Study. J. Music Ther. 2019, 56, 348–380. [Google Scholar] [CrossRef]
- Pluye, P.; Hong, Q. Combining the power of stories and the power of numbers: Mixed methods research and mixed studies reviews. Annu. Rev. Public Health 2014, 35, 29–45. [Google Scholar] [CrossRef]
- Warfa, A. Mixed-Methods Design in Biology Education Research: Approach and Uses. CBE Life Sci. Educ. 2016, 15, rm5. [Google Scholar] [CrossRef]
- Dornan, T.; Bundy, C. What can experience add to early medical education? Consensus survey. BMJ 2004, 329, 834–839. [Google Scholar] [CrossRef] [Green Version]
- Wallace, S.; Clark, M.; White, J. ‘It’s on my iPhone’: Attitudes to the use of mobile computing devices in medical education, a mixed-methods study. BMJ Open 2012, 2, e001099. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Surmon, L.; Bialocerkowski, A.; Hu, W. Perceptions of preparedness for the first medical clerkship: A systematic review and synthesis. BMC Med. Educ. 2016, 16, 89. [Google Scholar] [CrossRef] [Green Version]
- Dienstag, J. Evolution of the New Pathway curriculum at Harvard Medical School: The new integrated curriculum. Perspect. Biol. Med. 2011, 54, 36–54. [Google Scholar] [CrossRef]
- Kennedy, T.; Regehr, G.; Baker, G.; Lingard, L. ‘It’s a cultural expectation…’ The pressure on medical trainees to work independently in clinical practice. Med. Educ. 2009, 43, 645–653. [Google Scholar] [CrossRef]
- Birgand, G.; Azevedo, C.; Rukly, S.; Pissard-Gibollet, R.; Toupet, G.; Timsit, J.F.; Lucet, J.C. Motion-capture system to assess intraoperative staff movements and door openings: Impact on surrogates of the infectious risk in surgery. Infect. Control Hosp. Epidemiol. 2019, 40, 566–573. [Google Scholar] [CrossRef]
- Gray, T.; Hood, G.; Farrell, T. The results of a survey highlighting issues with feedback on medical training in the United Kingdom and how a Smartphone App could provide a solution. BMC Res. Notes 2015, 8, 653. [Google Scholar] [CrossRef] [Green Version]
- Aryal, K.; Pereira, J. E Learning in Surgery. Indian J. Surg. 2014, 76, 487–493. [Google Scholar] [CrossRef] [Green Version]
- Wierlemann, A.; Seyfried, F.; Germer, C. Multimediales E-Learning in der Chirurgie, 10 Jahre Erfahrung an der Universität Würzburg [Multimedia E-Learning in Surgery, 10 Years Experience at the University of Würzburg]. Zent. Chir. 2019, 144, 560–572. [Google Scholar] [CrossRef]
- Hau, H.-M.; Weitz, J.; Bork, U. Impact of the COVID-19 Pandemic on Student and Resident Teaching and Training in Surgical Oncology. J. Clin. Med. 2020, 9, 3431. [Google Scholar] [CrossRef] [PubMed]
- Hew, K.; Lo, C. Flipped classroom improves student learning in health professions education: A meta-analysis. BMC Med. Educ. 2018, 18, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romero-Martín, M.; Gómez-Salgado, J.; de la Fuente-Ginés, M.; Macías-Seda, J.; García-Díaz, A.; Ponce-Blandón, J.A. Assessment of reliability and validity of the Spanish version of the Nursing Students’ Perception of Instructor Caring (S-NSPIC). PLoS ONE 2019, 14, e0212803. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, W. Teaching surgery to medical students. Clin. Colon Rectal Surg. 2012, 25, 127. [Google Scholar] [CrossRef] [Green Version]
- O’Brien, B.; Cooke, M.; Irby, D. Perceptions and Attributions of Third-Year Student Struggles in Clerkships: Do Students and Clerkship Directors Agree? Acad. Med. 2007, 82, 970–978. [Google Scholar] [CrossRef]
- Vargo, D.; Zhu, L.; Benwell, B.; Yan, Z. Digital technology use during COVID-19 pandemic: A rapid review. Hum. Behav. Emerg. Technol. 2021, 3, 13–24. [Google Scholar] [CrossRef]
- Southworth, E.; Gleason, S.H. COVID-19: A Cause for Pause in Undergraduate Medical Education and Catalyst for Innovation. HEC Forum 2021, 33, 125–142. [Google Scholar] [CrossRef]
- Hair, J.; Black, W.; Babin, B.; Anderson, R. Multivariate Data Analysis, 7th ed.; Pearson Education: New York, NY, USA, 2009. [Google Scholar]
- Bressan, V.; Bagnasco, A.; Aleo, G.; Timmins, F.; Barisone, M.; Bianchi, M.; Pellegrini, R.; Sasso, L. Mixed-methods research in nursing—A critical review. J. Clin. Nurs. 2017, 26, 2878–2890. [Google Scholar] [CrossRef]
- Irby, D.; Cooke, M.; O’Brien, B. Calls for Reform of Medical Education by the Carnegie Foundation for the Advancement of Teaching: 1910 and 2010. Acad. Med. 2010, 85, 220–227. [Google Scholar] [CrossRef]



| Themes (Overall Frequency) | Subtheme/s (Frequency) | Wording Used in the Survey |
|---|---|---|
| Clerkship and rotations organization (49) | - General organization (25) - 1st day rotation organization (10) - Organizational data prior to surgery/rotation (14) | “The planning and the organization of the rotation activities have been adequate.” |
| Teacher involvement (40) | - Tutor involvement | “The teacher has been concerned about my learning during the rotation.” |
| Adequacy of clerkship content (35) | - Adequacy/Usefulness of the knowledge learned (23) - Variety of training offered (12) | “The content of the practice and the knowledge learned in it have been useful, complete and appropriate to the teaching objectives (of the guide).” |
| Student active participation in clinical clerkship (33) | - Student involvement in routine clinical practice (33) | “Participation in the activities of the Service/Unit during the rotation has been adequate.” |
| Self-management and organizational freedom (25) | - Self-management and organizational freedom (25) | “I positively value the self-management and organizational freedom allowed during the rotation.” |
| Tutor-student relationship (20) | - Doctor-student interaction (16) - Team/Interpersonal Environment (4) | “The doctor-student relationship has been promoted, to increase coordination and communication between both.” |
| Student agglomerations (18) | - Agglomeration of students | “I consider that there have been moments of student agglomeration that have limited my learning.” |
| Reference tutor availability (14) | - Reference teacher/tutor | “I have had a tutor or teaching person of reference to guide me and to whom I can turn.” |
| Attendance supervision methodology and profit of the practices (13) | - Methodology of care control (7) - Signature/time sheets (6) | “The methodology of care control and use of practices by the student has been adequate” |
| Prior academic knowledge related to surgery (13) | - Academic knowledge prior to surgery (8) - Access to medical records (5) | “I have been able to attend the activities of my rotation with sufficient prior academic knowledge to meet the teaching objectives.” |
| Assessment methodology (12) | - Evaluation methodology | “The methodology for evaluating clinical practices has been (clear) and adequate” |
| Student rejection (12) | - Student rejection | “I have received refusal to attend the practical activity from professionals” |
| Adjustment between the students’ practice schedule with the hospital clinical schedule (11) | -Concordance between the schedule of usual clinical practice and the student’s schedule | “The student’s practice schedule is adjusted appropriately to the Hospital’s care schedule.” |
| Adequate teaching and clinical load of the professional/tutor (8) | - Adequacy of the teaching and care load of the professional | “I perceive a teaching and care load from the professional that is adequate to receive quality care” |
| Clerkship time (7) | - Rotation time | “The duration of the general surgery practice rotation is adequate” |
| Workload (6) | - Workload | “There is an excessive workload required from students during rotation” |
| Knowledge of the student’s academic goals held by physicians (5) | - Knowledge of the student’s academic goals held by doctors | “There is adequate knowledge of the student’s objectives from the teaching physicians” |
| Medical facilities (2) | - Facilities | “The facilities used are adequate for my rotation.” |
| Cohesion and equity among hospitals (2) | - Cohesion/Equity among Hospitals | “There is adequate equity in the practices between the different hospitals.” |
| Self-knowledge of the required competencies (1) | - Self-knowledge of the required skills | “I have adequate knowledge about the skills I must obtain and that are required from me during the practices.” |
| Training feedback (1) | - Possibility of feedback | “The possibility of giving feedback on the practices is sufficient and adequate.” |
| Items from the Survey & Responses | Very Unsatisfied | Unsatisfied | Somewhat Satisfied | Satisfied | Very Satisfied | Total |
|---|---|---|---|---|---|---|
| Vx: Item | Fi (%) | Fi (%) | Fi (%) | Fi (%) | Fi (%) | M (±) |
| V1: The doctor-student relationship has been promoted to increase coordination and communication between both. | 8 (7%) | 20 (16%) | 42 (34%) | 40 (32%) | 14 (11%) | 3.26 (1.07) |
| V2: The faculty has been concerned about my learning during the clinical clerkship. | 4 (3%) | 25 (20%) | 46 (37%) | 32 (26%) | 17 (14%) | 3.27 (1.04) |
| V3: The student’s participation in the activities of the Service during the clinical clerkship has been adequate. | 11 (9%) | 25 (20%) | 37 (30%) | 32 (26%) | 19 (15%) | 3.19 (1.19) |
| V4: The training offered has been varied and complete. | 4 (3%) | 11 (9%) | 23 (19%) | 47 (38%) | 39 (32%) | 3.85 (1.07) |
| V5: The content of the practice and the knowledge learned in it have been useful and appropriate to the teaching objectives. | 5 (4%) | 20 (16%) | 37 (30%) | 40 (32%) | 22 (18%) | 3.44 (1.08) |
| V6: I consider that there have been moments of agglomeration of students which have limited my learning. | 15 (12%) | 28 (23%) | 27 (22%) | 27 (22%) | 27 (22%) | 3.19 (1.33) |
| V7: The clinical clerkship plan was defined from the beginning. | 12 (10%) | 8 (7%) | 27 (22%) | 28 (23%) | 49 (40%) | 3.76 (1.30) |
| V8: The planning and organization of the clinical clerkship activities has been adequate. | 4 (3%) | 16 (13%) | 27 (22%) | 51 (41%) | 26 (21%) | 3.64 (1.05) |
| V9: I positively value the self-management and organizational freedom allowed during the clinical clerkship. | 3 (2%) | 6 (5%) | 17 (14%) | 44 (36%) | 54 (44%) | 4.13 (0.99) |
| V10: I have had a tutor of reference to guide me and to whom I can talk to. | 28 (23%) | 34 (27%) | 26 (21%) | 24 (19%) | 12 (9%) | 2.66 (1.29) |
| V11: The methodology of care control and use of the practices by the students has been adequate. | 8 (7%) | 39 (32%) | 41 (33%) | 25 (20%) | 11 (9%) | 2.94 (1.07) |
| V12: I have been able to attend the activities of my clerkship with sufficient prior academic knowledge to meet the teaching objectives. | 21 (17%) | 48 (39%) | 36 (29%) | 14 (11%) | 5 (4%) | 2.47 (1.03) |
| V13: The methodology for evaluating clinical practices has been clear and adequate. | 13 (11%) | 24 (19%) | 22 (18%) | 50 (40%) | 15 (12%) | 3.24 (1.21) |
| V14: I have received refusal to attend the practical activity from professionals. | 27 (22%) | 38 (31%) | 24 (19%) | 19 (15%) | 16 (13%) | 2.67 (1.32) |
| V15: The student’s internship schedule is appropriately adjusted to the hospital’s care schedule. | 7 (6%) | 4 (3%) | 12 (10%) | 50 (40%) | 51 (41%) | 4.08 (1.07) |
| V16: I perceive a teaching and care load from the professional that is adequate to receive quality care. | 8 (7%) | 23 (19%) | 40 (32%) | 37 (30%) | 16 (13%) | 3.24 (1.21) |
| V17: The possibility of giving feedback on the practices is sufficient and adequate. | 22 (18%) | 29 (23%) | 28 (23%) | 35 (28%) | 10 (8%) | 2.85 (1.24) |
| V18: The teaching resources of the hospital are used in a rational way. | 4 (3%) | 23 (19%) | 33 (27%) | 39 (32%) | 25 (20%) | 3.47 (1.11) |
| V19: There is adequate equity in the practices between the different teaching hospitals. | 22 (18%) | 29 (23%) | 47 (38%) | 23 (19%) | 3 (2%) | 2.65 (1.05) |
| V20: You would like to use a mobile app to organize your clinical clerkship in general surgery. | 7 (6%) | 8 (7%) | 23 (19%) | 19 (15%) | 67 (54%) | 4.06 (1.23) |
| Evaluated Variables | TH1. | TH2 | TH3 | TH4 | H(3) | p |
|---|---|---|---|---|---|---|
| Vx: item | Mdn (min–max) | Mdn (min–max) | Mdn (min–max) | Mdn (min–max) | ||
| *V1: The doctor-student relationship has been promoted to increase coordination and communication between both. | 4 (1–5) | 3 (1–4) | 4 (1–5) | 3 (1–5) | 10.883 | 0.012 |
| *V2: The faculty has been concerned about my learning during the clinical clerkship. | 4 (2–5) | 3 (1–5) | 4 (1–5) | 3 (1–4) | 19.112 | <0.001 |
| V3: The student’s participation in the activities of the Service during the clinical clerkship has been adequate | 3 (1–5) | 3 (1–5) | 3 (1–5) | 3 (1–5) | 4.750 | 0.191 |
| V4: The training offered has been varied and complete | 4 (2–5) | 4 (1–5) | 4 (1–5) | 4 (1–5) | 0.788 | 0.853 |
| V5: The content of the practice and the knowledge learned in it have been useful and appropriate to the teaching objectives. | 3 (2–5) | 4 (1–5) | 4 (1–5) | 3 (1–5) | 6.498 | 0.090 |
| V6: I consider that there have been moments of agglomeration of students which have limited my learning. | 3 (1–5) | 3 (1–5) | 4 (1–5) | 2.5 (1–5) | 2.725 | 0.436 |
| *V7: The clinical clerkship plan was defined from the beginning. | 3 (1–5) | 4 (1–4) | 4.5 (1–5) | 4 (1–5) | 8.301 | 0.040 |
| V8: The planning and organization of the clinical clerkship activities has been adequate | 4 (2–5) | 4 (1–5) | 4 (2–5) | 3.5 (1–5) | 6.374 | 0.095 |
| V9: I positively value the self-management and organizational freedom allowed during the clinical clerkship | 4 (1–5) | 4 (1–5) | 4.5 (1–5) | 4 (2–5) | 1.176 | 0.759 |
| *V10: I have had a tutor of reference to guide me and to whom I can talk to. | 3 (1–5) | 2 (1–4) | 3 (1–5) | 2 (1–5) | 17.204 | <0.0001 |
| *V11: The methodology of care control and use of the practices by the students has been adequate. | 3 (1–5) | 2 (1–5) | 3 (2–5) | 2 (1–5) | 13.242 | 0.004 |
| *V12: I have been able to attend the activities of my clerkship with sufficient prior academic knowledge to meet the teaching objectives. | 2 (1–4) | 3 (1–5) | 2 (1–5) | 2 (1–4) | 12.036 | 0.007 |
| *V13: The methodology for evaluating clinical practices has been clear and adequate | 4 (2–5) | 3 (1–5) | 4 (1–5) | 2 (1–5) | 10.500 | 0.015 |
| V14: I have received refusal to attend the practical activity from professionals. | 2 (1–5) | 3 (1–5) | 2 (1–5) | 2 (1–5) | 1.954 | 0.582 |
| *V15: The student’s internship schedule is appropriately adjusted to the hospital’s care schedule. | 5 (1–5) | 4 (1–5) | 4 (1–5) | 5 (2–5) | 7.844 | 0.049 |
| V16: I perceive a teaching and care load from the professional that is adequate to receive quality care. | 3 (1–5) | 4 (1–5) | 3 (1–5) | 3 (1–5) | 2.606 | 0.456 |
| *V17: The possibility of giving feedback on the practices is sufficient and adequate. | 4 (1–5) | 2 (1–5) | 3 (1–5) | 2 (1–5) | 13.292 | 0.004 |
| *V18: The teaching resources of the hospital are used in a rational way. | 4 (2–5) | 3 (1–5) | 4 (1–5) | 3 (1–5) | 9.145 | 0.027 |
| V19: There is adequate equity in the practices among the different teaching hospitals. | 3 (1–5) | 3 (1–5) | 3 (1–4) | 2.5 (1–5) | 4.849 | 0.183 |
| *V20: You would like to use a mobile app to organize your clinical clerkship in general surgery. | 5 (1–5) | 5 (1–5) | 3 (1–5) | 5 (2–5) | 12.092 | 0.007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guadalajara, H.; Palazón, Á.; Lopez-Fernandez, O.; Esteban-Flores, P.; Garcia, J.M.; Gutiérrez-Misis, A.; Baca-García, E.; Garcia-Olmo, D. Towards an Open Medical School without Checkerboards during the COVID-19 Pandemic: How to Flexibly Self-Manage General Surgery Practices in Hospitals? Healthcare 2021, 9, 743. https://doi.org/10.3390/healthcare9060743
Guadalajara H, Palazón Á, Lopez-Fernandez O, Esteban-Flores P, Garcia JM, Gutiérrez-Misis A, Baca-García E, Garcia-Olmo D. Towards an Open Medical School without Checkerboards during the COVID-19 Pandemic: How to Flexibly Self-Manage General Surgery Practices in Hospitals? Healthcare. 2021; 9(6):743. https://doi.org/10.3390/healthcare9060743
Chicago/Turabian StyleGuadalajara, Héctor, Álvaro Palazón, Olatz Lopez-Fernandez, Pilar Esteban-Flores, José Miguel Garcia, Alicia Gutiérrez-Misis, Enrique Baca-García, and Damián Garcia-Olmo. 2021. "Towards an Open Medical School without Checkerboards during the COVID-19 Pandemic: How to Flexibly Self-Manage General Surgery Practices in Hospitals?" Healthcare 9, no. 6: 743. https://doi.org/10.3390/healthcare9060743







